Abstract
This study presents the numerical analysis of stem fixation in hip surgery using with/without cement methods since the use of cement is still controversial based on the clinical studies in the literature. Many different factors such as stress shielding, aseptic loosening, material properties of the stem, surgeon experiences etc. play an important role in the failure of the stem fixations. The stem fixation methods, cemented and uncemented, were evaluated in terms of mechanical failure aspects using computerized finite element method. For the modeling processes, three dimensional (3D) femur model was generated from computerized tomography (CT) images taken from a patient using the MIMICS Software. The design of the stem was also generated as 3D CAD model using the design parameters taken from the manufacturer catalogue. These 3D CAD models were generated and combined with/without cement considering the surgical procedure using SolidWorks program and then imported into ANSYS Workbench Software. Two different material properties, CoCrMo and Ti6Al4V, for the stem model and Poly Methyl Methacrylate (PMMA) for the cement were assigned. The material properties of the femur were described according to a density calculated from the CT images. Body weight and muscle forces were applied on the femur and the distal femur was fixed for the boundary conditions. The calculations of the stress distributions of the models including cement and relative movements of the contacts examined to evaluate the effects of the cement and different stem material usage on the failure of stem fixation. According to the results, the use of cement for the stem fixation reduces the stress shielding but increases the aseptic loosening depending on the cement crack formations. Additionally, using the stiffer material for the stem reduces the cement stress but increases the stress shielding. Based on the results obtained in the study, even when taking the disadvantages into account, the cement usage is more suitable for the hip fixations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip surgery is a procedure performed for hip pain relief using either cemented or uncemented approaches; each of these approaches has advantages and disadvantages. The most important disadvantage of the cemented method is osteolysis associated with cement disease [1, 2], whereas stress shielding and high cost are the disadvantages of the uncemented method [3, 4]. It is very difficult to decide which method is more successful based on the literature because of discrepancies among the published results. Some studies point out that the cemented method leads to higher revision rates in the first 10 years [5, 6]; that is exactly opposite of other studies [7–9]. In a similar way, some studies reported that total hip surgeries using the uncemented method have both a higher survival [3] and revision rates [9].
The studies show that whether the cemented or uncemented methods is superior one another since many factors such as stem design, patient age, bone quality, surgeon experiences, etc. [5] affected as seen in Table 1. However, the most important factor is the stem design, since recently the stem design have been developed due to clinical experiences [10, 11]. Also, the studies reported that the uncemented method should be preferred in young patients and the cemented method should be applied in older patients [10, 12–15]. There were no differences between the cemented and uncemented techniques used in clinical studies in terms of the survivorship [16, 17].
In this study, both methods, cemented and uncemented, were evaluated in terms of mechanical aspects using finite element analysis (FEA). In the FEA processes, the most important variables, the cement usage, and stem materials were considered. The equivalent stress and micro-motion between the stem and femur were compared to evaluate which one is the best for the hip surgery in view of different mechanical aspects.
Materials and methods
Model development
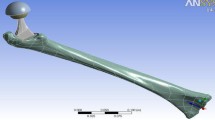
The femur was modeled in 3D using computerized tomography (CT) images obtained from a male patient (aged 63, Body-Mass Index 26 Kg/m2) taken from a Toshiba Aquilion CT scanner in the Department of Radiology, School of Medicine at Kocaeli University. CT images consist of parallel layers having a pixel size of 0.774 × 0.774 mm at the lateral position and a voxel resolution of 473 × 473 × 235. 1841-layer shootings were carried out to develop the model, recorded in the Digital Imaging and Communications in Medicine (DICOM) format, and transferred to the MIMICS 17 (Materialise, Leuven, Belgium) 3D image-processing software. The surface errors such as spikes, intersections etc. of the femur models were corrected using Geomagic Studio 10 software (Raindrop Inc., USA). After these corrections, the 3D smooth solid model was developed and imported into SolidWorks program (Dassault Systems SolidWorks Corp., USA) in IGES format.
The cemented and uncemented stems were modeled in SolidWorks using design parameters taken from the TIPSAN Catalog (TIPSAN Co. Inc., İzmir/Turkey). The cement thickness was created as 2 mm to obtain better results in the modeling processes [18–20]. The created femur head was operated according to surgery procedure and combined with the cement and stem. The combined femur and stem models were transferred into the ANSYS Workbench (ANSYS Inc. Canonsburg, PA) in STEP format.
Material properties mesh and contact assignments
It was assumed that the material properties of all models were selected as linear, elastic and isotropic. The most commonly used two different materials, Ti6Al4V and CoCrMo, were defined and imported their properties into the ANSYS Workbench Software as seen in Table 2 [21, 22]. The modulus of elasticity for the femur was described according to the density that was calculated from the CT images in MIMICS [22].
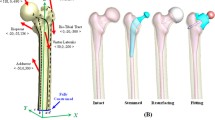
Mesh convergence was tested by refining the element size from 6 to 3 at 1 mm interval on the femur, 4 to 1 at 0.5 mm interval on the stem and 2 to 0.5 at 0.25 mm interval on the cement models. The most suitable element sizes for the optimum results were determined as 4, 1.5 and 0.75 mm for the whole femur, stem, and cement, respectively. Solid187 tetrahedron element was used in the whole finite element model, in which several mesh sizes along with additional refinements were defined at contact regions to get convergences. The number of the elements are changing between 400,000 and 800,000 and the nodes are changing from 600,000 to 950,000 in the FEA models, as seen in Fig. 1. Ten different models were named with their abbreviations of the methods, stem material names and contact definitions as seen in Table 3. The cement and bone interface was assumed to be bonded because of perfect connection in the cemented models [18, 21, 23–25]. The interface was also assumed frictional contact with the frictional coefficient of 1.0 [26]. The cement-stem interfaces were presumed to be either bonded [23] or frictional contact type [26]. The stem-bone contact types for the uncemented models were defined as either frictional [27, 28] or bonded contact [29, 30].
Boundary conditions
The boundary conditions were defined for the models as seen in Fig. 1. The stem-bone models were subjected to static loads obtained from literature in accordance with the value reported for a person walking at a normal speed. The coordinate system for the femur was defined based on the definition by Bergmann et al. [31]. Considering the body weight, the maximum forces resulting from walking were applied to the femoral head. The muscle forces were defined as presented by Duda et al. [32] (Table 4). The distal end of the femur was constrained in three directions considering the contact surface of the knee joint.
Results
Three different criteria were selected to evaluate the results obtained from the FEA. First, the von Mises stresses on the stem, femur contact surfaces and cement were calculated to assess the strength. Second, the relative micro-motions were investigated between the stem and femur to evaluate the formation of the osseointegration in the uncemented models [33]. Finally, the axial normal strain distributions of the femur were calculated to examine the stress shielding [29, 30, 34, 35].
The effects of the stem material
The stem material affected the stress distribution and micro-motion on the femur contact surfaces depending on the contact conditions. As can be seen Table 5, the Ti6Al4V alloy stem reduced the peak von Mises contact stress (PVMCS) on the femur surface among the uncemented models when comparing the CoCrMo Alloy stem (UcTiFri versus UcCoFri). However, the Ti6Al4V alloy stem increased the PVMCS of the femur in the cemented models with the frictional contact when compared to CoCrMo Alloy stems (CTiFriFri versus CCoFriFri and CTiFriBo versus CCoFriBo). Besides, the Ti6Al4V stem decreased the PVMCS of the femur in the models with bonded contact. Ti6Al4V stem usage caused more PVMS on the cement than CoCrMo stem usage in frictional contact conditions (CTiFriFri versus CCoFriFri and CTiFriBo versus CCoFriBo). However, Ti6Al4V stem decreased the peak von Mises stress (PVMS) on the cement in bonded contact (CTiBoBo versus CCoBoBo). The PVMS on the Ti6Al4V stems has lower than the CoCrMo stems as expected. The maximum PVMS of the stem was obtained lower than the yield stress of the materials as shown in Table 2. Therefore, the mechanical failures of stems were not expected according to these conditions. Osseointegration was available for all the uncemented models considering the peak micro-motion according to the study of Jasty et al. (lower than 40 microns) [33].
The effects of the contact conditions
The PVMCS of the femur surfaces were affected due to the contact types between stem and femur. As illustrated in Table 5, the PVMCS in the uncemented models obtained approximately four times the bonded contacts comparing the frictional contacts. However, the PVMCS of femur surfaces decreased in the bonded contacts versus frictional one in the cemented models. The PVMS on the stem increased in the bonded contacts. The contact type between stem and cement or cement and bone also affected the PVMS of cement. The PVMS of cement with bonded contacts was calculated lower than with frictional contacts. The lowest PVMS of cement was obtained in the CTiBoBo model. The micro-motion between bone and stem was calculated higher in frictional contact as expected.
The effects of the cement
As shown in Table 5, the cement usage with Ti6Al4V stem increased the PVMCS on the femur surfaces in the frictional contacts (UcTiFri versus CTiFriFri). When using the contact was bonded, cement usage with Ti6Al4V decreased the PVMCS on the femur surfaces (UcTiBo versus CTiFriBo and CTiBoBo). The cement usage with CoCrMo stem decreased the PMVCS of the femur in both frictional and bonded contacts (UcCoFri versus CCoFriFri, UcCoBo versus CCoFriBo and CCoBoBo). Finally, the cement usage caused to decrease the PVMCS of femur surfaces.
The cement usage with Ti6Al4V did not affect the PVMS of the stems in the frictional contacts (UcTiFri versus CTiFriFri and CTiFriBo). When the contact was bonded, the cement usage with Ti6Al4V decreased the PVMS of stems (UcTiBo versus UcTiBoBo). The cement usage with CoCrMo stem decreased the PVMS of stems in both frictional and bonded contacts as seen in Table 5 (UcCoFri versus CCoFriFri and CCoFriBo, UcCoBo versus CCoBoBo). Therefore, the cement usage causes to decrease the PVMS on the stem.
The effects of the stress shielding
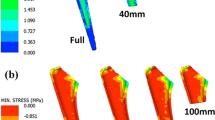
The axial normal strains were calculated at ten different designated points on the models as seen Fig. 2. The highest compressive strain was found on the intact (non-surgical) femur. The stem insertion caused to decrease strain values especially at point five and six. The cement usage increased the strains on the femur that decreased the stress shielding. Less stress shielding was obtained in the Ti6Al4V stem comparing the CoCrMo stem. The different contact types are also causing the stress shielding emerge in all implanted models. Therefore, the frictional contact caused to decrease the strain values more than bonded contacts.
Discussion
The selection of proper method, cemented or uncemented, considering the stress shielding and aseptic loosening issues is still unclear regarding clinical studies since it depends on surgeon experiences. The clinical treatment observations after hip surgeries can be evaluated numerically using engineering techniques such as FEA since the stress shielding and aseptic loosening are the most important issues for failing the hip surgeries [5, 29]. As mentioned above, there is no biomechanical study comparing those methods considering failure issues. For these reasons, both techniques were evaluated using two different materials (Ti6Al4V and CoCrMo) in biomechanical viewpoints.
According to the Wolff’s law [34], the meaning of stress shielding is the reduction of the stresses on the femur due to changing load transfer after the stem insertion. That is; the removal of stresses from the bone refers to the weak bone density. However, when the stem is implanted, the load is transferred through the stem rather than the femur, that results in the bone weakening and stress shielding. In addition, the stem design parameters and material types play important roles for the stress shielding problem [30, 34]. The stress shielding values are increasing when using the CoCrMo stem material as seen in Fig. 2. The stress transferring from the stem to the femur is much easier when using the Ti6Al4V having higher ductility as given Table 2. Therefore, the stem made out of stiffer material causes higher stress shielding as seen in Table 5. These results obtained in the study also confirmed the studies given in the literature [35]. Lower stress shielding was also obtained in cemented fixation technique rather than uncemented one, also confirmed by [29], since both cement and cancellous of the femur have similar material properties. Using the cement in the fixation process increases the strain values at the proximal part of the femur. The contact types also affect the load transfer between the femur and stem as obtained in the FEA process as illustrated in Fig. 2. The frictional contact is defined to represent the healing (post operation) process and bonded contact is defined to simulate the healed femur (osseointegrated femur). Therefore, the load transfer is more suitable in the healed femur to decelerate the stress shielding occurrence.
The strength of the cement is very important since the crack growth in the cement plays an important role for the generation of aseptic loosening [16]. Using the stiffer stem material reduces the stress occurrence in the cement as reported similarly in the literature [36, 37]. In the FEA process, the higher stress values leading crack growth were obtained in the cement when using Ti6Al4V material along with frictional contact. Therefore, using of CoCrMo material gives better results during the healing process, but the Ti6Al4V material is more convenient for healed femur in terms of nonformation of cement cracks.
The contact types of the cement-stem and cement-bone couples were described differently in the literature. The cement-bone interfaces were mostly described as either bonded contact type due to perfect bonding in the healing (post operation) process [18, 21, 23–25] or frictional contact by Ramaniraka et al. [26]. The frictional contact and bonded contact types were used by [18, 21, 23, 25, 26], respectively, between the cement-stem models. Therefore, all contact types were considered in our study, as given in Table 3. While the stress (PVMCS) values on the femur and (PVMS) on the cement decreased using the bonded contact but increased using the frictional contact. In the uncemented models, however, the stress occurrences are the other way around. Based on these obtained results, uncemented fixation method has lower survival rate comparing the cemented fixation technique which was also reported by Morshed et al. [38]. But, cemented fixation technique has riskier due to cement crack formation, using the frictional contact type that causes the revisions of the hip fixation also reported by Abdulkarim et al. study [16]. On the other hand, the femur contact stresses (PVMCS) evaluated in this study (Table 5) were not considered by the literature [21, 24, 29]. The higher PVMCS (Table 5) values on the contact surfaces cause femur contact surface failure that generates the small gaps and then results in the aseptic loosening.
After total hip fixation, the failures of the stem do not or rarely occur since the calculated PVMS values obtained changing from 150 to 565 MPa lower than the yield stress of the stem materials. This result was also confirmed by researchers [39, 40]. The micro-motion values between the stem and femur should not exceed the 40 microns for ideal osseointegration formation. If the micro-motion values exceed the 40 microns and lower than 150 microns, the fibrous tissues are taken place that weakens the bonding of the bone-stem couple. If the values exceed the 150 microns, then undesired aseptic loosening occurs [33]. Based on the results obtained in the study, the ideal osseointegration formation is available in uncemented fixation technique. Therefore, when using the uncemented fixation method, the risk of the aseptic loosening is rather low during the healing process.
In this study, some assumptions were used that may be limited the results. First, the values of loading conditions were taken into account during the only regular walking in the FEA modeling process. Second, the design parameters of the selected stem model taken from the TIPSAN Co. cataloque were also considered in both cemented and uncemented fixation modeling. Third, the bonding interfaces of the cement-femur, cement-stem, and femur-stem couples were assumed to be bonded perfectly but the contact ratio is variable depends on patients, surgeon experiences, stem, and cement qualities. Finally, the material properties of the bone models were defined as isotropic but the bone materials are usually accepted as anisotropic [41]. The isotropic material properties for bone can be acceptable because of small differences between the isotropic and anisotropic material properties of bone [42]. The definition of the bone material properties as isotropic in the modeling was also depended on the MIMICS Software. However, different boundary conditions, stem design parameters, and material properties may be used in the modeling process that may change the results slightly.
Conclusion
In this study, two different methods, cemented and uncemented for the stem fixation in hip surgeries using two different materials for the stem were compared and analyzed with the use of computerized FEA simulations. Different boundary conditions were also considered in the simulations. Based on the study, the following results can be concluded.
-
For the stem fixation in hip surgery, cement material usage reduces the stress shielding and aseptic loosening problems.
-
The stiffer material (CoCrMo) used for the stem reduces the stresses on the cement during the healing process but causes the cement cracks formation in healed femur. Therefore, the stiffer material used for the stem have shorter survivorship.
-
The stiffer stem material (CoCrMo) used for the stem causes higher stress shielding in the femur, therefore, the Ti6Al4V material selection for the stem is more convenient.
-
It was observed that the definition of contact types in the modeling process plays an important role in the results. Therefore, the contact types should be selected considering the modeling conditions.
The cement material usage in hip surgery is more suitable considering the stress shielding and aseptic loosening problems.
References
Huddleston HD (1988) Femoral lysis after cemented hip arthroplasty. J Arthroplasty 3:285–297
Harris WH, Mcgann WA (1986) Loosening of the femoral component after use of the medullary-plug cementing technique—follow-up note with a minimum 5-year follow-up. J Bone Joint Surg Am 68a:1064–1066
Unnanuntana A, Dimitroulias A, Bolognesi MP, Hwang KL, Goodman SB, Marcus RE (2009) Cementless femoral prostheses cost more to implant than cemented femoral prostheses. Clin Orthop Relat R 467:1546–1551
Khanuja HS, Vakil JJ, Goddard MS, Mont MA (2011) Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am 93a:500–509
Bordini B, Stea S, De Clerico M, Strazzari S, Sasdelli A, Toni A (2007) Factors affecting aseptic loosening of 4750 total hip arthroplasties: multivariate survival analysis. BMC Musculoskelet Disord 8:69
Makela KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V (2008) Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am 90:2160–2170
Hailer NP, Garellick G, Karrholm J (2010) Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register Evaluation of 170,413 operations. Acta Orthop 81:34–41
Weiss RJ, Hailer NP, Stark A, Karrholm J (2012) Survival of uncemented acetabular monoblock cups: evaluation of 210 hips in the Swedish Hip Arthroplasty Register. Acta Orthop 83:214–219
Smith AJ, Dieppe P, Howard PW, Blom AW, National Joint Registry For E, Wales (2012) Failure rates of metal-on-metal hip resurfacings: analysis of data from the National Joint Registry for England and Wales. Lancet 380:1759–1766
Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE (2000) The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 71:337–353
Sueyoshi T, Berend ME, Meding JB, Malinzak RA, Lackey WG, Ritter MA (2015) Changes in femoral stem geometry reduce intraoperative femoral fracture rates in total hip replacement. Open J Orthop 5:115–119
Lucht U (2000) The Danish Hip Arthroplasty Register. Acta Orthop Scand 71:433–439
Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P (2005) Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register—4661 primary replacements followed for 0–22 years. Acta Orthop 76:28–41
Hooper GJ, Rothwell AG, Stringer M, Frampton C (2009) Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg British Vol 91:451–458
Makela KT, Matilainen M, Pulkkinen P, Fenstad AM, Havelin L, Engesaeter L, Furnes O, Pedersen AB, Overgaard S, Karrholm J, Malchau H, Garellick G, Ranstam J, Eskelinen A (2014) Failure rate of cemented and uncemented total hip replacements: register study of combined Nordic database of four nations. Bmj-Brit Med J 348:f7592
Abdulkarim A, Ellanti P, Motterlini N, Fahey T, O’byrne JM (2013) Cemented versus uncemented fixation in total hip replacement: a systematic review and meta-analysis of randomized controlled trials. Orthop Rev (Pavia) 5:e8
Meding JB, Ritter MA, Davis KE, Hillery M (2016) Cemented and uncemented total hip arthroplasty using the same femoral component. Hip Int 26:62–66
Ramos A, Completo A, Relvas C, Simoes JA (2012) Design process of a novel cemented hip femoral stem concept. Mater Des 33:313–321
Ramos A, Simoes JA (2009) The influence of cement mantle thickness and stem geometry on fatigue damage in two different cemented hip femoral prostheses. J Biomech 42:2602–2610
Kayabasi O, Ekici B (2007) The effects of static, dynamic and fatigue behavior on three-dimensional shape optimization of hip prosthesis by finite element method. Mater Design 28:2269–2277
Senalp AZ, Kayabasi O, Kurtaran H (2007) Static, dynamic and fatigue behavior of newly designed stem shapes for hip prosthesis using finite element analysis. Mater Des 28:1577–1583
Rho JY, Hobatho MC, Ashman RB (1995) Relations of mechanical-properties to density and Ct numbers in human bone. Med Eng Phys 17:347–355
Higa M, Tanino H, Nishimura I, Mitamura Y, Matsuno T, Ito H (2015) Three-dimensional shape optimization of a cemented hip stem and experimental validations. J Artif Organs 18:79–85
Norman TL, Shultz T, Noble G, Gruen TA, Blaha JD (2013) Bone creep and short and long term subsidence after cemented stem total hip arthroplasty (THA). J Biomech 46:949–955
Oshkour AA, Davoodi MM, Abu Osman NA, Yau YH, Tarlochan F, Abas WaBW (2013) Finite element analysis of circumferential crack behavior in cement-femoral prosthesis interface. Mater Design 49:96–102
Ramaniraka NA, Rakotomanana LR, Leyvraz PF (2000) The fixation of the cemented femoral component—effects of stem stiffness, cement thickness and roughness of the cement-bone surface. J Bone Joint Surg Br 82b:297–303
Oshkour AA, Abu Osman NA, Bayat M, Afshar R, Berto F (2014) Three-dimensional finite element analyses of functionally graded femoral prostheses with different geometrical configurations. Mater Design 56:998–1008
Rancourt D, Shiraziadl A, Drouin G, Paiement G (1990) Friction properties of the interface between porous-surfaced metals and tibial cancellous bone. J Biomed Mater Res 24:1503–1519
Chen WP, Tai CL, Lee MS, Lee PC, Liu CP, Shih CH (2004) Comparison of stress shielding among different cement fixation modes of femoral stem in total hip arthroplasty—a three-dimensional finite element analysis. J Med Biol Eng 24:183–187
Goshulak P, Samiezadeh S, Aziz MS, Bougherara H, Zdero R, Schemitsch EH (2016) The biomechanical effect of anteversion and modular neck offset on stress shielding for short-stem versus conventional long-stem hip implants. Med Eng Phys 38:232–240
Bergmann G, Deuretzbacher G, Heller M, Graichen F, Rohlmann A, Strauss J, Duda GN (2001) Hip contact forces and gait patterns from routine activities. J Biomech 34:859–871
Duda GN, Schneider E, Chao EYS (1997) Internal forces and moments in the femur during walking. J Biomech 30:933–941
Jasty M, Bragdon C, Burke D, Oconnor D, Lowenstein J, Harris WH (1997) In vivo skeletal responses to porous-surfaced implants subjected to small induced motions. J Bone Joint Surg Am 79a:707–714
Ridzwan MIZ, Shuib S, Hassan AY, Shokri AA, Ibrahim MM (2007) Problem of stress shielding and improvement to the hip implant designs: a review. J Med Sci 7:460–467
Bitsakos C, Kerner J, Fisher I, Amis AA (2005) The effect of muscle loading on the simulation of bone remodelling in the proximal femur. J Biomech 38:133–139
Crowninshield RD, Pedersen DR, Brand RA, Johnston RC (1983) Analytical support for acetabular component metal backing. Hip 1983:207–215
Friedman RJ, Black J, Galante JO, Jacobs JJ, Skinner HB (1994) Current concepts in orthopaedic biomaterials and implant fixation. Instr Course Lect 43:233–255
Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM (2007) Comparison of cemented and uncemented fixation in total hip replacement—a meta-analysis. Acta Orthop 78:315–326
Wroblewski BM (1982) Fractured stem in total hip replacement. A clinical review of 120 cases. Acta Orthop Scand 53:279–284
Pellicci PM, Wilson PD, Sledge CB, Salvati EA, Ranawat CS, Poss R (1982) Revision total hip-arthroplasty. Clin Orthop Relat R 170:34–41
Wirtz DC, Schiffers N, Pandorf T, Radermacher K, Weichert D, Forst R (2000) Critical evaluation of known bone material properties to realize anisotropic FE-simulation of the proximal femur. J Biomech 33:1325–1330
Peng L, Bai J, Zeng XL, Zhou YX (2006) Comparison of isotropic and orthotropic material property assignments on femoral finite element models under two loading conditions. Med Eng Phys 28:227–233
Acknowledgements
This work is supported by the Scientific Research Projects Unit of Kocaeli University under project no. 2015/098 and 2015/074HD. The corresponding author thanks The Scientific and Technological Research Council of Turkey (TUBITAK) 2211-C Scholarship program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Ethical approval
Ethics appproval is not required for this study.
Rights and permissions
About this article
Cite this article
Çelik, T., Mutlu, İ., Özkan, A. et al. The effect of cement on hip stem fixation: a biomechanical study. Australas Phys Eng Sci Med 40, 349–357 (2017). https://doi.org/10.1007/s13246-017-0539-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-017-0539-1