Abstract
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) comprise a heterogeneous group of diseases. Advanced GEP-NENs are considered distinct disease entity with limited treatments. In this review, we will explore the biological rationale and clinical data of everolimus-based combinations for advanced GEP-NENs. PubMed/Medline, the Cochrane Library, and Google Scholar were searched using the terms “GEP-NENs” and “everolimus” and “systemic therapy” and selecting English literature only. Outcomes of interest included progression-free survival and overall survival (PFS and OS), toxicities, and tumor response. A total of 14 potentially relevant trials were initially identified, of which five studies were excluded. Hence, nine trials including 699 patients were included. Median PFS was reported in four out of the nine studies ranging from 14.6 to 16.4 months. The disease control rate was reported in all studies, and it ranged from 75 to 93 %. Frequently reported grade 3/4 toxicities were elevated transaminases, hyperglycemia, and hematologic toxicities. The presence of clinical and statistical heterogeneity of the primary studies precludes reliable evidence-based conclusions. Further well-conducted randomized controlled trials are awaited to better evaluate the treatment of GEP-NENs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) comprise a heterogeneous group of diseases [1–3]. In the current WHO grading system, GEP-NENs are classified according to their Ki-67 proliferation index into neuroendocrine tumor (NET) grade 1 (G1), with a Ki-67 index equal to or <2 %, NET G2 with a Ki-67 index between 3 and 20 %, and neuroendocrine carcinoma (NEC) G3 with a Ki-67 index greater than 20 % [4]. A number of prognostic factors have been described for GEP-NENs including the grading system which were found to correlate well with the clinical course of GEP-NENs patients [5]. Additionally, clinical features such as the primary site of the tumor, the secretory nature of the tumor, and the stage of the disease also contribute to their prognosis [6]. In patients with localized well-differentiated neuroendocrine tumors, 5-year survival is 60–100 % while with regional disease or distant metastases 5-year survival is 40–29 %, respectively [7]. Surgery has been usually advocated as a primary treatment of localized disease while systemic treatment has usually been evaluated in advanced/metastatic disease [8].
The available systemic treatments for advanced GEP-NENs are diverse, including cytotoxic chemotherapy, somatostatin analog (SSA), radionuclide therapy, and molecular targeted therapeutics. To date, targeted treatments with kinase inhibitors represent the only feasible approach for NEN-patients having a metastatic disease that show huge clinical/morphological progression [53]. Moreover during the past decade, a number of deregulated genes related to pathogenesis of NENs have been described with consequent assessment for potential therapeutic targets [9]. The mechanistic target of rapamycin (mTOR) pathway tops this list with demonstrated important role in the development of GEP-NENs, particularly from pancreas (pNENs) [10, 11]. Accordingly, the mTOR inhibitor everolimus has been largely studied in GEP-NENs and consequent to a landmark phase III study [12], it has been approved by Food and Drug Administration (FDA) and European Medical Agency (EMA) for patients with advanced well/moderately differentiated progressing pNENs. However, in spite of the progress made in this field, there are still unanswered questions with regard to mTOR targeting in GEP-NENs, with the suggested cross talk with other pathways active in NENs (e.g., MAP kinase pathway and VEGF pathway) emerging as an important mechanism of resistance and consequently opening the question about the value of co-targeting different pathways.
Biological rationale for combining everolimus with other systemic agents in advanced GEP-NENs
Basic biology of mTOR pathway activity in GEP-NENs
The mTOR is a serine/threonine kinase that regulates many cellular functions like growth, metabolism, angiogenesis, as well as cell cycle progression. mTOR is regulated by the molecular products of the phosphatidylinositol-3-kinase (PI3K)/AKT pathway. Abnormal activity of the mTOR pathway appears to be present in many tumor types, including NENs [13, 14]. For example, PI3K amplification, AKT over expression, as well as loss of phosphatase and tensin homolog (PTEN) function have all been associated with cancer development and progression [15]. The deregulation of PI3K/AKT signaling has been reported through a variety of biological mechanisms, including mutations/amplifications of both PI3K and AKT, in addition to mutations decreasing activity of PTEN [16, 17].
Rationale for everolimus combination with MAP kinase pathway-targeted therapeutics
The mitogen-activated protein kinase (MAPK) signaling pathway plays an essential role in coordinating gene expression in normal as well as malignant cells through transmitting extracellular signals to the intracellular mechanisms, i.e., growth, proliferation, and differentiation [18, 19].
Biology of many human cancers-including NENs provides a strong rationale for a co-targeting strategy of these two important pathways because of different methods of cross talk and compensatory activation loops between both pathways that may promote resistance in case of the use of single pathway targeting strategy [17]. For example, one interesting driver mechanism of carcinogenic deregulation of the mTOR pathway is the overexpression or activation of MAP kinase-related growth factor receptors such as HER-2 and insulin-like growth factor receptor (IGFR), which provides a real biological rationale for the co-targeting of both pathways in the treatment of many human cancers [20]. Preclinically, one study has evaluated the impact of co-targeting strategy in NENs cell lines. Zitzmann et al. examined the antitumor potential of combined targeting of mTOR (RAD001), mTOR/PI3K (NVP-BEZ235), and Raf (Raf265) on human NENs cell lines of heterogeneous origin. This study showed that the combined treatment with RAD001 or NVP-BEZ235 and Raf265 was more effective than single treatment with either kinase inhibitor alone. This study provides another strong rationale for dual targeting of PI3K–Akt–mTOR pathway and Ras–Raf–MEK–Erk1/2 pathway in NENs [21].
Rationale for everolimus combination with VEGF-targeted therapeutics
Vascular endothelial growth factor (VEGF) is one of the most commonly studied molecular markers in health and disease [22, 23]. Overexpression of angiogenic markers (like VEGF, endoglin, and CXCL-12) both in serum and tissue has been first proposed as an adverse prognostic factor in NENs; consequent to this, a number of preclinical and clinical studies have confirmed the prognostic value of the above markers [24–27].
Therapeutically, a Japanese group from Tokyo University has evaluated the tumor inhibitory effect of bevacizumab on pancreatic NENs cell lines both alone and in combination with gemcitabine with very encouraging results [28, 29]. This has been followed by a number of prospective studies for VEGF-targeted agents culminating in the approval of sunitinib for advanced pancreatic NETs [52]. Meanwhile, a number of preclinical studies have suggested a strong relationship between mTOR pathway and VEGF pathway [28, 30, 58], suggesting that combined VEGF and mTOR inhibition is an interesting proposal that needs to be further examined in clinical studies. Moreover, in the results of the biomarker analysis accompanying the landmark RADIANT-3 study (which investigated the effect of the mTOR inhibitor everolimus on PFS in patients with advanced pancreatic neuroendocrine tumors), significantly longer PFS was noted in patients with lower levels of VEGF-A and sVEGFR1 which provides another proof for a possible synergistic effect between everolimus and VEGF-targeted therapeutics.
Rationale for everolimus combination with somatostatin analogs
SSAs have long been used as a systemic treatment for advanced GEP-NETs [31]. SSAs are not only symptomatic agents but have also an anti-neoplastic action (although this is still discussed in the literature) [50, 54, 55]. However, more recently, many preclinical as well as clinical data have suggested a potential synergistic effect of combining SSAs with mTOR inhibitors like everolimus. Fernandes and coworkers have evaluated the prognostic significance of AKT/mTOR signaling in advanced neuroendocrine tumors treated with somatostatin analogs. They found that constitutive activation of the AKT/mTOR pathway was associated with shorter time-to-progression in patients undergoing treatment with SSAs [32]. Synergistic inhibition of proliferation and attenuated phosphorylation of all downstream targets of Akt: TSC2, mTOR, and p70S6K, were noted after combined administration of octreotide and RAD001 in a neuro-endocrine tumor cell line (rat insulinoma cell line, INS1) has shown [33]. This provides a strong rationale for a combined SSAs/mTOR inhibitors approach warranting further evaluation in prospective clinical studies.
Rationale for everolimus combination with metronomic chemotherapy
Low response rates and toxicity profiles have traditionally limited the widespread use of standard dose cytotoxic chemotherapy in the treatment of GEP-NET [35]. However, more recently, the use of newer chemotherapy combinations as well as metronomic chemotherapy dosing for agents like capecitabine or temozolomide (either as a monotherapy or in combination with other agents) has become popular in the management of advanced GEP-NET [36, 56, 57]. One of the main biological mechanisms of action of metronomic chemotherapy is through targeting of the VEGF pathway [37, 38]; thus, the combination of everolimus and metronomic chemotherapy may be considered biologically favorable as it provides an additional co-targeting strategy of mTOR pathway and VEGF pathway. Moreover, treatment with kinase inhibitors (like sunitinib) is also based on a metronomic scheme, and this scheme seems to be more effective in advanced NEN.
Objective of this review
In this systematic review, we will explore the true impact of everolimus-based combination on efficacy and toxicity parameters for patients with advanced GEP-NENS.
Methods
Search strategy
A comprehensive search for English-speaking literature was conducted in the following databases: the Medline, Cochrane library, and Google scholar, to identify all potentially relevant publications; the date of the last search was the first of July 2014. Meeting abstracts including ASCO, ESMO, ENETS, and NANETS were also reviewed. Articles with the following text words or Medical Subject Headings [MeSH] in their titles, abstracts, or keyword lists were examined: “GEP-NENs” and “everolimus” and “systemic therapy.” Reference lists of original studies and review articles were also reviewed for further related articles [cross-references].
Selection criteria
Inclusion criteria include the following:
-
1.
Clinical studies that describe everolimus-based combination for the treatment of advanced GEP-NENs.
-
2.
Tumor response and/or toxicities were reported.
Exclusion criteria are as follows:
-
1.
Non-English language records were also excluded.
Data extraction
Data were extracted by two independent reviewers. All eligible articles underwent initial review for relevancy and reporting of outcomes of interest. The following information/data were extracted from the studies where available: Eastern Cooperative Oncology Group (ECOG) Performance Status, treatment regimen and schedule, site of the tumor, WHO grade, complete response (CR) rate, partial response (PR) rate, stable disease (SD) rate, disease control rate (DCR: CR+PR+SD), response assessment strategy (WHO or Response Evaluation in Solid Tumors, RECIST), progression-free survival (PFS), overall survival (OS), and the incidence of toxicities.
Outcome measures
The outcome measures of interest were PFS, OS, tumor response, and toxicities. Toxicities were categorized using National Cancer Institute criteria. The main outcome measures are summarized using descriptive statistics. This systematic review adheres to the guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses report (PRISMA Statement) [34].
Results
Selection of studies
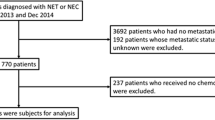
A total of 14 potentially relevant trials were identified in the literature search (Fig. 1). After initial review, two records were found to be non-English records and were excluded. The remaining 12 records underwent additional review for assessment of eligibility. Three studies were found to be ineligible because they did not report any of the relevant outcomes; thus, a total of nine trials met the eligibility criteria and were included in the systematic review.
Studies and patients characteristics
In our analysis, all the studies included were prospective studies of which there were three phase I studies, five phase II studies, and one phase III study included (Table 1).
The number of patients from individual trials ranged from 17 to 429. All the studies included only WHO grade I-II GEP-NENs that was not amenable to local surgical resection. Six of nine trials reported ECOG Performance Status. The vast majority (90–100 %) of patients had ECOG scores of 0 or 1.
Treatment regimens
Everolimus-based regimens were given in a continuous manner in all studies till progression or unacceptable toxicity.
Everolimus was scheduled as 5–10 mg daily and was combined with the following:
-
Cytotoxic chemotherapy: metronomic temozolomide in one study.
-
Somatostatin analogs, e.g., octreotide long-acting release (LAR) and pasireotide in five studies.
-
Targeted therapeutics, e.g., sorafenib (in one study), bevacizumab (in one study), erlotinib (in one study), and IMC-A12 (in one study).
Progression-free survival and overall survival
Median PFS was reported in four out of the nine studies and there was inter-trial variability in median PFS (Table 2, Fig. 3). Median reported PFS ranged from 14.6 to 16.4 months.
Median OS was not reached in three studies and was not reported in the other studies (Table 2).
Tumor response
Response assessment was done by RECIST in all studies. The Disease Control Rate (i.e., DCR defined as: complete response + partial response + stable disease) was reported 75–93 % in all studies (Fig. 2).
Stable disease was the major response subtype in most of the studies. Details of different response subtypes in each study were reported in Table 2.
Toxicities
All trials reported the toxicities experienced during combination therapy (Table 3). The most common all grade toxicities included elevated transaminases, stomatitis, fatigue, and hematologic toxicities. The most common grade 3 or 4 toxicities were elevated transaminases, hyperglycemia, and hematologic toxicities.
Discussion
Our systematic review is—to our knowledge—the first systematic review to examine the efficacy and safety of combination systemic anticancer therapies plus everolimus for the treatment of advanced GEP-NENS. Our review included nine clinical trials which involved 699 patients. There was an apparent lack of homogeneity between the studies in many aspects. However, in general, the results (PFS, OS, tumor response, and toxicities) from these trials indicate that combined everolimus-based treatment shows promises as an effective and tolerable treatment for advanced GEP-NENS.
Till now, the only two molecularly targeted therapies approved by the United States Food and Drug administration for the treatment of advanced well/moderately differentiated GEP-NENS are everolimus and sunitinib. A number of phase III clinical trials have explored the efficacy and safety of everolimus and sunitinib monotherapy in patients with advanced GEP-NENS. In the RADIANT-3 study evaluating everolimus monotherapy in advanced GEP-NENs, the median progression-free survival was 11.0 months with everolimus as compared with 4.6 months with placebo [12]. While in the sunitinib phase III study, median progression-free survival was 11.4 months in the sunitinib group as compared with 5.5 months in the placebo group [49]. Other non-targeted agents approved for both antiproliferative and functional benefits in advanced well/moderately differentiated GEP-NENs include octreotide LAR and this has been based on the PROMID trial which is a prospective randomized controlled study of octreotide LAR, 30 mg every 4 weeks which proved the antiproliferative efficacy of octreotide LAR. The median time to tumor progression was 14.3 months with octreotide LAR versus 6 months with placebo [50].
However, the survival benefit achieved with the above two targeted agents as well as that achieved by somatostatin analogs in the PROMID study was not convincing; thus, the search for alternative combinational strategies of two or more of the active agents seems very attractive.
Overall, the efficacy of the different everolimus-based combinations for the treatment of advanced GEP-NENs appears to compare favorably with that of other molecularly approved agents in advanced well/moderately differentiated GEP-NENs. All the four trials that reported median PFS in our systematic review reported rates that are greater than those reported in both everolimus monotherapy and sunitinib monotherapy trials (Fig. 3). This was particularly remarkable for the phase III combination of everolimus with octreotide LAR with a progression-free survival reaching 16.4 months, which further supports the suggestion of a possible cross talk between VEGF pathway and PI3K/mTOR pathway that needs to be further explored. However, it has to be noted that although the difference between everolimus/octreotide arm versus placebo/octreotide arm was p = 0.026, it did not reach the predefined level of statistical significance for this study [45]. Less remarkable results were achieved with everolimus/temozolomide combination as well as everolimus/bevacizumab combination.
Additionally, the DCR was around 92 % in six studies and around 82 % in two studies, and this also appears to compare favorably with the everolimus and sunitinib monotherapies. Taken together, these findings suggest that everolimus in combination with some other agents may prove to be a better therapeutic option for advanced GEP-NENs. Equally interesting, in the study of Yao et al. (2008) that reported median PFS, there was differential PFS among different subtypes of GEP-NENs, with the median PFS of 50 weeks for islet cell tumors versus 63 weeks for carcinoid tumors. Moreover, median PFS for patients with known stable disease at the start of treatment was 74 weeks versus 50 weeks for those in progression. These are the two interesting perspectives that need to be considered in the design and interpretation of prospective everolimus-based studies.
Two doses of everolimus were given in our systematic review: 5 and 10 mg (both daily in a nonstop fashion). In the study of Yao et al. (2008), median PFS for everolimus 5 mg was 50 weeks, while for everolimus 10 mg, it was 72 weeks. This has also been correlated with higher rates of everolimus-related toxicities in this cohort.
Everolimus was combined with cytotoxic chemotherapy, e.g., metronomic temozolomide in one study, somatostatin analogs, e.g., octreotide LAR and pasireotide in five studies, and targeted therapeutics, e.g., sorafenib [40], bevacizumab [46], erlotinib [48], and IMC-A12 [47]. Such combinations have largely affected the patterns of toxicity as well as the efficacy in different studies.
Similar to other mTOR inhibitors, everolimus is well known to be associated with some characteristic side effects, including fatigue, mucocutaneous toxicities, hyperglycemia, hyperlipidemia, and elevated transaminases [51]. Most of the side effects experienced by patients in this review were grade 1 or 2. However, certain toxicities were particularly annoying in some studies (depending on the companion drug) [40, 44]. This suggests that everolimus-based combination should be cautiously administered in certain patient populations based on concurrent illness and the type of companion drug.
Temsirolimus, another mTOR inhibitor, has been evaluated for the treatment of pancreatic neuroendocrine tumors in combination with bevacizumab in a phase II study. This combination has shown substantial activity with response rate of 44 % and 6-month PFS of 80 % well in excess of single targeted agents in pancreatic NENs [39]. This provides further rationale about the utility co-targeting mTOR and VEGF pathways in the management of GEP-NETs.
Future perspectives
Well-designed prospective randomized studies with robust biomarker program are important to further evaluate the issue of everolimus-based combination. Across the globe, a number of prospective studies are being conducted to evaluate novel everolimus-based combination (Table 4).
Limitations
This systematic review has a number of limitations that should be acknowledged. The most important of which is the obvious heterogeneity with respect to phase of the study and drug combinations that make inter-trial comparisons difficult. Moreover, the possibility of a publication bias is there (i.e., negative data may not be reported or published) which may compromise the reliability of the conclusions.
Conclusions
In conclusion, the presence of clinical and statistical heterogeneity of the primary studies precludes reliable evidence-based conclusions. Further well-conducted randomized controlled trials are awaited to better evaluate these treatment options with specific attention to subset analysis with regards to the site and grade of GEP-NENs, dose of everolimus and companion drug, as well as response status.
References
Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008;9(1):61–72.
Kwekkeboom DJ, Kam BL, Van Essen M, Teunissen JJ, van Eijck CH, Valkema R, et al. Somatostatin receptor-based imaging and therapy of gastroenteropancreatic neuroendocrine tumors. Endroc Relat Cancer. 2010;17(1):R53–73.
Kaltsas GA, Besser GM, Grossman AB. The diagnosis and medical management of advanced neuroendocrine tumors. Endocr Rev. 2004;25(3):458–511.
Rindi G, Klöppel G, Alhman H, Caplin M, Couvelard A, De Herder WW, et al. TNM staging of foregut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2006;449(4):395–401.
Pape UF, Jann H, Müller-Nordhorn J, Bockelbrink A, Berndt U, Willich SN, et al. Prognostic relevance of a novel TNM classification system for upper gastroenteropancreatic neuroendocrine tumors. Cancer. 2008;113(2):256–65.
Rindi GUIDO, Falconi M, Klersy C, Albarello L, Boninsegna L, Buchler MW, et al. TNM staging of neoplasms of the endocrine pancreas: results from a large international cohort study. J Natl Cancer Inst. 2012;104(10):764–77.
Plockinger U, Rindi G, Arnold R, Eriksson B, Krenning EP, de Herder WW, et al. Guidelines for the diagnosis and treatment of neuroendocrine gastrointestinal tumours. A consensus statement on behalf of the European Neuroendocrine Tumour Society (ENETS). Neuroendocrinology. 2004;80(6):394–424. doi:10.1159/000085237.
Abdel-Rahman O, Fouad M. Bevacizumab-based combination therapy for advanced gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs): a systematic review of the literature. J Cancer Res Clin Oncol. 2014. doi:10.1007/s00432-014-1757-5.
Öberg K. Biotherapies for GEP-NETs. Best Pract Res Clin Gastroenterol. 2012;26(6):833–41.
Ganetsky A, Bhatt V. Gastroenteropancreatic neuroendocrine tumors: update on therapeutics. Ann Pharmacother. 2012;46(6):851–62.
Shida T, Kishimoto T, Furuya M, Nikaido T, Koda K, Takano S, et al. Expression of an activated mammalian target of rapamycin (mTOR) in gastroenteropancreatic neuroendocrine tumors. Cancer Chemother Pharmacol. 2010;65(5):889–93.
Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514–23.
Wullschleger S, Loewith R, Hall M. TOR signaling in growth and metabolism. Cell. 2006;124:471–84.
Thoreen C, Chantranupong L, Keys HR, Wang T, Gray NS, Sabatini DM. A unifying model for mTORC1-mediated regulation of mRNA translation. Nature. 2012;485(7396):109–13.
Huang S, Houghton PJ. Inhibitors of mammalian target of rapamycin as novel antitumor agents: from bench to clinic. Curr Opin Investig Drugs. 2002;3:295–304.
Faivre S, Kroemer G, Raymond E. Current development of mTOR inhibitors as anticancer agents. Nat Rev Drug Discov. 2006;8:671–88.
Fazio N, Abdel-Rahman O, Spada F, Galdy S, De Dosso S, Capdevila J, et al. RAF signaling in neuroendocrine neoplasms: from bench to bedside. Cancer Treat Rev. 2014. doi:10.1016/j.ctrv.2014.06.009.
Mordret G. MAP kinase kinase: a node connecting multiple pathways. Biol Cell. 1993;79:193–207.
L′Allemain G. Deciphering the MAP kinase pathway. Program Growth Factor Res. 1994;5:291–334.
Meric-Bernstam F, Gonzalez-Angulo AM. Targeting the mTOR signaling network for cancer therapy. J Clin Oncol. 2008;13:2278–87.
Zitzmann K, Rüden J, Brand S, Goke B, Lichtl J, Spottl G, et al. Compensatory activation of Akt in response to mTOR and Raf inhibitors—a rationale for dual targeted therapy approaches in neuroendocrine tumor disease. Cancer Lett. 2010;295(1):100–9.
Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science. 1989;246:1306–9.
Abdel-Rahman O. Targeting vascular endothelial growth factor (VEGF) in gastric cancer; preclinical and clinical aspects. Crit Rev Oncol Hematol. 2014. doi:10.1016/j.critrevonc.2014.05.012.
Pinato DJ, Tan TM, Toussi ST, Ramachandran R, Martin N, Meeran K, et al. An expression signature of the angiogenic response in gastrointestinal neuroendocrine tumours: correlation with tumour phenotype and survival outcomes. Br J Cancer. 2014;110(1):115–22. doi:10.1038/bjc.2013.682. Epub 2013 Nov 14.
Kuiper P, Hawinkels LJ, de Jonge-Muller ES, Biemond I, Lamers CB, Verspaget HW. Angiogenic markers endoglin and vascular endothelial growth factor in gastroenteropancreatic neuroendocrine tumors. World J Gastroenterol. 2011;17(2):219–25. doi:10.3748/wjg.v17.i2.219.
Poncet G, Villaume K, Walter T, Pourreyron C, Theillaumas A, Lépinasse F, et al. Angiogenesis and tumor progression in neuroendocrine digestive tumors. J Surg Res. 2009;154(1):68–77. doi:10.1016/j.jss.2008.03.055. Epub 2008 Apr 29.
Takahashi Y, Akishima-Fukasawa Y, Kobayashi N, Sano T, Kosuge T, Nimura Y, et al. Prognostic value of tumor architecture, tumor-associated vascular characteristics, and expression of angiogenic molecules in pancreatic endocrine tumors. Clin Cancer Res. 2007;13(1):187–96.
Kasuya K, Nagakawa Y, Suzuki M, et al. Anti-vascular endothelial growth factor antibody single therapy for pancreatic neuroendocrine carcinoma exhibits a marked tumor growth-inhibitory effect. Exp Thermal Med. 2011;2(6):1047–52. Epub 2011 Sep 5.
Kasuya K, Nagakawa Y, Suzuki M, et al. Combination therapy of gemcitabine or oral S-1 with the anti-VEGF monoclonal antibody bevacizumab for pancreatic neuroendocrine carcinoma. Exp Thermal Med. 2012;3(4):599–602. Epub 2012 Jan 18.
Villaume K, Blanc M, Gouysse G, Walter T, Couderc C, Nejjari M, et al. VEGF secretion by neuroendocrine tumor cells is inhibited by octreotide and by inhibitors of the PI3K/AKT/mTOR pathway. Neuroendocrinology. 2010;91(3):268–78.
Valle JW, Eatock M, Clueit B, Gabriel Z, Ferdinand R, Mitchell S. A systematic review of non-surgical treatments for pancreatic neuroendocrine tumours. Cancer Treat Rev. 2014;40(3):376–89.
Fernandes I, Pacheco TR, Costa A, Santos AC, Fernandes AR, Santos M, et al. Prognostic significance of AKT/mTOR signaling in advanced neuroendocrine tumors treated with somatostatin analogs. Oncol Targets Ther. 2012;5:409.
Grozinsky-Glasberg S, Franchi G, Teng M, Leontiou CA, Dalino P, Salahuddin N, et al. Octreotide and the mTOR inhibitor RAD001 (everolimus) block proliferation and interact with the Akt-mTOR-p70S6K pathway in a neuro-endocrine tumour cell line. Neuroendocrinology. 2007;87(3):168–81.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):006–1012.
Tejani MA, Saif MW. Pancreatic neuroendocrine tumors: does chemotherapy work? J Pancreas. 2014;15(2):132–4.
Lamarca A, Hubner RA, Valle JW. Looking beyond chemotherapy in patients with advanced, well-differentiated, pancreatic neuroendocrine tumors. J Oncol Pathol. 2014;2(1):15–25.
André N, Carré M, Pasquier E. Metronomics: towards personalized chemotherapy? Nat Rev Clin Oncol. 2014;11:413–31.
Yao JC, Shah M, Panneerselvam A, Chen D, Stergiopoulos S, Ito T, et al. The VEGF pathway in pancreatic neuroendocrine tumors: prognostic and predictive capacity of baseline biomarker levels on efficacy of everolimus analyzed from the radiant-3 study. Pancreas. 2013;42(2):386–7.
Hobday T, Rubin J, Holen K, et al. MC044 h, a phase II trial of sorafenib in patients (pts) with metastatic neuroendocrine tumors (NET): a phase II consortium (P2C) study. J Clin Oncol. 2007;25(18):4504.
Chan JA, Mayer RJ, Jackson N, Malinowski P, Regan E, Kulke MH. Phase I study of sorafenib in combination with everolimus (RAD001) in patients with advanced neuroendocrine tumors. Cancer Chemother Pharmacol. 2013;71(5):1241–6.
Chan JA, Ryan DP, Zhu AX, Abrams TA, Wolpin BM, Malinowski P, et al. Phase I study of pasireotide (SOM 230) and everolimus (RAD001) in advanced neuroendocrine tumors. Endroc Relat Cancer. 2012;19(5):615–23.
Bajetta E, Catena L, Fazio N, Pusceddu S, Biondani P, Blanco G, et al. Everolimus in combination with octreotide long-acting repeatable in a first-line setting for patients with neuroendocrine tumors: An ITMO group study. Cancer. 2014;120(16):2457–63.
Yao JC, Phan AT, Chang DZ, Wolff RA, Hess K, Gupta S, et al. Efficacy of RAD001 (everolimus) and octreotide LAR in advanced low-to intermediate-grade neuroendocrine tumors: results of a phase II study. J Clin Oncol. 2008;26(26):4311–8.
Chan JA, Blaszkowsky L, Stuart K, Zhu AX, Allen J, Wadlow R, et al. A prospective, phase 1/2 study of everolimus and temozolomide in patients with advanced pancreatic neuroendocrine tumor. Cancer. 2013;119(17):3212–8.
Pavel ME, Hainsworth JD, Baudin E, Peeters M, Hörsch D, Winkler RE, et al. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT-2): a randomised, placebo-controlled, phase 3 study. Lancet. 2011;378(9808):2005–12.
Yao J, Phan A, Hess K, Fogelman D, Jacobs C, Dagohoy C et al. (2010) Randomized run-in study of Bevacizumab and everolimus in low to intermediate- grade neuroendocrine tumor (lgneTs) using perfusion CT (pCT) as functional biomarker. http://www.nanets.net/nanets_cd/2010/pdfs/C36.pdf. Accessed 29 April 2014.
Dasari A, Phan A, Gupta S, Hess KR, Culotta KS, Rashid A, et al. A phase I study of the anti-IGF-1R monoclonal antibody (MoAb), IMC-A12 (I), and everolimus (E) in well-differentiated neuroendocrine tumors (WD NET). J Clin Oncol. 2014;32(23):8. MILL ROAD, STE 800, ALEXANDRIA, VA 22314 USA: AMER SOC CLINICAL ONCOLOGY.
Bergsland EK, Watt L, Ko AH, Tempero MA, Korn WK, Kelley RK. A phase II study to evaluate the safety and efficacy of RAD001 plus erlotinib in patients with well-differentiated neuroendocrine tumors (NET). J Clin Oncol. 2012;30 Suppl 4:abstr 285.
Raymond E, Dahan L, Raoul JL, Bang YJ, Borbath I, Lombard-Bohas C, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):501–13.
Rinke A, Müller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID study group. J Clin Oncol. 2009;27(28):4656–63.
Abdel-Rahman O, Fouad M. Risk of mucocutaneous toxicities in patients with solid tumors treated with everolimus; a systematic review and meta-analysis. Expert Rev Anticancer Ther. 2014;14(12):1529-36.
Raymond, E., Niccoli-Sire, P., Bang, Y., Borbath, I., Lombard-Bohas, C., & Valle, J. W. (2010, January) Updated results of the phase III trial of sunitinib (SU) versus placebo (PBO) for treatment of advanced pancreatic neuroendocrine tumors (NET). In ASCO 2010 Gastrointestinal Cancers Symposium Abstract (Vol. 127).
Marotta V, Franzese MD, Del Prete M, Chiofalo MG, Ramundo V, Esposito R, et al. Targeted therapy with kinase inhibitors in aggressive endocrine tumors. Expert Opin Pharmacother. 2013;14(9):1187–203. doi:10.1517/14656566.2013.796931.
Ramundo V, Del Prete M, Marotta V, Marciello F, Camera L, Napolitano V, et al. Impact of long-acting octreotide in patients with early-stage MEN1-relate duodeno-pancreatic neuroendocrine tumors. Clin Endocrinol (Oxf). 2014;80(6):850–5. doi:10.1111/cen.12411.
Marciello F, Di Somma C, Del Prete M, Marotta V, Ramundo V, Carratu A, et al. Combined biological therapy with lanreotide autogel and cabergoline in the treatment of MEN-1-related insulinomas. Endocrine. 2014;46:678–81.
Strosberg JR, Fine RL, Choi J, Nasir A, Coppola D, Chen DT, et al. First‐line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer. 2011;117(2):268–75.
Ekeblad S, Sundin A, Janson ET, Welin S, Granberg D, Kindmark H, et al. Temozolomide as monotherapy is effective in treatment of advanced malignant neuroendocrine tumors. Clin Cancer Res. 2007;13(10):2986–91.
Abdel-Rahman O. Vascular endothelial growth factor (VEGF) pathway and neuroendocrine neoplasms (NENs): prognostic and therapeutic considerations. Tumor Biol. 2014;35(11):10615–25.
Conflicts of interest
None
Author’s contributions
OA: Provided the idea and study design and collected the data and wrote the manuscript.
MF: Collected the data and revised the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdel-Rahman, O., Fouad, M. Everolimus-based combination for the treatment of advanced gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs): biological rationale and critical review of published data. Tumor Biol. 36, 467–478 (2015). https://doi.org/10.1007/s13277-015-3064-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3064-4