Abstract
The Ser326Cys polymorphism in the human 8-oxogunaine DNA glycosylase (hOGG1) gene had been implicated in cancer susceptibility. Studies investigating the associations between the Ser326Cys polymorphism and digestion cancer susceptibility showed conflicting results. Therefore, a meta-analysis was performed to derive a more precise estimation of the relationship. We conducted a meta-analysis of 48 studies that included 12,073 cancer cases and 19,557 case-free controls. We assessed the strength of the association using odds ratios (ORs) with 95 % confidence intervals (CIs). In our analysis, the hOGG1 Ser326Cys polymorphism was significantly associated with the risk of digestive system cancers (Cys/Cys vs. Ser/Ser: OR = 1.17, 95 % CI = 1.00–1.35, P < 0.001; Cys/Cys vs. Cys/Ser + Ser/Ser: OR = 1.14, 95 % CI = 1.00–1.29, P < 0.001). In subgroup analyses by cancer types, we found that the hOGG1 Ser326Cys polymorphism may increase hepatocellular cancer and colorectal cancer risks, but decrease the risk of oral cancer. These findings supported that hOGG1 Ser326Cys polymorphism may contribute to the susceptibility of digestive cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Digestive tract cancers are complex, multistep, multifactorial, and highly fatal diseases. Genetic factors, environmental exposures, and gene–environment interactions all contribute to the risk of these cancers’ development. Digestive tract cancers contain alimentary tract and digestive gland cancers. Among them, hepatocellular, colorectal, gastric, and esophagus cancers were common cancers with high incidence and mortality in the world.
Inflammation, smoking, alcohol, and low-nutrition intake were known to be the main exogenous causes to the risk of digestive system cancer. The mechanism includes induce oxidative stress [1–6]. Reactive oxygen species (ROS) is one of the major oxidative pathways, which could increase damage to DNA and modify the structure of genes. When the production of ROS exceeds the antioxidant-defense capacity, the oxidative DNA damage occurs, resulting in mutations that can activate oncogenes or inactivate tumor suppressor genes and eventually lead to cancer [7, 8]. One of the well-studied products of ROS is 8-oxo-7, 8-dihydroguanine (8-oxoGua), a typical biomarker of oxidative stress, which is a strongly mutagenic lesion due to its ability to mispair with adenine during DNA replication, leading to G:C to T:A mutations [9, 10]. DNA repair systems are fundamental to the maintenance of genomic integrity and necessary for the restoration of the mismatched genes. Decreased efficiency of DNA repair accelerates genetic instability and the rate of genetic change, which may play a vital role in carcinogenesis [11]. An important mechanism to protect cell against mutagenic effect of ROS is base excision repair pathway (BER) [12–15]. BER removes modified base by specific glycosylases, which can be assisted by endonucleases. After abasic site priming, gap filling, and ligation, the changed base can be repaired, thus maintaining the stability of DNA. The DNA repair enzyme human oxoguanine glycosylase 1 (hOGG1), a key multifunctional gene involved in BER pathway, plays an important role in preventing carcinogenesis by repairing oxidative damage to DNA [16]. The hOGG1 gene is located at 3p25, a region which is found to be frequently missing in various tumors, which show loss of heterozygosity of markers [17]. Protein hOGG1, the product of hOGG1 gene, is a bifunctional glycosylase that could remove 8-oxoG directly from the oxidatively damaged DNA [18, 19]
Polymorphisms in DNA repair genes are assumed to cause deficit in DNA repair capacity, which may lead to genetic instability and carcinogenesis. Many sequence variants have been detected in hOGG1 gene. Among them, the 1,245 C > G (polymorphism Ser326Cys; rs1052133) is a well-known and well-studied hOGG1 gene polymorphism. This polymorphism is a C to G polymorphism in exon 7 of the hOGG1 gene, resulting in the substitution of cysteine for serine at codon 326. Activity of 8-oxoguanine DNA glycosylase is significantly affected by the Ser326Cys polymorphism in hOGG1. The DNA repair activity of hOGG1-Cys326 was weaker than the hOGG1-Ser326-encoded protein [20].
So far, there were so many reports about the correlation of hOGG1 Ser326Cys polymorphism with the risk of different cancers, including digestive cancers, such as pancreatic [21, 22], gallbladder [23–26], gastric [16, 27–38], colorectal [39–51], esophageal [52–58], oral cancer [59, 60], hepatocellular cancer [14, 61], and so on [13, 26]. Recent meta-analysis has reported the association of hOGG1 Ser326Cys polymorphism and cancers. However, by the limitation of inadequate publications, they did not calculate pooled ORs of digestive system cancers comprehensively, and results from each study have been conflicting and contradictory. To improve the efficiency of analysis on digestive system cancers and reduce the potential heterogeneity between studies which might derive from various cancers in diverse systems, we perform this meta-analysis for the association between hOGG1 Ser326Cys polymorphism and digestive system cancers.
Materials and methods
Identification and eligibility of relevant studies: PubMed, Embase, and other studies in the public domain (until 28 February 2013) search were performed using following search terms: “oxoguanine glycosylase 1, hOGG1 or OGG1,” “polymorphism or variant,” and “cancer, neoplasm or tumor.” Additional studies were identified by a hand search of the references of original studies. In case of the studies with the same or overlapping data, we selected the most recent ones with the largest number of subjects. Studies included in this meta-analysis should meet the following criteria: (a) evaluation of the association of hOGG1 Ser326Cys polymorphism and digestive system cancer risk published in English language; (b) study was designed using the methodology of a case–control study; (c) contains available genotype frequency, and there was sufficient data for the computation of odds ratios and corresponding 95 % confidence intervals (ORs, 95 % CIs).
Data extraction
Two investigators independently extracted the data and reached a consensus on all the items. For each study, the following characteristics were collected: last name of first author, year of publication, country of origin, ethnicity, cancer types, genotyping methods, matching criteria, source of control, and numbers of genotyped cases and controls. Different ethnic descents were categorized as Caucasians, Asians, and Africans. In addition, if only one cancer type was included in a study in the meta-analysis, it was combined into the “others” group. For the study of Hanaoka and colleagues [31], which included subjects of different ethnic groups, data were extracted separately for each ethnic group, and the study of Huang and colleagues [26] contains three cancer types, so we separately extracted the data as three studies.
Statistical analysis
The strength of the association between hOGG1 Ser326Cys polymorphism and digestive system cancer risk was measured by odds ratios (ORs) with 95 % confidence intervals (CIs). We first estimated the risks of the Cys/Cys and Ser/Cys genotypes on risk of cancer compared with the wild-type Ser/Ser as homozygote and heterozygote models, respectively, and then evaluated the risks of “Cys/Cys + Ser/Cys vs. Ser/Ser” and “Cys/Cys vs. Ser/Cys + Ser/Ser” on risk of digestive system cancer, assuming dominant and recessive effects of the variant Cys allele, respectively. Subgroup analysis was also performed based on different ethnicities, cancer types, and source of control.
Heterogeneity was evaluated with a chi-square-based Q test among the studies (P < 0.10 was considered significant) [62, 63]. When the heterogeneity was present, the random effects model was used to calculate the pooled OR [64], whereas the fixed effects model was used in its absence [65]. Sensitivity analysis was performed to assess the stability of the results.
Stratification by cancer types, source of controls, and ethnicity was conducted. All cancers were categorized into different groups based on cancer types: gallbladder cancer, gastric cancer, colorectal cancer, esophageal cancer, oral cancer, hepatocellular cancer, pancreatic cancer, and others. Eligible studies were classified into population-based and hospital-based according to control source. The subjects were classified by ethnicity into Caucasian group and Asian group.
The departure of frequencies of hOGG1 Ser326Cys polymorphism from expectation under Hardy–Weinberg equilibrium (HWE) in control population was judged by the chi-square test. P value less than 0.05 was considered to be a state of disequilibrium. Publication bias was diagnosed with Egger’s linear regression method [66, 67] and funnel plot. The P value less than 0.05 in Egger’s linear regression indicated the presence of potential publication bias. The standard error of logarithm for OR was plotted against its OR in funnel plot. Begg’s funnel plot was also plotted to detect the publication bias and influence of individual study on pooled OR. Log OR was plotted versus standard error of log OR for each included study in Begg’s funnel plot [68], and asymmetric or incomplete funnel-shaped plots demonstrated publication bias also. In the one-way sensitivity analysis, we excluded one single study each time, and the new pooled results could reflect the influence of that deleted study to the overall summary OR. All statistical analysis was implemented with STATA 11.0 (STATA Corp, College Station, TX). All P values were two-sided.
Results
Study characteristics
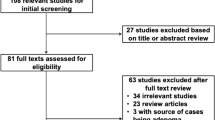
For digestive system cancer susceptibility, articles were retrieved based on the search criteria. Four hundred forty-one articles were screened. Two hundred forty-five articles were excluded because of no relevant study (e.g., review and meta-analysis). Ninety-one articles were excluded since they have no association with digestive cancer. Forty articles were not case–control studies. Eleven articles were not in English. Nine articles cannot extract useful data. Finally, a total of 48 case–control studies involving 12,073 cancer cases and 19,557 controls were included in the meta-analysis (we separate Hanaoka and colleagues’ study into two studies and Huang and colleagues’ studies into three). The characteristics of included studies were summarized in Table 1. There were 20 studies of Caucasian descendants and 28 studies of Asian descendants. Cancers were confirmed histologically or pathologically in most studies. There were 4 studies of gallbladder cancer, 14 studies of gastric cancer, 14 studies of colorectal cancer, 7 studies of esophageal cancer, 2 studies of oral studies, 2 studies of hepatocellular cancer, 2 studies of pancreatic cancer, and 4 studies of others. There were 23 studies in which the controls come from population-based (PB) source and 25 studies from hospital-based (HB) one. In addition, the distribution of genotypes in the controls was consistent with HWE in all studies, except six studies (P < 0.05).
Quantitative synthesis
The 326Cys allele frequencies in controls of different ethnicities were calculated. The frequency of the 326Cys allele was 40.70 % (95 % CI = 36.05–45.34 %) among Asian controls, which was significantly higher than that of Caucasian controls (20.95 %; 95 % CI = 19.06–22.84 %, P < 0.001).
We carried out a meta-analysis of the hOGG1 Ser326Cys polymorphism overall and in subgroups according to cancer types, ethnic groups, and source of controls under various genetic models (Table 2). Overall, we found that the hOGG1 Ser326Cys polymorphism was significantly associated with the risk of digestive system cancers (Cys/Cys vs. Ser/Ser: OR = 1.17, 95 % CI = 1.00–1.35, P < 0.001; Cys/Cys vs. Cys/Ser + Ser/Ser: OR = 1.14, 95 % CI = 1.00–1.29, P < 0.001; Table 2, Fig. 1).
The forest plot of the homozygote and recessive model. a Cys/Cys vs. Ser/Ser b Cys/Cys vs. Cys/Ser + Ser/Ser. The squares and horizontal lines correspond to the study-specific OR and 95 % CI. The area of the squares reflects the study specific weight (inverse of the variance). The diamond represents the pooled OR and 95 % CI
In subgroup analyses by cancer types, we found that the hOGG1 Ser326Cys polymorphism was significantly associated with hepatocellular cancer (Cys/Cys vs. Ser/Ser: OR = 1.49, 95 % CI = 1.07–2.09, P < 0.001; Table 2) and others in one model (Cys/Cys vs. Cys/Ser + Ser/Ser: OR = 1.51, 95 % CI = 1.03–2.20, P = 0.35; Table 2), but not with gallbladder, gastric, esophageal, and pancreatic cancer. In addition, we found that the hOGG1 Ser326Cys polymorphism was marginally associated with the risk of colorectal cancer (Cys/Cys + Cys/Ser vs. Ser/Ser: OR = 1.17, 95 % CI = 1.00 (0.999)–1.37, P < 0.001; Table 2). However, we found that hOGG1 Ser326Cys polymorphism could decrease the risk with oral cancer (Cys/Cys vs. Ser/Ser: OR = 0.67, 95 % CI = 0.49–0.91, P = 0.381; Ser/Ser vs. Cys/Cys: OR = 0.72, 95 % CI = 0.55–0.94; Table 2).In subgroup analyses by ethnicities, we did not found that the hOGG1 Ser326Cys polymorphism was associated with overall cancer risk in Asian population and Caucasian population. When stratified in source of control, we found that the hOGG1 Ser326Cys polymorphism was associated with digestive cancer risk in PB controls (Cys/Cys vs. Ser/Ser: OR = 1.25, 95 % CI = 1.02–1.53, P = 0.001; Cys/Cys vs. Cys/Ser + Ser/Ser: OR = 1.18, 95 % CI = 1.00–1.39, P = 0.018; Table 2), but not in HB controls group.
Test of heterogeneity
The heterogeneity was reckoned between each of the studies using the Q test. Overall, the significant heterogeneity was found (Cys/Cys vs. Ser/Ser: pheterogeneity < 0.001; Cys/ Ser vs. Ser/Ser: pheterogeneity < 0.001; Cys/Cys + Cys/Ser vs. Ser/Ser: pheterogeneity < 0.001; Cys/Cys vs. Cys/Ser + Ser/Ser: pheterogeneity < 0.001). In stratified analyses by cancer types, we did not find the significant heterogeneity for esophageal cancer and oral cancer in all models (esophageal cancer: Cys/Cys vs. Ser/Ser: pheterogeneity = 0.128; Cys/ Ser vs. Ser/Ser: pheterogeneity = 0.057; Cys/Cys + Cys/Ser vs. Ser/Ser: pheterogeneity = 0.069; Cys/Cys vs. Cys/ Ser + Ser/Ser: pheterogeneity = 0.058; oral cancer: Cys/Cys vs. Ser/Ser: pheterogeneity = 0.381; Cys/ Ser vs. Ser/Ser: pheterogeneity = 0.925; Cys/Cys + Cys/Ser vs. Ser/Ser: pheterogeneity = 0.650; Cys/Cys vs. Cys/Ser + Ser/Ser: pheterogeneity = 0.427). Then, we assessed the source of heterogeneity for dominant model (Cys/Cys vs. Cys/Ser + Ser/Ser) by cancer type, ethnicity, and source of controls. As a result, cancer type (x 2 = 17.75, df = 7, P = 0.013) and source of controls (x 2 = 5.63, df = 1, P = 0.017), but not ethnicity (x 2 = 0.23, df = 1, P = 0.631) were found to contribute to substantial heterogeneity. However, we did find the source of heterogeneity in meta-regression from the three covariates.
Sensitivity analysis
In the sensitivity analysis, the influence of each study on the pooled OR was examined by repeating the meta-analysis while omitting each study one at a time. This procedure confirmed the stability of the overall result (data not shown). Moreover, when we omitted the six studies that is not consistent with HWE, the final result was almost the same with the former one.
Publication bias
Begg’s funnel plot and Egger’s test were conducted to assess the publication bias of the literatures. The shape of funnel plots did not reveal any evidence of funnel plot asymmetry. Egger’s test further provided statistical evidence of funnel plot symmetry. The Egger’s test also shows that there are no publication bias in all the four models (Cys/Cys + Cys/Ser vs. Ser/Ser: P = 0.545; Fig. 2).
Discussion
Digestive system cancer is a kind of severe cancer type, which seriously affected people’s life and health. Among them, colorectal, gastric, liver, esophagus, and oral cavity cancers ranked the first ten cancers of the most estimated new cases in men. In women, colorectal, gastric, and liver cancers were placed in the first ten cancers. In addition, liver, gastric, colorectal, and esophagus cancer were the leading cause of cancer death with 1,539,400 estimated deaths in men. In women, colorectal, gastric, liver, esophagus, and pancreatic cancers ranked ahead in all cancers with 1,037,900 estimated deaths [69].
The presence of 8-oxodG residues, one of the most abundant oxidative products of cellular DNA, leads to GC/TA transversions since it preferentially pairs with adenine instead of cytosine during DNA replication [70–72]. An increase in 8-oxodG in DNA can contribute to the incidence of cancer risk [73]. hOGG1, an important DNA repair enzyme involved in BER pathway, is responsible for repairing 8-OHdG lesions [13, 74]. If hOGG1 could not function effectively, the DNA damage could be left unrepaired, leading to gene mutations or carcinogenesis. Codon 326 polymorphism (Ser326Cys, rs1052133) in hOGG1 gene was the most studied polymorphism. It is located in the 1a-specific exon7 of hOGG1 gene, resulting in an amino acid substitution of serine (Ser) with cysteine (Cys) at codon 326, which has been reported to affect the hOGG1 function [20] and to be associated with cancer susceptibility [75].
The hOGG1 has been studied extensively on its relationship with different cancer types of digestive system, such as pancreatic, gallbladder, gastric, colorectal, esophageal, and so on. Previous conclusions of numerous studies on the association between the hOGG1 Ser326Cys polymorphism and digestive system cancer risk remain conflicting and contradictory. Hence, this meta-analysis was needed to provide a quantitative approach for combining the different results.
The meta-analysis included 12,073 cancer cases and 19,557 controls. In the analysis, we found that hOGG1 Ser326Cys polymorphism was associated with digestive system cancers. This result is consistent with Wang’s meta-analysis of the whole cancers [76]. However, certain publication bias exists in the homozygote and recessive models so that the strength of the association lacks some convincing evidence.
It is well-known that digestive system cancers are intimately associated with inflammation reaction. The hepatitis virus and Helicobacter pylori infection are major causes of hepatocellular cancer and gastric cancer, respectively, and colitis can contribute to the carcinogenesis of colorectal cancer. Inflammation is associated with the release of large amounts of ROS [77], leading to oxidation of nucleic acids, proteins, and lipids [78, 79]. In addition, exposure to smoking, heave alcohol drinking, and unhealthy consumption could be the contributors to the risk of digestive system cancer, which could lead to oxidative stress or weak the antioxidative activity [2, 3, 5]. Exposure to smoking produce major classes of carcinogenic and DNA adducts-productive compounds, polycyclic aromatic hydrocarbons (PAHs), aromatic amines, and heterocyclic amines (HCA), involving ROS generation and oxidative DNA damage [1, 80]. Fresh fruits and vegetables contain micronutrients such as vitamins A, C, and E and β-carotene, which could exert antioxidative activities, scavenge free radicals, and prevent DNA damage, but fat, meat, and alcohol were the ROS-producing food [81–83]. So, the unhealthy diet could induce the micronutrient deficiency, resulting in poor cellular antioxidant status and more ROS generation.
The hOGG1 encodes a DNA glycosylase that is thought to be involved in BER of oxidatively damaged DNA [84], and it could catalyze the cleavage of the glycosylic bond between the modified base and the sugar moiety, leaving an abasic apurinic/apyrimidinic site in DNA. The resulting apurinic/apyrimidinic site is then incised, and the repair is completed by successive actions of a phosphodiesterase, a DNA polymerase, and a DNA ligase [85–87]. Due to the important roles of hOGG1 in DNA repair, it is biologically plausible that hOGG1 Ser326Cys polymorphism may modulate the risk of digestive system cancer, which was confirmed by our data.
In the subgroup analysis by cancer types, we found the hOGG1 Ser326Cys polymorphism has increased the risk of hepatocellular cancer and other cancers, but the results were significant in only one model. In addition, we found marginal significance with colorectal cancer risk. Epidemiology and clinical studies demonstrated that the major risk factors for hepatocellular carcinoma include alcoholism, hepatitis B and C, and liver cirrhosis [88]. Chronic hepatic inflammation caused by hepatitis and exposure to alcohol and tobacco stimulates the generation of ROS causing DNA damage [89–91]. In addition, chronic intestinal inflammation is a known risk factor for developing colorectal cancer [92], and the smoking, alcohol, and low intake of micronutrition could induce DNA damage through oxidative stress [93]. If the hOGG1 could not work properly due to the sequence variants, the DNA damage could silence suppressor genes and active oncogenes, which lead to carcinogenesis. However, the inverse effect existed in oral cancer. There may be some reasons. Firstly, the type of pathology is mainly squamous cancer in oral cancer. While in other digestive cancer type, adenocarcinoma occupied for most of the pathological types. The differentiated biological genesis may lead to the variant results for the hOGG1 polymorphism. Secondly, the number of studies on oral cancer is scary, which may induce some bias for the results. The conclusion should be confirmed further by the larger data. In the stratified analysis by source of controls, we found that hOGG1 Ser326Cys polymorphism could increase the risk of digestive system cancer in PB control group, but we did not find the association in HB control group. This may be because most of the controls in the hospital are somehow unhealthy people, thus affecting the results. When stratifying the ethnicities, we did not find any relationship with the risk of digestive system cancer in both Asian population and Caucasian population.
Unfortunately, the publication bias existed in our analysis. We have searched for or contacted the authors for the unpublished data to ameliorate the effect of publication bias on the results of a meta-analysis. However, these data were not suitable for this meta-analysis. Therefore, the data in our analysis need to be validated by further larger studies.
Several limitations of the meta-analysis should be addressed. First, limited data restricted our evaluation on potential gene–gene interaction. Second, there was not enough data on African population in this meta-analysis. Third, our results exist publication bias, which weak the convincing degree. Forth, some cancer types have limited sample size. In order to provide a more precise estimation, well-designed studies are warranted in the future.
In summary, this meta-analysis indicated that hOGG1 Ser326Cys polymorphism may increase the susceptibility of digestive system cancers, especially in hepatocellular cancer and maybe in colorectal cancer, but the polymorphism can decrease the risk of oral cancer. This SNP may considerably act as a candidate of biomarker for cancer screening, diagnosis, and therapy in the future. Due to the limitations, further well-designed studies with large sample size in diverse ethnic populations, more types of digestive system cancers were warranted to confirm our findings.
References
Barrowman JA, Rahman A, Lindstrom MB, Borgstrom B. Intestinal absorption and metabolism of hydrocarbons. Prog Lipid Res. 1989;28:189–203.
Bingham SA, Hughes R, Cross AJ. Effect of white versus red meat on endogenous N-nitrosation in the human colon and further evidence of a dose response. J Nutr. 2002;132:3522S–5S.
Knize MG, Salmon CP, Pais P, Felton JS. Food heating and the formation of heterocyclic aromatic amine and polycyclic aromatic hydrocarbon mutagens/carcinogens. Adv Exp Med Biol. 1999;459:179–93.
Kobayashi M, Tsubono Y, Sasazuki S, Sasaki S, Tsugane S. Vegetables, fruit and risk of gastric cancer in Japan: a 10-year follow-up of the JPHC Study Cohort I. Int J Cancer. 2002;102:39–44.
Levi F, Pasche C, La Vecchia C, Lucchini F, Franceschi S. Food groups and colorectal cancer risk. Br J Cancer. 1999;79:1283–7.
Floyd RA. The role of 8-hydroxyguanine in carcinogenesis. Carcinogenesis. 1990;11:1447–50.
Loft S, Deng XS, Tuo J, Wellejus A, Sorensen M, Poulsen HE. Experimental study of oxidative DNA damage. Free Radic Res. 1998;29:525–39.
Marnett LJ. Oxyradicals and DNA damage. Carcinogenesis. 2000;21:361–70.
Jaruga P, Zastawny TH, Skokowski J, Dizdaroglu M, Olinski R. Oxidative DNA base damage and antioxidant enzyme activities in human lung cancer. FEBS Lett. 1994;341:59–64.
Roldan-Arjona T, Wei YF, Carter KC, Klungland A, Anselmino C, Wang RP, et al. Molecular cloning and functional expression of a human cDNA encoding the antimutator enzyme 8-hydroxyguanine-DNA glycosylase. Proc Natl Acad Sci U S A. 1997;94:8016–20.
Wood RD, Mitchell M, Sgouros J, Lindahl T. Human DNA repair genes. Science. 2001;291:1284–9.
Chatterjee A, Mambo E, Zhang Y, Deweese T, Sidransky D. Targeting of mutant hogg1 in mammalian mitochondria and nucleus: effect on cellular survival upon oxidative stress. BMC Cancer. 2006;6:235.
Elahi A, Zheng Z, Park J, Eyring K, McCaffrey T, Lazarus P. The human OGG1 DNA repair enzyme and its association with orolaryngeal cancer risk. Carcinogenesis. 2002;23:1229–34.
Sakamoto T, Higaki Y, Hara M, Ichiba M, Horita M, Mizuta T, et al. hOGG1 Ser326Cys polymorphism and risk of hepatocellular carcinoma among Japanese. J Epidemiol. 2006;16:233–9.
Speina E, Arczewska KD, Gackowski D, Zielinska M, Siomek A, Kowalewski J, et al. Contribution of hMTH1 to the maintenance of 8-oxoguanine levels in lung DNA of non-small-cell lung cancer patients. J Natl Cancer Inst. 2005;97:384–95.
Poplawski T, Arabski M, Kozirowska D, Blasinska-Morawiec M, Morawiec Z, Morawiec-Bajda A, et al. DNA damage and repair in gastric cancer—a correlation with the hOGG1 and RAD51 genes polymorphisms. Mutat Res. 2006;601:83–91.
Park HW, Kim IJ, Kang HC, Jang SG, Ahn SA, Lee JS, et al. The hOGG1 Ser326Cys polymorphism is not associated with colorectal cancer risk. J Epidemiol. 2007;17:156–60.
Radicella JP, Dherin C, Desmaze C, Fox MS, Boiteux S. Cloning and characterization of hOGG1, a human homolog of the OGG1 gene of Saccharomyces cerevisiae. Proc Natl Acad Sci U S A. 1997;94:8010–5.
Aburatani H, Hippo Y, Ishida T, Takashima R, Matsuba C, Kodama T, et al. Cloning and characterization of mammalian 8-hydroxyguanine-specific DNA glycosylase/apurinic, apyrimidinic lyase, a functional mutM homologue. Cancer Res. 1997;57:2151–6.
Kohno T, Shinmura K, Tosaka M, Tani M, Kim SR, Sugimura H, et al. Genetic polymorphisms and alternative splicing of the hOGG1 gene, that is involved in the repair of 8-hydroxyguanine in damaged DNA. Oncogene. 1998;16:3219–25.
Li D, Suzuki H, Liu B, Morris J, Liu J, Okazaki T, et al. DNA repair gene polymorphisms and risk of pancreatic cancer. Clin Cancer Res. 2009;15:740–6.
McWilliams RR, Bamlet WR, Cunningham JM, Goode EL, de Andrade M, Boardman LA, et al. Polymorphisms in DNA repair genes, smoking, and pancreatic adenocarcinoma risk. Cancer Res. 2008;68:4928–35.
Jiao X, Huang J, Wu S, Lv M, Hu Y, Jianfu S. X, Luo C, Ce B. hOGG1 Ser326Cys polymorphism and susceptibility to gallbladder cancer in a Chinese population. Int J Cancer. 2007;121:501–5.
Srivastava A, Srivastava K, Pandey SN, Choudhuri G, Mittal B. Single-nucleotide polymorphisms of DNA repair genes OGG1 and XRCC1: association with gallbladder cancer in North Indian population. Ann Surg Oncol. 2009;16:1695–703.
Srivastava K, Srivastava A, Mittal B. Polymorphisms in ERCC2, MSH2, and OGG1 DNA repair genes and gallbladder cancer risk in a population of Northern India. Cancer. 2010;116:3160–9.
Huang WY, Gao YT, Rashid A, Sakoda LC, Deng J, Shen MC, et al. Selected base excision repair gene polymorphisms and susceptibility to biliary tract cancer and biliary stones: a population-based case–control study in China. Carcinogenesis. 2008;29:100–5.
Canbay E, Agachan B, Gulluoglu M, Isbir T, Balik E, Yamaner S, et al. Possible associations of APE1 polymorphism with susceptibility and HOGG1 polymorphism with prognosis in gastric cancer. Anticancer Res. 2010;30:1359–64.
Capella G, Pera G, Sala N, Agudo A, Rico F, Del GG, et al. DNA repair polymorphisms and the risk of stomach adenocarcinoma and severe chronic gastritis in the EPIC-EURGAST study. Int J Epidemiol. 2008;37:1316–25.
Engin AB, Karahalil B, Engin A, Karakaya AE. DNA repair enzyme polymorphisms and oxidative stress in a Turkish population with gastric carcinoma. Mol Biol Rep. 2011;38:5379–86.
Farinati F, Cardin R, Bortolami M, Nitti D, Basso D, de Bernard M, et al. Oxidative DNA damage in gastric cancer: CagA status and OGG1 gene polymorphism. Int J Cancer. 2008;123:51–5.
Hanaoka T, Sugimura H, Nagura K, Ihara M, Li XJ, Hamada GS, et al. hOGG1 exon7 polymorphism and gastric cancer in case–control studies of Japanese Brazilians and non-Japanese Brazilians. Cancer Lett. 2001;170:53–61.
Liu X, Xiao N, Guo W, Wu Y, Cai Z, He Q, et al. The hOGG1 gene 5′-UTR variant c.-53G > C contributes to the risk of gastric cancer but not colorectal cancer in the Chinese population: the functional variation of hOGG1 for gastric cancer risk. J Cancer Res Clin Oncol. 2011;137:1477–85.
Malik MA, Zargar SA, Mittal B. Lack of influence of DNA repair gene OGG1 codon 326 polymorphisms of gastric cancer risk in the Kashmir valley. Asian Pac J Cancer Prev. 2010;11:165–8.
Palli D, Polidoro S, D’Errico M, Saieva C, Guarrera S, Calcagnile AS, et al. Polymorphic DNA repair and metabolic genes: a multigenic study on gastric cancer. Mutagenesis. 2010;25:569–75.
Sun LM, Shang Y, Zeng YM, Deng YY, Cheng JF. HOGG1 polymorphism in atrophic gastritis and gastric cancer after Helicobacter pylori eradication. World J Gastroenterol. 2010;16:4476–82.
Takezaki T, Gao CM, Wu JZ, Li ZY, Wang JD, Ding JH, et al. hOGG1 Ser(326)Cys polymorphism and modification by environmental factors of stomach cancer risk in Chinese. Int J Cancer. 2002;99:624–7.
Tsukino H, Hanaoka T, Otani T, Iwasaki M, Kobayashi M, Hara M, et al. hOGG1 Ser326Cys polymorphism, interaction with environmental exposures, and gastric cancer risk in Japanese populations. Cancer Sci. 2004;95:977–83.
Shinmura K, Kohno T, Kasai H, Koda K, Sugimura H, Yokota J. Infrequent mutations of the hOGG1 gene, that is involved in the excision of 8-hydroxyguanine in damaged DNA, in human gastric cancer. Jpn J Cancer Res. 1998;89:825–8.
Brevik A, Joshi AD, Corral R, Onland-Moret NC, Siegmund KD, Le Marchand L, et al. Polymorphisms in base excision repair genes as colorectal cancer risk factors and modifiers of the effect of diets high in red meat. Cancer Epidemiol Biomarkers Prev. 2010;19:3167–73.
Canbay E, Cakmakoglu B, Zeybek U, Sozen S, Cacina C, Gulluoglu M, et al. Association of APE1 and hOGG1 polymorphisms with colorectal cancer risk in a Turkish population. Curr Med Res Opin. 2011;27:1295–302.
Curtin K, Samowitz WS, Wolff RK, Ulrich CM, Caan BJ, Potter JD, et al. Assessing tumor mutations to gain insight into base excision repair sequence polymorphisms and smoking in colon cancer. Cancer Epidemiol Biomarkers Prev. 2009;18:3384–8.
Engin AB, Karahalil B, Engin A, Karakaya AE. Oxidative stress, Helicobacter pylori, and OGG1 Ser326Cys, XPC Lys939Gln, and XPD Lys751Gln polymorphisms in a Turkish population with colorectal carcinoma. Genet Test Mol Biomarkers. 2010;14:559–64.
Hansen R, Saebo M, Skjelbred CF, Nexo BA, Hagen PC, Bock G, et al. GPX Pro198Leu and OGG1 Ser326Cys polymorphisms and risk of development of colorectal adenomas and colorectal cancer. Cancer Lett. 2005;229:85–91.
Hansen RD, Krath BN, Frederiksen K, Tjonneland A, Overvad K, Roswall N, et al. GPX1 Pro(198)Leu polymorphism, erythrocyte GPX activity, interaction with alcohol consumption and smoking, and risk of colorectal cancer. Mutat Res. 2009;664:13–9.
Kasahara M, Osawa K, Yoshida K, Miyaishi A, Osawa Y, Inoue N, et al. Association of MUTYH Gln324His and APEX1 Asp148Glu with colorectal cancer and smoking in a Japanese population. J Exp Clin Cancer Res. 2008;27:49.
Kim JI, Park YJ, Kim KH, Kim JI, Song BJ, Lee MS, et al. hOGG1 Ser326Cys polymorphism modifies the significance of the environmental risk factor for colon cancer. World J Gastroenterol. 2003;9:956–60.
Moreno V, Gemignani F, Landi S, Gioia-Patricola L, Chabrier A, Blanco I, et al. Polymorphisms in genes of nucleotide and base excision repair: risk and prognosis of colorectal cancer. Clin Cancer Res. 2006;12:2101–8.
Obtulowicz T, Swoboda M, Speina E, Gackowski D, Rozalski R, Siomek A, et al. Oxidative stress and 8-oxoguanine repair are enhanced in colon adenoma and carcinoma patients. Mutagenesis. 2010;25:463–71.
Sliwinski T, Krupa R, Wisniewska-Jarosinska M, Pawlowska E, Lech J, Chojnacki J, et al. Common polymorphisms in the XPD and hOGG1 genes are not associated with the risk of colorectal cancer in a Polish population. Tohoku J Exp Med. 2009;218:185–91.
Stern MC, Conti DV, Siegmund KD, Corral R, Yuan JM, Koh WP, et al. DNA repair single-nucleotide polymorphisms in colorectal cancer and their role as modifiers of the effect of cigarette smoking and alcohol in the Singapore Chinese Health Study. Cancer Epidemiol Biomarkers Prev. 2007;16:2363–72.
Pardini B, Naccarati A, Novotny J, Smerhovsky Z, Vodickova L, Polakova V, et al. DNA repair genetic polymorphisms and risk of colorectal cancer in the Czech Republic. Mutat Res. 2008;638:146–53.
Ferguson HR, Wild CP, Anderson LA, Murphy SJ, Johnston BT, Murray LJ, et al. No association between hOGG1, XRCC1, and XPD polymorphisms and risk of reflux esophagitis, Barrett’s esophagus, or esophageal adenocarcinoma: results from the factors influencing the Barrett’s adenocarcinoma relationship case–control study. Cancer Epidemiol Biomarkers Prev. 2008;17:736–9.
Hao B, Wang H, Zhou K, Li Y, Chen X, Zhou G, et al. Identification of genetic variants in base excision repair pathway and their associations with risk of esophageal squamous cell carcinoma. Cancer Res. 2004;64:4378–84.
Lagadu S, Lechevrel M, Sichel F, Breton J, Pottier D, Couderc R, et al. 8-oxo-7,8-dihydro-2'-deoxyguanosine as a biomarker of oxidative damage in oesophageal cancer patients: lack of association with antioxidant vitamins and polymorphism of hOGG1 and GST. J Exp Clin Cancer Res. 2010;29:157.
Li QD, Li H, Wang MS, Diao TY, Zhou ZY, Fang QX, et al. Multi-susceptibility genes associated with the risk of the development stages of esophageal squamous cell cancer in Feicheng County. BMC Gastroenterol. 2011;11:74.
Upadhyay R, Malik MA, Zargar SA, Mittal B. OGG1 Ser326Cys polymorphism and susceptibility to esophageal cancer in low and high at-risk populations of northern India. J Gastrointest Cancer. 2010;41:110–5.
Xing DY, Tan W, Song N, Lin DX. Ser326Cys polymorphism in hOGG1 gene and risk of esophageal cancer in a Chinese population. Int J Cancer. 2001;95:140–3.
Tse D, Zhai R, Zhou W, Heist RS, Asomaning K, Su L, et al. Polymorphisms of the NER pathway genes, ERCC1 and XPD are associated with esophageal adenocarcinoma risk. Cancer Causes Control. 2008;19:1077–83.
Tsou YA, Hua CH, Tseng HC, Hsu CF, Tsai CW, Sun SS, et al. The joint effect of hOGG1 single nucleotide polymorphism and betel quid chewing on oral cancer in Taiwan. Anticancer Res. 2010;30:4205–8.
Gorgens H, Muller A, Kruger S, Kuhlisch E, Konig IR, Ziegler A, et al. Analysis of the base excision repair genes MTH1, OGG1 and MUTYH in patients with squamous oral carcinomas. Oral Oncol. 2007;43:791–5.
Yuan T, Wei J, Luo J, Liu M, Deng S, Chen P. Polymorphisms of base-excision repair genes hOGG1 326cys and XRCC1 280His increase hepatocellular carcinoma risk. Dig Dis Sci. 2012;57:2451–7.
Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127:820–6.
Berman NG, Parker RA. Meta-analysis: neither quick nor easy. BMC Med Res Methodol. 2002;2:10.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
MANTEL N, HAENSZEL W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48.
Hayashino Y, Noguchi Y, Fukui T. Systematic evaluation and comparison of statistical tests for publication bias. J Epidemiol. 2005;15:235–43.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295:676–80.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Ames BN. Endogenous oxidative DNA damage, aging, and cancer. Free Radic Res Commun. 1989;7:121–8.
Shibutani S, Takeshita M, Grollman AP. Insertion of specific bases during DNA synthesis past the oxidation-damaged base 8-oxodG. Nature. 1991;349:431–4.
Kasai H. Analysis of a form of oxidative DNA damage, 8-hydroxy-2'-deoxyguanosine, as a marker of cellular oxidative stress during carcinogenesis. Mutat Res. 1997;387:147–63.
Greim H, Csanady G, Filser JG, Kreuzer P, Schwarz L, Wolff T, et al. Biomarkers as tools in human health risk assessment. Clin Chem. 1995;41:1804–8.
Nishioka K, Ohtsubo T, Oda H, Fujiwara T, Kang D, Sugimachi K, et al. Expression and differential intracellular localization of two major forms of human 8-oxoguanine DNA glycosylase encoded by alternatively spliced OGG1 mRNAs. Mol Biol Cell. 1999;10:1637–52.
Weiss JM, Goode EL, Ladiges WC, Ulrich CM. Polymorphic variation in hOGG1 and risk of cancer: a review of the functional and epidemiologic literature. Mol Carcinog. 2005;42:127–41.
Wang W, Wang M, Chen Y, Zhang Z, Wang S, Xu M, et al. The hOGG1 Ser326Cys polymorphism contributes to cancer susceptibility: evidence from 83 case–control studies. Mutagenesis. 2012;27:329–36.
Dizdaroglu M, Olinski R, Doroshow JH, Akman SA. Modification of DNA bases in chromatin of intact target human cells by activated human polymorphonuclear leukocytes. Cancer Res. 1993;53:1269–72.
Obst B, Wagner S, Sewing KF, Beil W. Helicobacter pylori causes DNA damage in gastric epithelial cells. Carcinogenesis. 2000;21:1111–5.
Bagchi D, McGinn TR, Ye X, Bagchi M, Krohn RL, Chatterjee A, et al. Helicobacter pylori-induced oxidative stress and DNA damage in a primary culture of human gastric mucosal cells. Dig Dis Sci. 2002;47:1405–12.
Church DF, Pryor WA. Free-radical chemistry of cigarette smoke and its toxicological implications. Environ Health Perspect. 1985;64:111–26.
Chen J, Geissler C, Parpia B, Li J, Campbell TC. Antioxidant status and cancer mortality in China. Int J Epidemiol. 1992;21:625–35.
Cheng KK, Day NE. Nutrition and esophageal cancer. Cancer Causes Control. 1996;7:33–40.
Glei M, Latunde-Dada GO, Klinder A, Becker TW, Hermann U, Voigt K, et al. Iron-overload induces oxidative DNA damage in the human colon carcinoma cell line HT29 clone 19A. Mutat Res. 2002;519:151–61.
Boiteux S, Radicella JP. The human OGG1 gene: structure, functions, and its implication in the process of carcinogenesis. Arch Biochem Biophys. 2000;377:1–8.
Dianov GL, Souza-Pinto N, Nyaga SG, Thybo T, Stevnsner T, Bohr VA. Base excision repair in nuclear and mitochondrial DNA. Prog Nucleic Acid Res Mol Biol. 2001;68:285–97.
Karahalil B, Hogue BA, de Souza-Pinto NC, Bohr VA. Base excision repair capacity in mitochondria and nuclei: tissue-specific variations. FASEB J. 2002;16:1895–902.
Gu D, Wang M, Zhang Z, Chen J. Lack of association between the hOGG1 Ser326Cys polymorphism and breast cancer risk: evidence from 11 case–control studies. Breast Cancer Res Treat. 2010;122:527–31.
Niwa Y, Matsuo K, Ito H, Hirose K, Tajima K, Nakanishi T, et al. Association of XRCC1 Arg399Gln and OGG1 Ser326Cys polymorphisms with the risk of cervical cancer in Japanese subjects. Gynecol Oncol. 2005;99:43–9.
Albano E. Free radical mechanisms in immune reactions associated with alcoholic liver disease. Free Radic Biol Med. 2002;32:110–4.
Shimoda R, Nagashima M, Sakamoto M, Yamaguchi N, Hirohashi S, Yokota J, et al. Increased formation of oxidative DNA damage, 8-hydroxydeoxyguanosine, in human livers with chronic hepatitis. Cancer Res. 1994;54:3171–2.
Asami S, Hirano T, Yamaguchi R, Tomioka Y, Itoh H, Kasai H. Increase of a type of oxidative DNA damage, 8-hydroxyguanine, and its repair activity in human leukocytes by cigarette smoking. Cancer Res. 1996;56:2546–9.
Shacter E,Weitzman SA. Chronic inflammation and cancer. Oncology (Williston Park). 2002;16:217–26, 229; discussion 230–2
Block G, Patterson B, Subar A. Fruit, vegetables, and cancer prevention: a review of the epidemiological evidence. Nutr Cancer. 1992;18:1–29.
Acknowledgments
This manuscript is supported by the National Basic Research Program of China (973program) No. 2012CB9333004.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Yang Wang is the first author
Rights and permissions
About this article
Cite this article
Wang, Y., Gao, X., Wei, F. et al. The hOGG1 Ser326Cys polymorphism contributes to digestive system cancer susceptibility: evidence from 48 case–control studies. Tumor Biol. 36, 1029–1038 (2015). https://doi.org/10.1007/s13277-014-2710-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2710-6