Abstract
KPNβ1, also known as importin β, P97, is reported as one of soluble transport factors that mediates transportion of proteins and RNAs between the nucleus and cytoplasm in cellular process. Recent studies show that KPNβ1 is a tumor gene which is highly expressed in several malignant tumors such as ovarian cancer, cervical tumor, neck cancer, and lung cancer via promoting cell proliferation or inhibiting cell apoptotic pathways. However, the the role of KPNβ1 in gastric cancer remains unclear. In this study, Western blot and immunohistochemistrical analyses showed that KPNβ1 was significantly upregulated in clinical gastric cancer specimens compared with adjacent noncancerous tissues. KPNβ1 was positively correlated with tumor grade, Ki-67, and predicted poor prognosis of gastric cancer. More importantly, through starvation-refeeding model, CCK8 assay, flow cytometry, colony formation assays, the vitro studies demonstrated that KPNβ1 promoted proliferation of gastric cancer cells, while KPNβ1 knockdown led to decreased cell proliferation and arrested cell cycle at G1 phase. Furthermore, our results also indicated that KPNβ1 expression could result in docetaxel resistance. And, KPNβ1 could interact with Stat1, contributed to its nucleus import in gastric cancer cells. These findings provided a novel promising therapeutic targets for clinical treatment against human gastric cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer ranks the fourth malignant tumor with a low postoperative survival rate in all kinds of cancers around the world [1]. Due to its late diagnosis, lack of specificity, high postoperative recurrence, and metastasis, these characteristics seriously affect the total survival rates in patients with gastric cancer [2, 3]. Despite various risk factors such as Helicobacter pylori infection, a high-salt diet, genetic factors, chemical carcinogen are defined participating in the progress of gastric cancer; the exact molecular mechanisms remain unclear [4]. Therefore, it is urgent to identify novel molecules that take part in the regulation of the progression of gastric cancer which may provide new opportunities for the diagnosis and treatment of gastric cancer.
KPNβ1 (also knows as importin β, P97) belongs to karyopherin β family which functions as transporting proteins and RNAs between the nucleus and cytoplasm in a lot of cellular process [5–7]. In general, molecules smaller than approximately 50 kDa can diffuse through the nuclear pore complexes (NPC) passively; however, molecules larger than 50 kDa require active receptor-mediated transport across the NPC for into and out of the nucleus which is completed by importin β [8, 9]. The structure of importin β includes an N-terminal RanGTP-binding motif (RanGTP binding provides the energy required for importin β-mediated transport), a large size between 90 and 130 kDa, an acidic isoelectric point between 4.6 and 5.9, and an ability to interact directly with the NPC [10]. Recently, studies have suggested that KPNβ1 played a crucial role in importing cell cycle proteins, cell signaling proteins, transcription factors, and in this way impacted many of the integral processes in the cells. Furthermore, KPNβ1 can involve in cell cycle regulation by binding E2F transcription factor which is a well-known S phase regulator [11, 12]. However, little is known about the role of KPNβ1 in the development of cancers. Previous studies showed that KPNβ1 expressed at elevated levels in ovarian cancer, cervical tumor tissues via promoting cell proliferation or inhibiting apoptotic pathways [13]. KPNβ1 also played an important role in the progress of head and neck and lung cancer [14]. These findings together implicated that KPNβ1 might serve as a tumor gene and became a potential anticancer therapeutic target.
In our study, we aimed to elaborate a comprehensive analysis of KPNβ1 and its biological characteristics in the development of gastric cancer for the first time. First, we investigated the expression of KPNβ1 in gastric cancer tissues by Western blot analysis and immunohistochemical assay. Then, we examined the correlation between KPNβ1 expression and clinicopathological parameters. Moreover, we explored the ability of KPNβ1 in proliferation and docetaxel resistance in gastric cancer cells by using small interfering RNA (siRNA). At last, our study also showed that KPNβ1 could interact with Stat1 in gastric cancer. These may provide a novel insight into developing experimental therapies in gastric cancer.
Materials and methods
Patients and tissue samples
Eight fresh gastric cancer samples and matched noncancerous samples were stored at −80 °C immediately for Western blot analysis after surgical removal. For immunohistochemical analysis, 150 gastric cancer tissues were obtained from Nantong Tumor Hospital who were diagnosed with gastric cancer during 2007 to 2013. All above tissues were fixed in 10 % buffered formalin and embedded in paraffin for sectioning. The information of 150 specimens included age, gender, tumor grade, infiltration depth, TNM stage, lymph node metastasis, nerve invasion. Resected specimens were classified according to the Seventh Edition of the TNM Classification for Gastric Cancer [1]. All cases for this study were approved of the Ethics Committee of Nantong Tumor Hospital. Signed informed consent was also acquired.
Western blot and antibodies
In order to detect some proteins, Western blot analysis was done as previously detailed [2, 15, 16]. At first, gastric cancer cells and tissues were homogenized in a homogenization buffer (1 M Tris–HCl pH 7.5, 1 % Triton X-100, 10 % sodium sulfate (SDS), 1 % NP-40, 0.5 M EDTA, 0.5 % sodium deoxycholate, 10 μg/mL aprotinin, 1 mM PMSF, 10 μg/mL leupeptin) and then centrifuged at 10,000×g for 30 min to collect the supernatant. The supernatant was diluted in 2× SDS loading buffer, and equal amounts of proteins from each sample were electrophoresed by 10 % sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE). Last, the proteins were transferred on to a polyvinylidene fluoride (PVDF) membrane (Immbilon; Millipore). The membranes were blocked with phosphate-buffered saline (PBS) containing 0.1 % Tween 20 and 5 % nonfat milk, incubated overnight at 4 °C with the primary antibodies described below. After washing with PBST for three times, the membranes were incubated with horseradish peroxidase-conjugated secondary human anti-mouse or anti-rabbit antibodies (1:8000; Pierce Biotechnology) for 2 h at room temperature. Immunecomplexes were visualized by chemiluminescence detection system (NEN Life Science Products, Boston, MA, USA). After the chemiluminescence was exposed to X-ray films, the films were scanned using a Molecular Dynamics densitometer (Imaging Technology, Ontario, Canada). The primary antibodies used were as follows: (1) anti-KPNβ1 (1:500, Santa Cruz Biotechnology), (2) anti-PCNA (1:1000, Santa Cruz Biotechnology), (3) anti-GAPDH (1:1000, Sigma), (4) anti-Cyclin E (1:500, Santa Cruz Biotechnology), (5) anti-Stat1 (1:500, Santa Cruz Biotechnology), (6) anti-LaminB (1:1000, Santa Cruz Biotechnology), (7) anti-aTublin (1:1000, Santa Cruz Biotechnology).
Immunohistochemical analyses
Sections (5 μm thick) of gastric cancer specimens which were formalin-fixed and paraffin-embedded were prepared on glass slides. The sections were deparaffinized in xylene for about 30 min and rehydrated with graded alcohol, furthermore put that in 10 mmol/l citrate buffer (pH 6.0) with an autoclave at 121 °C for 3 min for antigen retrieval. After that, hydrogen peroxide (0.3 %) was used to block endogenous peroxide activity for 20 min. Then, the sections were incubated with the anti-KPNβ1 (1:100, Santa Cruz Biotechnology) and anti-Ki-67 (1:400, Santa Cruz Biotechnology) for 120 min at room temperature. All slides were processed using the peroxidase–antiperoxidase method (Dako, Hamburg, Germany), and the peroxidase reaction was visualized by incubating the sections with DAB. Finally, slides were counterstained with hematoxylin, dehydrated, and mounted in resin mount. In the present study, both the extent of immunoreactivity and the intensity were evaluated and scored in order to quantify KPNβ1, Ki-67 expression. Five high-power fields were chosen randomly for each section, and at least 300 cells were counted per field under a Leica fluorescence microscope (Germany). Intensity was scored as follows: 0, negative staining; 1, weak staining; 2, moderate staining; 3, strong staining. Also, the extent of staining was recorded: 1 (≤25 % tumor cells stained), 2 (26–50 % tumor cells stained), 3 (51–75 % tumor cells stained), 4 (76–100 % tumor cells stained). Then, we multiplied the two scores and classified them into two groups: low expression and high expression. As for statistical analysis of Ki-67, <50 % tumor cells stained as low expression and ≥50 % tumor cells stained as high expression. In order to avoid technical errors, staining was repeated at least three times, and similar results were obtained.
Cell cultures and transfection
The human gastric cell lines MGC803 and HGC27 were purchased from the cell library of the Chinese Academy of Sciences and cultured in RPMI-1640 medium (GIBCO-BRL, Grand Island, NY), while SGC7901 and GES1 were kindly provided by the Department of Pathology Research of Nantong University and cultured in DMEM medium (Life Technologies). All medium were hybridized with 10 % fetal bovine serum at 37 °C in a 5 % CO2 incubator. KPNβ1 small-interfering RNA (siRNA) were designed and synthesized by Shanghai Genechem (China). The siRNA targeting KPNβ1 sequences were as follows: 5′-GAGATCGAAGACTAACAAA-3′ (siRNA#1), 5′-CAGTGTAGTTGTTCGAGAT-3′ (siRNA#2),5′-ACGAGAAGTCAAGAACTAT-3′ (siRNA#3), and 5′-GCTGTTAGTGAGCTAAGTA-3′ (siRNA#4). A nonspecific, scrambled siRNA with a sequence of 5′-UUC UCC GAA CGU GUCACG U-3′ was used as a negative control. According to the manufacturer’s instructions, when the cell density reached 70 %, KPNβ1-siRNA and control siRNA were transfected into gastric cells using lipotransfectamine 2000 (Invitrogen, Carlsbad, CA). Scraping the cell protein for the following experiments after 48 h.
Flow cytometric analysis
For cell cycle analysis, starvation-refeeding model was used. To begin with, MGC803 cells were incubated without fetal bovine serum for 48 h to synchronize cells, then changed into complete medium and collected cells after 0, 4, 8, 12, and 24 h, respectively. Furthermore, cells were fixed in 70 % ethanol for at least 24 h at −20 °C. Subsequently, the cells incubated with 1 mg/mL RNase A for 30 min at 37 °C in PBS, stained with propidium iodide (PI, 50 μg/mL) in PBS-Triton × 100 for an additional 20 min at 4 °C, and analyzed using a Becton Dickinson flow cytometer BD FACScan (San Jose, CA) as well as CellQuest acquisition and analysis programs. For celll apoptosis analysis, MGC803 cells were transfected with KPNβ1-siRNA and control siRNA, then collected the above cells in suspension to each tube and added 60-μL MuseTM Annexin V and Dead Cell Reagent (Part No. 4700–1485, 100 tests/bottle) for incubating for 20 min. The apoptosis assay was completed by MuseTM Cell Analyser (EMD Millipore corporation).
Cell proliferation assay
Cell counting Kit-8(CCK-8) assay was used to detect cell proliferation ability. In brief, cells were seeded onto 96-well cell culture cluster plates (Corning inc, Corning NY) at a density of 2 × 104 cells/well in 100-μL culture after transfecting KPNβ1-siRNA and control siRNA. Then, 10-μL CCK-8 reagents were added to each well for 2-h incubation at 37 °C according to the manufacturer’s instructions. The absorbance was read at the wavelength of 490 nm in an automated plate reader. The experiments must repeat at least three times.
Colony formation assays
Cells were cultivated in 6-well culture plates at a density of 200 cells/well after transfecting KPNβ1-siRNA and control siRNA. After 2 weeks, the cell colonies (≥50 cells/colony) were counted by staining with 0.5 % crystal violet.
Immunofluorescent staining
First, cells were fixed with 4 % paraformaldehyde-PBS for about 30 min at room temperature and washed 5 min three times with PBS. Second, cells were blocked with 1 % BSA in PBS for 2 h and incubated with primary antibodies (anti-KPNβ1, 1:100, Santa Cruz Biotechnology; anti-Stat1, 1:100, Santa Cruz Biotechnology) overnight at 4 °C. At last, the cells were incubated with AlexFluor-conjugated secondary antibodies (Molecular Probe, Inc), counterstained with hochest after being washed with PBS 5 min three times. The assay was showed through a fluorescence microscope (Leica CTR 5000).
Statistical analysis
All statistical analysis was carried out using the SPSS statistics 19 software package. The expression of KPNβ1, Ki-67, and clinical pathological parameters was analyzed using the χ2 test. Survival curve analysis was performed using the Kaplan-Meier method and tested with the log-rank test. Multivariate analysis of Cox proportional hazards model was used to identify independent prognostic factors for gastric cancer samples. P < 0.05 was considered statistically significant.
Results
The expression of KPNβ1 was upregulated in gastric cancer cell lines and tissues
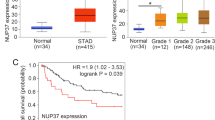
Since it was reported that KPNβ1 could participate in the progression of cancers such as ovarian cancer, cervical cancer [13], it was interesting to explore the role of KPNβ1 in the progression of gastric cancer. We investigated the expression of KPNβ1 in eight fresh gastric cancer tissues and adjacent normal tissues. We found that KPNβ1 was obviously upregulated in gastric cancer tissues compared with adjacent normal tissues. More importantly, KPNβ1 was consistent with the expression of PCNA (Fig. 1a, b). Then, we explored the expression of KPNβ1 in normal gastric epithelial cell GES1 and several gastric cancer cells including SGC7901, MGC803, HGC27 by Western blot. As expected, KPNβ1 was highly expressed in gastric cancer cell lines than in normal gastric epithelial cell (Fig. 1c). Moreover, immunohistochemical (IHC) analyses were used for further study among 150 gastric cancer samples. KPNβ1 was highly expressed in the cytoplasm and nucleus in gastric cancer tissues than the normal tissues. At the same time, we found that KPNβ1 had a remarkably higher expression in poorly differentiated specimens than in well-differentiated specimens as well as the expression of Ki-67 (Fig. 2). After that, Pearson’s correlation coefficient was also used to analyze the correlation between KPNβ1 and Ki-67. Figure 3a shows that they had a positive correlation with a coefficient of r =0.638 (P < 0.001). All the above data suggested that KPNβ1 might contribute to the development of gastric cancer.
The KPNβ1 and PCNA expression in eight paired gastric cancer tissues (T) and adjacent normal tissues (N). a Eight paired tissues of gastric cancer (T) and adjacent normal tissues (N) were analyzed by Western blot analysis. The KPNβ1 expression was significantly higher in gastric cancer compared with adjacent normal tissues. b The bar chart showed the ratio of KPNβ1 protein to GADPH. Mean ± SD of three independent experiments. *P < 0.05 compared with control nontumorous adjacent tissues. c The KPNβ1 expression was upregulated in three gastric cancer cells compared with normal gastric epithelial cell
Immunohistochemical evaluation of the expression of KPNβ1 and Ki-67 in 150 gastric cancer and noncancerous tissues. a, b Negative staining of KPNβ1 and Ki-67 in adjacent normal tissues; c, d weak staining of KPNβ1 and Ki-67 in well-differentiated gastric cancer tissues; e, f moderate staining of KPNβ1 and Ki-67 in moderately differentiated gastric cancer tissues; g, h strong staining of KPNβ1 and Ki-67 in poorly differentiated gastric cancer tissues, amplification (×200)
a Pearson correlation analysis of the expression of KPNβ1 and proliferation index Ki-67 in 150 gastric cancer specimens. KPNβ1 was postively correlated with Ki-67 (r = 0.638 , P < 0.001). b Kaplan–Meier survival curves for KPNβ1 expression in 150 gastric cancer tissues. Patients in the high-expression KPNβ1 group had a significantly shorter overall survival (P < 0.05)
Overexpression of KPNβ1 is associated with poor prognosis in gastric cancer
To evaluate the correlation between KPNβ1 expression and clinicopathological factors, immunohistochemistry analysis was performed in 150 gastric cancer samples. As listed in Table 1, high expression of KPNβ1 was positively associated with tumor grade (P = 0.013), infiltration depth (P = 0.000), Ki-67 expression (P = 0.008). However, there was no significant relation between KPNβ1 and other prognostic factors such as age, gender, nerve invasion, lymph node metastasis, and TNM stage. According to the above data, we hypothesized that KPNβ1 was an independent prognostic factor to predict patient’s survival. Interesting univariate survival analysis showed that tumor grade (P = 0.017), KPNβ1 expression (P = 0.000), and Ki-67 expression (P = 0.049) were prognostic factors of overall survival (Table 2). Besides, multivariate analysis of the Cox proportional hazards model suggested that KPNβ1 was an independent prognostic indicators of patients’ overall survival (P = 0.002; Table 3). What is more, Kaplan-Meier analysis of 150 patients’ survival status showed that patients with high expression of KPNβ1 had a poorer survival compared with low expression of KPNβ1 (P < 0.05, Fig. 3b). These research highlighted that KPNβ1 could serve as a poor prognostic indicator of gastric cancer.
KPNβ1 was highly expressed in proliferating gastric cancer cells
Since we had demonstrated the role of KPNβ1 in gastric cancer tissues, then we used gastric cancer cell lines to do a deeper research. Due to the above mentioned, high expression of KPNβ1 was mainly associated with poorly tumor grade and Ki-67 expression, we next speculated whether KPNβ1 might influence the proliferation of cells by starvation-refeeding model. MGC803 cells were arrested in G1 phase by serum deprivation for 72 h and then changed RPMI-1640 medium with 10 % fetal bovine serum which led the cells entered S phase. Flow cytometry analysis showed that cells were arrested in G1 phase after serum starvation. Then, after serum readdition as time went on, the S phase was increased from 7.36 to 43.09 % (Fig. 4a, b). In order to detect the proliferation ability of KPNβ1, Western blot revealed that as the the time of serum addition extended, KPNβ1 expression became higher. And, the trend of PCNA, Cyclin E, is the same as KPNβ1, whereas the expression of P21 was reduced (Fig. 4c, d). All these results suggested that KPNβ1 might serve as a positive regulator in the progress of cell proliferation.
KPNβ1 was upregulated in proliferating gastric cells. Cell cycle distribution was measured in MGC803 cells by flow cytometry analysis. a, b Cells were arrested in G1 phase by serum deprivation for 72 h and then entered S phase at different time points (S6, S12, S24, S48). Mean ± SD of three independent experiments. (*, #, P < 0.05). c, d The starvation-refeeding model in MGC803 cells was analyzed by Western blot using antibodies against KPNβ1, Cyclin E, P21, PCNA, and GAPDH (loading control). The bar chart below showed the ratio of KPNβ1, Cyclin E, P21, PCNA to GAPDH by densitometry. Mean ± SD of three independent experiments. (*, #, ^, $, P < 0.05)
Knockdown of KPNβ1 inhibited proliferation of gastric cancer cells
In order to further understand the role of KPNβ1 on cell growth, chemically synthesized KPNβ1-siRNA and control siRNA were transfected into MGC803 cells when cell density reached 70 %. After 48 h, cell proteins were collected to choose the highest interference efficiency by Western blot analysis. Figure 5a shows that KPNβ1-siRNA#1 had a significant higher interference efficiency compared with other three si-RNA. So, we use KPNβ1-siRNA#1 to complete the following experiments. Importantly, we observed a significant reducion of Cyclin E and PCNA and a elevation of P21 in KPNβ1-depleted cells (Fig. 5b). Cell Counting Kit-8 (CCK-8) assay and colony-forming assay also proved that the proliferation ability was cut down in KPNβ1-siRNA#1-transfected cells compared with control siRNA cells (Fig. 5c, d). To understand which phase of the cell cycle did KPNβ1 might affect, we performed flow cytometrical analysis after transient transfection KPNβ1-siRNA and control siRNA. Flow cytometrical analysis showed that KPNβ1 knockdown led to an increased population in G1 phase, and a decreased population in S phase, which suggested that KPNβ1 promoted G1-S conversion, thus increased cell proliferation (Fig. 5e).
Knockdown of KPNβ1 suppressed cell proliferation. a KPNβ1 expression was measured by Western blot after transfecting KPNβ1-siRNA for 48 h in MGC803 cells, and KPNβ1-siRNA#1 achieved the highest interference efficiency. The relative level of KPNβ1 was tested by densitometry. Mean ± SD of three independent experiments (*, P < 0.05). b Cell cycle related proteins such as PCNA, Cyclin E were measured by Western blot. The expression of PCNA, Cyclin E was downregulated in KPNβ1-siRNA#1 cells compared with control. c, d CCK-8 and colony-forming assay were used to detect cell proliferation. MGC803 cells treated with KPNβ1-siRNA#1 revealed a weaken proliferation. The results are responsible for three independent experiments. e Cell cycle analysis was used to show the role of KPNβ1. KPNβ1 depletion resulted in increasing cell population in G1 phase and decreasing cell population in S phase
The expression of KPNβ1 in gastric cancer cells resulted in docetaxel resistance
As is known to all, docetaxel was a potent antitumor drug which was often used in clinical treatment of gastric cancer and many other cancers [17, 18]. First, we added docetaxel from low to high concentrations in the MGC803 cells to select a most effective inhibitory concentration (0.1 μmol/L) by CCK-8 (Fig. 6a). Second, we performed the contribution of KPNβ1 to docetaxel sensitivity by Annexin V-FITC/PI double staining. Figure 6b demonstrates that docetaxel or KPNβ1-siRNA#1 alone induced cell apoptosis, while added together further increased cell apoptosis. To confirm the results, Western assay was used to detect apoptosis-related proteins such as Bcl-2, P21, and active caspase 3. figure 6c shows that knockdown KPNβ1 led to increased expression of active caspase 3 and inhibited expression of P21, Bcl-2, no matter if there is docetaxel addition or not. Adding docetaxel and KPNβ1-siRNA#1 together had a more obvious effect. The above results suggested that KPNβ1 expression might contribute to docetaxel resistance due to its antiapoptotic ability.
The effects of KPNβ1 on the sensitiveness of docetaxel in gastric cancer cells. a CCK8 assays showed cell growth rate with different concentration of docetaxel addition in MGC803 cells. Data represented mean ± SEM from three independent experiments. b Silencing KPNβ1 could promote cell apoptosis which was triggered by docetaxel in MGC803 cells by Annexin V-FITC/PI double staining. c Apoptosis-related proteins such as Bcl-2, P21, and active caspase 3 were measured by Western blot when knockdown KPNβ1 with or without docetaxel addition
KPNβ1 interacted with Stat1 and contributed to its nucleus import, then by this pathway to inhibit apoptosis
As KPNβ1 could transport proteins into nuclear, Stat1 was one of the common nuclear pathway and controlled cell proliferation and apoptosis [19]. Evidence showed that STAT1 correlated negatively with gastric cancer tissues [20]. It was interesting to explore the relationship between KPNβ1 and STAT1. The research showed that KPNβ1 could interact with Stat1 by immunoprecipitation in MGC803 cells and gastric cancer tissues (Fig. 7a). And, the cell immunofluorescence also showed the costaining of the KPNβ1 and Stat1 proteins and proved that their interaction was mainly in the nucleus (Fig. 7b). To further investigate the contribution of KPNβ1 on Stat1, we used siRNA to knockdown the KPNβ1. Stat1 was measured in the cytoplasm and nucleus, respectively. figure 7c, d shows that Stat1 was increased in the cytoplasm and reduced in the nucleus after KPNβ1 knockdown by immunofluorescent and Western blot. As is known to all, P21 is the downstream of Stat1, and we had proved that P21 was negatively associated with KPNβ1. This might suggest that KPNβ1 transported Stat1 and by this control apoptosis. But, the mechanism needed further research.
KPNβ1 interact with Stat1 and contributes to its nuclear import. a MGC803 cells and gastric cancer tissues were immunoprecipitated with antibodies against KPNβ1, Stat1, and analyzed by immunoblotting with the indicated antibodies. b Immunofluorescent was used to show costaining of the KPNβ1, Stat1 proteins and their localization and interaction. c Immunofluorescent was used to show the change of location of Stat1. d The levels of Stat1 were analyzed in cytoplasmic and nuclear extracts from control and KPNβ1-siRNA#1 cells by Western blot
Discussion
Despite the development of the diagnosis and treatment technology of gastric cancer, the prognosis of gastric cancer patients remained unsatisfied. The patients with gastric cancer often appeared chemoresistance, relapse, and high metastasis rate in postoperative. The tumorigenesis of gastric cancer was associated with some biological events such as H. pylori infection, genetic factors, chemical carcinogen [21]. So, it was a huge challenge to explore the specific molecular mechanism involved in the process of gastric cancer. It was reported that KPNβ1 involved in the development of ovarian cancer, cervical cancer, and lung cancer [13, 14]. In this study, we described the role of KPNβ1 in gastric cancer for the first time. We found that KPNβ1 expression was upregulated in gastric cancer tissues compared with adjacent normal tissues and significantly correlated with several clinicopathological characteristics including tumor grade, Ki-67. In addition, KPNβ1 could serve as an independent prognostic indicator of patients’ survival by Cox’s proportional hazards model. The above data proved that KPNβ1 might be a novel prognostic indicator and therapeutic target of gastric cancer.
In vitro, our study showed that KPNβ1 could inhibit cell growth after transfecting KPNβ1-siRNA#1 into gastric cancer cells by starvation-refeeding model, CCK-8, colony formation assay. Flow cytometry analysis showed that KPNβ1 acted as an important cell cycle regulator during G1-S phase. These results are consistent with the function of KPNβ1 in cervical cancer, head and neck cancer, nerve cells [22]. Then, we analyzed the impact of KPNβ1 on apoptosis and docetaxel resistance. Notably, through flow cytometry and Western blot, Fig. 6 shows that silencing KPNβ1 could increase the expression of apoptosis-related proteins such as Bcl-2, P21, active caspase 3 and expand the cytotoxic effect of docetaxel in MGC803 cells.
KPNβ1 was one of soluble transport factors that functioned as transporting proteins and RNAs between the nucleus and cytoplasm; evidence showed that it could transport NF-kappaB/P65, Erk1, Erk2, SOX9, Smad3 into the nucleus [23–26]. It was interesting to find that KPNβ1 could interact with Stat1 and contribute to its nucleus import (Fig. 7). The potential function of STAT1 in cancer was supported by several observations that STAT1 inappropriate activation and even loss of its expression in malignant tumors such as breast cancer, ovarian cancer, colorectal cancer [27–29]. And, the result was the same for gastric cancer [20]. STAT1 mainly controlled cell proliferation, apoptosis, and immune system [19]. KPNβ1 transported Stat1 into the nucleus, while knocking down of KPNβ1 made Stat1 mainly locate in the nucleus. P21 is the downstream of Stat1 [30], KPNβ1 might be through transferring Stat1 and regulating P21 to control apoptosis in gastric cancer cells. But, the mechanism remained to be further studied in-depth.
In summary, this study for the first time showed that KPNβ1 was significantly highly expressed in gastric cancer and was correlated with tumor grade as well as poor prognosis. Furthermore, silencing KPNβ1 restrained cell growth and increased sensitivity to docetaxel in gastric cancer cells. KPNβ1 could interact with Stat1, contributed to its nucleus import in gastric cancer cells.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Zhang D, Sun L, Zhu H, Wang L, Wu W, Xie J, et al. Microglial lox-1 reacts with extracellular hsp60 to bridge neuroinflammation and neurotoxicity. Neurochem Int. 2012;61:1021–35.
Cao Y, DePinho RA, Ernst M, Vousden K. Cancer research: past, present and future. Nat Rev Cancer. 2011;11:749–54.
de Martel C, Forman D, Plummer M. Gastric cancer: epidemiology and risk factors. Gastroenterol Clin N Am. 2013;42:219–40.
Gorlich D, Kutay U. Transport between the cell nucleus and the cytoplasm. Annu Rev Cell Dev Biol. 1999;15:607–60.
Kutay U, Izaurralde E, Bischoff FR, Mattaj IW, Gorlich D. Dominant-negative mutants of importin-beta block multiple pathways of import and export through the nuclear pore complex. EMBO J. 1997;16:1153–63.
Kau TR, Way JC, Silver PA. Nuclear transport and cancer: from mechanism to intervention. Nat Rev Cancer. 2004;4:106–17.
Harel A, Forbes DJ. Importin beta: conducting a much larger cellular symphony. Mol Cell. 2004;16:319–30.
van der Watt PJ, Stowell CL, Leaner VD. The nuclear import receptor kpnbeta1 and its potential as an anticancer therapeutic target. Crit Rev Eukaryot Gene Expr. 2013;23:1–10.
Moroianu J. Distinct nuclear import and export pathways mediated by members of the karyopherin beta family. J Cell Biochem. 1998;70:231–9.
Quan Y, Ji ZL, Wang X, Tartakoff AM, Tao T. Evolutionary and transcriptional analysis of karyopherin beta superfamily proteins. Mol Cell Proteomics. 2008;7:1254–69.
van der Watt PJ, Ngarande E, Leaner VD. Overexpression of kpnbeta1 and kpnalpha2 importin proteins in cancer derives from deregulated e2f activity. PLoS One. 2011;6:e27723.
van der Watt PJ, Maske CP, Hendricks DT, Parker MI, Denny L, Govender D, et al. The karyopherin proteins, crm1 and karyopherin beta1, are overexpressed in cervical cancer and are critical for cancer cell survival and proliferation. Int J Cancer. 2009;124:1829–40.
Martens-de Kemp SR, Nagel R, Stigter-van Walsum M, van der Meulen IH, van Beusechem VW, Braakhuis BJ, et al. Functional genetic screens identify genes essential for tumor cell survival in head and neck and lung cancer. Clin Cancer Res. 2013;19:1994–2003.
Ji Y, Tao T, Cheng C, Yang H, Wang Y, Yang J, et al. Ssecks is a suppressor in schwann cell differentiation and myelination. Neurochem Res. 2010;35:219–26.
Liu Y, Chen Y, Lu X, Wang Y, Duan Y, Cheng C, et al. Scyl1bp1 modulates neurite outgrowth and regeneration by regulating the mdm2/p53 pathway. Mol Biol Cell. 2012;23:4506–14.
Roth AD, Ajani J. Docetaxel-based chemotherapy in the treatment of gastric cancer. Ann Oncol. 2003;14 Suppl 2:ii41–4.
Ajani JA. Docetaxel for gastric and esophageal carcinomas. Oncology. 2002;16:89–96.
Adamkova L, Souckova K, Kovarik J. Transcription protein stat1: biology and relation to cancer. Folia Biol. 2007;53:1–6.
Deng H, Zhen H, Fu Z, Huang X, Zhou H, Liu L. The antagonistic effect between stat1 and survivin and its clinical significance in gastric cancer. Oncol Lett. 2012;3:193–9.
Milne AN, Carneiro F, O’Morain C, Offerhaus GJ. Nature meets nurture: molecular genetics of gastric cancer. Hum Genet. 2009;126:615–28.
Zhang P, Yang X, Ma X, Ingram DR, Lazar AJ, Torres KE, et al. Antitumor effects of pharmacological ezh2 inhibition on malignant peripheral nerve sheath tumor through the mir-30a and kpnb1 pathway. Mol Cancer. 2015;14:55.
Liang P, Zhang H, Wang G, Li S, Cong S, Luo Y, et al. Kpnb1, xpo7 and ipo8 mediate the translocation ofnf-kappab/p65 into the nucleus. Traffic. 2013;14:1132–43.
Perlson E, Hanz S, Ben-Yaakov K, Segal-Ruder Y, Seger R, Fainzilber M. Vimentin-dependent spatial translocation of an activated map kinase in injured nerve. Neuron. 2005;45:715–26.
Malki S, Nef S, Notarnicola C, Thevenet L, Gasca S, Mejean C, et al. Prostaglandin d2 induces nuclear import of the sex-determining factor sox9 via its camp-pka phosphorylation. EMBO J. 2005;24:1798–809.
Kurisaki A, Kose S, Yoneda Y, Heldin CH, Moustakas A. Transforming growth factor-beta induces nuclear import of smad3 in an importin-beta1 and ran-dependent manner. Mol Biol Cell. 2001;12:1079–91.
Bowman T, Garcia R, Turkson J, Jove R. Stats in oncogenesis. Oncogene. 2000;19:2474–88.
Stronach EA, Alfraidi A, Rama N, Datler C, Studd JB, Agarwal R, et al. Hdac4-regulated stat1 activation mediates platinum resistance in ovarian cancer. Cancer Res. 2011;71:4412–22.
McDermott U, Longley DB, Galligan L, Allen W, Wilson T, Johnston PG. Effect of p53 status and stat1 on chemotherapy-induced, fas-mediated apoptosis in colorectal cancer. Cancer Res. 2005;65:8951–60.
Gooch JL, Herrera RE, Yee D. The role of p21 in interferon gamma-mediated growth inhibition of human breast cancer cells. Cell Growth Differ. 2000;11:335–42.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No.81302285, No. 81402015); the Natural Science Foundation of Nantong University (No.12Z009).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jia Zhu and Yingying Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhu, J., Wang, Y., Huang, H. et al. Upregulation of KPNβ1 in gastric cancer cell promotes tumor cell proliferation and predicts poor prognosis. Tumor Biol. 37, 661–672 (2016). https://doi.org/10.1007/s13277-015-3839-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3839-7