Abstract
Backgrounds
The direct and indirect interactions between multiple myeloma (MM) cells and bone marrow mesenchymal stromal cells (MSCs) play crucial roles in the formation of the bone marrow environment, disease progression, and drug resistance development. However, it remains unclear how MM cells and MSCs individually influence each other to induce these phenomena.
Objective
In this study, we focused on observing changes in MSCs induced by MM cells. Changes in MSCs due to exposure to MM cells were observed by assessing cell proliferation, apoptosis, cell cycle, and morphology. Furthermore, the unique abilities of MSCs were confirmed through differentiation potential and MSC marker expression, along with the demonstration of senescence. Gene profiling was performed to elucidate the mechanisms underlying these changes.
Results
Co-culturing MM cells with MSCs did not alter the morphology or proliferation of MSCs but increased apoptosis. As apoptosis increased, damaged deoxyribonucleic acid (DNA) was repaired, leading to the activation of the cell cycle with an increase in the S phase, resulting in no significant changes in cell proliferation and morphology. Osteogenesis and adipogenesis generally decreased by co-culturing with MM cells, and senescence increased. Significant differences were observed in the expression of MSC marker genes. Gene profiling revealed changes in gene expression following osteogenic differentiation.
Conclusion
Based on these results, MSCs exposed to MM cells exhibited an increase in the S phase of the cell cycle, leading to the recovery of cells undergoing apoptosis. Osteogenesis and adipogenesis decreased, whereas senescence increased, suggesting that these changes were attributed to the overall MSC characteristics and genetic mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) represents the malignant end in the spectrum of plasma cell dyscrasias, characterized by the clonal expansion of terminally differentiated plasma cells in bone marrow (BM) (Landgren et al. 2009). Clinically overt MM stage is almost always preceded by a precursor stage called monoclonal gammopathy of undetermined significance, that is considered a benign stage of the clinical spectrum in which patients are asymptomatic and only have elevated levels of monoclonal immunoglobulins (M proteins) (Kumar et al. 2017). With disease progression, MM cells, M proteins, or cytokines produced by the malignant cells lead to a clinical stage manifested by organ damage, such as anemia, renal insufficiency, and bone injury, which requires treatment. Although advances in autologous stem cell transplantation and the introduction of novel agents in the past two decades have allowed remarkable survival improvements (Attal et al. 2017; McCarthy et al. 2017; Moreau et al. 2019), most patients eventually relapse during or after treatment, while some experience aggressive treatment-refractory progression, rendering MM an incurable disease (Moreau et al. 2021).
Extensive research in the past decade has revealed the highly immunosuppressive nature of the MM BM microenvironment (BMM) (Allegra et al. 2021; Diaz-Tejedor et al. 2021). Mesenchymal stem cells (MSCs) are the key compartment of specialized supporting cells in the formation of a tumor-favoring microenvironment that can differentiate into other non-immune cell types, such as osteoid cells, fibroblasts, and endothelial cells. These are also important constituents of BM stroma. Similar to other tumors, direct and indirect interactions between MM cells and BM-MSCs have been shown to play a crucial role in the formation of BMM, supporting MM development, disease progression, and drug resistance (Xu et al. 2018). The direct cell-to-cell contact between MM cells and BM-MSCs mediated by cell-adhesion molecules, such as very late antigen 4, very late antigen 5, CD44, leukocyte function-associated antigen 1, and intercellular adhesion molecule 1, is a well-known pathophysiology of MM, specifically related to the homing of malignant plasma cells to the BM (García-Sánchez et al. 2023). On the other hand, among many cellular interactions in BM, due to the wide variety of soluble and non-soluble factors secreted by MSCs the indirect crosstalk between these two cells through soluble cytokines has stronger impact on MM pathophysiology. Specifically, cytokine stromal cell-derived factor 1α, also known as CXCL12 produced by BM-MSCs, plays as a key factor in the communication between BM cells and MM cells during the first stages of BM colonization, and then many other factors, such as vascular endothelial growth factor, fibroblast growth factors, osteopontin, interleukin, tumor necrosis factor-α, and many more factors secreted by BM-MSCs and many other cell types in the BMM activate signaling pathways of onco-genesis, anti-apoptosis, pro-survival, and cell proliferation (García-Sánchez et al. 2023).
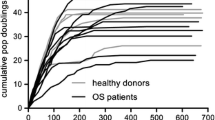
BM-MSCs from patients with MM are genetically and functionally different from MSCs of healthy populations. A distinctive genomic expression profile of genes coding for growth factors and osteogenesis-related factors, as well as senescence and cell-cycle-related genes has been observed in MM-MSCs as compared with those from normal donors (Berenstein et al. 2015; Guo et al. 2018; Mehdi et al. 2019; Corre et al. 2007; Garayoa et al. 2009). Several studies demonstrate that BM-MSCs of patients with MM have a distinctive phenotype in culture, featured by larger and uneven shape, decreased proliferative potential (Guo et al. 2018; Garderet et al. 2007; Choi et al. 2020; Andre et al. 2013), less differentiation potential for osteogenesis (Guo et al. 2018; Corre et al. 2007; Choi et al. 2020; Andre et al. 2013; Xu et al. 2012), increased senescence-associated beta-galactosidase activity (Guo et al. 2018; Mehdi et al. 2019; Choi et al. 2020), and increased senescence-associated secretory profile including IL-6, tumor-necrosis factor-alpha (TNF-a), and growth differentiation factor 15 (GDF-15) (Corre et al. 2007; Garderet et al. 2007; Arnulf et al. 2007).
However, owing to the complexity and heterogeneity of BMM in MM, it remains unclear whether these biological alterations of BM-MSCs in MM were first driven and influenced by MM cells or whether the intrinsic changes of MSCs were caused by other reasons such as aging (Xu et al. 2018). It is assumed that normal MSCs are influenced by MM cells to become MM-MSCs, which then interact with MM cells to facilitate MM cell survival and proliferation. We investigated whether MSCs are altered by MM cells to elucidate the mechanisms underlying such changes.
Materials and methods
Cell culture
We procured mesenchymal stromal cell (MSC) line HS-5 and MM cell lines RPMI-8226 and IM-9 from the cell bank at Seoul National University Hospital. HS-5 cells were cultured in Dulbecco's modified Eagle's medium (DMEM, Gibco, USA, Massachusetts) supplemented with 10% fetal bovine serum (FBS, Gibco) and 1% penicillin–streptomycin (P/S, Gibco). Multiple myeloma cell lines were maintained in RPMI1640 (Corning, USA, New York) supplemented with 10% FBS and 1% P/S.
Co-culture of multiple myeloma cell and mesenchymal stromal cells
HS-5 cells were initially seeded into 6-well plates (SPL Life Sciences, Korea) at a density of 2.5 × 105 cells per well. After 24 h, multiple myeloma cells were seeded into the same 6-well plates at a density of 5 × 105 cells per well. These cells were co-cultured for a period of 72 h and then harvested using trypsin 0.25% for subsequent experiments.
Cell viability, apoptosis, and cycle assay
Cells were harvested through trypsinization and suspended in Hanks' Balanced Salt Solution (Welgene, Korea) supplemented with 2% FBS (HF2). Subsequently, cells were prepared for assessments of cell count and viability (Luminex, USA, Texas), apoptosis (Annexin V and Dead Cell Kit, Luminex), and cell cycle (Luminex) using appropriate kits. Staining was conducted according to the manufacturer's instructions, and analysis was carried out utilizing the Guava Muse Cell Analyzer (Luminex).
Flow cytometry
Cells were harvested and suspended in 100 μL of HF2 solution. Subsequently, they were stained with specific markers. Markers include MSC positive CD105, CD73, CD90, CD44, and MSC negative HLA-DR, CD34, and CD19. Cells were stained for one hour and washed with HF2 solution. BD FACS CantoII (BD Biosciences, USA, New Jersey) was used to analyze stained cells by flow cytometry.
Cell senescence assay
Both control and co-culture group cells were harvested at 24 h, 48 h, and 72 h of culture for a cell senescence assay (Cell Signalling Technology, USA, Massachusetts). The assay was conducted using the manufacturer’s instructions.
Differentiation of MSCs
MSCs were harvested after 72 h of co-culture with MM cells and re-plated. After a 24-h stabilization period, cells were exposed to adipogenic media (StemPro™ Adipogenesis Differentiation Kit, Gibco) or osteogenic media. Adipogenic cells were periodically exposed to proliferation media for stabilization in between adipogenic media treatments. Osteogenic media consisted of DMEM supplemented with 10% FBS, 1% P/S, 100 nM dexamethasone, 5 mM β-glycerophosphate, and 50 μg/mL L-ascorbic acid. Differentiation medium is supplied for 7 days for each condition.
Oil Red O and ALP staining assay
Differentiated cells were subjected to ALP staining for osteogenic cells and Oil Red O staining for adipogenic cells. ALP (SIGMA FAST, BCiP/NBT, USA, Missouri) and Oil Red O (Merck, Germany) staining procedures were carried out following the manufacturer's instructions, and cell analysis was conducted using a light microscope.
RNA isolation
Total RNA was isolated using Trizol reagent (Invitrogen). RNA quality was assessed by Agilent TapeStation system (Agilent Technologies, Amstelveen, The Netherlands), and RNA quantification was performed using Qubit (Thermo Fisher Scientific Inc., USA).
Library preparation and sequencing
For control and test RNAs, the construction of library was performed using QuantSeq 3’ mRNA-Seq Library Prep Kit (Lexogen, Inc., Austria) according to the manufacturer’s instructions. In brief, each total RNA was prepared and an oligo-dT primer containing an Illumina-compatible sequence at its 5′ end was hybridized to the RNA and reverse transcription was performed. After degradation of the RNA template, second strand synthesis was initiated by a random primer containing an Illumina-compatible linker sequence at its 5′ end. The double-stranded library was purified using magnetic beads to remove all reaction components. The library was amplified to add the complete adapter sequences required for cluster generation. The finished library is purified from PCR components. High-throughput sequencing was performed as single-end 75 sequencing using NextSeq 550 (Illumina, Inc., USA).
Data analysis
QuantSeq 3′ mRNA-Seq reads were aligned using STAR (Dobin et al. 2013). STAR indices were either generated from genome assembly sequence or the representative transcript sequences for aligning to the genome and transcriptome. The alignment file was used for assembling transcripts, estimating their abundances, and detecting differential expression of genes. Differentially expressed genes were determined based on counts from unique and multiple alignments using coverage in HTSeq-count (Anders et al. 2015). The RC (Read Count) data were processed based on TMM + CPM normalization method using EdgeR within R (R development Core Team, 2020) using Bioconductor (Gentleman et al. 2004). Gene classification was based on searches done by DAVID (http://david.abcc.ncifcrf.gov/) and Medline databases (http://www.ncbi.nlm.nih.gov/). Data mining and graphic visualization were performed using ExDEGA (Ebiogen Inc., Korea).
Results
Establishment of an in vitro model for MM tumor microenvironment research
Understanding the tumor microenvironment in patients with MM is crucial for the development of treatments and the discovery of targeted therapies. In this regard, we aimed to observe the changes in normal MSCs induced by MM cells using a co-culture with the MM cell lines IM-9 and RPMI-8226, which are mesenchymal stromal cell lines (Fig. 1). Through the co-culture of MM cells and MSCs, we sought to replicate the tumor microenvironment of patients with MM.
Proliferation, apoptosis, and cell cycle due to co-culture of MM cells and MSCs
Following the co-culture of HS-5 cells with RPMI-8226 or IM-9, we observed cell morphology at 24 and 72 h. The results showed no significant changes in cell morphology during co-culturing or over time (Fig. 2A). After RPMI-8226 and IM-9 were co-cultivated with HS5, cell viability was measured. When HS-5 was cultured alone, it decreased slightly to 95%, and when RPMI-8226 and IM-9 were co-cultured, it decreased slightly to 88% and 91%. However, all of them showed high cell viability (Fig. 2B). However, apoptosis was significantly increased when co-cultured with RPMI-8226 and IM-9. In the case of RPMI-8226, it increased by approximately 3.5-fold, whereas for IM-9, it increased by approximately 2.5-fold (Fig. 2C). Cell cycle analysis did not show significant differences in the G0/G1 or G2/M phases due to co-culture; however, a significant increase was observed in the S phase, which corrects errors during DNA replication, suggesting ongoing cell cycle progression to repair damaged DNA (Fig. 2D). These results suggest that while MSCs may not be significantly affected by MM in terms of cell viability, a substantial number of cells undergo apoptosis, leading to continuous DNA replication in the cell cycle, especially during the S phase, to correct errors.
Observation of MSCs co-cultured with MM cells. A Observation of MSCs co-cultured with MM cells at 0, 24, and 72 h. Harvesting of MM cells and co-cultured MSCs at 72 h for analysis of cell viability (B), apoptosis (C), and cell cycle (D) (*P < 0.05, **P < 0.01, ***P < 0.001). MSC mesenchymal stromal cell, MM multiple myeloma
MSC senescence due to co-culture with MM cells
Senescence was assessed after co-culturing MSCs with RPMI-8226 and IM-9. Co-culturing with RPMI-8226 and IM-9 increased MSC senescence, with IM-9 showing senescence in most cells (Fig. 2A). Cells that entered senescence were counted and quantified graphically (Fig. 2B–D. These results indicate that MM cells promote MSC senescence (Fig. 3).
MSC differentiation due to co-culture with MM cells
MSCs co-cultured with MM cells were re-plated to induce osteogenesis and adipogenesis. Analysis of osteogenesis by ALP staining showed that co-culturing with RPMI-8226 and IM-9 significantly reduced ALP expression. However, when assessing adipogenesis using Oil Red O staining, no significant difference in adipogenesis was observed in the co-culture with RPMI-8226 and IM-9. These results indicate that co-culturing with MM cells affects osteogenesis but not adipogenesis (Fig. 4).
Changes in MSC differentiation capacity induced by co-culturing with MM cells. Co-cultured MSCs was induced for osteogenesis, and an ALP assay was performed (A). Adipogenesis was induced and Oil Red O staining was performed (B). MSC mesenchymal stromal cell, MM multiple myeloma, ALP alkaline phosphatase
Changes in MSC characterization due to co-culture with MM cells
To determine whether the observed changes in senescence and osteogenesis were due to alterations in MSC characteristics, we examined the expression of MSC markers. The confirmation of MSC marker expression is based on the results obtained from five separate co-culture experiments. CD73, CD90, CD105, and CD44 are positive markers of MSCs, whereas CD34, CD19, and HLA-DR are negative markers. Flow cytometry revealed that co-culturing with both RPMI-8226 and IM-9, led to decreased expression of the positive markers CD73, CD90, CD105, and CD144. The IM-9 co-culture showed significant differences in CD73, CD90, CD105, and CD144, while the RPMI-8226 co-culture exhibited decreased expression of all markers but showed significant differences only in CD73 and CD44. Conversely, the expression of the negative markers CD19 and HLA-DR increased significantly when co-cultured with RPMI-8226 and IM-9, while no difference was observed in CD34 expression. These results suggest that co-culturing with MM cells alters the characteristics of MSCs in the tumor microenvironment (Fig. 5).
Characterization of MM cells and co-cultured MSCs. The expression of MSC markers was examined after 72 h of co-culture with MM cells. The expression of positive and negative markers was determined using flow cytometry. (*P < 0.05, **P < 0.01, ***P < 0.001). MSC mesenchymal stromal cell, MM multiple myeloma
Gene profiling after osteogenesis of co-cultured MSCs with MM cells
To investigate the mechanism underlying the observed decrease in osteogenesis following co-culture with MM cells, gene profiling was performed. The heat map shows significant changes in gene expression after co-culturing with RPMI-8226 and IM-9 (Fig. 6A). Compared with normal MSCs, co-culture with IM-9 led to an increase in 126 genes and a downregulation of 211 genes. The genes with significant changes in expression included 48 upregulated and 26 downregulated genes. RPMI-8226 cells had 48 overexpressed and 80 underexpressed genes, with four genes showing significant differences in both overexpression and expression (Fig. 6B). Scatter plots (Fig. 6C) illustrate the changes in gene expression induced by co-culturing with MM cell lines. Notably, the expression of genes involved in growth arrest and DNA damage induction, such as GADD45A, increased significantly in RPMI-8226 and IM-9 co-cultures, as did genes such as IRF-1. This mediates the function of TH1 cells and HLA-B, which plays a crucial role in the immune response and provides instructions for protein synthesis. Furthermore, when co-cultured with MM cell lines and osteogenesis was induced, changes in gene expression related to angiogenesis, cell cycle, DNA repair, immune response, and inflammatory response were observed. The IM-9 coculture showed more significant changes in gene expression than the RPMI-8226 coculture (Table 1). These results suggest that co-culturing with MM cells leads to a decrease in the osteogenic capacity of MSCs, which is associated with changes in the expression of various genes.
Gene profiling changes in MM co-cultured MSCs induced by osteogenesis. mRNA sequencing was performed after coculturing with MM cells for osteogenesis. Overexpressed and underexpressed genes are represented using a heat map and dendrogram (A), and the gene distribution is shown as a scatter plot (C). On the left side of the Venn diagram, it represents overall gene expression, while on the right, it indicates only the significant genes. On the left side of the scatter plot, it compares the control and IM9, and on the right, it compares the control and RPMI8226. MSC mesenchymal stromal cell, MM multiple myeloma
Discussion
As a tumor microenvironment in hematological malignancies, MSCs have been recognized as important factors by several researchers (Pan et al. 2023; Plakhova et al. 2023; Vanegas et al. 2021; Agarwal et al. 2019), and studies on the interactions between MM cells and MSCs have been reported (Corre et al. 2007; Andre et al. 2013; Desantis et al. 2022). MM is also supported by the tumor microenvironment (TME), which consists of various cell types, such as autocrine signaling pathways, stromal cells, immune cells, and extracellular matrix components. The TME plays a crucial role in inducing proliferation and preventing cell death. Therefore, the interaction between MM cells and the TME is highly significant in MM progression, with MSCs known as key regulators within the MM TME (Forster et al. 2023). However, it remains unclear whether MSCs are fundamentally damaged by MM cells. In this study, we aimed to investigate whether MM cells cause damage to normal bone marrow by observing the interactions between MSCs and MM cells in co-culture.
Although co-culturing with MM cells did not result in significant differences in the morphology and viability of MSCs, apoptosis increased significantly. These results contrast with those of some studies that reported increased proliferation and no difference in apoptosis due to MM cells (Andre et al. 2013), but it is not clear whether these results were due to damaged MSCs in patients with MM or MSCs controlled by MM cells. Our results demonstrate that normal MSCs are influenced by MM cells, leading to an increase in apoptosis. Cell proliferation did not increase regardless of an increase in apoptosis could be due to an increased S phase in the cell cycle. During S phase, damaged DNA is repaired, leading to cell cycle activation and compensation for the damage caused by apoptosis. Overall, MM cells maintained the morphology and the number of MSCs.
A comparison of normal MSCs with those from patients with MM revealed differences in senescence, osteogenesis, and adipogenesis. These differences were explained by changes in various genes in patients with MM when analyzing gene profiling (Andre et al. 2013; Cao et al. 2022; Fernando et al. 2019). In this study, we aimed to investigate whether osteogenic failure in damaged MSCs exposed to MM cells was due to changes in specific genes. After exposing MM cells to MSCs and inducing osteogenesis, we aimed to confirm whether gene expression differences occurred due to the failure of osteogenesis. The results showed significant differences in the expression of various genes, and it was concluded that the decrease in osteogenesis was caused by changes in gene expression.
MSCs expressed both positive and negative markers. CD73, CD90, CD105, and CD44 are positive markers, whereas CD34, CD19, and HLA-DR are negative markers (Lovell-Badge et al. 2021). Some studies have reported changes in MSC marker expression due to co-culturing with hematopoietic malignancies; however, these results are also controversial (Flores-Figueroa et al. 2005; Kawano et al. 2023; Rathnayake et al. 2016; Corradi et al. 2018). In this study, co-culturing of MSCs and MM cells significantly altered the expression of MSC markers, and these changes were believed to result in a decrease in the unique potential of MSCs.
Changes in gene expression in normal MSCs and MSCs from patients with MM have been reported previously. The altered expression of genes, such as IL-6 and CD106, which are MM cell growth factors, as well as fibronectin, DKK1, IL-1β, and TNF-α, has been explained (Corre et al. 2007; Yaccoby et al. 2002; Wallace et al. 2001; Garderet et al. 2007). In this study, gene expression was analyzed after osteogenesis, and a significant increase was observed in the expression of GADD45A, a growth arrest- and DNA damage-inducing gene. Additionally, other genes showed differential expression, with more genes being underexpressed than overexpressed. This suggests that the decrease in osteogenesis may be due to the predominance of underexpressed genes related to angiogenesis, cell cycle, immune response, and inflammatory response. Although increased GADD45A expression may help repair DNA damage, it has limitations in the overall gene expression recovery.
In conclusion, we co-cultured MM cells and MSCs to investigate the impact of MM cells on the tumor microenvironment. The results showed that while MM cells did not significantly affect the viability of MSCs, apoptosis increased significantly, and there was a notable increase in the S phase of the cell cycle. Co-culture with MM cells decreased senescence, adipogenesis, and osteogenesis. When these changes were confirmed using MSC markers, the expression of positive markers decreased owing to co-culturing with MM cells, whereas the expression of negative markers increased. Furthermore, a clear decrease in osteogenesis was observed following co-culture with MM cells, which was attributed to changes in gene profiling. Overall, co-culture with MM cells not only altered the characteristics of MSCs but also lead to changes in senescence, osteogenesis, and adipogenesis, which are influenced by changes in gene expression.
The use of novel agents has improved the outcomes for MM patients. However, a significant issue remains as the majority of patients experience relapse and develop treatment resistance. To improve the efficacy of MM treatment, it is essential to accurately understand the interactions between MM cells and MSCs. Essentially, there is a need for further research to understand the interaction between MM cells and tumor microenvironment in order to develop treatments that can effectively prevent MM progression and relapse. In future research, we will investigate not only the effects of MM cells on MSCs, but also the process by which patient-derived MSCs influence HSCs from multiple perspectives. Through such diverse studies, elucidating the interaction between MM cells and MSCs can greatly contribute to the enhancement of MM treatments (Fig. 7).
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Agarwal P, Isringhausen S, Li H, Paterson AJ, He J et al (2019) Mesenchymal niche-specific expression of Cxcl12 controls quiescence of treatment-resistant leukemia stem cells. Cell Stem Cell 24(5):769-784.e6
Allegra A, Di Gioacchino M, Tonacci A, Petrarca C, Musolino C et al (2021) Multiple myeloma cell-derived exosomes: implications on tumorigenesis, diagnosis. Progn Ther Strat Cells 10(11):2865
Andre T, Meuleman N, Stamatopoulos B, De Bruyn C, Pieters K et al (2013) Evidences of early senescence in multiple myeloma bone marrow mesenchymal stromal cells. PLoS ONE 8(3):e59756
Arnulf B, Lecourt S, Soulier J, Ternaux B, Lacassagne MN et al (2007) Phenotypic and functional characterization of bone marrow mesenchymal stem cells derived from patients with multiple myeloma. Leukemia 21(1):158–163
Attal M, Lauwers-Cances V, Hulin C, Leleu X, Caillot D et al (2017) Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N Engl J Med 376(14):1311–1320
Berenstein R, Blau O, Nogai A, Waechter M, Slonova E et al (2015) Multiple myeloma cells alter the senescence phenotype of bone marrow mesenchymal stromal cells under participation of the DLK1-DIO3 genomic region. BMC Cancer 15:68
Cao YJ, Zheng YH, Li Q, Zheng J, Ma LT et al (2022) MSC senescence-related genes are associated with myeloma prognosis and lipid metabolism-mediated resistance to proteasome inhibitors. J Oncol 2022:4705654
Choi H, Kim Y, Kang D, Kwon A, Kim J et al (2020) Common and different alterations of bone marrow mesenchymal stromal cells in myelodysplastic syndrome and multiple myeloma. Cell Prolif 53(5):e12819
Corradi G, Baldazzi C, Očadlíková D, Marconi G, Parisi S et al (2018) Mesenchymal stromal cells from myelodysplastic and acute myeloid leukemia patients display in vitro reduced proliferative potential and similar capacity to support leukemia cell survival. Stem Cell Res Ther 9(1):271
Corre J, Mahtouk K, Attal M, Gadelorge M, Huynh A et al (2007) Bone marrow mesenchymal stem cells are abnormal in multiple myeloma. Leukemia 21(5):1079–1088
Desantis V, Savino FD, Scaringella A, Potenza MA, Nacci C et al (2022) The leading role of the immune microenvironment in multiple myeloma: a new target with a great prognostic and clinical value. J Clin Med 11(9):2513
Diaz-Tejedor A, Lorenzo-Mohamed M, Puig N, Garcia-Sanz R, Mateos MV et al (2021) Immune system alterations in multiple myeloma: molecular mechanisms and therapeutic strategies to reverse immunosuppression. Cancers (basel) 13(6):1353
Fernando RC, Mazzotti DR, Azevedo H, Sandes AF, Rizzatti EG et al (2019) Transcriptome analysis of mesenchymal stem cells from multiple myeloma patients reveals downregulation of genes involved in cell cycle progression, immune response, and bone metabolism. Sci Rep 9(1):1056
Flores-Figueroa E, Arana-Trejo RM, Gutiérrez-Espíndola G, Pérez-Cabrera A, Mayani H (2005) Mesenchymal stem cells in myelodysplastic syndromes: phenotypic and cytogenetic characterization. Leuk Res 29(2):215–224
Forster S, Radpour R, Ochsenbein AF (2023) Molecular and immunological mechanisms of clonal evolution in multiple myeloma. Front Immunol 14:1243997
Garayoa M, Garcia JL, Santamaria C, Garcia-Gomez A, Blanco JF et al (2009) Mesenchymal stem cells from multiple myeloma patients display distinct genomic profile as compared with those from normal donors. Leukemia 23(8):1515–1527
García-Sánchez D, González-González A, Alfonso-Fernández A, Del Dujo-Gutiérrez M, Pérez-Campo FM (2023) Communication between bone marrow mesenchymal stem cells and multiple myeloma cells: Impact on disease progression. World J Stem Cells 15(5):421–437
Garderet L, Mazurier C, Chapel A, Ernou I, Boutin L et al (2007) Mesenchymal stem cell abnormalities in patients with multiple myeloma. Leuk Lymphoma 48(10):2032–2041
Guo J, Zhao Y, Fei C, Zhao S, Zheng Q et al (2018) Dicer1 downregulation by multiple myeloma cells promotes the senescence and tumor-supporting capacity and decreases the differentiation potential of mesenchymal stem cells. Cell Death Dis 9(5):512
Gupta D, Treon SP, Shima Y, Hideshima T, Podar K et al (2001) Adherence of multiple myeloma cells to bone marrow stromal cells upregulates vascular endothelial growth factor secretion: therapeutic applications. Leukemia 15(12):1950–1961
Kawano Y, Kawano H, Ghoneim D, Fountaine TJ, Byun DK et al (2023) Myelodysplastic syndromes disable human CD271+VCAM1+CD146+ niches supporting normal hematopoietic stem/progenitor cells. bioRxiv 2023.04.09.536176 (2023).
Kumar SK, Rajkumar V, Kyle RA, van Duin M, Sonneveld P et al (2017) Multiple myeloma. Nat Rev Dis Primers 3:17046
Landgren O, Kyle RA, Pfeiffer RM, Katzmann JA, Caporaso NE et al (2009) Monoclonal gammopathy of undetermined significance (MGUS) consistently precedes multiple myeloma: a prospective study. Blood 113(22):5412–5417
Lovell-Badge R, Anthony E, Barker RA, Bubela T, Brivanlou AH et al (2021) ISSCR guidelines for stem cell research and clinical translation: the 2021 update. Stem Cell Rep 16(6):1398–1408
McCarthy PL, Holstein SA, Petrucci MT, Richardson PG, Hulin C et al (2017) Lenalidomide maintenance after autologous stem-cell transplantation in newly diagnosed multiple myeloma: a meta-analysis. J Clin Oncol 35(29):3279–3289
Mehdi SJ, Johnson SK, Epstein J, Zangari M, Qu P et al (2019) Mesenchymal stem cells gene signature in high-risk myeloma bone marrow linked to suppression of distinct IGFBP2-expressing small adipocytes. Br J Haematol 184(4):578–593
Moreau P, Attal M, Hulin C, Arnulf B, Belhadj K et al (2019) Bortezomib, thalidomide, and dexamethasone with or without daratumumab before and after autologous stem-cell transplantation for newly diagnosed multiple myeloma (CASSIOPEIA): a randomised, open-label, phase 3 study. Lancet 394(10192):29–38
Moreau P, Kumar SK, San Miguel J, Davies F, Zamagni E et al (2021) Treatment of relapsed and refractory multiple myeloma: recommendations from the International Myeloma Working Group. Lancet Oncol 22(3):e105–e118
Pan C, Hu T, Liu P, Ma D, Cao S et al (2023) BM-MSCs display altered gene expression profiles in B-cell acute lymphoblastic leukemia niches and exert pro-proliferative effects via overexpression of IFI6. J Transl Med 21(1):593
Plakhova N, Panagopoulos V, Vandyke K, Zannettino ACW, Mrozik KM (2023) Mesenchymal stromal cell senescence in haematological malignancies. Cancer Metastasis Rev 42(1):277–296
Rathnayake AJ, Goonasekera HW, Dissanayake VH (2016) Phenotypic and cytogenetic characterization of mesenchymal stromal cells in de novo myelodysplastic syndromes. Anal Cell Pathol (Amst) 2016:8012716.
Vanegas NP, Ruiz-Aparicio PF, Uribe GI, Linares-Ballesteros A, Vernot JP (2021) Leukemia-induced cellular senescence and stemness alterations in mesenchymal stem cells are reversible upon withdrawal of B-cell acute lymphoblastic leukemia cells. Int J Mol Sci 22(15):8166
Wallace SR, Oken MM, Lunetta KL, Panoskaltsis-Mortari A, Masellis AM (2001) Abnormalities of bone marrow mesenchymal cells in multiple myeloma patients. Cancer 91(7):1219–1230
Xu S, Evans H, Buckle C, De Veirman K, Hu J et al (2012) Impaired osteogenic differentiation of mesenchymal stem cells derived from multiple myeloma patients is associated with a blockade in the deactivation of the Notch signaling pathway. Leukemia 26(12):2546–2549
Xu S, De Veirman K, De Becker A, Vanderkerken K, Van Riet I (2018) Mesenchymal stem cells in multiple myeloma: a therapeutical tool or target? Leukemia 32(7):1500–1514
Yaccoby S, Pearse RN, Johnson CL, Barlogie B, Choi Y et al (2002) Myeloma interacts with the bone marrow microenvironment to induce osteoclastogenesis and is dependent on osteoclast activity. Br J Haematol 116(2):278–290
Acknowledgements
The author(s) wish(es) to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2015. Also, this work was supported by the National Research Foundation (NRF) grant (No. 2022R1F1A1075163) funded by the MSIT of Korea (2022M3A9B6018217); and the Technology Innovation Program (No.20012378) funded by the Ministry of Trade, Industry & Energy (MOTIE, Korea).
Author information
Authors and Affiliations
Contributions
HJK and S-AY designed the research study. SYE and SH performed the experiments. SYE and SH and HK analyzed the experiment data. HJK and S-AY and SYE interpreted data and wrote manuscript. According to the experimental contribution, HJK stated as the first co-first author.
Corresponding author
Ethics declarations
Conflict of interest
Hye Joung Kim declares that she has no conflict of interest. So Young Eom declares that she has no conflict of interest. Saeyeon Hwang declares that he has no conflict of interest. Hyunsoo Kim declares that he has no conflict of interest. Seok Chung declares that he has no conflict of interest. Seung-Ah Yahng declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, H.J., Eom, S.Y., Hwang, S. et al. Phenotypic and functional alterations of bone marrow MSCs exposed to multiple myeloma cells. Mol. Cell. Toxicol. 20, 723–733 (2024). https://doi.org/10.1007/s13273-023-00415-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13273-023-00415-5