Abstract
When implementing Acuros XB (AXB) as a substitute for anisotropic analytic algorithm (AAA) in the Eclipse Treatment Planning System, one is faced with a dilemma of reporting either dose to medium, AXB-Dm or dose to water, AXB-Dw. To assist with decision making on selecting either AXB-Dm or AXB-Dw for dose reporting, a retrospective study of treated patients for head & neck (H&N), prostate, breast and lung is presented. Ten patients, previously treated using AAA plans, were selected for each site and re-planned with AXB-Dm and AXB-Dw. Re-planning was done with fixed monitor units (MU) as well as non-fixed MUs. Dose volume histograms (DVH) of targets and organs at risk (OAR), were analyzed in conjunction with ICRU-83 recommended dose reporting metrics. Additionally, comparisons of plan homogeneity indices (HI) and MUs were done to further highlight the differences between the algorithms. Results showed that, on average AAA overestimated dose to the target volume and OARs by less than 2.0 %. Comparisons between AXB-Dw and AXB-Dm, for all sites, also showed overall dose differences to be small (<1.5 %). However, in non-water biological media, dose differences between AXB-Dw and AXB-Dm, as large as 4.6 % were observed. AXB-Dw also tended to have unexpectedly high 3D maximum dose values (>135 % of prescription dose) for target volumes with high density materials. Homogeneity indices showed that AAA planning and optimization templates would need to be adjusted only for the H&N and Lung sites. MU comparison showed insignificant differences between AXB-Dw relative to AAA and between AXB-Dw relative to AXB-Dm. However AXB-Dm MUs relative to AAA, showed an average difference of about 1.3 % signifying an underdosage by AAA. In conclusion, when dose is reported as AXB-Dw, the effect that high density structures in the PTV has on the dose distribution should be carefully considered. As the results show overall small dose differences between the algorithms, when transitioning from AAA to AXB, no significant change to existing prescription protocols is expected. As most of the clinical experience is dose-to-water based and calibration protocols and clinical trials are also dose-to-water based and there still exists uncertainties in converting CT number to medium, selecting AXB-Dw is strongly recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The shortcomings of the Anisotropic analytic algorithm (AAA) in the Eclipse treatment planning system (Varian Medical Systems, Inc., Palo Alto, CA, USA) are well documented. It has been shown that AAA overestimates doses in the lung region [1–4]. AAA is also unable to correctly handle altered attenuation along large density gradients [5] and resultantly overestimates doses beyond low density material and underestimates dose beyond high density materials.
To improve on the handling of these discrepancies, Acuros XB (AXB), a photon dose calculation algorithm, was introduced in the eclipse treatment planning system (TPS). AXB was developed from the work done by Vassiliev et al. [6] and is based on solving the linear Boltzmann transport equation using numeric methods. The issues affecting AAA were to be addressed by AXB with the promise of accuracy and speed [7, 8]. AXB dose calculation consists of four steps [7]: 1. transport of source model fluence into patient, calculation of 2. photon and 3. electron scatter in patient (medium) and 4. the final dose calculation. The calculation of the AXB dose to medium (AXB-Dm) and AXB dose to water (AXB-Dw) differs only in the final dose calculation step where with AXB-Dm the energy dependent response function is based on a voxel material property whereas with AXB-Dw, this function is based on water. In AXB, the material composition of an individual voxel is derived from the Hounsfield unit value which is converted to mass density using CT calibration curves [7]. From the calculated mass density, the voxel material is determined based on a hard coded look up table. Users can override the automatic material assignment. AAA on the other hand, uses a three dimensional pencil beam convolution/superposition algorithm [9, 10]. The longitudinal distribution of the pencil beam is scaled according to equivalent path lengths and the lateral distribution is scaled with densities relative to water in directions normal to the pencil beam. There have been many publications indicating that AXB is equally comparable in terms of accuracy in high and low density regions, to Monte Carlo (MC) methods with the added advantage of having no statistical noise [1, 6–8, 11, 12].
The issues in converting Monte Carlo calculated Dose to medium (Dm) to Dose to water (Dw) have been discussed by several investigators [13–18]. Following the AAPM Task Group 105 [19] recommendations, Ma et al. [16] demonstrated that up to 11.0 % dose differences are possible when doses are converted from Dm to Dw using stopping power ratios. Walters et al. [20], in their study on dose to sensitive skeletal tissue, put forward a strong argument why dose should be reported as Dw instead of Dm.
A number of studies compared AXB to AAA in phantoms [1, 11, 12, 21, 22] as well as using clinical plans [2, 3, 8, 21–23]. Most of these studies concluded that AXB is more accurate than AAA especially when dealing with junctions and regions of high density gradients e.g. in lung and bone. Rana et al. [23] present a comprehensive evaluation of AXB-Dm and AXB-Dw for prostate, lung and breast cancer but does not include comparison to AAA. The investigation by Kathirvel et al. [3] critically appraises the accuracy of AXB and AAA but does not distinguish between AXB-Dw and AXB-Dm and focuses more on dose verification using a 2D array. Fogliata et al. [2] and Kroon et al. [8] report clinical case comparisons of AXB to AAA but again do not distinguish between AXB-Dm and AXB-Dw. Hirata et al. [21] and Kan et al. [22] also present a study of AAA vs AXB for oropharyngeal, hypopharyngeal, laryngeal carcinomas and nasopharyngeal carcinomas respectively, but only use AXB-Dm for comparison. The study by Fogliata et al. [24], does compare AAA, AXB-Dm and AXB-Dw but they only looked at soft-tissue sarcoma.
The aim of this study was to fill a gap in literature on which mode to select between AXB-Dm and AXB-Dw, when moving from AAA. Using recommended dose metrics, this was achieved by performing a retrospective study of plans generated with AAA (used clinically for four common treatment sites) compared to plans generated using the two Acuros modes. This study was not intended to show which algorithm was more accurate, but rather to assist with the decision making on the selection of an option which would be in line with currently available data and taking into account clinical impact.
Methods
AAA calculated treatment plans were selected as originals and used as reference for most of the comparisons. Four sites were selected for investigation namely H&N, Prostate, Breast and Lung. For these sites, analysis was performed for: (a) fixed MU AXB plans versus AAA plans, (b) non-fixed MU AXB plans versus AAA plans and (c) AXB-Dw versus AXB-Dm for both fixed and non-fixed MU plans (with AXB-Dm as reference). In part (a), as this was a retrospective study, the fixed MU plan comparison demonstrated the differences between what was actually treated using AAA plans compared to AXB plans. In part (b), to reflect normal planning procedures, the non-fixed MU comparison demonstrated the differences between AAA and AXB that one would see if all plans are normalized to the same reference (ICRU reference point for conformal plans or PTV median dose for IMRT plans). In part (c), the difference between the two AXB modes was demonstrated.
The same beam data used for configuring AAA was used for AXB. Furthermore, to eliminate algorithm version differences, all original reference plans calculated using earlier AAA versions were re-calculated using AAA version 11.0.31 with a grid size of 2.5 mm. All subsequent AXB plans were calculated using AXB clinical version 11.0.31 with the same grid size. All IMRT plans were normalized to the median dose of the planning target volume (PTV).
Patient selection
40 AAA patient plans were selected and used to compare to AXB (AXB-Dm and AXB-Dw) plans. The selected plans consisted of 10 IMRT H&N plans (60 Gy to the primary volume in 30 fractions for all patients), 10 IMRT Prostate plans (74 Gy in 32 fractions for all patients), 10 Breast plans (50 Gy in 25 fractions for all patients) and 10 conformal Lung plans (60 Gy in 30 fractions for all patients). As some of the Breast plans had no delineated PTV, the 100 % isodose curve from the AAA plan was converted to a PTV for analysis purposes.
Fixed MU plans
Two copies, per patient, of the original AAA plan were created and the dose calculation algorithm was changed to AXB: AXB-Dm for one copy and AXB-Dw for the other copy. Both copies were re-calculated keeping all the geometric parameters and MUs fixed. These AXB plans were then compared to AAA plans.
Non-fixed MU plans
An additional two copies, per patient, were created and the dose calculation algorithm was again changed to AXB: AXB-Dm for one copy and AXB-Dw for the other copy. Both copies were re-calculated normalizing to either the ICRU reference point or the PTV median depending on treatment technique. These AXB plans were also then compared to AAA plans.
AXB-Dw versus AXB-Dm
AXB-Dw plans were also compared to their respective AXB-Dm plans for all sites.
Plan evaluation
All in all, a total of 200 plans were analyzed. ICRU-83 [25] recommended dose reporting metrics for dose volume prescribing and reporting were followed. DVHs were created for all the plans and from these the PTV Dmedian, D98 %, and the D2 % dose metrics were assessed. The PTV D95 % dose metric was only used for the analysis of H&N plans. Dose metrics assessed for OARs are shown in Table 1.
For each cohort of the 10 patients per treatment site, the average percent dose difference for each dose metric considered, were plotted and analyzed. The percent dose difference between AXB plans and AAA plans were calculated using the following equation:
and the percent dose difference between the AXB modes:
The dose distribution in the PTV was also evaluated using Homogeneity indices (HI), as defined in ICRU-83. The lower the HI value the more homogeneous the target dose distribution. Furthermore to assess any dose calculation differences between the algorithms, MUs were recorded.
Results
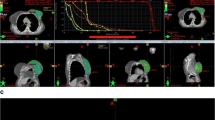
Figure 1 shows sample DVHs for fixed and non-fixed MU H&N plans of one of the patients in this study. For this particular patient, Fig. 1a shows that AXB-Dm underestimated dose to the PTV compared to both AAA and AXB-Dw. OARs show no significant differences except for the ipsi-lateral parotid where AXB-Dm underestimated dose.
Fixed MU plans
All fixed MU plan dose comparisons shown in Fig. 2, indicate that AAA overestimated dose to the PTV for all sites. The only exception was the D2 % for the H&N PTV, Fig. 2a, which showed that AAA underestimated dose relative to AXB-Dw.
As for the OARs, AAA also overestimated dose to the OARs for the H&N plans as shown in Fig. 2a. Figure 2b for the Prostate plans showed that for the OARs, AAA underestimated dose to the femurs compared to AXB-Dw but significantly overestimated dose relative to AXB-Dm. For the Breast plans, Fig. 2c, AAA underestimated the lung V20 values whereas it overestimated the lung V30 values relative to both AXB modes. In contrast to the Breast plans’ lung V20 and V30 values, the Lung plans in Fig. 2d showed a switch where AAA overestimated the lung V20 value and underestimated the lung V30 value.
Non-fixed MU plans
The average differences in the PTV dose metrics between the algorithms were all within ±1.5 %. For the H&N plans, shown in Fig. 3a, AAA in general overestimated dose to the OARs. However, significantly large standard deviations in the AXB-Dw values could be indicative of how sensitive this AXB mode is to variation in material density composition. As in the fixed MU plans, Fig. 3b for the Prostate plans showed that AAA underestimated dose to the femurs relative to AXB-Dw. The Breast and Lung plans, Fig. 3c, d respectively, showed a similar trend as the fixed MU plans.
AXB-Dw versus AXB-Dm
For all dose metrics considered in the H&N and prostate plans, Fig. 4a, b showed that AXB-Dw overestimated dose relative to AXB-Dm for fixed MUs. The exception was for the H&N OARs which showed AXB-Dw underestimated dose. In Fig. 4b, for the Prostate plans, the dose estimated for the femurs by AXB-Dw for both fixed and non-fixed MU plans were significantly higher (≈4.6 %) than any other dose metric difference.
For the lung and breast plans, Fig. 4c, d, the average dose differences for all dose metrics were all within ±1.2 %. In the case of the Breast plans, Fig. 4c, the PTV dose metrics for both the fixed and non-fixed MU plans showed that AXB-Dw underestimated dose. The OARs for both fixed and non-fixed MU plans, however, showed dose differences of less than 0.8 %. In Fig. 4d, for the Lung plans, all the dose metrics for the non-fixed MU plans showed that AXB-Dw underestimated dose whereas no obvious trend was observed for the fixed MU plans.
In Table 2, the differences in HI values for the fixed MU plans showed that, in general AAA produced more homogeneous plans. The HI values for AXB-Dw relative to AXB-Dm (not recorded in the table) showed no significant difference for all sites. Similar analysis for the non-fixed MU plans, for all sites, showed very similar trends to that of the fixed MU plans. The HI value comparison of AXB-Dw and AXB-Dm to AAA for the Prostate and Breast plans in general showed no significant difference except for Prostate AXB-Dw. For the H&N and Lung plans, the comparison to AAA showed the differences were significant.
The calculated MU differences between plans are summarised in Table 3. For the average percent MU variation between AXB-Dm and AAA, all sites showed significant differences except for Prostate site. When comparing the average percent MU variation between AXB-Dw and AAA, only the Breast site showed significant differences. As for the comparison between AXB-Dw and AXB-Dm, only the Lung site showed significant differences for the average percent MU variation.
Discussion
It is well documented that selecting AXB (AXB-Dm or AXB-Dw) over AAA represents a better dose estimation [1, 2, 7, 8, 12, 21, 22]. The question that remains then is whether to use AXB-Dm or AXB-Dw. This study was aimed at showing the clinical differences between AAA algorithm and the two AXB dose reporting modes in the Eclipse TPS environment to assist in making an informed decision on which AXB dose reporting mode to select when changing over from AAA to AXB.
The issue of whether to report dose as Dw or Dm has long been debated in MC dosimetry. Lui [15] argued in favor of the use of Dm for reporting stating that Dw reporting was only historically motivated. Lui also cited studies indicating that there would be little clinical impact when changing from Dw to Dm as most tissues of interest in radiotherapy are similar to water. Based on their findings, Ma et al. [16] also recommended that for MC photon algorithms the dose should be reported as Dm. In Lui et al. [15], Keall on the other hand, argued for maintaining Dw for dose reporting as most dosimetry protocols and clinical trials are based on a Dw calibration. Keall was also concerned that reporting Dm involved using non standardized CT number conversion to medium, based on ICRU or ICRP publications, and therefore at best the medium to report to was a guess. This is a very important point as everything else involved in producing a patient’s treatment plan is heavily depended on the input CT dataset.
Earlier studies already demonstrated that only significant differences would be seen in targets that include bones or other high Z materials. Using the fixed MU method, Kan et al. [22] found that AXB-Dm estimated lower mean doses ranging from 0.9 to 2 % for PTVs with normal tissue to those that included bone compared to AAA. For PTVs with air they found AXB-Dm to estimate higher mean doses by about 1.5 %. This is in line with the results seen here in Fig. 2a, and would explain the high variability in the PTV dose metrics for H&N plans as some volumes included bone and air.
In general our results, in agreement with published literature [2, 8, 24], showed that AAA overestimated the target dose which constitutes an under-dosage increasing the chances of possible local recurrence. On average the overestimation of the target dose by AAA was found to be less than 2 % for all sites. This was expected because targets are basically soft tissues and stopping power ratios for soft tissues vary by less than 3 %. Therefore, the differences between the two algorithms, AAA and AXB, were small and the effects were limited. Fogliata et al. [2] predict that the target dose overestimation by AAA leads to an equivalent MU underestimation of approximately 1–2 %. This MU underestimation is dependent on the site being treated in conjunction with the biological material within the target as well as the surrounding tissue in agreement with what is shown in Table 3.
In the H&N site where some of the PTV volumes included bone and air, AXB-Dw estimated higher values for the maximum D2 % dose metric than AAA. It was also noted that for Prostate PTVs with fudicial markers, AXB-Dw tended to have unexpectedly high 3D maximum dose values (>135 % of prescription dose). The high dose estimation was also seen in OARs that had densities significantly greater than water e.g. femoral heads in Prostate plans (see Fig. 2b and 3b). The reason for the occurrence of these hotspots has been dealt with by Failla et al. [7]. We can therefore conclude that AXB-Dw, in contrast with AXB-Dm, is relatively more sensitive to an increase in compositional inhomogeneity of the PTV which results in a more inhomogeneous dose distribution in the PTV. Consequently, if the dose is reported as AXB-Dw, the effect that high density structures in the PTV has on the dose distribution in the PTV for this AXB mode should be carefully considered.
Breast tissues are composed of about 70 % fat and 30 % parenchyma and on average the breast tissue density is around 0.9 g/cm3 compared to water which is 1.0 g/cm3. When comparing the PDDs for AAA, AXB-Dm and AXB-Dw, Failla et al. [7] demonstrated that there is very little difference in the behavior of the two algorithms in water. Subsequently, no significant difference in the buildup regions for the breast plans was observed. The AXB lung V30 values showed a significant difference to AAA and this could be due to the relatively small lung volumes included in the assessment.
The Lung plan results indicated that AXB median lung target doses were lower by 0.4 ± 0.8 % and 0.3 ± 0.7 % for AXB-Dm and AXB-Dw respectively. This is in agreement with Fogliata et al. [2], who found AXB target doses for 3 dimensional 6MV conformal lung plans to be lower by 0.3± 0.3 %. Our results indicated that there is not a huge difference to target doses between AAA and the two AXB options. For both the breast and lung sites, it is worth noting that the lung V20 and V30 values are highly depended on the prescriptions.
Comparing AXB-Dw against AXB-Dm, for all sites, showed overall dose differences up to 1.5 % as seen in Fig. 4a–d. The only exceptions were in Prostate plans where dose differences in the femurs were as high as 4.6 % where AXB-Dw overestimated dose. This is in agreement with Dogan et al. [13] who compared MC calculated D2 % femoral heads doses for Dm and Dw (Dw was converted from Dm using stopping power ratios) and found an average dose difference of about 5.3 %. Fogliata et al. [24] also came to a similar conclusion with AXB-Dw predicting 5 % higher doses in the bone compared to AXB-Dm and explains that the differences is due to the femur being composed of half cortical bone (stopping power ratio 1.11) and half cartilage (stopping power ratio 1.035).
In Table 2, AAA plans overall had lower HI values (indicating a more homogeneous PTV dose distribution) compared to the two AXB modes. This was partly due to all AXB plans being subjected to AAA planning parameters including restrictions to MUs without any further optimization. As the PTV densities for prostate and breasts are approximately close to water, there were no significant HI differences between AAA and the two AXB modes. The exception to this was AXB-Dw statistics for Prostates which was due to the majority of the Prostate PTVs having fiducial markers and AXB-Dw had a tendency to produce hotspots in high density objects as mentioned earlier. The difference between AAA and the two AXB modes for the H&N and Lung plans was significant because the PTVs for these sites were inhomogeneous with some including air and bone. AXB is able to correctly handle altered attenuation along large density gradients and resultantly correctly estimates doses beyond low and high density materials. The general take from this is that if transitioning from AAA to AXB, more work needs to be done on the plans to optimise the dose to the PTVs for the H&N and Lung sites. On the contrary, for the prostate and breast sites, the currently used planning and optimization templates might only need slight adjustments, if any.
Comparison of percent MU variation, in Table 3 between AAA and AXB-Dm on average showed significant differences. AAA utilized fewer MUs with the resultant dose to the PTV lower by about 1.5 % for the H&N, Breast and Lung sites. This is in agreement with published results [24] of 2.0 % underdose using AAA. As the location of the volumes for these sites would result in having beams passing through bone and or lung, as mentioned above, AXB better estimates dose beyond low or high density materials than AAA. For Prostate site, the beam arrangement usually avoids bone (femur) and the PTV consist of soft tissue hence the dose differences are insignificant.
Comparison of percent MU variation between AAA and AXB-Dw on average showed no significant differences. The exception was for the Breast site which showed a significant difference of about 2 % which would result in underdose using AAA. Both AXB-Dm and AXB-Dw showed significant differences for the Breast site, however this was more pronounced for AXB-Dw. AXB better handles missing tissue and the only difference between the two AXB modes is in the final dose calculation step.
For the comparison between the two AXB modes, only the Lung site showed significant differences in average percent MU variation. AXB-Dw predicts lower dose to the PTV which would constitute an underdose to the target. There was no obvious explanation as to why this was the case.
Conclusion
The results presented showed that the effect of a high density object in the PTV will only be significant if a large portion of the target includes high Z materials (e.g., sometimes a physician would include teeth, part of skull in the target contour). Then, we may see hot spots in the target. If the bone density is only 20–50 % higher than water, the effect is much reduced, and the dose could be different by 3–5 % between AXB-Dm and AXB-Dw.
Overall, the dose differences between AXB-Dm, AXB-Dw and AAA are small in regions that have densities close to water (<2.0 %) and therefore, no radical changes to existing dose regimes or prescriptions is foreseen. It should be noted that by selecting AXB-Dw as opposed to AXB-Dm there may be dose differences as large as 4.6 % in non-water biological media (e.g., compact bone) between the two AXB modes. This difference becomes clinically significant if an OAR is receiving doses close to its tolerance dose limit which can influence selection or rejection of a particular plan. However, this dose difference should not have major consequences as the body is made up of approximately 75 % water and the majority of the treatment sites are in tissue with density close to water.
As most of the clinical experience is dose-to-water based and calibration protocols and clinical trials are also dose-to-water based and there still exists uncertainties in converting CT number to medium, we strongly recommend using AXB-Dw.
References
Fogliata A, Nicolini G, Clivio A, Vanetti E, Cozzi L (2011) Dosimetric evaluation of Acuros XB advanced dose calculation algorithm in heterogeneous media. Radiat Oncol 6:82
Fogliata A, Nicolini G, Clivio A, Vanetti E, Cozzi L (2012) Critical appraisal of Acuros XB and anisotropic analytic algorithm dose calculation in advanced non-small-cell lung cancer treatments. Int J Radiat Oncol Biol Phys 83(5):1587–1595
Kathirvel M, Subramanian S, Clivio A, Arun G, Fogliata A, Nicolini G, Subramani V, Thirumalai Swamy S, Vanetti E, Cozzi L (2013) Critical appraisal of the accuracy of Acuros-XB and anisotropic analytical algorithm compared to measurement and calculations with the compass system in the delivery of RapidArc clinical plans. Radiat Oncol 8(1):140
Ono K, Endo S, Tanaka K, Hoshi M, Hirokawa Y (2010) Dosimetric verification of the anisotropic analytical algorithm in lung equivalent heterogeneities with and without bone equivalent heterogeneities. Med Phys 37(8):4456–4463
Robinson D (2008) Inhomogeneity correction and the analytic anisotropic algorithm. J Appl Clin Med Phys 9(2):2786
Vassiliev ON, Wareing TA, Davis IM, McGhee J, Barnett D, Horton JL, Gifford K, Failla G, Titt U, Mourtada F (2008) Feasibility of a multigroup deterministic solution method for three-dimensional radiotherapy dose calculations. Int J Radiat Oncol Biol Phys 72(1):220–227
Failla GA, Wareing T, Archambault Y, Thompson S Acuros XB Advanced dose calculation for the eclipse treatment planning system. Varian Medical Systems, Clinical Perspectives, Acuros XB
Kroon PS, Hol S, Essers M (2013) Dosimetric accuracy and clinical quality of Acuros XB and AAA dose calculation algorithm for stereotactic and conventional lung volumetric modulated arc therapy plans. Radiat Oncol 8(1):149
Fogliata A, Nicolini G, Vanetti E, Clivio A, Cozzi L (2006) Dosimetric validation of the anisotropic analytical algorithm for photon dose calculation: fundamental characterization in water. Phys Med Biol 51(6):1421–1438
Knoos T, Wieslander E, Cozzi L, Brink C, Fogliata A, Albers D, Nystrom H, Lassen S (2006) Comparison of dose calculation algorithms for treatment planning in external photon beam therapy for clinical situations. Phys Med Biol 51(22):5785–5807
Bush K, Gagne I, Zavgorodni S, Ansbacher W, Beckham W (2011) Dosimetric validation of Acuros XB with Monte Carlo methods for photon dose calculations. Med Phys 38(4):2208–2221
Han T, Mikell JK, Salehpour M, Mourtada F (2011) Dosimetric comparison of Acuros XB deterministic radiation transport method with Monte Carlo and model-based convolution methods in heterogeneous media. Med Phys 38(5):2651–2664
Dogan N, Siebers JV, Keall PJ (2006) Clinical comparison of head and neck and prostate IMRT plans using absorbed dose to medium and absorbed dose to water. Phys Med Biol 51(19):4967–4980
Fippel M, Nusslin F (2000) Comments on ‘Converting absorbed dose to medium to absorbed dose to water for Monte Carlo based photon beam dose calculations’. Phys Med Biol 45(8):L17–L19
Liu HH, Keall P (2002) Dm rather than Dw should be used in Monte Carlo treatment planning. Med Phys 29(5):922–923
Ma CM, Li J (2011) Dose specification for radiation therapy: dose to water or dose to medium? Phys Med Biol 56(10):3073–3089
Siebers JV, Keall PJ, Nahum AE, Mohan R (2000) Converting absorbed dose to medium to absorbed dose to water for Monte Carlo based photon beam dose calculations. Phys Med Biol 45(4):983–995
Siebers JV, Keall PJ, Nahum AE, Mohan R (2000) Reply to comments on converting absorbed dose to medium to absorbed dose to water for Monte Carlo based photon beam dose calculations. Phys Med Biol 45(8):L18–L19
Chetty IJ, Curran B, Cygler JE, DeMarco JJ, Ezzell G, Faddegon BA, Kawrakow I, Keall PJ, Liu H, Ma CM, Rogers DW, Seuntjens J, Sheikh-Bagheri D, Siebers JV (2007) Report of the AAPM TASK Group No. 105: issues associated with clinical implementation of Monte Carlo-based photon and electron external beam treatment planning. Med Phys 34(12):4818–4853
Walters BR, Kramer R, Kawrakow I (2010) Dose to medium versus dose to water as an estimator of dose to sensitive skeletal tissue. Phys Med Biol 55(16):4535–4546
Hirata K, Nakamura M, Yoshimura M, Mukumoto N, Nakata M, Ito H, Inokuchi H, Matsuo Y, Mizowaki T, Hiraoka M (2015) Dosimetric evaluation of the Acuros XB algorithm for a 4MV photon beam in head and neck intensity-modulated radiation therapy. J Appl Clin Med Phys 16(4):5222
Kan MW, Leung LH, Yu PK (2013) Dosimetric impact of using the Acuros XB algorithm for intensity modulated radiation therapy and RapidArc planning in nasopharyngeal carcinomas. Int J Radiat Oncol Biol Phys 85(1):e73–e80
Rana S, Pokharel S (2014) Dose-to-medium vs. dose-to-water: dosimetric evaluation of dose reporting modes in Acuros XB for prostate, lung and breast cancer. Int J Cancer Ther Oncol 2(4):020421
Fogliata A, Scorsetti M, Navarria P, Catalano M, Clivio A, Cozzi L, Lobefalo F, Nicolini G, Palumbo V, Pellegrini C, Reggiori G, Roggio A, Vanetti E, Alongi F, Pentimalli S, Mancosu P (2013) Dosimetric comparison between VMAT with different dose calculation algorithms and protons for soft-tissue sarcoma radiotherapy. Acta Oncol 52(3):545–552
Menzel HG, Wambersie A, Jones DTL, Dawson P, DeLuca PM, Doi K, Fantuzzi E, Gahbauer RA, Michael BD, Paretzke HG, Seltzer SM, Tatsuzaki H, Whitmore GF, Allisy A (2010) Prescribing, Recording and Reporting Photon-Beam Intensity-Modulated Radiation Therapy (IMRT). J ICRU, ICRU Report 83
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zifodya, J.M., Challens, C.H.C. & Hsieh, WL. From AAA to Acuros XB-clinical implications of selecting either Acuros XB dose-to-water or dose-to-medium. Australas Phys Eng Sci Med 39, 431–439 (2016). https://doi.org/10.1007/s13246-016-0436-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-016-0436-z