Abstract
Breast cancer is the most common cancer in women worldwide. Aberrant lipid metabolism is an established hallmark of cancer cells. The recently isolated lysophosphatidylcholine acyltransferase 1 (LPCAT1), the most important enzyme in membrane biogenesis, has been currently implicated in cancer development and progression. The published literature lacks comprehensive reports on LPCAT1 expression in breast cancer and its impact on patients’ outcome. We evaluated the immunohistochemical expression of LPCAT1 in 80 primary breast carcinomas, 24 metastatic lymph nodes, and 30 non-neoplastic breast tissue specimens and statistically analyzed the association between LPCAT1 expression and clinicopathological variables and patients’ outcome. LPCAT1 protein was significantly upregulated in primary breast carcinoma and showed a significant ascending pattern being the lowest in normal breast tissues, relatively increased in fibrocystic disease, and the highest in primary carcinoma. LPCAT1 expression was significantly higher at tumor’s advancing edge and correlated positively with tumor’s grade and TNM stage. Compared to primary tumor, LPCAT1 expression was significantly lower in ductal carcinoma in situ and significantly higher in metastatic lymph nodes. LPCAT1 overexpression was significantly associated with increased proliferative activity, negative estrogen receptor (ER) and progesterone receptor (PR) status, positive human epidermal growth factor receptor 2 (HER2) status, as well as triple-negative and HER2 disease molecular subtypes. Multivariate analysis showed that advanced stage, high grade, and LPCAT1 overexpression were independent predictors of early tumor recurrence. We conclude that LPCAT1 is implicated in breast cancer pathogenesis, evolution, and progression and appears to play a potentially crucial role as a determinant of local invasiveness and metastasis. LPCAT1 is an independent predictor of early tumor recurrence of breast carcinoma and represents a novel prognostic biomarker that reflects underlying biological alterations and thus constitutes a potentially promising target for new therapeutic strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the leading cause of cancer-related mortality in women worldwide [1]. In Egypt, breast cancer is the most common type of cancer in women [2].
Determination of therapeutic strategies based on outcome prediction is one of the most intriguing issues in cancer management. Biomarkers could play a pivotal role in accomplishing this task [3].
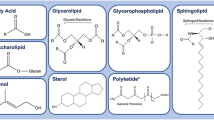
Alteration of cell membrane phospholipids, particularly phosphatidylcholine (PC) profile, is increasingly recognized as a hallmark of carcinogenesis [4]. PC is the most abundant phospholipid in mammalian cells and plays important roles in cellular structure and biological functions [5–7]. PC synthesis and metabolism has been recently implicated in the pathogenesis and progression of cancer [4].
PC, like other phospholipids, is synthesized de novo and then remodeled. The remodeling pathway (Lands’ cycle) involves consecutive deacylation and reacylation reactions controlled by the coordinated action of crucially important enzymes [4, 8–10].
Lysophosphatidylcholine acyltransferase 1 (LPCAT1), a key enzyme for PC remodeling in Lands’ cycle, is responsible for generation of PC from lysophosphatidylcholine (LPC) [4, 10, 11].
LPCAT1 protein, encoded by AYTL2 gene, was recently cloned and characterized in mouse alveolar type II cells where it is hypothesized to play a fundamental role in the biosynthesis of pulmonary surfactant [9, 12].
Subsequently, human LPCAT1 was cloned and characterized [13, 14]. LPCAT1 also plays an important role in retinal photoreceptor homeostasis and is involved in inflammatory lipid regulation [7, 15].
Through genomic efforts, three additional members of the LPCAT family: LPCAT2, LPCAT3, and LPCAT4, have been recently identified and partially characterized. LPCAT2 is 48 % homologous to LPCAT1, and it catalyzes both platelet-activating factor (PAF) and PC synthesis mainly in inflammatory cells. LPCAT3 is expressed ubiquitously and is primarily responsible for hepatic LPCAT activity. LPCAT4 is highly expressed in the epididymis, testis, ovary, and brain [5, 8].
Recent reports have argued that there is a close relationship between LPCAT1 overexpression and cancer development and progression. Few studies on prostatic, colorectal, and gastric carcinomas have probed this postulation [4, 15, 16].
The published literature lacks comprehensive reports on LPCAT1 expression in breast cancer and its impact on patients’ outcome. Therefore, this study was designed to evaluate the immunohistochemical expression of LPCAT1 protein in breast carcinoma and to correlate its expression with clinicopathological variables and patients’ outcome.
Materials and methods
Patients’ and specimens’ characteristics
Formalin-fixed and paraffin-embedded (FFPE) consecutive specimens from 80 Egyptian female patients (mean age = 44.4, standard deviation (SD) = 6.2, range = 33–59 years), who had undergone modified radical mastectomy for primary breast carcinoma (from June 2009 to June 2010), were retrospectively retrieved from the files of the Surgical Pathology Laboratory, Alexandria Faculty of Medicine, Egypt. Demographic, clinical, and follow-up data were available for all patients.
Eighty representative H&E-stained sections of primary invasive ductal carcinoma of no special type (IDC(NST)), including both representative viable tumor tissue and tumor's advancing edge, were selected; 62/80 (77.5 %) cases were lymph node-positive (mean number of positive nodes = 6.7, SD = 5.3, range = 1–25). Representative positive lymph nodes from 24/62 (38.7 %) node-positive cases were selected for LPCAT1 analysis. Grading and TNM staging were done according to established criteria [17–19].
Information on hormonal receptor and human epidermal growth factor receptor 2 (HER2) status was obtained from the pathological records and reviewed according to published guidelines [20, 21]. Accordingly, 56/80 (70 %) cases were estrogen receptor (ER)-positive, 51/80 (63.75 %) cases were progesterone receptor (PR)-positive, and 22/80 (27.5 %) cases were HER2-positive.
Clinicopathological characteristics of the studied cases are summarized in Table 1.
Exclusion criteria included: preoperative (neoadjuvant) chemotherapy, incomplete clinicopathological and follow-up information, diagnoses other than IDC(NST), HER2 immunohistochemical score of 2+ not confirmed by FISH analysis, and insufficient tissue for immunostaining.
Follow-up information was collected from the files of the Oncology Department, Main University Hospital, Alexandria Faculty of Medicine, Egypt. During the follow-up period (range = 8–48 months, median (Mdn) = 20, mean (M) = 22.6, SD = 10.6), a total of 18 (22.5 %) patients had events (defined as the first documented evidence of local, regional, or distant recurrence, or death of cancer) [22, 23]. The disease-free survival (DFS) time ranged from 4 to 30 months with an estimated mean survival time of 38.05 months (95 % confidence interval (CI) = 34.1, 42.0). The first 2-year hazard rate was 1 %. The estimated hazard rates in later intervals (<30 patients entered) were not presented.
In addition, 30 cases of non-neoplastic breast tissue specimens (normal breast tissue, 10 cases; non-proliferative fibrocystic disease (NPFCD), 10 cases; and proliferative fibrocystic disease (PFCD), 10 cases), obtained from Egyptian female patients (mean age 50.3, SD = 10.7, range = 27–74 years), served as a control group.
The local scientific ethical committee approved the study and REMARK criteria were applied [24].
Immunohistochemistry
An avidin-biotinylated immunoperoxidase methodology was utilized [15]. Antigen retrieval with HIER and 10 mM citrate buffer (pH 6.0) was done. The rabbit polyclonal LPCAT1 antibody (anti-human LPCAT1, ID; US Biological, USA) was applied in a dilution of 1:150. The rabbit monoclonal Ki67 antibody Clone:SP6 (Thermo Scientific™ Lab Vision™, USA) was applied in a dilution of 1:100. The bound antibodies were visualized by the UltraVision Detection System Anti-Polyvalent, HRP/DAB (Thermo Scientific™, USA). Negative and positive controls (human cerebellar tissue for LPCAT1 and human tonsil for Ki67) were included in all runs.
Immunohistochemistry scoring system
Evaluation of the immunostained slides was performed in a blinded manner without knowledge of the assigned clinical data. LPCAT1 immunostain was analyzed in benign and cancerous mammary glandular cells for the extent and intensity of staining [15]. The extent (%) of immunoreactive cells observed in each case was recorded as follows: 0, no immunoreactive cells; 1, 1–25 %; 2, >25–50 %; 3, >50–75 %; and 4, >75 %. The staining intensity was graded as weak (1), moderate (2), and strong (3). The final score was calculated by multiplying the extent and intensity scores, with a maximum score of 12. The staining pattern (cytoplasmic or cytoplasmic and nuclear) was recorded. Scoring for stromal cell staining followed the same scheme. In addition, LPCAT1 score was assessed in each primary tumor section at the tumor’s center and tumor’s advancing edge. Whenever detected, adjacent non-neoplastic tissue or ductal carcinoma in situ (DCIS) was evaluated for LPCAT1 staining. LPCAT1 scoring was also assessed in the studied 24 metastatic lymph nodes.
The proliferative activity, as assessed by Ki67 immunostaining, was expressed as an average percentage of positive tumor cells across each section of primary breast carcinoma [25]. A cutoff point at 20 % was used to categorize cases as belonging to high-expression (≥20 %) or low-expression (<20 %) groups [26, 27].
Statistical analysis
Statistical analyses were performed using SPSS® Statistics 21. Quantitative data were described using Mdn, range (minimum and maximum) as well as M and SD. Qualitative data were described using number and percentage. Various tests were used including Mann-Whitney (U), independent Student t (t), Wilcoxon signed rank (Z), paired t, Kruskal-Wallis (H), Pearson’s correlation (r), Spearman’s rho correlation coefficient (ρ), and pair-wise comparisons. Log rank test was used to compare the patients’ outcome between different groups. Univariate Cox regression was used to evaluate the effect of continuous covariates on patients’ outcome.
Several multivariate Cox regression models were developed to predict early tumor recurrence. Selection of variables was based on scientific backgrounds as well as the stability of the resulting models (measured by the size of standard errors (SE) of the estimated coefficients and the width of the resulting 95 % CI).
The hazard ratio (HR) assumption was checked by plots of log (-log survival time) with categorization of continuous variable by their median values. Validation of the resulting model was conducted by systematically removing each observation from the data set, estimating the regression equation, and computing “predicted \( {R}^2 \).” To plot Kaplan-Meier estimates for continuous markers, tertiles were used. Significance was judged at the 5 % level.
Results
Clinicopathological findings
The clinicopathological characteristics of the study group are summarized in Table 1. Molecular subtypes were determined according to hormonal receptor and HER2 status [26]. Hormonal receptor-positive and HER2-negative tumors were classified as luminal A subtype (44 cases, 55 %); hormonal receptor-positive and HER2-positive tumors as luminal B subtype (12 cases, 15 %); hormonal receptor-negative and HER2-positive tumors as HER2 disease (10 cases, 12.5 %); and hormonal receptor-negative and HER2-negative tumors as triple-negative subtype (14 cases, 17.5 %).
Proliferative activity in primary IDC(NST) specimens ranged from 5 to 60 % (M = 22.8, SD = 16.4). At a cutoff value of 20 %, 36 cases (45 %) showed high expression and 44 cases (55 %) showed low expression levels.
Expression of LPCAT1 and evolution and progression of breast cancer
We evaluated the immunohistochemical expression of LPCAT1 in 80 primary IDC(NST), 24 metastatic lymph nodes and 30 non-neoplastic breast tissue specimens (Figs. 1 and 2).
LPCAT1 protein immunohistochemical expression: (a) weak staining in a normal breast lobule (×40). (b) Focal staining of moderate intensity (arrow) in NPFCD (×40). (c) PFCD showing LPCAT1 staining of moderate intensity (×40). (d) Strong diffuse staining in invasive ductal carcinoma; note the weak staining in adjacent normal glands (arrow) (×40). (e) DCIS showing diffuse LPCAT1 staining of moderate intensity; note the nearby invasive tumor clusters with strong staining intensity (arrow) (×40). (f) Invasive ductal carcinoma showing diffuse LPCAT1 staining of strong intensity; note the focal moderate stromal staining (arrow) (×40)
LPCAT1 protein immunohistochemical expression: (a) Invasive ductal carcinoma showing moderate staining intensity at the tumor’s center (×100). (b) The same case shown in (a) with strong LPCAT1 signal at the tumor’s advancing edge (×100). (c) Grade 1 invasive ductal carcinoma showing weak LPCAT1 expression (×400). (d) Grade 2 invasive ductal carcinoma showing cytoplasmic staining of LPCAT1 of moderate intensity (×400). (e) Grade 3 invasive ductal carcinoma showing strong cytoplasmic and nuclear LPCAT1 staining (×400). (f) Lymph node with metastatic breast carcinoma from case depicted in (c) showing diffuse LPCAT1 staining of moderate intensity (×100)
LPCAT1 immunostaining detected in 76/80 (95 %) cases of IDC(NST) was significantly higher (M = 6.6, SD = 3.2) than the non-neoplastic control group (28/30 (93.33 %) cases, M = 2.8, SD = 1.4), (t = 8.62, p = .000). Adjacent non-neoplastic tissue was available in 31/80 (38.75 %) cases of IDC(NST), and it showed LPCAT1 expression in 29/31 (93.55 %) cases, M = 2.7, SD = 1.6, which was significantly lower (t = 6.9, p < .001) compared to the nearby invasive tumor (M = 6.8, SD = 3.2). LPCAT1 expression showed no statistically significant difference between adjacent non-neoplastic tissue and the control group (t = .145, p = .886).
LPCAT1 expression showed a statistically significant ascending pattern (ρ = .523, p = .000) being the lowest in normal breast tissues (Mdn = 2, range = 0–3), relatively increased in NPFCD (Mdn = 3, range = 1–6) and PFCD (Mdn = 4, range = 1–6), and the highest in primary invasive carcinoma (Mdn = 7, range = 0–12). A significant difference was detected among the aforementioned groups (H = 29.87, p = .000), with a significantly higher LPCAT1 expression in IDC(NST) compared to normal breast tissue (p = 0.025), NPFCD (p = 0.025), and PFCD (p = 0.025).
DCIS, seen in 22/80 (27.5 %) cases, showed a significantly lower (Z = 4.026, p = .000) LPCAT1 expression (19/22 (86.36 %) cases, Mdn = 6, range = 0–9) compared to the adjacent invasive tumor (Mdn = 8.5, range = 5–12).
LPCAT1 staining was significantly higher (t = 11.8, p < .001) at tumor’s advancing edge (M = 7.6, SD = 3.6) compared to tumor’s center (M = 5.4, SD = 2.9).
In addition, LPCAT1 expression in the 24 metastatic lymph nodes (Mdn = 8.5, range = 0–12) was significantly higher (Z = 4.3, p = .000) compared to their respective primary tumor tissue (Mdn = 7.5, range = 2–10).
Overall, staining pattern was cytoplasmic or cytoplasmic and nuclear with no statistically significant difference among IDC(NST) and control cases (X 2 = .005, p = .945). Similarly, stromal LPCAT1 staining was demonstrated in 41/80 (51.25 %) cases of IDC(NST) (Mdn = 1, range = 0–9) and in 17/30 (56.67 %) of control cases (Mdn = 1, range = 0–2) with no statistically significant difference (U = 1194.5, p = .968).
Correlation between LPCAT1 expression and clinicopathological parameters (Table 1)
LPCAT1 expression in IDC(NST) cases showed a significant positive correlation with grade, TNM stage, T stage, lymph node stage, number of positive lymph nodes (r = .520, p = .000), and proliferative activity (r = .582, p = .000). Correlation with age was statistically insignificant (r = .033, p = .864).
In addition, there were statistically significant associations between LPCAT1 overexpression and the presence of distant metastasis at diagnosis, negative ER, PR status and positive HER2 status, as well as tumors with high proliferative activity (≥20 %).
Correlation with molecular subtypes showed that LPCAT1 was significantly overexpressed in triple-negative and HER2 disease subtypes compared to luminal A subtype (p = .001 and p = .013, respectively).
The influence of clinicopathological variables and LPCAT1 expression on patients’ outcome
A bivariate analysis showed that the risk of early tumor recurrence (during the first 2 years) increased incrementally per unit increase in LPCAT1 expression (HR = 1.73, 95 % CI = 1.33, 2.24), proliferative activity (HR = 1.09, 95 % CI = 1.05, 1.12), and the number of positive lymph nodes (HR = 1.67, 95 % CI = 1.40, 1.99).
As shown in Table 2, higher rate of early recurrence and shorter DFS interval were significantly associated with higher grade, higher T and nodal stage, presence of distant metastasis, higher TNM stage, negative ER and PR status, high proliferative activity, and molecular subtype with triple-negative and HER2 disease subtypes being the worst compared to luminal A subtype (p = .000 and p = .006, respectively).
On the other hand, patients’ age (HR = .99, 95 % CI = .95, 1.03) and HER2 status had no significant impact on patients’ outcome.
A multivariate Cox regression model was built, and variables that showed high multicollinearity were excluded. Categorization of the included variables was tested until a stable model with better predictability was developed. Five variables were included in the final model: TNM stage (IV vs. I, II, III), tumor grade (3 vs. 1, 2), molecular subtype (luminal A vs. luminal B, HER2 disease and triple negative), Ki67 (continuous variable), and LPCAT1 expression (continuous variable). Using stepwise regression (Table 3), advanced TNM stage (stage IV), high tumor grade (grade 3), and LPCAT1 overexpression were independent predictors of early tumor recurrence (HR = 38.8, 95 % CI = 10.1, 149.4; HR = 6.0, 95 % CI = 1.7, 20.7; and HR = 1.6, 95 % CI = 1.1, 2.4, respectively). Figure 3
Validation of the resulting model was conducted by systematically removing each observation from the data set, and predicted \( {R}^2 \)” was estimated at 55.4 %.
Discussion
Breast cancer is the most frequently diagnosed cancer in women worldwide [28]. Lipid profile alterations represent a relatively new concept in oncogenesis and have been recently implicated in breast cancer pathogenesis [27, 29]. Aberrancy in PC metabolism was indicated in breast cancer cell lines, and PC accumulation was reported in breast tissues during progression to a malignant phenotype [30, 31].
The characterization of breast cancer tissues by differentiating among molecular species of PCs has been previously reported [32, 33]. Some specific PCs composed of monounsaturated fatty acids (MUFA-PCs) and saturated fatty acids (SFA-PCs) are relatively localized in cancerous areas compared to adjacent non-neoplastic tissue [27]. Stearoyl-CoA desaturase-1 (SCD1), which regulates the conversion of SFA into MUFA, showed accumulation in the cancerous breast tissues, indicating that it partially mediates the production of MUFA-PCs [27, 34]. SCD1 is suggested to play an important role in cancer progression, and higher SCD1 expression in breast cancer has been recently proposed as a poor prognostic marker [35].
The production of MUFA-PCs is also catalyzed by LPCAT1, which transfer MUFAs to LPCs [27, 36]. However, the expression of LPCAT1 in breast cancer tissue and its impact on prognosis has not been previously investigated.
In the study of Mansilla et al. [4], a limited number of breast tissue samples, in a tissue microarray containing various human tumors and corresponding normal tissues, were studied for LPCAT1 expression. Neither statistical analysis nor correlation with prognosis was done. Mansilla et al. [4] reported that all the tumor tissues, with the exception of adrenal gland, showed the same or stronger LPCAT1 intensity compared to normal tissues.
In our study, the noted overexpression of LPCAT1 protein (a synthetic enzyme of MUFA-PCs) in breast cancer tissue compared to the non-neoplastic breast tissue is consistent with the previously reported accelerated synthesis and accumulation of MUFA-PCs in the cancerous breast tissues [27]. Thus, we propose that LPCAT1 overexpression contributes to PC profile alterations which might fuel breast cancer tumorigenesis.
Mansilla et al. [4] reported LPCAT1 to be upregulated at both the transcript and protein levels in human colorectal adenocarcinomas compared to normal mucosa and concluded that LPCAT1 may contribute to total choline metabolite accumulation via PC remodeling, thereby altering the lipid profile of colorectal carcinomas, a characteristic of malignancy.
Similarly, higher LPCAT1 expression was reported in prostatic and gastric carcinomas compared to their respective non-neoplastic counterparts [15, 16]. Kikuchi et al. [16] have concluded that lipid alterations in the gastric mucosa, particularly overexpressed LPCAT1, appear to be involved in gastric cancer carcinogenesis.
Our study demonstrated that LPCAT1 expression showed a significant ascending pattern along with the evolution and progression of breast carcinoma being the highest in metastatic breast cancer and the lowest in normal breast tissue. Expression in primary carcinoma was significantly higher than non-neoplastic breast tissues and DCIS. In addition, the expression in primary tumors was significantly higher at tumors’ advancing edge and correlated positively with tumors’ grade. Our results suggest that LPCAT1 is implicated in the evolution of breast cancer, correlates with poor morphological phenotype, promotes local invasiveness and metastasis, and, thus, plays an important role in the progression of breast carcinoma.
The postulated role of LPCAT1 in the pathogenesis, evolution, and progression of cancer might also be explained by its possible epigenetic effects. The pattern of genes affected by LPCAT1 overexpression was reported to be complex and includes genes that encode proteins involved in signaling, inflammation, matrix proteases, and membrane receptors [37].
In accordance with our findings, Zhou et al. [15] demonstrated that LPCAT1 expression was the highest in metastatic prostatic tissue, was significantly higher in primary prostatic carcinoma compared to high-grade prostatic intraepithelial neoplasia and non-neoplastic prostatic tissues, and correlated with the grade of primary prostatic carcinoma. Grupp et al. [38] reported that increased LPCAT1 expression in prostatic carcinoma was associated with high Gleason score and positive surgical margin.
On the other hand, Kikuchi et al. [16] reported that LPCAT1 in gastric cancer was higher in differentiated than poorly differentiated adenocarcinoma.
LPCAT1 is characterized as an endoplasmic reticulum protein; hence, it mainly localizes in the cytoplasm; however, it might relocate into the nucleus under certain conditions and differentially regulates the expression of several genes [37]. In our study, LPCAT1 was localized to the cytoplasm or cytoplasm and nucleus of epithelial cells, a finding that lacked significant difference among neoplastic and non-neoplastic breast tissues. Zhou et al. [15] have reported cytoplasmic and nuclear localization of LPCAT1 in high-grade primary and metastatic prostate cancer. Mansilla et al. [4] reported cytoplasmic localization of LPCAT1 in colorectal carcinoma cells and adjacent benign mucosa.
In this study, LPCAT1 staining was mainly visualized in the epithelial cells; however, focal stromal expression was demonstrated. Future studies might elucidate this finding.
The present study demonstrated that LPCAT1 overexpression in breast cancer significantly correlated with higher TNM stage, higher tumor and nodal stages, higher number of positive lymph nodes, and the presence of distant metastasis at diagnosis. Similar results in prostate cancer were reported by Zhou et al. [15] and Grupp et al. [38] who found that increased LPCAT1 expression was significantly associated with advanced tumor stage. Grupp et al.[38] have in addition shown that higher LPCAT1 expression was significantly correlated with positive nodal involvement. On the other hand, Mansilla et al. [4] reported that LPCAT1 upregulation in colorectal carcinoma was independent of Dukes stage.
The discrepancies noted between our study and studies on LPCAT1 expression in gastric and colorectal carcinomas [4, 16], together with the similarities noted between our findings and previous studies on LPCAT1 expression in prostate cancer [15, 38], further emphasizes the commonality between breast and prostate cancer and adds to our understanding of the pathobiology of these two common cancers which will certainly pave the way for more effective therapies in the future [39].
Taken together, the noted correlation between LPCAT1 overexpression and nodal and distant metastasis as well as its higher expression at advancing tumor’s edge and metastatic tissue all point to its potentially crucial role as a determinant of local invasiveness and metastasis in breast cancer. This might be supported by previous studies that have postulated that LPCAT1 overexpression regulates matrix proteases, influences membrane fluidity with alterations in cell adhesion, and thus potentially plays a role in cancer cell local invasiveness and progression towards metastasis [4, 37].
Prognosis of breast cancer varies greatly depending on the molecular subtype of breast cancer which depends largely on hormonal receptor and HER2 expression [26]. Hormonal receptor negativity and HER2 positivity are known to be poor prognostic indicators in breast cancer [40]. Therefore, we attempted to study the relation between LPCAT1 expression and hormonal receptor and HER2 status as well as molecular subtype.
Our study showed significant associations between LPCAT1 overexpression and negative ER and PR status. In line with our findings, Hilvo et al. [33] reported high PC accumulation in ER-negative breast cancer cases. In contrast, Ide et al. [27] reported higher MUFA-PC level in ER-positive breast carcinomas and suggested a regulatory role for LPCATs [41, 42]. Higher LPCAT3 was reported in ER-positive than in ER-negative breast tissues [43]; however, the endogenous mechanisms regulating LPCATs’ activity are still poorly understood.
In breast cancer cells, the pathway involving HER2 receptor is generally considered to regulate lipogenic enzymes [44]. Our study further emphasized this suggestion, as a significant association between LPCAT1 overexpression and positive HER2 status was demonstrated. Future studies should look into the possible crosstalk between these two pathways.
In our study, subgroup analysis showed that LPCAT1 is significantly upregulated in certain molecular subtypes well-known for their aggressiveness, namely, triple-negative and HER2 disease compared to the more favorable luminal A subtype. There is no good molecular biomarker or targeted therapeutic approach for triple-negative breast cancer; thus, there is an urgent clinical need to identify underlying molecular mechanisms that would aid in patients’ management [45].
As the full extent and nature of LPCAT1 role in breast cancer unravels, its intricate mechanisms will become more apparent and provide unique opportunities for new forms of therapy. It is noteworthy that lipid profile changes may potentially influence current therapies because the dynamic and structural properties of lipid membranes can affect drug delivery [46].
Increased synthesis of membrane phospholipids is required for rapid growth during tumor development [4, 29, 47]; thus, the noted correlation between LPCAT1 overexpression and higher proliferative activity was expected. This finding strengthens our suggestion that overexpressed LPCAT1 contributes to evolution and progression of breast cancer.
Similarly, Mansilla et al. [4] reported a significant increase in colon cancer cell growth rate in association with LPCAT1 overexpression and hypothesized that LPCAT1 upregulation contributes to increased PC recycling, enhanced membrane synthesis, and increased proliferative activity.
It is well-known that tumor stage, grade, HER2 status, proliferative activity, and gene profiling are among the most important prognostic factors in breast cancer [26, 48]. Our study identified multiple indicators of early tumor recurrence. Multivariate analysis showed that advanced stage at diagnosis, high grade, and LPCAT1 overexpression were independent predictors of early tumor recurrence, among which, LPCAT1 represents a novel prognostic biomarker that reflects underlying biological alterations and thus constitutes a potentially promising target for new therapeutic models.
Zhou et al. [15] reported that the association of LPCAT1 expression with poor patient’s outcome in prostate cancer is independent of existing prognostic factors and concluded that LPCAT1 expression level in primary prostate cancer might be used as an indicator of future biochemical recurrence and/or metastasis. Grupp et al.[38] reported that the prognostic impact of LPCAT1 expression in prostate cancer was independent of histological and clinical parameters and concluded that LPCAT1 measurement may be utilized for better clinical decision-making.
We conclude that LPCAT1 exerts an important, albeit not fully understood, role in breast cancer oncogenicity, possibly via alterations in lipid profile. LPCAT1 is a novel biomarker in the evolution and progression of breast cancer and appears to play a potentially crucial role as a determinant of local invasiveness and metastasis. The influence of LPCAT1 expression on prediction of early tumor recurrence is independent of well-established prognostic factors of breast cancer.
To the best of our knowledge, this is the first published study analyzing LPCAT1 expression in a cohort of breast cancer patients with special emphasis on its impact on patients’ outcome. Our results open new horizons in the understanding of breast cancer pathobiology and establish new paths for potential novel therapeutic approaches.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
Hirko KA, Soliman AS, Ahmed Hablas, et al. (2013) Trends in breast cancer incidence rates by age and stage at diagnosis in Gharbiah, Egypt, over 10 years (1999–2008). Journal of Cancer Epidemiology, vol. 2013, Article ID 916394, 7 pages. doi:10.1155/2013/916394
Madu CO, Lu Y. Novel diagnostic biomarkers for prostate cancer. J Cancer. 2010;1:150–77. doi:10.7150/jca.1.150.
Mansilla F, da Costa KA, Wang S, Kruhøffer M, Lewin TM, Orntoft TF, et al. Lysophosphatidylcholine acyltransferase 1 (LPCAT1) overexpression in human colorectal cancer. J Mol Med (Berl). 2009;87(1):85–97. doi:10.1007/s00109-008-0409-0.
Bridges JP, Ikegami M, Brilli LL, Chen X, Mason RJ, Shannon JM. LPCAT1 regulates surfactant phospholipid synthesis and is required for transitioning to air breathing in mice. J Clin Invest. 2010;120(5):1736–48. doi:10.1172/JCI38061.
Ekroos K, Ejsing CS, Bahr U, Karas M, Simons K, et al. Charting molecular composition of phosphatidylcholines by fatty acid scanning and ion trap MS3 fragmentation. J Lipid Res. 2003;44:2181–92. doi:10.1194/jlr. D300020-JLR200.
Soupene E, Kuypers FA. Phosphatidylcholine formation by LPCAT1 is regulated by Ca(2+) and the redox status of the cell. BMC Biochem. 2012;7(13):8. doi:10.1186/1471-2091-13-8.
Yamazaki T1, Wakabayashi M, Ikeda E, Tanaka S, Sakamoto T, Mitsumoto A, et al. Induction of 1-acylglycerophosphocholine acyltransferase genes by fibrates in the liver of rats. Biol Pharm Bull. 2012;35(9):1509–15. doi:10.1248/bpb. b12-00243.
Nakanishi H, Shindou H, Hishikawa D, Harayama T, Ogasawara R, Suwabe A, Taguchi R, Shimizu T (2006) Cloning and characterization of mouse lung-type acylCoA:lysophosphatidylcholine acyltransferase 1(LPCAT1). Expression in alveolar type II cells and possible involvement in surfactant production. J Biol Chem. 21;281(29):20140-20147. doi:10.1074/jbc.M600225200.
Lands WE (2000) Stories about acyl chains. Biochim Biophys Acta. 3;1483(1):1-14. DOI: 10.1016/S1388-1981(99)00177-8.
Soupene E, Fyrst H, Kuypers FA (2008) Mammalian acyl-CoA:lysophosphatidylcholine acyltransferase enzymes. Proc Natl Acad Sci U S A. 8;105(1):88-93. doi: 10.1073/pnas.0709737104.
Chen X, Hyatt B, Mucenski M, Mason R, Shannon J. Identification and characterization of a lysophosphatidylcholine acyltransferase in alveolar type II cells. Proc Natl Acad Sci U S A. 2006;103:11724–9. doi:10.1073/pnas.0604946103.
Agarwal AK, Sukumaran S, Bartz R, Barnes RI, Garg A. Functional characterization of human 1-acylglycerol-3-phosphate-O acyltransferase isoform 9: cloning, tissue distribution, gene structure, and enzymatic activity. J Endocrinol. 2007;193(3):445–57. doi:10.1677/JOE-07-0027.
Harayama T, Shindou H, Shimizu T. Biosynthesis of phosphatidylcholine by human lysophosphatidylcholine acyltransferase 1. J Lipid Res. 2009;50(9):1824–31. doi:10.1194/jlr. M800500-JLR200.
Zhou X, Lawrence TJ, He Z, Pound CR, Mao J, Bigler SA. The expression level of lysophosphatidylcholine acyltransferase 1 (LPCAT1) correlates to the progression of prostate cancer. Exp Mol Pathol. 2012;92(1):105–10. doi:10.1016/j.yexmp.2011.11.001.
Kikuchi H, Uehara T, Setoguchi T, Yamamoto M, Ohta M, Kamiya K, et al. 2012 Overexpression of LPCAT1 and concomitant lipid alterations in gastric cancer. Cancer Research 72(8) .doi: 10.1158/1538-7445.AM2012-3022.
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver, M.J, eds. (2012) WHO classification of tumours of the breast, IARC Press, Lyon, France, Volume 4, 4th ed.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. the value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 1991;19(5):403–10. doi:10.1111/j.1365-2559.1991.tb00229.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, eds. (2010) AJCC cancer staging manual. Springer, New York, 7th ed.
Hammond MEH, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010;28:2784–95.
Wolff AC, Hammond MEH, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45. doi:10.1200/JCO.2006.09.2775.
Fisher B, Brown AM, Dimitrov NV, et al. Two months of doxorubicin-cyclophosphamide with and without interval reinduction therapy compared with 6 months of cyclophosphamide, methotrexate, and fluorouracil in positive-node breast cancer patients with tamoxifen-nonresponsive tumors: results from the National Surgical Adjuvant Breast and Bowel Project B-15. J Clin Oncol. 1990;8(9):1483–96.
Mansour EG, Gray R, Shatila AH, et al. Survival advantage of adjuvant chemotherapy in high risk node-negative breast cancer: ten year analysis—an intergroup study. J Clin Oncol. 1998;16:3486–92.
Altman DG, McShane LM, Sauerbrei W, Taube SE. Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK): explanation and elaboration. PLoS Med. 2012;9(5):e1001216. doi:10.1371/journal.pmed.1001216.
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J, et al. Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer Working Group. J Natl Cancer Inst. 2011;103:1656–64. doi:10.1093/jnci/djr393.
Nishimura R, Osako T, Okumura Y, Hayashi M, Toyozumi Y, et al. Ki-67 as a prognostic marker according to breast cancer subtype and a predictor of recurrence time in primary breast cancer. Exp Ther Med. 2010;1:747–54. doi:10.3892/etm.2010.133.
Ide Y, Waki M, Hayasaka T, Nishio T, Morita Y, et al. Human breast cancer tissues contain abundant phosphatidylcholine (36:1) with high stearoyl-CoA desaturase-1 expression. PLoS ONE. 2013;8(4):e61204. doi:10.1371/journal.pone.0061204.
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. Cancer incidence and mortality worldwide. Lyon: IARC Press; 2013.
Menendez JA, Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat Rev Cancer. 2007;7:763–77. doi:10.1038/nrc2222.
Ridgway ND. The role of phosphatidylcholine and choline metabolites to cell proliferation and survival. Crit Rev Biochem Molec. 2013;48(1):20–38. doi:10.3109/10409238.2012.735643.
Podo F, Saradanelli F, Iorio E, Canese R, Carpinelli G, et al. Abnormal choline phospholipid metabolism in breast and ovary cancer: molecular bases for noninvasive imaging approaches. Curr Med Imag Rev. 2007;3:123–37. doi:10.2174/157340507780619160.
Bougnoux P, Chajes V, Lanson M, Hacene K, Body G, et al. Prognostic significance of tumor phosphatidylcholine stearic acid level in breast carcinoma. Breast Cancer Res Treat. 1992;20:185–94.
Hilvo M, Denkert C, Lehtinen L, Muller B, Brockmoller S, et al. Novel theranostic opportunities offered by characterization of altered membrane lipid metabolism in breast cancer progression. Cancer Res. 2011;71:3236–45. doi:10.1158/0008-5472.CAN-10-3894.
Mauvoisin D, Mounier C. Hormonal and nutritional regulation of SCD1 gene expression. Biochimie. 2011;93:78–86. doi:10.1016/j.biochi.2010.08.001.
Holder AM, Gonzalez-Angulo AM, Chen H, Akcakanat A, Do KA, et al. High stearoyl-CoA desaturase 1 expression is associated with shorter survival in breast cancer patients. Breast Cancer Res Treat. 2013;137:319–27. doi:10.1007/s10549-012-2354-4.
Hishikawa D, Shindou H, Kobayashi S, Nakanishi H, Taguchi R, et al. Discovery of a lysophospholipid acyltransferase family essential for membrane asymmetry and diversity. Proc Natl Acad Sci U S A. 2008;105:2830–5. doi:10.1073/pnas.0712245105.
Ellis B, Kaercher L, Snavely C, Zhao Y (2012) Lipopolysaccharide triggers nuclear import of Lpcat1 to regulate inducible gene expression in lung epithelia. Chunbin ZouWorld J Biol Chem 26; 3(7): 159-166. doi: 10.4331/wjbc.v3.i7.159.
Grupp K, Sanader S, Sirma H, Simon R, et al. High lysophosphatidylcholine acyltransferase 1 expression independently predicts high risk for biochemical recurrence in prostate cancers. Online Molec Oncol. 2013;7(6):1001–11. doi:10.1016/j.molonc.2013.07.009.
Davis ID, Birrell SN, et al. Breast and prostate cancer: more similar than different. Nat Rev Cancer. 2010;10:205–12. doi:10.1038/nrc2795.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 2003;100:8418–23.
Shindou H, Hishikawa D, Harayama T, Yuki K, Shimizu T. Recent progress on acyl CoA: lysophospholipid acyltransferase research. J Lipid Res. 2009;50(Suppl):S46–51. doi:10.1194/jlr. R800035-JLR200.
Zhao Y, Chen YQ, Bonacci TM, Bredt DS, Li S, et al. Identification and characterization of a major liver lysophosphatidylcholine acyltransferase. J Biol Chem. 2008;283:8258–65. doi:10.1074/jbc.M710422200.
Cheng AS, Culhane AC, Chan MW, Venkataramu CR, Ehrich M, et al. Epithelial progeny of estrogen-exposed breast progenitor cells display a cancer-like methylome. Cancer Res. 2008;68:1786–96. doi:10.1158/0008-5472.CAN-07-5547.
Yoon S, Lee MY, Park SW, Moon JS, Koh YK, et al. Up-regulation of acetyl-CoA carboxylase alpha and fatty acid synthase by human epidermal growth factor receptor 2 at the translational level in breast cancer cells. J Biol Chem. 2007;282:26122–31. doi:10.1074/jbc.M702854200.
McDonald L, Ferrari N, Terry A, Bell M, Mohammed ZM, Cl O, et al. RUNX2 correlates with subtype-specific breast cancer in a human tissue microarray, and ectopic expression of Runx2 perturbs differentiation in the mouse mammary gland. Dis Model Mech. 2014;7:525–34. doi:10.1242/dmm.015040.
Jorgensen K, Hoyrup P, Pedersen TB, Mouritsen OG. Dynamical and structural properties of lipid membranes in relation to liposomal drug delivery systems. Cell Mol Biol Lett. 2001;6:255–63.
Scaglia N, Chisholm JW, Igal RA. Inhibition of stearoylcoa desaturase-1 inactivates acetyl-CoA carboxylase and impairs proliferation in cancer cells: role of AMPK. PLoS ONE. 2009;4:e6812. doi:10.1371/journal.pone.0006812.
Soerjomataram I, Louwman MWJ, et al. An overview of prognostic factors for long-term survivors of breast cancer. Breast Cancer Res Treat. 2008;107:309–30. doi:10.1007/s10549-007-9556-1.
Acknowledgments
The authors would like to thank all technicians at the Pathology Department, Alexandria Faculty of Medicine, Egypt.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdelzaher, E., Mostafa, M.F. Lysophosphatidylcholine acyltransferase 1 (LPCAT1) upregulation in breast carcinoma contributes to tumor progression and predicts early tumor recurrence. Tumor Biol. 36, 5473–5483 (2015). https://doi.org/10.1007/s13277-015-3214-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3214-8