Abstract
Purpose
Failure of transcatheter heart valves (THV) may potentially be treated with repeat transcatheter aortic valve implantation (redo TAVI). We assessed hydrodynamic performance, stability and pinwheeling utilizing the ALLEGRA (New Valve Technology, Hechingen, Germany) THV, a CE approved and marketed THV in Europe, inside different THVs.
Methods
Redo TAVI was simulated with the 27 mm ALLEGRA THV at three implantation depths (−4 mm, 0 mm and +4 mm) in seven different ‘failed’ THVs: 26 mm Evolut Pro, 25 mm Lotus, 25 mm JenaValve, 25 mm Portico, 23 mm Sapien 3, 27 mm ALLEGRA and M ACURATE neo. Hydrodynamic evaluation was performed according to International Standards Organization 5840-3:2021.
Results
The ALLEGRA THV was stable with acceptable performance (gradient <20 mmHg, effective orifice area >2 cm2, and regurgitant fraction <20%) in all ‘failed’ THVs except the Evolut Pro at −4 mm implantation depth. In this configuration, the outflow of the ALLEGRA frame was constrained by the Evolut Pro THV and the ALLEGRA leaflets were unable to fully close. Pinwheeling was severe for the ALLEGRA in Evolut Pro. The neo-skirt was higher with taller frame THVs.
Conclusion
The ALLEGRA THV had favorable hydrodynamic performance, stability and pinwheeling in all redo TAVI samples except the Evolut Pro at low implantation depth with compromised function. The choice of initial THV may have late implications on new THV choice and function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transcatheter aortic valve implantation (TAVI) indications are expanding and TAVI is increasingly being performed in patients with longer life expectancy.6,10 Given the bioprosthetic nature of transcatheter heart valves (THV), they may eventually fail and require repeat intervention (redo TAVI).5 Recently, redo TAVI (deployment of a new THV into a failed THV) has shown to be feasible and safe with both balloon- or self-expandable devices,5 but the impact of different THV platforms and implantation technique of redo TAVI on hydrodynamic performance is unknown. This knowledge gap is furthered by the limited clinical experience with newer THV platforms being considered for use in redo TAVI procedures. Moreover, the impact of the choice of a first THV on the outcome of a later redo TAVI procedure is poorly understood. These knowledge gaps can be partially addressed through bench testing, which may provide guidance to operators, when clinical experience is limited.
Therefore, we aimed to evaluate the use of the self-expandable ALLEGRA THV (New Valve Technology, Hechingen, Germany), a CE approved and marketed THV in Europe, in a bench study of redo TAVI. The ALLEGRA THV has demonstrated favourable outcomes in both native aortic stenosis and valve-in-valve (ViV) procedures in failed surgical bioprosthesis.2,9,17 Acceptable hydrodynamic performance has been shown with the ALLEGRA THV, even in small (labeled size <23 mm) surgical bioprosthesis.11 However, the optimum implantation technique with the ALLEGRA THV and subsequent impact on function in redo TAVI remains unknown. We assessed the hydrodynamic performance, stability, and pinwheeling of redo TAVI utilizing the ALLEGRA THV platform.
Materials and Methods
Testing was performed at the Cardiovascular Translational Laboratory (Vancouver, Canada) and New Valve Technology (Hechingen, Germany). Redo TAVI was evaluated with the 27 mm ALLEGRA THV in 7 ‘failed’ THVs that would be able to be implanted into an area of 338–430 mm2 and/or a diameter of 22–25 mm and/or a perimeter of 62.8–79 mm.4,8,13,14,15,16 ‘Failed’ valves constituted new/non-implanted THVs at nominal deployment meant to model a failed THV.
Valves
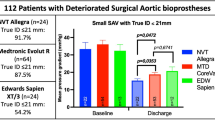
The ‘failed’ THV included the 26 mm Evolut Pro (Medtronic, Minneapolis, MN, USA), 25 mm Lotus (Boston Scientific, Lotus, Marlborough, MA), 25 mm JenaValve (JenaValve Technology GmbH, Munich, Germany), 25 mm Portico (Abbott Vascular, Santa Clara, CA), 23 mm Sapien 3 (Edwards Lifesciences Inc., Irvine, CA), 27 mm ALLEGRA and M ACURATE neo (Boston Scientific Corporation, Natick, MA). Redo TAVI configurations are presented in Fig. 1.
Redo TAVI multimodality imaging, hydrodynamic performances, and neo-skirt measurements for all redo TAVI configurations with the 27 mm ALLEGRA THV. Redo TAVI multimodality imaging, hydrodynamic performances, and neo-skirt measurements for all redo TAVI configurations with the 27 mm ALLEGRA THV in the 26 mm Evolut Pro, 25 mm Lotus, 25 mm Jena-valve, 25 mm Portico, 23 mm Sapien 3 and M ACURATE neo THVs at −4, 0 and +4 mm implantation depths. Mean PG denotes mean gradient (mmHg), EOA denotes effective orifice area (cm2) and RF denotes regurgitant fraction (%).
The ALLEGRA THV is a self-expanding valve with a tri-leaflet design made of bovine pericardial attached to a nitinol stent frame, available in three sizes (23, 27 and 31 mm) and with a supra-annular leaflet design.17 The 27 mm ALLEGRA THV inflow and outflow diameters are 27.4 mm and 24.0 mm, respectively, the maximal diameter is 28 mm at the top of the leaflets and the frame height is 41.3 mm according to manufacturers (Fig. 2).17 The skirt height for the 27 mm ALLEGRA THV is 15 mm.
27 mm ALLEGRA dimensions, implantation depth measurement and material testing machine. (a) 27 mm ALLEGRA dimensions: inflow and outflow diameters are 27.4 mm and 24.0 mm, respectively and frame height is 41.3 mm; (b) Implantation depth of the 27 mm ALLEGRA THV measured lower border of the “failed” Lotus THV stent frame to the lower border of the 27 mm ALLEGRA THV (−4 mm, 0 mm and +4 mm) on fluoroscopy; (c) Pulse duplicator used for hydrodynamic testing; (d) Zwicki-line 500N materials testing machine used for pull-out testing; (e) neo-skirt measurement from the from the inflow of the “failed” Evolut Pro THV to the top of the “failed” Evolut Pro THV leaflets jailed by the ALLEGRA THV.
The design and characteristics of the Evolut Pro, Lotus, JenaValve, Portico, Sapien 3 and ACURATE neo THVs have already been described.4,8,13,14,15,16 The smallest width of the frame diameter for the 26 mm Evolut Pro, 25 mm Lotus, 25 mm Jena-valve, 25 mm Portico, 23 mm Sapien 3 and M ACURATE neo THVs is 22 mm, 25 mm, 25 mm, 25 mm, 23 mm and 25 mm, respectively.4,8,13,14,15,16 In our study, the measured skirt height by caliper for the 26 mm Evolut Pro, 25 mm Lotus, 25 mm Jena-valve, 25 mm Portico, 23 mm Sapien 3 and M ACURATE neo THVs is 11.3 mm, 11.7 mm, 9.5 mm, 5.7 mm, 12.2 mm and 16 mm respectively.
Redo TAVI Samples
Three implantation depths (−4 mm, 0 mm and +4 mm relative to the initial THV) were tested using a 27 mm ALLEGRA THV for Redo TAVI interventions in the 7 different ‘failed’ THV. Implantation depth was measured from the lower border of the failed THV stent frame to the lower border of the 27 mm ALLEGRA THV (Fig. 2). Fluoroscopy and macroscopic caliper measurements were used to measure the implantation depth. Measurements of the neo-skirt, e.g. the length of THV skirt plus the length of the leaflets jailed between the two stent frames, were also assessed.
Imaging
Multimodality imaging including fluoroscopy and high-resolution photography was performed with each THV at each implantation depth. The latter was performed at a pre-specified magnification and fixed camera height. Fluoroscopic images were acquired at a standard adult cardiac catheterization laboratory (General Electric Healthcare, Chicago, IL, USA). High-speed video from hydrodynamic testing were also performed.11 All images and videos were recorded in a dedicated software (Carestream Health DRX-Evolution).
Hydrodynamic Assessment
A pulse duplicator with pressure transducers on the ventricular and aortic side (ViVitro Labs Inc., Victoria, Canada) (Fig. 2), was used to perform all the hydrodynamic testing according to International Standards Organization (ISO) 5840-3:2021 guidelines on in vitro pulsatile flow testing for heart valve substitutes implanted by transcatheter techniques.1
As previously described, the THVs were placed in a holder fabricated from silicone with a durometer of scale Shore A hardness of 25. Selection of sample holder hardness was made according to data on acceptable tissue compliance matched with data on the silicone material hardness scale.1 A 0.9±0.2% sodium chloride test solution maintained at 37±2 °C. THVs were tested on the aortic side of the pulse duplicator with a Mitroflow 29 on the mitral side of the pulse duplicator. Results taken from 10 consecutive cycles were averaged. High-speed video was captured at each step condition. Pulsatile forward flow performance was tested at a nominal beat rate of 70±1 beats per minute, systolic duration of 35 ± 5%, mean aortic pressure of 80 to 120 ± 2 mmHg, and simulated cardiac output of 5 ± 0.1 liters per minute. All measurements were assessed after 15 min. The pressures were measured continuously throughout the entire cardiac cycle. Mean gradient (mmHg), regurgitant fraction (RF) (%) and effective orifice area (cm2) were assessed. Regurgitant fraction was measured via the flow meter integrated into the ViVitro Pulse duplicator and effective orifice area was measured based on flow and pressure data.
The RF, mean gradient and effective orifice area (EOA) for a 27 mm THV required for a minimum performance are <20%, <20 mmHg and <2 cm2 according to the ISO standards, respectively. The effective orifice area (EOA) was defined according to a simplified version of the Bernoulli equation, as previously described.1
Pinwheeling
According to ISO guidelines for THV testing, pinwheeling is defined as twisting of the leaflet free edges resulting from excessive leaflet redundancy.1 High-speed videos with backward pressure were used to assess the degree of pinwheeling. The degree of pinwheeling was assessed based on visual estimation, in diastole.
Pull-Out Force
The samples implanted at the implantation height with the best hydrodynamic performance for each of the ‘failed’ THV underwent additional testing including pull-out force assessment. Briefly, pull-out force testing was done using a Zwicki-line 500N materials testing machine with extraction of the ALLEGRA THV from the ‘failed’ THVs (Fig. 2). For the tests, a specially designed device was used to pull ALLEGRA vertically out of the failed THV. The pull-out was performed at a slow and steady speed. Pull-out force was assessed to establish stability of the anchorage of the ALLEGRA THV in failed THVs.
Neo-skirt
The neo-skirt was measured from the inflow of the “failed” THV to the top of the “failed” THV leaflets jailed by the ALLEGRA THV in redo TAVI (Fig. 2).
Ethical and Statistics
This study was a purely bench study with no human or animal participants, and ethics approval was not required. Hydrodynamic variables are reported as mean ±SD. Statistical analyses were performed with SPSS version 24 (IBM Corp, Armonk, NY, USA).
Results
Hydrodynamic Function
Hydrodynamic measurements were feasible in all failed THVs at −4 mm, 0 mm, and +4 mm implant depth except for the ALLEGRA 27 mm in the Evolut Pro THV at −4 mm implantation depth. In this position, the ALLEGRA frame at its outflow (normally 28 mm at the top of the leaflets) was severely constrained by the Evolut Pro waist (normally 22 mm). As a result of the constrained frame, the ALLEGRA leaflets were unable to fully close, and did not allow for hydrodynamic testing in this configuration (Fig. 3, Video 1).
The 27 mm ALLEGRA in “failed” 26 mm Evolut Pro THV at −4 mm implantation depth (a) Constrained ALLEGRA THV frame (28 mm at the leaflets top, red line) by the waist of the Evolut Pro THV (22 mm, black arrow); high-speed video image showing ALLEGRA leaflets redundancy and pinwheeling (b, c), unable to close completely (diastole phase, red circle) (d), and opening during systole (e).
Transvalvular Gradient
The transvalvular gradient was < 20 mmHg in the 7 “failed” THVs with the 27 mm ALLEGRA THV at all feasible implant depths. Mean transvalvular gradient according to failed THV type and implantation depth are presented in Table 1 and Figs. 1, 4. A higher implantation (+4 mm) was associated with a slightly lower mean gradient for the Evolut Pro (10.6 ± 0.08 mmHg), Lotus (8.4 ± 0.08 mmHg), Portico (8.9 ± 0.3 mmHg), ALLEGRA (8.5 ± 0.09 mmHg) and the ACURATE Neo (9.1 ± 0.8 mmHg). The mean gradient was <20 mmHg and similar at all implantation depths for the Sapien 3 THV. A lower mean gradient was obtained at an implantation depth of 0 mm with the JenaValve THV (7.6 ± 0.4 mmHg).
High-quality photography, fluoroscopy images and mean transvalvular gradient according to failed THV type and implantation depth. (a) 27 mm ALLEGRA in 26 mm Evolut Pro; (b) 27 mm ALLEGRA in 25 mm Lotus; (c) 27 mm ALLEGRA in 25 mm JenaValve; (d) 27 mm ALLEGRA in 25 mm Portico; (e) 27 mm ALLEGRA in 27 mm ALLEGRA; (f): 27 mm ALLEGRA in M ACURATE Neo.
Effective Orifice Area
EOA according to failed THV type and implantation depth are reported in Table 2 and Fig. 1. The EOA was acceptable and >2 cm2 in all failed THV with the ALLEGRA THV according to ISO guidelines. Higher implantation depth was associated with lower EOAs for the JenaValve THV with EOAs of 2.4 ± 0.05, 2.5 ± 0.07 and 2.1 ± 0.009 at −4 mm, 0 mm and +4 mm respectively.
Low implantation depth was associated with lower EOA for the ALLEGRA in ALLEGRA THV with EOAs of 2.1 ± 0.01, 2.3 ± 0.04 and 2.3 ± 0.01 at −4 mm, 0 mm and +4 mm, respectively, and for the ALLEGRA in Lotus with EOAs of 2.1 ± 0.02, 2.3 ± 0.02 and 2.4 ± 0.02 at −4 mm, 0 mm and +4 mm respectively. For the Sapien 3, Portico and the ACURATE neo THV, EOAs were similar regardless the implantation depth. The EOAs were lower for the Evolut with EOAs of 2.0 ± 0.02 and 2.1 ± 0.007 at 0 mm and +4 mm, respectively.
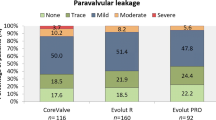
Regurgitant Fraction
RF for the failed THV at different implantation depths are reported in Table 3 and Fig. 1. The RF was acceptable (< 20%) at all implantation depth for all THVs. A higher RF was found with the ACURATE Neo THV (16.5 ± 0.3, 16.3 ± 0.07 and 15.8 ± 0.08 at −4 mm, 0 mm and +4 mm, respectively) and for the Portico THV (13.9 ± 0.6, 17.2 ± 0.1 and 11.9 ± 0.3 at −4 mm, 0 mm and +4 mm, respectively) regardless of implantation depth. Implantation depth had an impact on the RF for the ALLEGRA and the Evolut THVs with higher RF at 0 mm (11.9 ± 0.5) and +4 mm (10.7 ± 0.8) implantation depth, respectively. The failed THVs were not sealed into the silicon rings, so that RF was a combination of both paravalvular and intravalvular regurgitation for both THVs in the setup.
Pinwheeling
The degree of ALLEGRA leaflet pinwheeling in different failed THV is shown in Fig. 5. Pinwheeling was more pronounced in the Evolut Pro THV at all implantation depths and the ALLEGRA leaflets were unable to close totally at −4 mm implantation depth. The degree of pinwheeling was lower for high implantation depth and similar for the Lotus, JenaValve, Portico, Sapien 3 and ACURATE neo THVs. A lower implantation depth was associated with worse but minimal pinwheeling in all THVs configuration.
Pull-Out Force
Pull-out force assessment showed stability of the ALLEGRA THV in all “failed” THVs.
The highest pull-out force (8.2 and 8.5 N) was measured with the ACURATE Neo and the Evolut Pro THVs, respectively, resulting in a worse pinwheeling. The lowest pull-out force (1.8 N) was obtained with the ALLEGRA THV regarding a larger minimal inner THV diameter.
Neo-skirt
The neo-skirt was higher for the tall frame THVs including the ACURATE Neo, the ALLEGRA, the Evolut Pro and the Portico THVs (32 mm, 29 mm, 25 mm and 20 mm respectively), Fig. 1. Compared to baseline THV skirt, the neo-skirt height increase was greater for the ACURATE Neo (+16 mm), the ALLEGRA (+14 mm), the Portico (+14.3 mm) and the Evolut Pro (+13.7 mm) THVs. The increase in the neo-skirt was minimal for the short frame THVs including the JenaValve (+7 mm), the Lotus (+2 mm) and the Sapien 3 (+2 mm) THVs.
Discussion
This study assessed the ALLEGRA THV in different “failed” THVs providing insights on performance, stability and impact of implantation depth in redo TAVI with the ALLEGRA THV.
Clinical experience utilizing the ALLEGRA THV in redo TAVI is limited, and bench testing can provide important insights. A recent multicentre registry has shown safety and feasibility of redo TAVI in patients with THV dysfunction.5 However, the ALLEGRA THV was not utilized in this multicentre study and the optimal THVs combination in redo TAVI as well as the optimal implantation depth remain unknown to date. In our study, redo TAVI with the ALLEGRA THVs showed favorable hydrodynamic performances regarding the mean gradient, EOAs and RF for all tested THVs except the Evolut Pro THV at low implantation depth. Additionally, implantation depth did not have a significant impact on performance with acceptable hydrodynamic function even with low implantation depths. Bench studies including different THVs platforms have previously shown that a higher implantation depth was desirable to obtain favorable hydrodynamic performances for TAVI in failed surgical valves.12 In contrast a bench study assessing implantation depth of the ALLEGRA THV showed favorable performance at all implantation depths in surgical valve prosthesis,11 similarly to our findings. This may be related to the supra-annular position of the ALLEGRA THV leaflets or its unique barrel-like frame design resulting in minimal interaction between the frame of the Allegra and the previously implanted THV. This highlights the need to assess each novel THV design on its own merits. Valves may perform differently despite having a similar mode of deployment or leaflet position to established THV platforms.
In the present study, the only non-functional configuration was the ALLEGRA in the Evolut Pro THV at low implantation depth (−4 mm). In this configuration, the ALLEGRA THV frame was constrained by the Evolut Pro, and the ALLEGRA leaflets were unable to close completely, preventing adequate hydrodynamic assessment. As the waist of the 26 mm Evolut Pro is 22 mm, this limited frame expansion of the ALLEGRA at low implantation depth, which normally expands to 28 mm diameter at the leaflet level. Redo TAVI using ALLEGRA at low implantation depth in an Evolut Pro is an undesirable configuration, which compromises leaflet function.
Similarly, leaflet pinwheeling was acceptable for all THVs combination, except for the Evolut Pro THV. However, pinwheeling was slightly worse in low implantation depth (−4 mm) in all configurations. For the redo TAVI configuration including the Evolut Pro THV, the pinwheeling was severe at all implantation depths and worse at low implantation depth. Pinwheeling may increase mechanical leaflet stress and increase the risk of THV thrombosis and degeneration.7,12
A higher neo-skirt was observed following redo TAVI with the Allegra THV in tall frame valves with a supra-annular leaflet position. This is consistent with a recent study showing a higher neo-skirt assessed on computed tomography scan in redo TAVI in tall frame THVs.3 A higher neo-skirt may increase the risk of coronary obstruction or compromise future coronary access. Indeed, in the study of De Backer et al. evaluating the feasibility of coronary access after redo TAVI, the authors highlighted that a coronary ostium below the neo-skirt was associated with a potentially higher risk of impaired coronary access.3
Taking all this into consideration, both the second THV as well as the first THV selection when performing the initial TAVI procedure must be considered. Indeed, our study shows that the impact of the choice of the first THV on the performance of the THV used in the redo TAVI procedure can be significant. Other factors such as implantation depth had less of an effect on the results as the choice of the type of first THV, in the case of redo TAVI using the ALLEGRA THV.
Limitations
Bench testing may not reflect physiological conditions in clinical practice. THV anchoring and interaction with the “failed” THV may be different using normal THVs for bench- testing compared to degenerated and calcified failed THVs in clinical practice. Indeed, explanted THVs are challenging to obtain and failed THVs are very difficult to properly replicate. Given limited THV availability for bench studies, only one THVs range size was utilized in this study, not allowing testing of different THVs size combinations. Moreover, the same THV was used for different implantation depth for each THVs combination. However, given the limited assessed implantation depths (3), these serial deployments are unlikely to damage THV function. Finally, in a degenerated in vivo failed valve which is calcified, the paravalvular leak may vary compared to our findings.
Conclusion
The ALLEGRA THV had favorable hydrodynamic performance, stability and pinwheeling in all redo TAVI samples except the Evolut Pro THV at low implantation depth. Low implantation of the ALLEGRA in a tall frame Evolut Pro THV is associated with constrained ALLEGRA expansion and compromised function.
References
Cardiovascular implants - cardiac valve prosthesis. Part 3: Heart valve substitutes implanted by trans catheter techniques. In: organization Is, editor. Geneva, Switzerland: International standard organization; 2013.
Cuevas, O., R. Moreno, V. Pascual-Tejerina, S. Toggweiler, M. Brinkert, J. Baz, et al. The Allegra transcatheter heart valve: European multicentre experience with a novel self-expanding transcatheter aortic valve. EuroIntervention. 15:71–73, 2019. https://doi.org/10.4244/EIJ-D-18-00861.
DeBacker, O., U. Landes, A. Fuchs, S.-H. Yoon, O. N. Mathiassen, A. Sedaghat, et al. Coronary Access After TAVR-in-TAVR as Evaluated by Multidetector Computed Tomography. JACC Cardiovascular Interventions. 13:2528–2538, 2020. https://doi.org/10.1016/j.jcin.2020.06.016.
Hellhammer, K., K. Piayda, S. Afzal, L. Kleinebrecht, M. Makosch, I. Hennig, et al. The latest evolution of the medtronic corevalve system in the era of transcatheter aortic valve replacement: matched comparison of the Evolut PRO and Evolut R. JACC Cardiovasc Interv. 11(22):2314–2322, 2018.
Landes, U., J. G. Webb, O. De Backer, L. Sondergaard, M. Abdel-Wahab, L. Crusius, et al. Repeat transcatheter aortic valve replacement for transcatheter prosthesis dysfunction. J Am Coll Cardiol. 75(16):1882–1893, 2020. https://doi.org/10.1016/j.jacc.2020.02.051.
Mack, M. J., M. B. Leon, V. H. Thourani, R. Makkar, S. K. Kodali, M. Russo, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 380(18):1695–1705, 2019. https://doi.org/10.1056/NEJMoa1814052.
Midha, P. A., V. Raghav, J. F. Condado, I. U. Okafor, S. Lerakis, V. H. Thourani, et al. Valve type, size, and deployment location affect hemodynamics in an in vitro valve-in-valve model. JACC. 9:1618–1628, 2016. https://doi.org/10.1016/j.jcin.2016.05.030.
Perlman, G. Y., A. Cheung, E. Dumont, D. Stub, D. Dvir, M. Del Trigo, et al. Transcatheter aortic valve replacement with the Portico valve: one-year results of the early Canadian experience. EuroIntervention. 12(13):1653–1659, 2017.
Pighi, M., M. Lunardi, and F. L. Ribichini. NVT ALLEGRA transcatheter heart valve for valve-in-valve procedures in failing surgical aortic bioprostheses: let us wait and see. EuroIntervention. 15(9):e739–e741, 2019. https://doi.org/10.4244/EIJV15I9A137.
Popma, J. J., G. M. Deeb, S. J. Yakubov, M. Mumtaz, H. Gada, D. O’Hair, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 380(18):1706–1715, 2019. https://doi.org/10.1056/NEJMoa1816885.
Sathananthan, J., R. Fraser, M. Kütting, M. Hensey, U. Landes, A. Alkhodair, et al. Impact of implant depth on hydrodynamic function of the ALLEGRA bioprosthesis in valve-in-valve interventions. EuroIntervention. 15:e1335–e1342, 2020. https://doi.org/10.4244/EIJ-D-19-00782.
Sathananthan, J., R. Fraser, U. Landes, C. Rich, S. L. Sellers, J. Leipsic, et al. Repeat transcatheter aortic valve replacement and implications for transcatheter heart valve performance: insights from bench testing. EuroIntervention. 2021. https://doi.org/10.4244/EIJ-D-20-00697.
Sathananthan, J., S. L. Sellers, R. Fraser, D. Dvir, M. Hensey, D. J. Murdoch, et al. Impact of implant depth on hydrodynamic function with the ACURATE neo transcatheter heart valve following valve-in-valve transcatheter aortic valve replacement in Mitroflow bioprosthetic valves: an ex vivo bench study. EuroIntervention. 15(1):78–87, 2019.
Seigerman, M. E., A. Nathan, and S. Anwaruddin. the lotus valve system: an in-depth review of the technology. Curr Cardiol Rep. 21:157, 2019. https://doi.org/10.1007/s11886-019-1234-5.
Treede, H., A. Rastan, M. Ferrari, S. Ensminger, H.-R. Figulla, and F.-W. Mohr. JenaValve. EuroIntervention. 8:88–93, 2012. https://doi.org/10.4244/EIJV8SQA16.
Webb, J., G. Gerosa, T. Lefèvre, J. Leipsic, M. Spence, M. Thomas, et al. Multicenter evaluation of a next-generation balloon-expandable transcatheter aortic valve. J Am Coll Cardiol. 64(21):2235–2243, 2014. https://doi.org/10.1016/j.jacc.2014.09.026.
Wenaweser, P., S. Stortecky, T. Schütz, F. Praz, S. Gloekler, S. Windecker, et al. Transcatheter aortic valve implantation with the NVT Allegra transcatheter heart valve system: first-in-human experience with a novel self-expanding transcatheter heart valve. EuroIntervention. 12(71–77):1, 2016. https://doi.org/10.4244/EIJV12I1A13.
Funding
This study has no relevant funding
Author information
Authors and Affiliations
Contributions
MA: Conceptualization, Formal analysis, Methodology, Visualization, Writing—original draft, Writing—review & editing; MK: Conceptualization, Formal analysis, Methodology, Visualization, Validation, Writing—review & editing; SS: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Visualization, Writing—review & editing; AK: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing—review & editing; PM: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing—review & editing; IK: Methodology, Visualization, Writing—review & editing; JL Writing—review & editing ; LS Writing—review & editing; ST Writing—review & editing ; DA Visualization, Writing—review & editing ; JG W Visualization, Writing—review & editing ; JS Conceptualization, Formal analysis, Methodology, Supervision, Visualization, Validation, Writing—original draft, Writing—review & editing
Corresponding author
Ethics declarations
Data availability
Yes
Code availability
Not applicable
Conflict of interest
Dr Akodad has received research funding from Medtronic, Biotronik, MUSE Explore and Federation Française de Cardiologie. Dr Kütting, A. Kirsten and Philipp Marx are employees of NVT. Dr. Sellers is supported by fellowships from the Canadian Institutes of Health Research and the Michael Smith Foundation for Health Research. Dr Leipsic is consultant to Edwards Lifesciences and provide CT core lab services for Edwards Lifesciences, Medtronic, Neovasc, Guided Delivery Systems, and Abbott, for which no direct compensation is received. Dr. Toggweiler is a proctor and consultant for Biosensors / New Valve Technology, Medtronic and Boston Scientific, a proctor for Abbott, a consultant for Shockwave, Teleflex, Medira, at Heart Medical, Veosource, has received institutional research grants from Boston Scientific and Fumedica and holds equity in Hi-D Imaging. Dr Wood is a consultant to, and has received research funding from, Edwards Lifesciences and Abbott. Dr. Webb is a consultant to, and has received research funding from, Edwards Lifesciences, Abbott, and Medtronic. Lars Sondergaard has received consultant fees and institutional research grants from Abbott, Boston Scientific, Edwards Lifesciences, Medtronic, and Symetis. Dr Sathananthan is a consultant to Edwards Lifesciences, Boston Scientific and Medtronic. He has received research funding from Medtronic and Edwards Lifesciences. The other authors do not have any relevant disclosures.
Ethical Approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Associate Editor Jamshid Karimov oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Video 1 High-speed video showing the 27 mm ALLEGRA in “failed” 26 mm Evolut Pro THV at −4 mm. Constrained ALLEGRA THV frame by the Evolut Pro THV and ALLEGRA leaflets unable to close. Supplementary file1 (MOV 3709 kb).
Rights and permissions
About this article
Cite this article
Akodad, M., Kütting, M., Sellers, S. et al. Redo Transcatheter Aortic Valve Implantation with the ALLEGRA Transcatheter Heart Valve: Insights from Bench Testing. Cardiovasc Eng Tech 13, 930–938 (2022). https://doi.org/10.1007/s13239-022-00627-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-022-00627-1