Abstract
Leucine-rich α2 glycoprotein 1 (LRG1) has been shown to be aberrantly expressed in multiple human malignancies. However, the biological functions of LRG1 in human glioblastoma remain unknown. Here, we report for the first time the role of LRG1 in glioblastoma development based on the preliminary in vitro and in vivo data. We first confirmed the expression of LRG1 in human glioblastoma cell lines. Next, to investigate the role of LRG1 in the tumorigenesis and development of glioblastoma, a short hairpin RNA (shRNA) construct targeting LRG1 mRNA was transfected into U251 glioblastoma cells to generate a cell line with stably silenced LRG1 expression. The results showed that silencing of LRG1 significantly inhibited cell proliferation, induced cell cycle arrest at G0/G1 phase, and enhanced apoptosis in U251 cells in vitro. Consistently, LRG1 silencing resulted in the downregulation of key cell cycle factors including cyclin D1, B, and E and apoptotic gene Bcl-2 while elevated the levels of pro-apoptotic Bax and cleaved caspase-3, as determined by Western blot analysis. We further demonstrate that the silencing of LRG1 expression effectively reduced the tumorigenicity of U251 cells, delayed tumor formation, and promoted apoptosis in a xenograft tumor model in vivo. In conclusion, silencing the expression of LRG1 suppresses the growth of glioblastoma U251 cells in vitro and in vivo, suggesting that LRG1 may play a critical role in glioblastoma development, and it may have potential clinical implications in glioblastoma therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma, originating from neuroepithelial cells, is the most common and lethal tumor in the central nervous system with a 5-year survival rate of less than 5 % [1]. Histopathological and clinical criteria established by the World Health Organization indicate that glioblastoma is the grade IV glioma that originates from poorly differentiated astrocytes [2]. The aggressive nature of glioblastoma is ascribed to excessive cell proliferation, high resistance to apoptosis, and marked diffuse infiltration. Current treatment approaches for glioblastoma include surgery, chemotherapy, radiotherapy, as well as ongoing researches on gene therapy and immunotherapy [3, 4], but most patients have poor outcomes and die within the first year of diagnosis [5]. Molecular mechanisms underlying glioblastoma development and progression are poorly understood at the moment, and glioblastoma remains the focus of concern in the field of neurosurgery. Therefore, it is important to elucidate the mechanism for glioblastoma development, which has significant implications in the development of effective therapies.
Leucine-rich α2 glycoprotein (LRG) was isolated from human serum as a trace protein by Haupt and Baudner in 1977 [6]. The primary sequence of LRG consists of 312 amino acid residues, 66 of which are leucines. This protein contains eight repeating consensus sequences of 24 amino acid residues and exhibits a periodic pattern in the occurrence of leucine, proline, and asparagine [7, 8]. LRG1, a member of LRG family protein, has been demonstrated to play critical roles in many physiological and pathological processes [9, 10]. Studies have shown that upregulation of LRG1 is associated with multiple types of tumors [11, 12] and can promote endothelial cell proliferation and angiogenesis via the transforming growth factor-β (TGF-β) signaling pathway [13]. However, the role of LRG1 in the tumorigenesis and progression of human glioblastoma is not yet clear, and it is interesting to be elucidated.
In this study, we investigated the role of LRG1 in glioblastoma cell proliferation and apoptosis by knocking down LRG1 in a human glioblastoma cell line by short hairpin RNA (shRNA) interference strategy and examined the tumorigenicity and tumor growth capacity of LRG1-silenced glioblastoma cells in nude mice. The results indicated that silencing of LRG1 inhibited growth and induced the apoptosis of glioblastoma cells in vitro and in vivo.
Materials and methods
Cell culture
Human glioblastoma cell lines, U373, U251, U87-MG, and A172, and a malignant glioma cell line SHG-44 were obtained from the Cell Bank of Chinese Academy of Sciences (Shanghai, China). SHG-44 cells were cultured in RPMI-1640 (Gibco, Grand Island, NY, USA) supplemented with 10 % of FBS, while the rest of the cell lines were cultured in DMEM (Gibco) supplemented with 10 % FBS. The cells were maintained in a humidified atmosphere of 5 % CO2 at 37 °C. The cells at the exponential phase were used for experiments.
Generation of LRG1-silenced glioblastoma cell line
shRNA construct containing LRG1 shRNA, namely LRG1-pGCH1/Neo, and non-targeting control construct NC-pGCH1/Neo were designed and synthesized by GeneChem (Shanghai, China). The sequences of LRG1 shRNA are 5′-GATCCCCGATGTTTTCCCAGAATGACTTCAAGAGAGTCATTCTGGGAAAACATCTTTTT-3′, and the sequences of NC shRNA are 5′-GATCCCCTTCTCCGAACGTGTCACGTTTCAAGAGAACGTGACACGTTCGGAGAATTTTT-3′. U251 cells with the high expression of LRG1 were transfected with LRG1-pGCH1/Neo or NC-pGCH1/Neo using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s protocol. Twenty-four hours after transfection, the cells were selected with 200 μg/ml G418 (Invitrogen) for stable expression clones for over a week, and positive clones were picked for identification.
Real-time polymerase chain reaction (PCR)
Total messenger RNA (mRNA) from cultured cells was extracted with TRIzol (TIANGEN Biotech, Beijing, China) according to the manufacturer’s instructions. cDNA was obtained by reverse transcription. The primers for LRG1 and β-actin are as follows: LRG1 forward: 5′-GGTATTGAAAGAAAACCAGC-3′ and reverse: 5′-TGGCAAGGTCTCCAACTG-3′; β-actin forward: 5′-CTTAGTTGCGTTACACCCTTTCTTG-3′ and reverse: 5′-CTGTCACCTTCACCGTTCCAGTTT-3′. Quantitative analysis was performed using SYBR GREEN master mix (TIANGEN Biotech) in an Exicycler™ 96 quantitative fluorescence analyzer (Bioneer, Daejeon, Korea).
Western blot analysis
Cultured cells were lysed with NP-40 lysis buffer (Beyotime Institute of Biotechnology, Haimen, China), and total proteins from xenograft tumors were extracted using radio-immunoprecipitation assay (RIPA) lysis buffer (Beyotime). The protein concentration was determined with bicinchoninic acid (BCA) kits (Beyotime). Forty micrograms of total proteins from each sample were separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and electro-transferred to a polyvinylidene fluoride (PVDF) membrane (Millipore, Bedford, MA, USA). After blocking with 5 % non-fat milk at room temperature for 1 h, the membrane was incubated with a specific primary antibody (anti-LRG1, 1:500, Bioss, Beijing, China; anti-cleaved caspase-3, anti-Bax, anti-Bcl-2, anti-cyclin D1, E, B, anti-β-actin, 1:1000, Wanleibio, Shenyang, China) at 4 °C overnight followed by incubation with horseradish peroxidase (HRP)-labeled secondary antibody (Beyotime) at room temperature for 45 min. Proteins were visualized using ECL reagents (Wanleibio). After exposure, films were scanned and images were analyzed with Gel-Pro-Analyzer software for gray density comparison.
Colony formation assay
Cells were seeded sparsely onto 35-mm dishes at a density of 200 cells per dish, followed by incubation for 14 days at 37 °C in a humidified atmosphere with 5 % CO2. The colonies were rinsed with PBS, fixed with paraformaldehyde for 20 min, and stained with Giemsa (Nanjing Jiancheng Bioengineering Institute, Nanjing, China) for 5–8 min. The colonies consisting of at least 50 cells were counted under a microscope. Colony formation efficiency was calculated as (number of colonies/number of cells inoculated) × 100 %.
MTT assay
Cell proliferation was assessed by 3-(4,5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay. Cells were seeded in 96-well microplates at a density of 2 × 103 cells/well. The cells were incubated and allowed to adhere, and MTT (Sigma-Aldrich, St. Louis, MO, USA) was added to each well to a final concentration of 0.2 mg/ml at the indicated time point (12, 24, 48, 72, or 96 h). Following incubation at 37 °C for 4 h, the supernatant was removed, and formazan crystals were dissolved in 200 μl DMSO (Sigma-Aldrich) per well for 15 min. The optical density (OD) at 490 nm was determined with plate reader ELX-800 (BioTek, Vermont, USA).
Flow cytometric analysis
For cell cycle analysis, cells were fixed in 70 % cold ethanol at 4 °C for 2 h, incubated in staining buffer containing propidium iodide (PI) and RNase A for 30 min at 37 °C in the dark and analyzed for cell cycle distribution by flow cytometry in FACSCalibur (BD, Franklin Lakes, NJ, USA).
Apoptotic cells were detected using Annexin V/PI Apoptosis Detection Kit (Wanleibio) according to the manufacturer’s instructions. Cells were incubated with anti-Annexin V-FITC and PI in 500-μl binding buffer for 15 min at room temperature in the dark, and then subjected to flow cytometric analysis.
Hoechst assay
Apoptotic cells were detected using Hoechst staining Kit (Beyotime) according to the manufacturer’s instructions. Cells were seeded in 12-well microplates at a density of 1 × 105 cells/well and cultured for 24 h. When reaching 80 % confluence, cells were fixed, stained with Hoechst staining solution for 5 min, washed with PBS, and observed under a fluorescence microscope.
Xenograft transplantation into nude mice
Animal experiments were conducted with the approval of the Experimental Animal Ethics Committee of Harbin Medical University. Four- to six-week-old BABL/c nude mice were purchased from Vital River Laboratory Animal Technology Co. Ltd (Beijing, China). The mice were maintained under pathogen-free conditions at 22 °C, with 40–50 % humidity and a 12-h light/dark cycle, and allowed to access food and water ad libitum. The mice were assigned randomly to receive a subcutaneous inoculation of 106 parental U251 cells, U251 cells expressing NC construct, or U251 cells expressing LRG1 shRNA at the right armpit flank (n = 6 each group). Tumor sizes were measured every 3 days with calipers, and the tumor volumes were calculated as follows: volumes = a × b 2/2, where a is the larger of the two dimensions and b is the smaller.
Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay
Apoptotic cells in tumor tissues were detected using In Situ Cell Death Detection Kit (Wanleibio) according to the manufacturer’s instructions. Xenograft tumors were excised after the mice were sacrificed. Tumor tissues were paraffin embedded and sectioned. Paraffin sections were inactivated with H2O2 and then incubated with 50 μl TUNEL reaction solution at 37 °C for 60 min. After washing with PBS, the sections were incubated with 50 μl Converter-POD working solution at 37 °C for 30 min and developed with 3′-diaminobenzidine (DAB). The sections were then stained with hematoxylin for the nuclei and observed under an optical microscope at ×400 magnification.
Statistical analysis
Data and figures were processed in GraphPad Prism 5.0 software (San Diego, CA, USA). Values are presented as the mean ± standard deviation. Comparison between groups was performed using a one-way analysis of variance (ANOVA), and multiple comparisons were performed using Bonferroni post hoc test. P < 0.05 was considered statistically significant.
Results
Establishment of LRG1-silenced human glioblastoma cell line
To investigate the function of LRG1 in glioblastoma, we first examined the expression levels of LRG1 in various glioblastoma and malignant glioma cell lines by Western blot analysis. The results showed that LRG1 expression was the highest in U251 cells among the cell lines tested and the lowest in SHG-44 cells that originated from a grade III glioma (Fig. 1a). U251 cells were transfected with LRG1 shRNA construct and selected for stable expression clones. LRG1 expression in the stable expression clones was assessed, and the selected strain stably expressing LRG1 shRNA construct (LRG1 shRNA) exhibited reduced expression of LRG1 at both protein (Fig. 1b) and mRNA levels (Fig. 1c) as compared with parental U251 cells as well as U251 cells expressing NC construct (NC) (P < 0.001). These results indicated an efficient inhibition of LRG1 expression by shRNA interference.
Generation of a LRG1-silenced glioblastoma cell line. a Western blot analysis was performed to determine the levels of LRG1 expression in multiple human glioblastoma cell lines. b U251 cells were transfected with non-targeting control shRNA construct (NC) or LRG1 shRNA construct (LRG1 shRNA), and the stable expression clones were selected and examined for the protein levels of LRG1 by Western blot analysis. β-actin was used as an internal control; c real-time PCR analysis was performed to detect LRG1 mRNA level in the stably transfected cell strains. This figure shows the representative images of three independent experiments, and the values are presented as the mean ± standard deviation. Compared with NC control, ***P < 0.001
Silencing of LRG1 inhibited glioblastoma cell proliferation and induced cell cycle arrest
Colony formation assay was performed to assess the single-cell growth capacity of LRG1-silenced U251 cells. The colony number was significantly reduced in LRG1-silenced cells compared with control cells (Fig. 2a, b; P < 0.01), implying that LRG1 silencing impaired the growth of U251 cells. MTT results demonstrated that cell proliferation rate was notably decreased in LRG1-silenced cells compared with NC control (Fig. 2c). Furthermore, LRG1 silencing resulted in the accumulation of cells in G0/G1 phase (P < 0.001) and reduced cell numbers in S and G2/M phase (P < 0.01, P < 0.001), while no significant difference was observed between U251 and NC cells (Fig. 2d, e). The protein levels of several critical cell cycle regulators were examined by Western blot analysis, and the results indicated that the expression levels of the cyclin D1, B, and E proteins in LRG1-silenced cells were significantly reduced compared with NC cells (Fig. 2f–h; P < 0.001, P < 0.05, and P < 0.001, respectively). In summary, silencing of LRG1 inhibited cell growth by suppressing cell proliferation and inducing cell cycle arrest in glioblastoma U251 cells.
Silencing of LRG1 inhibited glioblastoma cell proliferation and cell cycle progression. a, b Single-cell proliferative capacity of LRG1-silenced cells was evaluated by colony formation assay; c MTT assay was performed to assess cell proliferation in vitro; d, e cultured cells were fixed, stained with PI, and subjected to flow cytometry for cell cycle analysis; f–h expression levels of cyclin D1, B, and E in LRG1-silenced and control cells were determined by Western blot analysis with β-actin as the internal control for grayscale comparison. This figure shows the representative images of repeated experiments, and data are presented as the mean ± standard deviation. Compared with NC, *P < 0.05, **P < 0.01, ***P < 0.001
LRG1 silencing induced apoptosis in glioblastoma cells
Cell apoptotic status of LRG1-silenced cells was analyzed with Annexin V/PI double staining and Hoechst assay. The number of apoptotic cells was significantly increased due to LRG1 silencing, and the apoptotic ratio of LRG1-silenced cells was 5.9-fold of NC cells as indicated by flow cytometry results (Fig. 3a, b; P < 0.001). LRG1 silencing also caused increased membrane permeability to Hoechst stain and chromatin fragmentation as revealed by Hoechst assay (Fig. 3c), which again indicated an enhanced cell apoptosis in LRG1-silenced cells. We further detected the levels of apoptotic suppressor Bcl-2 and its downstream executors such as pro-apoptotic protein Bax and cleaved caspase-3 by Western blot analysis. The results showed that the expression of Bcl-2 in LRG1-silenced cells was markedly downregulated (Fig. 3d, e; P < 0.001), whereas the levels of Bax and cleaved caspase-3 in LRG1-silenced cells were significantly elevated compared with NC cells (Fig. 3d, f, g; P < 0.001). These findings suggest that silencing of LRG1 expression resulted in enhanced apoptosis in glioblastoma U251 cells.
LRG1 silencing induced apoptosis of glioblastoma cells. a, b Cultured cells were double stained with FITC-conjugated anti-Annexin V antibody and PI, followed by flow cytometry analysis for cell apoptosis. The cells falling in the lower right and upper right quadrants were considered as early and late apoptotic cells which were analyzed with statistics; c cells cultured on glass slides were incubated with Hoechst solution to stain DNA in the apoptotic cells; d–g Western blot analysis was performed to determine the protein levels of Bcl-2, Bax, and cleaved caspase-3 in LRG1-silenced and control cells. β-actin was used as an internal control for grayscale analysis. This figure shows the representative images of three independent experiments, and data are presented as the mean ± standard deviation. Compared with NC cells, ***P < 0.001
LRG1 silencing inhibited glioblastoma growth in vivo
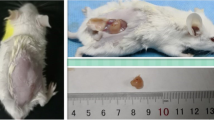
Since we had observed an inhibitory role of LRG1 in the growth of glioblastoma cells in vitro, we further investigated the biological role of LRG1 in glioblastoma development and progression in vivo with a glioblastoma xenograft model. LRG1-silenced cells, in parallel with parental U251 and NC control cells, were subcutaneously injected into 4- to 6-week-old nude mice. Tumor growth was followed for 30 days, and the tumors were weighed at the endpoint. Xenograft tumors derived from LRG1-silenced cells grew more slowly in mice, and LRG1-silenced cell-derived tumors were significantly smaller than control tumors at the endpoint (Fig. 4a, b; P < 0.05, P < 0.05). LRG1 silencing in vivo was confirmed by Western blot analysis (Fig. 4c; P < 0.001). Moreover, apoptosis in xenograft tumors was assessed by TUNEL assay, and more apoptotic cells were observed in LRG1-silenced cell-derived tumors than NC-derived tumors. These results indicated that LRG1 silencing suppressed tumor growth and induced apoptosis in vivo.
Silencing of LRG1 inhibited tumor growth in vivo. 106 U251 cells, NC cells, or LRG1-silenced cells were subcutaneously inoculated into 4- to 6-week-old nude mice. a Tumor volumes were recorded every 3 days for 30 days and b tumor weights were measured at the endpoint after the mice were sacrificed; c expression levels of LRG1 in xenograft tumor tissues were determined by Western blot analysis, and β-actin was used as an internal control for grayscale analysis; d xenograft tumor tissues were paraffin embedded, sectioned, and assayed by TUNEL to detect apoptotic cells in the tumor tissues. This figure shows the representative images from all the experiment animals, and data are expressed as the mean ± standard deviation. Compared with NC group, *P < 0.05, ***P < 0.001
Discussion
Studies have shown that LRG1 is highly expressed in various malignant tumors such as ovarian [14], lung [15], and colon cancer [16], yet the role LRG1 in glioblastoma has not been addressed, and whether inhibiting the expression of LRG1 can affect glioblastoma development remains to be elucidated. In the current study, a human glioblastoma cell line with a stable knockdown of LRG1 was established. LRG1 shRNA efficiently inhibited LRG1 expression in U251 cells, resulting in the marked suppression of cell proliferation and the induction of apoptosis. In addition, the silencing of LRG1 expression effectively reduced the tumorigenicity of glioblastoma cells, delayed tumor formation, and promoted apoptosis in glioblastoma xenograft tumors in nude mice. These findings demonstrate that LRG1 plays a critical role in the growth of glioblastoma in vitro and in vivo, suggesting that LRG1 might be further investigated as a potential therapeutic target for glioblastoma.
Proliferation and cell cycle are important factors in determining the degree of malignancy of tumors [17]. The cell cycle of eukaryotic cells is the fundamental process of cell proliferation [18]. Cyclins and cyclin-dependent protein kinases (CDKs) are two key protein families for the cell cycle regulation [19, 20]. Cyclins such as cyclin B, cyclin D1, and cyclin E has been demonstrated to play pivotal roles in G1/S phase transition during cell cycle, cell proliferation, and differentiation [21], and they are frequently over-expressed in a variety of carcinomas including lung cancer [22] and glioma [23], leading to shortened G1 phase and accelerated tumor formation [24]. The upregulation of cyclin B, D1, and E has been observed in glioma and glioblastoma tissues with positive correlation with tumor grade, yet the causes are elusive [25, 26]. Herein, we demonstrate that LRG1 acts as a master regulator for cell cycle genes in glioblastoma U251 cells, thereby modulating cell cycle, proliferation, and tumor growth. We found that LRG1 was highly expressed in the glioblastoma (grade IV glioma) cell lines but was expressed at a relatively lower level in SHG-44 cells that originated from grade III glioma, suggesting that LRG1 expression in glioma might be correlated with tumor grade. The silencing of LRG1 in U251 cells by RNA interference approach resulted in cell cycle arrest with the accumulation of cells in G0/G1 phase and reduced cell numbers in S and G2/M phases. Correspondingly, LRG1 silencing led to the downregulation of cell cycle genes including cyclin B, D1, and E, implying that LRG1 may regulate the cell cycle of glioblastoma cells through these cyclins. The above findings suggest that LRG1 plays an important regulatory role in the expression of cyclins, thereby modulating cell cycle, cell proliferation, and growth of glioblastoma.
The imbalance between cell proliferation and cell death is known to be an early and critical event in tumorigenesis, and apoptosis is a well-orchestrated cellular mechanism to maintain the balance [27]. Apoptosis is regulated by multiple factors at molecular level, such as the expression levels of Bcl-2 and Bax, as well as the cleavage of caspase-3. The disruption of the balance between anti-apoptotic protein Bcl-2 and pro-apoptotic protein Bax can activate the caspase pathway, resulting in a serial cleavage of caspases and ultimate apoptosis [28]. Our study showed that the silencing of LRG1 expression in glioblastoma U251 cells effectively promoted apoptosis in vitro and in xenograft tumors. Meanwhile, LRG1 silencing resulted in the downregulation of Bcl-2 expression and the elevated levels of Bax and cleaved caspase-3, indicating an enhanced apoptosis in LRG1-silenced cells. These results suggest that LRG1 may play an inhibitory role in the apoptosis of glioblastoma cells through these classic apoptotic players.
Although a number of clinical studies have indicated a strong association of LRG1 upregulation with tumor progression in patients [14–16], surprisingly, little has been reported about the role of LRG1 in tumor development. In the present study, we established a xenograft tumor model in nude mice using parental U251 and, NC and LRG1-silenced cells, and found that LRG1 silencing significantly inhibited the growth of xenograft tumors and induced apoptosis in vivo. Here, we report for the first time that LRG1 silencing suppresses tumor growth in vivo, revealing the biological importance of LRG1 in tumor development. The levels of sera LRG1 are elevated in several carcinomas, and sera LRG1 has been proposed as a promising prognostic marker for ovarian, lung, and colon cancers [14–16]. Future studies on the levels of LRG1 in the sera and tumor tissues of glioblastoma patients are the primary task to validate the role of LRG1 in glioblastoma development. In addition, for those tumors wherein LRG1 upregulation has been detected, further studies can be conducted to assess the therapeutic potentials of LRG1.
Conclusions
Our study demonstrate that the silencing of LRG1 in human glioblastoma cells suppresses cell proliferation and induces cell apoptosis in vitro and in vivo, indicating that LRG1 promotes cell proliferation while inhibiting apoptosis in glioblastoma. LRG1 plays a critical role in glioblastoma development, and it may have potential clinical values in glioblastoma prognosis and therapy.
Conflicts of interest
None
References
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–96.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 who classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109.
Cuddapah VA, Robel S, Watkins S, Sontheimer H. A neurocentric perspective on glioma invasion. Nat Rev Neurosci. 2014;15:455–65.
Arrillaga-Romany I, Reardon DA, Wen PY. Current status of antiangiogenic therapies for glioblastomas. Expert Opin Investig Drugs. 2014;23:199–210.
Cloughesy TF, Cavenee WK, Mischel PS. Glioblastoma: from molecular pathology to targeted treatment. Annu Rev Pathol. 2014;9:1–25.
Shirai R, Hirano F, Ohkura N, Ikeda K, Inoue S. Up-regulation of the expression of leucine-rich alpha(2)-glycoprotein in hepatocytes by the mediators of acute-phase response. Biochem Biophys Res Commun. 2009;382:776–9.
Haupt H, Baudner S. Isolation and characterization of an unknown, leucine-rich 3.1-s-alpha2-glycoprotein from human serum (author's transl). Hoppe Seylers Z Physiol Chem. 1977;358:639–46.
Weivoda S, Andersen JD, Skogen A, Schlievert PM, Fontana D, Schacker T, et al. Elisa for human serum leucine-rich alpha-2-glycoprotein-1 employing cytochrome c as the capturing ligand. J Immunol Methods. 2008;336:22–9.
O'Donnell LC, Druhan LJ, Avalos BR. Molecular characterization and expression analysis of leucine-rich alpha2-glycoprotein, a novel marker of granulocytic differentiation. J Leukoc Biol. 2002;72:478–85.
Nakajima M, Miyajima M, Ogino I, Watanabe M, Miyata H, Karagiozov KL, et al. Leucine-rich alpha-2-glycoprotein is a marker for idiopathic normal pressure hydrocephalus. Acta Neurochir (Wien). 2011;153:1339–46. discussion 1346.
Linden M, Segersten U, Runeson M, Wester K, Busch C, Pettersson U, et al. Tumour expression of bladder cancer-associated urinary proteins. BJU Int. 2013;112:407–15.
Liu Y, Luo X, Hu H, Wang R, Sun Y, Zeng R, et al. Integrative proteomics and tissue microarray profiling indicate the association between overexpressed serum proteins and non-small cell lung cancer. PLoS One. 2012;7:e51748.
Wang X, Abraham S, McKenzie JA, Jeffs N, Swire M, Tripathi VB, et al. Lrg1 promotes angiogenesis by modulating endothelial tgf-beta signalling. Nature. 2013;499:306–11.
Andersen JD, Boylan KL, Jemmerson R, Geller MA, Misemer B, Harrington KM, et al. Leucine-rich alpha-2-glycoprotein-1 is upregulated in sera and tumors of ovarian cancer patients. J Ovarian Res. 2010;3:21.
Li Y, Zhang Y, Qiu F, Qiu Z. Proteomic identification of exosomal lrg1: a potential urinary biomarker for detecting nsclc. Electrophoresis. 2011;32:1976–83.
Ladd JJ, Busald T, Johnson MM, Zhang Q, Pitteri SJ, Wang H, et al. Increased plasma levels of the apc-interacting protein mapre1, lrg1, and igfbp2 preceding a diagnosis of colorectal cancer in women. Cancer Prev Res (Phila). 2012;5:655–64.
Schonberg DL, Lubelski D, Miller TE, Rich JN. Brain tumor stem cells: molecular characteristics and their impact on therapy. Mol Asp Med. 2014;39:82–101.
Sherr CJ. Cancer cell cycles. Science. 1996;274:1672–7.
Schafer KA. The cell cycle: a review. Vet Pathol. 1998;35:461–78.
Lee MH, Yang HY. Regulators of g1 cyclin-dependent kinases and cancers. Cancer Metastasis Rev. 2003;22:435–49.
Hochegger H, Takeda S, Hunt T. Cyclin-dependent kinases and cell-cycle transitions: does one fit all? Nat Rev Mol Cell Biol. 2008;9:910–6.
Gautschi O, Ratschiller D, Gugger M, Betticher DC, Heighway J. Cyclin d1 in non-small cell lung cancer: a key driver of malignant transformation. Lung Cancer. 2007;55:1–14.
Chen X, Zhao T, Li L, Xu C, Zhang X, Tse V, et al. Ccnd1 g870a polymorphism with altered cyclin d1 transcripts expression is associated with the risk of glioma in a Chinese population. DNA Cell Biol. 2012;31:1107–13.
Simpson DJ, Fryer AA, Grossman AB, Wass JA, Pfeifer M, Kros JM, et al. Cyclin d1 (ccnd1) genotype is associated with tumour grade in sporadic pituitary adenomas. Carcinogenesis. 2001;22:1801–7.
Sun G, Shi L, Yan S, Wan Z, Jiang N, Fu L, et al. Mir-15b targets cyclin d1 to regulate proliferation and apoptosis in glioma cells. Biomed Res Int. 2014;2014:687826.
Daniel P, Filiz G, Brown DV, Hollande F, Gonzales M, D'Abaco G, et al. Selective creb-dependent cyclin expression mediated by the pi3k and mapk pathways supports glioma cell proliferation. Oncogenesis. 2014;3:e108.
Qi S, Song Y, Peng Y, Wang H, Long H, Yu X, et al. Zeb2 mediates multiple pathways regulating cell proliferation, migration, invasion, and apoptosis in glioma. PLoS One. 2012;7:e38842.
Cory S, Adams JM. The bcl2 family: regulators of the cellular life-or-death switch. Nat Rev Cancer. 2002;2:647–56.
Acknowledgments
This study was supported by a grant from the National Natural Science Foundation of China (No.: 30640008).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhong, D., Zhao, S., He, G. et al. Stable knockdown of LRG1 by RNA interference inhibits growth and promotes apoptosis of glioblastoma cells in vitro and in vivo. Tumor Biol. 36, 4271–4278 (2015). https://doi.org/10.1007/s13277-015-3065-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3065-3