Abstract
Ovarian cancer is the most deadly gynecological cancer. The first line in treatment is platinum-based drugs. However, most patients suffer from tumor recurrence, characterized by resistance to cisplatin. A plausible approach to address the tumor resistance is to co-administer the chemotherapeutic agents along with natural products to offer a synergistic effect and optimize the dosage regimen. Cucurbitacin B is a natural product and displays antitumor activity against a wide array of cancer cell lines. The aim of this work is to determine the antitumor activity against ovarian cancer cell line (A2780) and possible sensitization activity on cisplatin-resistant cell line (A2780CP) in 2D and 3D culture model. 3D spheroids were generated from A2780CP cell line. A2780, A2780CP, and the spheroids were treated with cucurbitacin B, cisplatin alone, or pretreated with cucurbitacin B followed by cisplatin. The viability, cell cycle, and apoptosis were analyzed. Level of ROS and total glutathione was measured. In this study, cucurbitacin B showed cytotoxicity against the ovarian cancer cell lines, and pretreatment of A2780CP cells leads to a significant increase in the cytotoxicity of cisplatin. The mechanism behind the sensitization effect was dependent in part on the depletion of the total glutathione, an increase in ROS through a decrease in the level of dual-specificity tyrosine-regulated kinase (Dyrk1B), decrease in pERK1/2 and pSTAT3 level. The viability of spheroids treated with a combination of cisplatin and cucurbitacin B were significantly decreased. The resulting data shows that cucurbitacin B is a promising chemosensitizer for the cisplatin-resistant ovarian cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is the most deadly gynecological cancer and known as a “silent killer” because, when diagnosed, the disease usually has already spread into the peritoneum through the detachment of spheroids. The 5-year survival rate is over 90 % for patients who are diagnosed early and decreases to 30 % for late diagnoses [1, 2]. The spheroids are resistant to the common therapeutic drugs such as cisplatin. The resistance could be in part due to the low penetration rate of the drug through the spheroids, hypoxic conditions, and the low proliferating cells inside the spheroid, dormant [3, 4]. The first line in chemotherapy for ovarian cancer is platinum-based drugs. These are typically administered as a single drug or in a combination with taxanes. However, most patients suffer from tumor recurrence, characterized by resistance to cisplatin. There are different mechanisms in the resistance induction such as the overexpression of drug-efflux proteins, increasing the redox proteins leading to drug inactivation, elevating DNA damage tolerance, and enhancing antiapoptotic proteins [5, 6]. Therefore, an urgent need remains to find a novel approach in the treatment of drug-resistant ovarian cancer. A plausible approach to address the tumor resistance is to co-administer the chemotherapeutic agents along with natural products to offer a synergistic effect and optimize the dosage regimen.
Nuclear factor kappa B (NFκB) is one of the transcription factors that regulate the gene expression of several genes responsible for regulating immune, stress response, and cell survival. NFκB induces the expression of antiapoptotic genes in response to either the death receptor or mitochondrial apoptosis [7]. Those antiapoptotic proteins such as cellular inhibitor of apoptosis (c-IAP) and X-chromosome linked IAP (XIAP) [8] increase the rate of resistance of tumor to the chemotherapeutic drugs. Signal transducer and activator of transcription 3 (STAT3), on activation, its phosphorylated form translocates into the nucleus leading to the expression of genes required for different physiological functions such as cell proliferation, differentiation, and survival [9]. pSTAT3 was found in greater levels in the drug-resistant cell lines and in the high-grade ovarian cancers [10, 11]. Recently, it was revealed that silencing STAT3 in resistant ovarian cancer cells leads to an increase in the apoptotic rate [12]. Taking together, these data suggest that STAT3 is an emerging molecular target for treatment of these types of tumors [9, 12].
Extracellular-regulated kinase (ERK1/2) belongs to mitogen-activated protein (MAP) kinases which regulates cell growth, differentiation, and survival in response to an extracellular signal such as growth factors [13]. In addition to the prosurvival role of ERK1/2, it induces apoptosis as well. The persistent activation of ERK1/2 leads to glutamate-induced oxidative cytotoxicity in neuronal cells [14]. DNA damage by chemotherapeutic drugs such as cisplatin and etoposide, adriamycin, and ionizing irradiation activates ERK1/2, which, in turn, activates proapoptotic proteins such as BAX and the release of cytochrome c into the cytoplasm. Contrary to the previous report of ERK1/2 activation, it was found that inhibition of ERK1/2 sensitizes ovarian cancer cells to cisplatin cytotoxicity [15, 16]. It can be concluded from this conflicting reported data, ERK1/2 possesses a dual function (proapoptotic and antiapoptotic). Wulfkuhle et al. has shown via coupling reverse-phase protein array technology with laser capture microdissection that the signaling pathway such as ERK1/2 and its phosphorylation state may be a patient-dependent rather than stage type. This hypothesis is a result of the pERK1/2 level only being slightly higher in late stage but considerably different within the same stage [17].
Following cytoreductive surgery and chemotherapy of ovarian cancer, deposits of residual tumors, spheroids, can be found in half of the patients. The recurrent tumor in these patient does not respond to chemotherapy [18]. The cells in dormant state (quiescent state) can resist the nutrient deficiency, hypoxia, and acidic conditions. Dual-specificity tyrosine-regulated kinase (Dyrk1B), also known as minibrain-related kinase (Mirk), is a serine/threonine kinase. It plays a role in maintaining the viability of quiescent cells by reducing the level of the reactive oxygen species (ROS) via upregulation of antioxidant enzymes, superoxide dismutase, and ferroxidase in ovarian cancer cells. The depletion of Dyrk1B by miRNA leads to the sensitization of the resistant cells to cisplatin [19]. Elevated levels of reduced glutathione in different cancer types leads to an increase in the drug resistance due to the inactivation of cisplatin by conjugation to the nucleophilic group, increasing the DNA repair [20] or elevated level of the antiapoptotic B cell lymphoma 2 (Bcl-2) protein [21].
Therefore, co-administration of natural products along with chemotherapeutic agents has been investigated as a potential therapeutic approach toward sensitization of the resistant cells toward platinum-based compounds. Cucurbitacins are tetracyclic triterpene natural products that are mainly found in the members of family Cucurbitaceae. In India and China, it is used as remedies because they exhibit different biological activities such as antiinflammatory, antidiabetic, and anticancer activities against different cancer cell lines [22]. Cucurbitacin B displays antitumor activity against a wide array of cancer cell lines such as breast, colon, leukemia, hepatic, pancreatic and glioblastoma, and xenografts [22–24]. Cucurbitacin B possesses synergetic activity with cisplatin in squamous cell carcinoma [25], gemcitabine in the treatment of pancreatic cancer [26], and methotrexate in osteosarcoma treatment [27].
The effect of cucurbitacin B on ovarian cancer cell lines previously has not been evaluated. The aim of this work is to determine the antitumor activity against ovarian cancer cell line (A2780) and possible sensitization activity of cucurbitacin B on cisplatin-resistant ovarian cancer cell line (A2780CP) in 2D and 3D culture model. 3D cell culture has proven to be a physiologic mimic of the in vivo tissue because they produce a similar cellular microenvironment [28, 29].
Material and methods
Ovarian cancer cell lines and the drugs
The cisplatin-sensitive (A2780) and cisplatin-resistant (A2780CP) ovarian cancer cell lines [30] were obtained from Dr. Stephen Howell, University of California, San Diego. The cells were maintained in RPMI-1640 (Thermoscientific™ Hyclone™) supplemented with 10 % fetal bovine serum (FBS) (Thermoscientific™ Hyclone™) and 1 % pencillin (100 IU/mL)/streptomycin (100 μg/mL) (Corning™Cellgro™). In order to maintain the resistance, 1 μM cisplatin was added to the medium every two to three passages. Cisplatin (cis-diamineplatinum(II) dichloride) was obtained from Sigma and dissolved in 0.9 % saline then stored as 8 mM stock solution at −20 °C. Cucurbitacins were isolated from Cucurbita texana and characterized by spectroscopic techniques [31].
Cytotoxicity assay
The sensitive ovarian cancer cells (A2780) and the cisplatin-resistant cells (A2780CP) were seeded in 96-well plate as 5 × 104 cells/mL (100 μL/well). A serial dilution of cucurbitacins was added after overnight incubation of the cells at 37 °C and 5 % CO2. Dimethyl sulfoxide (DMSO) was used as a control (0.1 %). The cells were incubated with the cucurbitacin or cisplatin for 48 h. After that, 15 μL of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) (5 mg/mL phosphate-buffered saline (PBS)) were added to each well, and the plate was incubated for another 4 h. The formazan crystals were solubilized by 100 μL acidified sodium dodecyl sulfate (SDS) solution (10 % SDS/0.01 NHCl). The absorbance was measured after 14 h of incubation at 37 °C and 5 % CO2 at 570 nm by Biotek plate reader.
Sensitization assay
The cells were seeded as in cytotoxicity assay and incubated with cucurbitacins for 1, 2, 4, 8, and 24 h followed by addition of serial dilutions of cisplatin (5 mM/mL NaCl) then incubated for a total of 48 h. The viability of the cells was measured by MTT. The control was cells treated with both DMSO and NaCl.
Cell cycle analysis
The cells were seeded 2.5 × 105 cells/mL in a 6-well plate (2 mL/well) and allowed to adhere overnight at 37 °C and 5 % CO2. The cells were either incubated with different concentrations of cucurbitacin B alone (0.5, 1, 2, 4, and 6 μM) for 24 h or preincubated with 2 μM cucurbitacin B for 24 h then further incubated for another 24 h with 20 μM cisplatin. The cells were washed twice with ice-cold 1× PBS and collected after trypsinzation. The cell pellet was washed two times with ice-cold 1× PBS and fixed with ice-cold 70 % ethanol overnight at −20 °C. After that, the cells were washed once with ice-cold PBS, and the second wash was done with ice-cold PBS-2 % FBS. The cell pellet was re-suspended in 500 μL propidium iodide (PI)/RNase (BD Biosciences, BDB550825) staining solution for 15 min at room temperature (RT) in the dark and analyzed within 1 h by FacsCalibur, Becton Dickinson.
Apoptosis assay
The cells were seeded at 2.5 × 105 cells/mL in a 6-well plate. The cells were either treated with 2 μM of cucurbitacin B alone for 24, 48, or 72 h, treated with 40 μM of cisplatin for 48 h or pretreated with 2 μM cucurbitacin B for 2 h then incubated for 46 h with cisplatin. The cells were collected after accutase enzyme treatment and washed two times with ice-cold 1× PBS. The cells were incubated for 2 h at 4 °C in PBS then centrifuged and re-suspended in 1× binding buffer. Five microliters of phycoerythrin (PE) annexin-V and 5 μL 7-amino-actinomycin D (7-AAD) were added to 100 μL of cell suspension and incubated for 15 min at RT in the dark; then, 400 μL of 1× binding buffer was added to the cell suspension and analyzed within 1 h by FacsCalibur, Becton Dickinson. The following controls were used to setup the machine: cells unstained with PE annexin V or 7-AAD, cells stained with PE annexin V only, and cells stained with 7-AAD only.
Caspase 3/7 detection
Caspase 3/7 activity was measured by using Caspase-Glo 3/7 assay Promega. A2780CP cells were seeded in 96-well white walled plate (5 × 104 cells/mL) and incubated overnight for attachment. The cells were treated either with DMSO/NaCl as control, 40 μM cisplatin or pretreated with 2 μM cucurbitacin B for 2 h then treated with 40 μM cisplatin. The total incubation time was 48 h. After that, 100 μL of Caspase-Glo 3/7 detection reagent were added to each well. After 1 h, the luminescence was measured by using Synergy2, Biotek. The sensitivity was adjusted to 135, and the integration time was 1 s. The luminescence values were subtracted from the no-cell values.
Nuclear fragmentation
A2780CP cells were seeded on a coverslip in 24-well plate and incubated overnight. After treatment, the cells were fixed by 3.7 % paraformaldehyde after washing with PBS. The nuclei were stained for 5 min with 4′,6-diamidino-2-phenylindole (DAPI) (0.3 μM in PBS). The stained cells were washed 5× with PBS before mounting on the glass slide by Fluoromount-G™ (Southern Biotech). The images were captured by Leica DMI 4000 B microscope at 63× magnification.
Detection of GSH/GSSG ratio
A2780CP and A2780 cells were seeded in 96-well white walled plate (5 × 104 cells/mL) and incubated overnight for attachment. The cells were treated either with DMSO/NaCl, DMSO, NaCl, cisplatin (10, 20, or 40 μM), pretreated with 2 μM cucurbitacin B for 2 h then treated with 10, 20, or 40 μM cisplatin or with cucurbitacin B alone (2 or 4 μM). The total incubation time was 48 h. The oxidized and total glutathione were measured according to the instructions of the kit (GSH/GSSG-Glo™, Promega).
Detection of ROS
A2780CP and A2780 cells were seeded in 96-well white walled plate (5 × 104 cells/mL) and incubated overnight for attachment. The cells were treated either with DMSO/NaCl, DMSO, NaCl, cisplatin (5, 10, 20, or 40 μM), pretreated with 2 μM cucurbitacin B for 1 h then treated with 5, 10, 20, or 40 μM cisplatin or with cucurbitacin B alone (1, 2, 4, or 8 μM). The total incubation time was 4 h. ROS level was detected through the measurement of H2O2 in the cells, because most of ROS converted to H2O2 and easy to be detected due to the long half-life [32], according to the instructions of the kit (ROS-Glo™ H2O2 Assay, Promega).
Generation of spheroids of cisplatin-resistant ovarian cancer cells (A2780CP)
The spheroids were generated by using GravityPLUS™ Hanging Drop Plate, 500 cells/drop/well. After 4 days, the spheroids were transferred to the GravityTRAP™ Plate for longer term maintenance. Spheroids were treated either with cisplatin (5, 10, 20, or 40 μM), pretreated with 2 μM cucurbitacin B for 2 h then treated with 5, 10, 20, or 40 μM cisplatin or with cucurbitacin B alone (2 μM). The total incubation time was 48 h. The cell viability in the 3D culture was detected by measuring level of ATP by using CellTiter-Glo® 3D Cell Viability Assay, Promega.
Western blot analysis
The cells were seeded and treated as described above then lysed by 1× RIPA buffer containing 1× protease and phosphatase inhibitor cocktail. The protein content was quantified by BCA protein assay kit. Different protein concentrations were loaded in the well of SDS-PAGE. The protein was transferred to a nitrocellulose membrane 0.2 or 0.45 μm for 45 or 90 min at 100 or 90 V, respectively. The membrane was reacted with the primary antibodies (Online resource 1 Table S1). GAPDH or β-actin was used as a loading control. The secondary antibody (Online resource 1 Table S1) was applied to the membrane and was detected either with the GE Healthcare Amersham ECL Plus Western Blotting Detection Reagents (Piscataway, NJ), and the signal was recorded by a UVP gel documentation system (UVP, Upland, CA) or by Odyssey® Imager.
Results
Cytotoxicity and sensitization screening of cucurbitacins on ovarian cancer cell lines
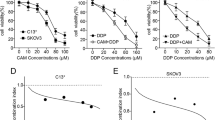
To determine the cytotoxicity of cucurbitacins on ovarian cancer cells, the cells were treated for 48 h and the viability was determined by MTT assay. Fig. 1a, b shows the cytotoxic effects of the cucurbitacins on cisplatin sensitive and resistant cell lines. Table 1 summarizes the IC50 values of each cucurbitacin and reveals cucurbitacin E as the most active compound against both cell lines. The sensitization activity of each cucurbitacin was tested by preincubating the cells for different time points with cucurbitacins, according to their respective IC50 values, followed by incubation with serial dilutions of cisplatin or treated with cisplatin alone for 48 h. It was found that a shorter preincubation with cucurbitacins and a longer incubation time with cisplatin provided a more synergetic effect (Online resource 1 Fig. S1). One hour of pretreatment followed by 47 h of incubation with cisplatin significantly increased the cytotoxicity of cisplatin toward the cisplatin-resistant ovarian cancer cell line (Fig. 1c). The tested cucurbitacins showed variable ability in the sensitization, and isocucurbitacin D showed the greatest synergetic activity. The IC50 values for cisplatin were significantly reduced due to sensitization (Table 2).
Cytotoxicity of cucurbitacins on ovarian cancer cells. a Cisplatin-sensitive (A2780) and b cisplatin-resistant (A2780CP) were incubated with cucurbitacins for 48 h, and DMSO was used as a control. The cell viability was detected by MTT assay. c Sensitization activity of cucurbitacins for the resistant ovarian cancer cells. The cells were pretreated for 1 h with the indicated concentrations of cucurbitacins (B, D, Iso D, E, and E glucoside) and incubated for 48 h total with serial dilutions of cisplatin. Sensitization of the cisplatin-resistant ovarian cancer cell line (A2780CP) by cucurbitacin B. d The cells were treated with different concentrations (μM) of cucurbitacin B for 24 h or e cells pretreated for different time points with 1 μM cucurbitacin B then treated with serial dilutions of cisplatin. The total incubation time was 48 h. The cells treated with DMSO and NaCl were considered as the control. f Cytotoxicity of cucurbitacin B alone on the cells at different time intervals
In this study, cucurbitacin B was chosen for further investigation because it is the most abundant and available cucurbitacin, and its activity toward ovarian cancer was not previously reported. According to Chou [33], one fourth and four times the IC50 value of cucurbitacin B were used in the sensitization experiment. Cucurbitacin B with different concentrations (0.5, 1, 2, 4, 6, and 8 μM) showed the same effect on the resistant ovarian cancer cells, rendering them sensitive to cisplatin toxicity (Fig. 1d). It was further investigated whether the short pretreatment of the cells with cucurbitacin B will have asimilar sensitization effect or not. Results revealed that just 1-h preincubation of cells with cucurbitacin B leads to sensitization of the resistant cells to cisplatin (Fig. 1e). The viability of the pretreated cells were determined at different time intervals after treatment with cucurbitacin B alone via MTT assay. More than 90 % of the cells were still viable after treatment with cucurbitacin B alone (Fig. 1f).
Cucurbitacin B effect on cell cycle distribution
The cells were incubated with different concentrations of cucurbitacin B for 24 h; then, the DNA content was quantified in each phase of the cell cycle. The cells treated with cucurbitacin B alone were arrested permanently at G2/M phase, even at one fourth its IC50 value (Fig. 2a). G2/M phase was increased twofold to threefold for both cell lines (Fig. 2a, c). The cell cycle arrest at G2/M phase was confirmed by detection of cyclin B1 level in the cell lysate by Western blot. The level of cyclin B1 was slightly decreased (Fig. 2b, d). The effect of combining cucurbitacin B and cisplatin on the cell cycle was investigated next. The sensitive and cisplatin-resistant cells were treated with cucurbitacin B for 24 h followed by another 24 h with cisplatin. The cells were then stained with propidium iodide after RNase treatment to quantify the DNA content. Cisplatin alone arrested a low number of cells at G2/M phase while the pretreatment of cells with 2 μM cucurbitacin B led to a significant increase of the cells that were arrested at G2/M phase (Fig. 2e, g). Following cisplatin treatment, the cyclin B1 level was increased while the pretreatment with cucurbitacin B led to a decrease in the cyclin B1 level in the cell lysate leading to G2/M arrest (Fig. 2f, h).
Cucurbitacin B treatment leads to cell cycle arrest at G2/M phase. The sensitive ovarian cancer cells A2780 (a) or A2780CP (c) were treated with the indicated concentrations of cucurbitacin B for 24 h. Then, the DNA content was quantified by propidium iodide and analyzed within 1 h by FACSCalibur. c and d shows the slight decrease in the cyclin B1 level in cisplatin sensitive and resistant, respectively, treated cells with the indicated concentrations (μM). The pretreatment of the ovarian cancer cells with cucurbitacin B increased the level of the arrested cells in G2/M phase. e A2780 and g A2780CP cells were incubated either with 20 μM cisplatin for 24 h or pretreated with 2 μM cucurbitacin B for 24 h followed by 24 h with 20 μM of cisplatin. f and h Cyclin B 1 level after either treatment with 20 μM cisplatin for 48 h or pretreatment for 24 h with 2 μM cucurbitacin B then another 48 h with 20 μM cisplatin
Increasing rate of apoptosis by cucurbitacin B
The detection of apoptosis and discrimination between the viable and nonviable cells were done using 7-AAD and PE annexin-V. The treatment of cisplatin-resistant ovarian cancer cell line (A2780CP) with 2 μM cucurbitacin B for different times led to the induction of apoptosis (Fig. 3a), and the percentage of the cells that stained with 7-AAD and PE annexin-V was increased with increasing the time of incubation, from 1.38 to 34.17 % after 72-h treatment (Fig. 3e). Immunofluorescence staining for the nucleus by DAPI showed the morphological pattern of the apoptotic cells, cell shrinkage, chromatin condensation, and nuclear fragmentation (Fig. 3f).
Effect of cucurbitacin treatment on the induction of apoptosis. a The cisplatin-resistant ovarian cancer cells (A2780CP) treated with DMSO. b Cells treated with 2 μM cucurbitacin B for 24 h. c Cells treated for 48 h. d Cells treated for 72 h. e Cells detached after treatment with accutase enzyme and washing two times with PBS then stained with 7-AAD and PE annexin-V and analyzed by FACSCalibur within 1 h. The data represented as mean values ± standard deviation (n = 3). f Immunofluorescence staining for the apoptotic cells by DAPI after DMSO or g 2 μM cucurbitacin B treatment. h Effect of cucurbitacin B treatment on the expression level of proapoptotic and antiapoptotic proteins. The cells were treated with different concentrations of cucurbitacin B (μM) for 48 h. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as a loading control. NFκB nuclear factor kappa B, NFκB-NE buclear factor kappa B-nuclear extract, PARP poly ADP ribose polymerase, Bcl-2 B cell lymphoma 2, BAX Bcl-2-associated X protein, Apaf-1 apoptotic protease activating factor 1
Synergetic effect on apoptotic induction by cisplatin
Apoptosis rate was detected after treatment with cisplatin alone or with combined treatment of cucurbitacin B and cisplatin. Detection of the viability of the cells by MTT showed that the 2-h pretreatment with cucurbitacin B followed by cisplatin for 46 h sensitizes the cells to the cytotoxicity of the cisplatin. Therefore, the apoptotic induction was detected in these models of cell treatment. As shown in Fig. 4a, b, 2-h treatment of the cells with 2 μM cucurbitacin B and incubation for another 46 h with cisplatin increased the number of apoptotic cells. The same significant increase was found when the cells were treated for 24 h with 2 μM cucurbitacin B and another 24 h with 40 μM cisplatin (Fig. 4c, d). The increase in apoptotic rate was confirmed by immunostaining of the nuclei with DAPI. The cisplatin-treated cells showed a lower number of apoptotic cells (Fig. 4g) while the pretreatment for 2 h led to a significant increase in this number (Fig. 4h). Further confirmation of the synergetic effect of cucurbitacin B toward cisplatin cytotoxicity was shown by measuring the level of activated caspases 3 and 7 using aluminance assay. As seen in Fig. 4e, the pretreatment of cells led to a significant increase in the activated caspases 3 and 7. The cleaved caspases 3 were detected by Western blotting for the lysate, and the results of cucurbitacin B treatment showed an increase in the cleaved caspases 3 in a dose-dependent manner (Fig. 3h). Pretreatment of the cells with cucurbitacin B followed by cisplatin led to an increase in the procaspase 3 and the corresponding cleaved fragment in comparison to the treatment with cisplatin alone (Fig. 4i, Online resource 1 Fig. S2).
Effect of short pretreatment of the cisplatin-resistant ovarian cancer cells with cucurbitacin B. a A2780CP cells were treated for 48 h with 40 μM cisplatin. b Cells treated for 2 h with 2 μM cucurbitacin B and 46 h with 40 μM cisplatin. c Cells treated for 24 h with 40 μM cisplatin. d Cells treated for 24 h with 2 μM cucurbitacin B and 24 h with 40 μM cisplatin. e The level of cleaved caspases 3/7 in cells treated either with 40 μM cisplatin or pretreated with 2 μM cucurbitacin B for 2 h then with 40 μM cisplatin for 46 h. The data represented as mean values ± standard deviation (n = 3). f, g, h Immunofluorescence staining for the apoptotic cells, g cells treated either with 40 μM cisplatin, or h pretreated with 2 μM cucurbitacin B for 2 h then with 40 μM cisplatin for 46 h; arrow indicates the damage to nuclei. i Sensitization effect of cucurbitacin B on the expression level of proapoptotic and antiapoptotic proteins. The resistant ovarian cancer cells (A2780CP) were treated with the indicated concentrations of cisplatin (μM) or pretreated with (2 μM) cucurbitacin B for 24 h followed by 48 h with cisplatin (10 or 20 μM). NFκB-TE nuclear factor kappa B in total protein extract, NFκB-NE nuclear factor kappa B-nuclear extract, PARP poly ADP ribose polymerase, Bcl-2 B cell lymphoma 2, BAX Bcl-2-associated X protein, Apaf-1 apoptotic protease activating factor 1. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as a loading control
Mechanism of cytotoxic and synergetic effect of cucurbitacin B
NFκB regulates and inhibits apoptosis through the overexpression of antiapoptotic proteins such as Bcl-2 [8]. The level of NFκB p65 either in the total lysate or in the nuclear extract was detected after cell treatment with indicated concentrations of cucurbitacin B. As seen in Fig. 3h, the level of NFκB p65 was increased in a concentration-dependent manner; then, at 8 μM, the level was decreased in the resistant cells while the sensitive one showed a decreased in the level at 0.5 μM cucurbitacin B (Online resource 1 Fig. S2). The effect of cucurbitacin B treatment on the translocation of NFκB p65 subunit into the nucleus was detected. We found that the level was decreased after cucurbitacin B treatment of both cell lines (Fig. 3h and Online resource 1 Fig. S2). In comparison to the single-drug treatment, the NFκB p65 subunit was absent in the combination treatment in both total lysate and the nuclear extract of sensitive and resistant cells (Fig. 4i, Online resource 1 Fig. S3).
The inhibition of NFκB p65 activity was confirmed by the detection of antiapoptotic Bcl-2 protein. The cells were treated with the indicated concentrations of cucurbitacin B, and the results showed a decrease in the level at higher concentrations (Fig. 3h). Bcl-2 level was significantly reduced in the sensitized cells by cucurbitacin B for 24 h (Fig. 4i). Bcl-2 inhibits Bcl-2-associated X protein (BAX) which regulates the mitochondrial outer membrane permeabilization which accordingly controls the activation of apoptotic caspases [34]. Therefore, the level of BAX was determined after single or combined drug treatment. Fig. 3h shows that BAX level was increased after cucurbitacin B treatment for 48 h and greatly increased in the cells treated with both cucurbitacin B and cisplatin (Fig. 4i). Proteolytic cleavage of poly (ADP)-ribose polymerase 1 (PARP-1) by caspases 3 and 7 is a hallmark of apoptosis. Cucurbitacin B led to an increase in the cleaved PARP-1 in both cell lines (Fig. 3h, Online resource 1 Fig. S2) while the treatment with both cucurbitacin B and cisplatin significantly increased the cleaved fragment along with complete disappearance of the full-length PARP (Fig. 4i, Online resource 1 Fig. S3).
Tan and his researchers [35] showed that the endogenous expression level of apoptotic protease activating factor 1 (Apaf-1) in ovarian cancer tumor is not predictive to the cisplatin response. Even when Apaf-1 level was higher in the tumor, it did not respond to the treatment indicating a dysfunction in Apaf-1. For this reason, we propped the lysate after 48-h treatment for Apaf-1 to detect its level, the cucurbitacin B treatment led to a nonsignificant increase in Apaf-1 in sensitive and resistant ovarian cancer cells and a complete disappearance of Apaf-1 at the higher concentration suggesting early formation of apoptosome before 48 h (Fig. 3h, Online resource 1 Fig. S2), so the level of Apaf-1 was detected at different time points of incubation with cucurbitacin B (Online resource 1 Fig. S4a). The expression level was increased at earlier times of incubation then began to decrease suggesting that the Apaf-1 was degraded after a certain time point. In agreement with this phenomena is that the sensitized cells by cucurbitacin B showed a complete disappearance of Apaf-1 and an increase in the cleaved caspases 9 (Fig. 4i, Online resource 1 Fig. S3) which were cleaved by apoptosome before the degradation of Apaf-1. To confirm that the apoptosome could be formed at early time of incubation, the cytochrome c was detected in the cytoplasmic extract of resistant cells after treatment with cisplatin alone for different time points or after pretreatment with 2 μM cucurbitacin B for 2 h followed by cisplatin treatment at the same time points. Cytochrome c release in the cytoplasm was higher in the cells that were pretreated with cucurbitacin B, followed by cisplatin for 1 h. The cytochrome c level decreased with a longer time of incubation, and then, at 24 h, the level increased greatly in the sensitized cells pretreated with cucurbitacin B (Online resource 1 Fig. S4b). Cucurbitacin B in a single treatment induced the release of cytochrome c in the cytosol at 8 μM after 48 h (Online resource 1 Fig. S4c); then, the level decreased at 40 μM.
Since the glutathione level in the cells contributes greatly on the resistance through the inactivation of cisplatin and a major indicator for oxidative stress, its level was detected. It was found that the level of total glutathione was highly reduced in cucurbitacin B-treated cells and in the combination-treated cells (Online resource 1 Fig. S5). It is known that cisplatin kills the cells by increasing the level of ROS, so we detected ROS level and the level of Dyrk1B after exposure to cisplatin alone or in combination with cucurbitacin B. Cucurbitacin B or cisplatin alone slightly increased ROS level, but significantly, ROS production was increased in combination treatment (Fig. 5a). The level of Dyrk1B increased in a dose-dependent manner up to 8 μM of cucurbitacin B; then, the level decreased (Fig. 5b, c). The cells treated with cisplatin alone increased the level of Dyrk1B while the level in the cells that were pretreated with cucurbitacin B then cisplatin was decreased in comparison to the single treatment with cisplatin (Fig. 5d, e).
An increase in ROS production and downregulation of dual-specificity tyrosine-regulated kinase (Dyrk1B) after cucurbitacin B and the combination treatments. a The resistant cells were either treated with cucurbitacin B (2 μM), cisplatin (20 μM), or cucurbitacin B plus cisplatin (2 + 20) for 48 h. ROS level was detected by ROS-Glo™ H2O2 Assay, Promega. The data represented as mean values ± standard deviation (n = 3). b The sensitive and c resistant ovarian cancer cells were treated with the indicated concentrations of cucurbitacin B (μM) for 48 h. d Sensitive or e resistant cells either treated with cisplatin for 48 h or pretreated with 2 μM cucurbitacin B for 24 h followed by 48-h treatment with cisplatin. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as a loading control
Cucurbitacin B leads to an alteration in the signaling pathways
The level of pSTAT-3 was detected after cucurbitacin B or the combination drug treatment. Cucurbitacin B showed an effect on the two isoforms of STAT-3 beta and gamma. It was found that the phosphorylation level of beta and gamma isoforms was decreased in a dose-dependent manner in the sensitive cells (Fig. 6a). In contrast to the sensitive cells, cucurbitacin B showed only effect at 40 μM and reduced total STAT-3 (Fig. 6c). The combined drug treatment leads to a decrease in pSTAT-3 isoforms in A2780 cell line (Fig. 6b) and a decrease in the resistant cells (Fig. 6d). Moreover, the level of ERK and its phosphorylated form was detected. Cucurbitacin B leads to an increase in the phosphorylated ERK1/2 in a dose-dependent manner in both cell lines (Fig. 6a, c). In contrast to the single treatment, cucurbitacin B combined with cisplatin leads to the complete depletion of pERK1/2 (Fig. 6b, d).
Changes in the expression level of signaling proteins by cucurbitacin B. a The cisplatin-sensitive (A2780) and b cisplatin-resistant ovarian cancer cells (A2780CP) were treated with the indicated concentrations of cucurbitacin B (μM) for 48 h. c A2780 or d A2780CP cells either treated with 20 μM cisplatin for 48 h or pretreated with 2 μM cucurbitacin B for 24 h followed by 48-h treatment with 20 μM cisplatin. GAPDH was used as a loading control. pSTAT-3 phosphorylated signal transducer and activator of transcription 3, STAT-3 signal transducer and activator of transcription 3, pERK phosphorylated extracellular-signal-regulated kinase, ERK extracellular-signal-regulated kinase, GADPH glyceraldehyde-3-phosphate dehydrogenase
Cucurbitacin B sensitized the spheroids to cytotoxicity of cisplatin
We further investigated the effectiveness of cucurbitacin B as a sensitizer for spheroids generated from the cisplatin-resistant ovarian cancer cells. The spheroids were either treated with cucurbitacin B, cisplatin alone or sensitized for 2 h with cucurbitacin B and incubated for another 46 h with cisplatin. The viability of the spheroids was measured via detection of ATP level. Cucurbitacin B alone was able to reduce the amount of ATP which is an indicator for viability at 8 μM (Fig. 7a). ATP content was reduced after cisplatin treatment, but the pretreatment of the spheroids just for 2 h significantly reduced the viability of the spheroid (Fig. 7b). The morphology of the spheroids was monitored, and it was found that the untreated and cisplatin-treated spheroids showed a compact and cohesive morphology while cucurbitacin B-treated spheroids were less compact. In comparison to the single treatment, the spheroids were completely disaggregated after the combined treatment with cucurbitacin B and cisplatin (Fig. 7c, Online resource 1 Fig. 6). The interesting finding on the morphology was also observed even with one eighth IC50 of cisplatin in this study (Online resource 1 Fig. S6).
Effectiveness of cucurbitacin B as chemosensitizer against ovarian cancer spheroids. Spheroids were generated from cisplatin-resistant ovarian cancer cells using GravityPLUS™ Hanging Drop Plates. After 4 days, the spheroids either a, c treated with the indicated concentrations of cucurbitacin B for 48 h, b, c cisplatin (μM), or pretreated with 2 μM cucurbitacin B for 2 h followed by 20 μM cisplatin treatment for 48 h. The viability was detected by measurement of ATP content in the spheroid. The data represented as mean values ± standard deviation (n = 3)
Discussion
Ovarian cancer is the most deadly gynecological disease in patients suffering from recurrent cancer. Cisplatin and carboplatin are the most effective platinum-based drugs for ovarian cancer treatment. Most solid tumors, such as ovarian cancer, possess high levels of survival proteins that are responsible for decreasing the response to common chemotherapeutic drugs. Single-drug targeted therapy achieves less than 10 % recovery from recurrent ovarian cancer [18]. In the present study, cucurbitacin B alone showed an inhibitory effect on both cisplatin-sensitive and cisplatin-resistant ovarian cancer cell lines. Moreover, the combination of 2 μM cucurbitacin B with 5 μM cisplatin leads to a significant increase in the cytotoxicity of cisplatin toward the cisplatin sensitive and resistant cells. These combination of drugs was effective on killing the spheroids generated from resistant cells. Cucurbitacin B activity against ovarian cancer was through cell cycle arrest at G2/M phase, an increase in the apoptosis rate through the alteration in the signaling pathways such as STAT-3 and ERK1/2, inhibition of NFκB activity, decrease in the total glutathione, increase in ROS, and decrease in Dyrk1B level in the cells.
Accumulation of cyclin B1 is required for the transition from G2 to mitosis through activation of the cyclin-dependent kinase (Cdk1) leading to the phosphorylation of different substrates required for cells to move to the mitosis state [36]. It has been found that cyclin B1 is overexpressed in low-malignant ovarian cancer [37]. The activation and translocation of NFκB p65 after cisplatin treatment leads to the expression of different survival proteins such as Bcl-2, Bcl-xl, inhibitors of apoptosis (IAPs) [38] which, in turn, increases the resistance of the tumor to the treatment [39]. Annunziata et al. showed that overexpression of NFκB subunits leads to a poor prognosis in the patients [40]. Thus, the combination of natural products that may have NFκB inhibitor activity with the common chemotherapeutic drugs such as cisplatin is a practical approach for addressing these undesired cellular responses. Cucurbitacin B showed an inhibitory effect on NFκB activity by inhibiting its translocation into the nucleus leading to a decrease in Bcl-2 and an increase in BAX. However, it was found that cucurbitacin B did not affect the nuclear translocation induced by TNF-α in Hela cells, [41] rather it inhibited NFκB transcription activity through inhibiting RelA/p65 transactivation activity[41].
Cucurbitacin B cytotoxicity against other cancer cells is dependent or independent on the inhibition of STAT-3 phosphorylation [42–45], suggesting that the cytotoxicity may be through another mechanism. In squamous cancer carcinoma, cucurbitacin B sensitized the cells to cisplatin through the inhibition of STAT-3 phosphorylation [45]. In the present research, cucurbitacin B inhibited the phosphorylation of STAT-3 either in the single form or in combination with cisplatin leading to a decrease in Bcl-2 protein, whose expression is controlled by STAT-3 activation.
Caspase 3 cleaves 1 16 KDa PARP-1 into 85 and 24 KDa PARP-1 which are required for DNA repair [46]. It senses the single DNA strand damage and binds to DNA leading to the recruitment of proteins required for base excision repair [47]. Overexpression of PARP-1 was correlated to the poor prognosis and survival of ovarian cancer patients due to an increase in the DNA-damage repair system [48]. Godoy et al. showed that PARP-1 was overexpressed in about 61 % of the cases that were studied [49]. Inhibition of PARP-1 is proposed in increasing the sensitivity to DNA-damaging drugs such as cisplatin [50]. Cucurbitacin B induced the cleavage of caspase 9 which activates caspase 3 leading to inhibition of PARP-1 either in the single form or in combination with cisplatin.
The effect of cucurbitacin B on the mitogen-activated protein kinase (MAPK)/ERK1/2 pathway was different for single treatment compared to its use in combination with cisplatin. Cucurbitacin B alone led to an increase in the pERK1/2 level in the cisplatin sensitive and resistant ovarian cancer cells. It has been reported before that ERK1/2 might have proapoptotic or prosurvival signals [14]. There are even contradicting reports of the effects cucurbitacin B has on the phosphorylation state of ERK1/2. In the present report, cucurbitacin B showed induction of the phosphorylation of ERK1/2 followed by cell death. Opposite to single treatment, pretreatment of the cisplatin sensitive and resistant ovarian cancer cells with cucurbitacin B followed by cisplatin showed an inhibitory effect on the phosphorylation of ERK1/2 leading to the induction of apoptosis. These results show the dual effect of cucurbitacin B on the MAPK/ERK1/2 signaling pathway.
Impairment of STAT3 phosphorylation was the same in either single cucurbitacin B treatment or in combination with cisplatin, leading to an increase in the growth inhibitory effect of cisplatin. Previously, cucurbitacin B exhibited the same phenomena on squamous cell carcinoma cells leading to the sensitization of cells to cisplatin cytotoxicity [45]. One of the mechanisms for the inactivation of cisplatin in tumor cells is the presence of high levels of reduced glutathione [51, 52]. Moreover, it was found that the prolonged depletion of glutathione by buthionine sulfoximine leads to a potentiation in cisplatin cytotoxicity [53]. In nonsmall-cell lung cancer, cucurbitacin B decreased the level of thiol content in the cells [54], and in the present study, cucurbitacin B decreased the level of total glutathione in both single treatment and in combination with cisplatin. As a result, inhibition of the glutathione content in the cisplatin-resistant ovarian cancer cells by cucurbitacin B led to an increase in the activity of cisplatin. Silencing of Dyrk1B in ovarian cancer cells sensitized the cells to cisplatin through an increase in ROS and decrease in the amount of antioxidant enzymes [19]. Cucurbitacin B treatment showed an increase then decrease in the level of Dyrk1B at higher concentration. Cisplatin treatment leads to an increase in Dyrk1B as a resistant response from the cells, but the pretreatment with cucurbitacin B inhibited the increase in Dyrk1B expression. The decrease in Dyrk1B level was confirmed by measuring the level of ROS produced in the treated cells. Cucurbitacin B alone showed an increase in ROS production at 4 μM. Cisplatin induced ROS production, and this production was highly increased in the cells pretreated with cucurbitacin B for 1 h.
Cucurbitacin B showed cytotoxic effect on the ovarian cancer cell lines in the 2D culture model and sensitized the cells toward the cytotoxicity of cisplatin. Studies showed that 3D tissue culture system resemble the pathophysiological situation as tumor in human [28] because the gene expression in the spheroids is identical to the tumor. Ovarian cancer spreads because of the tumor cells shed from the surface of the ovary into peritoneal cavity. Once they attach to the mesothelial layer, they can induce the formation of tumor at distant site [55]. Unattached tumor cells in the ascites form spheroids. These spheroids are resistant to chemotherapy and radiotherapy [56–59]. The cohesive morphology of the tumor leads to a low rate of penetration of drugs, high tolerance to the DNA-damaged effect, overexpression of DNA repair proteins [56]. There are different ways to initiate the formation of spheroids in vitro and using them as a model in drug discovery and elucidating the mechanisms of resistance [60–62]. In this work, the efficacy of cucurbitacin B, cisplatin, or treatment of spheroids with both drugs was tested. The integrity of spheroids after cucurbitacin B was changed and was less compact than the control spheroids. Cisplatin-treated spheroids were compact and cohesive. Both drugs together completely disaggregated the spheroid architecture and reduced the level of ATP content in the spheroid. The outcomes of this study may help in proposing a valuable piece of information which may open a new horizon for diagnosis and chemotherapeutic management of highly resistant ovarian cancer patients.
Conclusion
This work highlights the cytotoxicity of cucurbitacin B on cisplatin sensitive and resistant ovarian cancer cells and the mechanism behind this effect. Moreover, cucurbitacin B sensitized efficiently the resistant cells and the spheroids toward the cytotoxicity of cisplatin through an increase in apoptotic rate, by altering STAT-3 and ERK1/2 signaling pathways, changing redox state of the cells, and increasing ROS production via inhibition of Dyrk1B expression. To the knowledge of the authors, this is the first report showing effect of cucurbitacin B on spheroid morphology, and Dyrk1B as a new target for cucurbitacin B and its effect on its kinase activity are worth further investigation. The results from this study may provide a combination therapy to ovarian cancer in patients suffering from recurrence of tumor after initial cisplatin treatment.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59(4):225–49. doi:10.3322/caac.20006.
Iwanicki MP, Davidowitz RA, Ng MR, Besser A, Muranen T, Merritt M, et al. Ovarian cancer spheroids use myosin-generated force to clear the mesothelium. Cancer Discov. 2011;1(2):144–57. doi:10.1158/2159-8274.cd-11-0010.
Nederman T, Acker H, Carlsson J. Penetration of substances into tumor tissue: a methodological study with microelectrodes and cellular spheroids. In Vitro. 1983;19(6):479–88.
Rebucci M, Michiels C. Molecular aspects of cancer cell resistance to chemotherapy. Biochem Pharmacol. 2013;85(9):1219–26. doi:10.1016/j.bcp.2013.02.017.
Stewart DJ. Mechanisms of resistance to cisplatin and carboplatin. Crit Rev Oncol Hematol. 2007;63(1):12–31. doi:10.1016/j.critrevonc.2007.02.001.
Mercurio F, Manning AM. Multiple signals converging on NF-kappaB. Curr Opin Cell Biol. 1999;11(2):226–32.
Karin M, Lin A. NF-kappaB at the crossroads of life and death. Nat Immunol. 2002;3(3):221–7. doi:10.1038/ni0302-221.
Hua Y, Jove R. The STATs of cancer—new molecular targets come of age. Nat Rev Cancer. 2004;4(2):97–105. doi:10.1038/nrc1275.
Meinhold-Heerlein I, Bauerschlag D, Hilpert F, Dimitrov P, Sapinoso LM, Orlowska-Volk M, et al. Molecular and prognostic distinction between serous ovarian carcinomas of varying grade and malignant potential. Oncogene. 2005;24(6):1053–65. doi:10.1038/sj.onc.1208298.
Duan Z, Foster R, Bell DA, Mahoney J, Wolak K, Vaidya A, et al. Signal transducers and activators of transcription 3 pathway activation in drug-resistant ovarian cancer. Clin Cancer Res. 2006;12(17):5055–63. doi:10.1158/1078-0432.ccr-06-0861.
Han Z, Feng J, Hong Z, Chen L, Li W, Liao S, et al. Silencing of the STAT3 signaling pathway reverses the inherent and induced chemoresistance of human ovarian cancer cells. Biochem Biophys Res Commun. 2013;435(2):188–94. doi:10.1016/j.bbrc.2013.04.087.
Platanias LC. Map kinase signaling pathways and hematologic malignancies. Blood. 2003;101(12):4667–79. doi:10.1182/blood-2002-12-3647.
Lu Z, Xu S. ERK1/2 MAP kinases in cell survival and apoptosis. IUBMB Life. 2006;58(11):621–31. doi:10.1080/15216540600957438.
Kim KY, Choi KC, Park SH, Auersperg N, Leung PC. Extracellular signal-regulated protein kinase, but not c-Jun N-terminal kinase, is activated by type II gonadotropin-releasing hormone involved in the inhibition of ovarian cancer cell proliferation. J Clin Endocrinol Metab. 2005;90(3):1670–7. doi:10.1210/jc.2004-1636.
Hayakawa J, Ohmichi M, Kurachi H, Ikegami H, Kimura A, Matsuoka T, et al. Inhibition of extracellular signal-regulated protein kinase or c-Jun N-terminal protein kinase cascade, differentially activated by cisplatin, sensitizes human ovarian cancer cell line. J Biol Chem. 1999;274(44):31648–54.
Wulfkuhle JD, Aquino JA, Calvert VS, Fishman DA, Coukos G, Liotta LA, et al. Signal pathway profiling of ovarian cancer from human tissue specimens using reverse-phase protein microarrays. Proteomics. 2003;3(11):2085–90. doi:10.1002/pmic.200300591.
Bast Jr RC. Molecular approaches to personalizing management of ovarian cancer. Ann Oncol. 2011;22 Suppl 8:viii5–viii15. doi:10.1093/annonc/mdr516.
Hu J, Friedman E. Depleting mirk kinase increases cisplatin toxicity in ovarian cancer cells. Genes Cancer. 2010;1(8):803–11. doi:10.1177/1947601910377644.
Lai GM, Ozols RF, Young RC, Hamilton TC. Effect of glutathione on DNA repair in cisplatin-resistant human ovarian cancer cell lines. J Natl Cancer Inst. 1989;81(7):535–9.
Hockenbery DM, Oltvai ZN, Yin XM, Milliman CL, Korsmeyer SJ. Bcl-2 functions in an antioxidant pathway to prevent apoptosis. Cell. 1993;75(2):241–51.
Chen X, Bao J, Guo J, Ding Q, Lu J, Huang M, et al. Biological activities and potential molecular targets of cucurbitacins: a focus on cancer. Anticancer Drugs. 2012;23(8):777–87. doi:10.1097/CAD.0b013e3283541384.
Alghasham AA. Cucurbitacins - a promising target for cancer therapy. Int J Health Sci. 2013;7(1):77–89.
Chen JC, Chiu MH, Nie RL, Cordell GA, Qiu SX. Cucurbitacins and cucurbitane glycosides: structures and biological activities. Nat Prod Rep. 2005;22(3):386–99. doi:10.1039/b418841c.
Chen W, Leiter A, Yin D, Meiring M, Louw VJ, Koeffler HP. Cucurbitacin B inhibits growth, arrests the cell cycle, and potentiates antiproliferative efficacy of cisplatin in cutaneous squamous cell carcinoma cell lines. Int J Oncol. 2010;37(3):737–43.
Iwanski GB, Lee DH, En-Gal S, Doan NB, Castor B, Vogt M, et al. Cucurbitacin B, a novel in vivo potentiator of gemcitabine with low toxicity in the treatment of pancreatic cancer. Br J Pharmacol. 2010;160(4):998–1007. doi:10.1111/j.1476-5381.2010.00741.x.
Lee DH, Thoennissen NH, Goff C, Iwanski GB, Forscher C, Doan NB, et al. Synergistic effect of low-dose cucurbitacin B and low-dose methotrexate for treatment of human osteosarcoma. Cancer Lett. 2011;306(2):161–70. doi:10.1016/j.canlet.2011.03.001.
Friedrich J, Seidel C, Ebner R, Kunz-Schughart LA. Spheroid-based drug screen: considerations and practical approach. Nat Protoc. 2009;4(3):309–24. doi:10.1038/nprot.2008.226.
Tung YC, Hsiao AY, Allen SG, Torisawa YS, Ho M, Takayama S. High-throughput 3D spheroid culture and drug testing using a 384 hanging drop array. Analyst. 2011;136(3):473–8. doi:10.1039/c0an00609b.
Hamaguchi K, Godwin AK, Yakushiji M, O'Dwyer PJ, Ozols RF, Hamilton TC. Cross-resistance to diverse drugs is associated with primary cisplatin resistance in ovarian cancer cell lines. Cancer Res. 1993;53(21):5225–32.
Bartalis J, Halaweish FT. In vitro and QSAR studies of cucurbitacins on HepG2 and HSC-T6 liver cell lines. Bioorg Med Chem. 2011;19(8):2757–66. doi:10.1016/j.bmc.2011.01.037.
Alfadda AA, Sallam RM. Reactive oxygen species in health and disease. J Biomed Biotechnol. 2012;2012:936486. doi:10.1155/2012/936486.
Chou TC, Martin N. CompuSyn for drug combinations: PC software and user’s guide: a computer program for quantitation of synergism and antagonism in drug combinations, and the determination of IC50 and ED50 and LD50 Values, ComboSyn Inc, Paramus, (NJ), 2005.
Tait SWG, Green DR. Mitochondria and cell death: outer membrane permeabilization and beyond. Nat Rev Mol Cell Biol. 2010;11(9):621–32. doi:10.1038/nrm2952.
Tan L, Kwok RP, Shukla A, Kshirsagar M, Zhao L, Opipari Jr AW, et al. Trichostatin A restores Apaf-1 function in chemoresistant ovarian cancer cells. Cancer. 2011;117(4):784–94. doi:10.1002/cncr.25649.
Shen M, Feng Y, Gao C, Tao D, Hu J, Reed E, et al. Detection of Cyclin B1 Expression in G1-phase cancer cell lines and cancer tissues by postsorting western blot analysis. Cancer Res. 2004;64(5):1607–10. doi:10.1158/0008-5472.can-03-3321.
Zheng H, Hu W, Deavers MT, Shen D-Y, Fu S, Li Y-F, et al. Nuclear cyclin B1 is overexpressed in low-malignant-potential ovarian tumors but not in epithelial ovarian cancer. Am J Obstet Gynecol. 2009;201(4):367.e1-.e6. doi:10.1016/j.ajog.2009.05.021.
Pahl HL. Activators and target genes of Rel/NF-kappaB transcription factors. Oncogene. 1999;18(49):6853–66. doi:10.1038/sj.onc.1203239.
Wang CY, Cusack Jr JC, Liu R, Baldwin Jr AS. Control of inducible chemoresistance: enhanced anti-tumor therapy through increased apoptosis by inhibition of NF-kappaB. Nat Med. 1999;5(4):412–7. doi:10.1038/7410.
Annunziata CM, Stavnes HT, Kleinberg L, Berner A, Hernandez LF, Birrer MJ, et al. Nuclear factor kappaB transcription factors are coexpressed and convey a poor outcome in ovarian cancer. Cancer. 2010;116(13):3276–84. doi:10.1002/cncr.25190.
Jin HR, Jin X, Dat NT, Lee JJ. Cucurbitacin B suppresses the transactivation activity of RelA/p65. J Cell Biochem. 2011;112(6):1643–50. doi:10.1002/jcb.23078.
Chan KT, Li K, Liu SL, Chu KH, Toh M, Xie WD. Cucurbitacin B inhibits STAT3 and the Raf/MEK/ERK pathway in leukemia cell line K562. Cancer Lett. 2010;289(1):46–52. doi:10.1016/j.canlet.2009.07.015.
Chan KT, Meng FY, Li Q, Ho CY, Lam TS, To Y, et al. Cucurbitacin B induces apoptosis and S phase cell cycle arrest in BEL-7402 human hepatocellular carcinoma cells and is effective via oral administration. Cancer Lett. 2010;294(1):118–24. doi:10.1016/j.canlet.2010.01.029.
Duangmano S, Sae-Lim P, Suksamrarn A, Patmasiriwat P, Domann FE. Cucurbitacin B causes increased radiation sensitivity of human breast cancer Cells via G2/M Cell Cycle Arrest. J Oncol. 2012;2012:601682. doi:10.1155/2012/601682.
Liu T, Peng H, Zhang M, Deng Y, Wu Z. Cucurbitacin B, a small molecule inhibitor of the Stat3 signaling pathway, enhances the chemosensitivity of laryngeal squamous cell carcinoma cells to cisplatin. Eur J Pharmacol. 2010;641(1):15–22. doi:10.1016/j.ejphar.2010.04.062.
Kaufmann SH, Desnoyers S, Ottaviano Y, Davidson NE, Poirier GG. Specific Proteolytic Cleavage of Poly(ADP-ribose) Polymerase: an early marker of chemotherapy-induced apoptosis. Cancer Res. 1993;53(17):3976–85.
Dantzer F, de la Rubia G, Ménissier-de Murcia J, Hostomsky Z, de Murcia G, Schreiber V. Base excision repair is impaired in mammalian cells lacking poly(adp-ribose) polymerase-1†. Biochemistry. 2000;39(25):7559–69. doi:10.1021/bi0003442.
Bowman KJ, Newell DR, Calvert AH, Curtin NJ. Differential effects of the poly (ADP-ribose) polymerase (PARP) inhibitor NU1025 on topoisomerase I and II inhibitor cytotoxicity in L1210 cells in vitro. Br J Cancer. 2001;84(1):106.
Godoy H, Mhawech-Fauceglia P, Beck A, Miller A, Lele S, Odunsi K. Expression of poly (adenosine diphosphate-ribose) polymerase and p53 in epithelial ovarian cancer and their role in prognosis and disease outcome. Int J Gynecol Pathol: Off J Int Soc Gynecol Pathol. 2011;30(2):139–44. doi:10.1097/PGP.0b013e3181fa5a64.
Michels J, Vitale I, Galluzzi L, Adam J, Olaussen KA, Kepp O, et al. Cisplatin resistance associated with PARP hyperactivation. Cancer Res. 2013;73(7):2271–80. doi:10.1158/0008-5472.CAN-12-3000.
Godwin AK, Meister A, O'Dwyer PJ, Huang CS, Hamilton TC, Anderson ME. High resistance to cisplatin in human ovarian cancer cell lines is associated with marked increase of glutathione synthesis. Proc Natl Acad Sci U S A. 1992;89(7):3070–4.
Gamcsik MP, Kasibhatla MS, Teeter SD, Colvin OM. Glutathione levels in human tumors. Biomarkers. 2012;17(8):671–91. doi:10.3109/1354750X.2012.715672.
Andrews PA, Schiefer MA, Murphy MP, Howell SB. Enhanced potentiation of cisplatin cytotoxicity in human ovarian carcinoma cells by prolonged glutathione depletion. Chem Biol Interact. 1988;65(1):51–8.
Kausar H, Munagala R, Bansal SS, Aqil F, Vadhanam MV, Gupta RC. Cucurbitacin B potently suppresses non-small-cell lung cancer growth: identification of intracellular thiols as critical targets. Cancer Lett. 2013;332(1):35–45. doi:10.1016/j.canlet.2013.01.008.
Burleson K, Hansen L, Skubitz A. Ovarian carcinoma spheroids disseminate on type I collagen and invade live human mesothelial cell monolayers. Clin Exp Metastasis. 2005;21:685-697.
Durand R, Sutherland R. Effects of intercellular contact on repair of radiation damage. Exp Cell Res. 1972;71:75–80.
Filipovich I, Sorokina N, Robillard N, Chatal J. Radiation-induced apoptosis in human ovarian carcinoma cells growing as a monolayer and as multicell spheroids. Int J Cancer. 1997;72:851–9.
Graham C, Kobayashi H, Stankiewicz K, Man S, Kapitain S, Kerbel R. Rapid acquisition of multicellular drug resistance after a single exposure of mammary tumor cells to antitumor alkylating agents. J Natl Cancer Inst. 1994;86:975–82.
Makhija S, Taylor D, Gibb R, Gercel-Taylor. Taxol-induced Bcl-2 phosphorylation in ovarian cancer cell monolayer and spheroids. Int J Oncol. 1999;14:515–21.
Bardies M, Thedrez P, Gestin J, Marcille B, Guerreau D, Faivre-Chauvet A, et al. Use of multi-cell spheroids of ovarian carcinoma as an intraperitoneal radio-immunotherapy model: uptake, retention kinetics and dosimetric evaluation. Int J Cancer. 1992;50:984–91.
Sutherland R, MacDonald H, Howell R. Multicellular spheroids: a new model target for in vitro studies of immunity to solid tumor allografts. J Natl Cancer Inst. 1977;58:1849–53.
Sutherland R, McCredie J, Inch W. Growth of multicell spheroids in tissue culture as a model of nodular carcinoma. J Natl Cancer Inst. 1971;46:113–20.
Acknowledgments
We would like to thank Lucas Kopel and Mahmoud Salama (Chemistry and Biochemistry Department, South Dakota State University, Brookings, SD, USA). This work was supported by the Egyptian government via the Egyptian Ministry of Higher Education and Scientific Research.
Conflict of interest
None
Authors’ contributions
FE helped in the design of the study, carried out the research, and drafted the manuscript. FB, AE, and FH participated in the design and conceive of the study. SC helped in the design and revision of the draft. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 2.30 MB)
Rights and permissions
About this article
Cite this article
El-Senduny, F.F., Badria, F.A., EL-Waseef, A.M. et al. Approach for chemosensitization of cisplatin-resistant ovarian cancer by cucurbitacin B. Tumor Biol. 37, 685–698 (2016). https://doi.org/10.1007/s13277-015-3773-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3773-8