Abstract
Objectives
Previous studies have observed an increase in low frequency diastolic heart sounds in patients with coronary artery disease (CAD). The aim was to develop and validate a diagnostic, computerized acoustic CAD-score based on heart sounds for the non-invasive detection of CAD.
Methods
Prospective study enrolling 463 patients referred for elective coronary angiography. Pre-procedure non-invasive recordings of heart sounds were obtained using a novel acoustic sensor. A CAD-score was defined as the power ratio between the 10–90 Hz frequency spectrum and the 90–300 Hz frequency spectrum of the mid-diastolic heart sound. Quantitative coronary angiography analysis was performed by a blinded core laboratory and patients grouped according to the results: obstructive CAD defined by the presence of at least one ≥ 50% stenosis, non-obstructive CAD as patients with a maximal stenosis in the 25–50% interval and non-CAD as no coronary lesions exceeding 25%.
We excluded patients with potential confounders or incomplete data (n = 245). To avoid over-fitting the final cohort of 218 patients was randomly divided into to a training group for development (n = 127) and a validation group (n = 91).
Results
In both the training and the validation group the CAD-score was significantly increased in CAD patients compared to non-CAD patients (p < 0.0001). In the validation group the area under the receiver-operating curve was 77% (95% CI 63–91%). Sensitivity was 71% (95% CI 59–82%) and specificity 64% (95% CI 45–83%).
Conclusion
The acoustic CAD-score is a new, inexpensive, non-invasive method to detect CAD, which may supplement clinical risk stratification and reduce the need for subsequent non-invasive and invasive testing.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is one of the leading causes of death worldwide. Patients with suspected stable coronary ischemic syndromes and low to intermediate risk usually undergo non-invasive testing as the initial work-up. Modalities such as computerized tomographic angiography (CTA) or myocardial scientigraphy are preferred over exercise stress testing before referral for coronary angiography (CAG). However, several studies demonstrate a low prevalence of CAD and revascularization rate in patients referred for CTA and CAG.29 Despite increased use of CTA and other non-invasive modalities such as stress echocardiography and myocardial perfusion imaging, these tests have disadvantages like radiation and patient discomfort and still the low prevalence in patients undergoing CAG remains a challenge.15
In the 1960s Dock reported about diastolic murmurs in patients with CAD, referred to as the “Dock's Murmur”8. Subsequently, Semmlow et al. documented that CAD introduces changes in the frequency distribution of diastolic heart sounds a sensitive accelerometer was used for recording of diastolic heart sounds from patients undergoing CAG.1,4,28 Early studies required a soundproof room19 to identify the relative energy increase in the 300–1200 Hz frequency band, presumed to relate to murmurs originating from post-stenotic turbulence. Although the diagnostic accuracy was acceptable,3 the method was impractical with excessive influence of both ambient and physiological noise. Recent research has focused on applicability, realistic settings, robust equipment and with larger sample sizes.2,10,23,25,27 Recently, investigations have compared Makaryus et al. tested a multichannel heart sound algorithm in patients referred to CTA.5,17 It’s well established that low frequency heart sounds such as the third and the fourth heart sounds7,18 are markers of cardiovascular diseases and the most recent and largest studies in this field used very low frequency (< 100 Hz) diastolic heart sounds to differentiate CAD and non-CAD patients.7,26,30,31 In the present study, we present some of our earliest research in non-invasive method for detection of CAD based on analysis of low frequency heart sounds. In contrast to recent studies based on multi feature machine learning24,30 or deep learning20 we focus on direct analyse and quantification of the diastolic frequency spectrum of heart sounds.
Methods
The study was performed in patients referred for elective CAG at Rigshospitalet, University Hospital of Copenhagen, Denmark, during March 2010 to March 2011 (ClinicalTrials.gov Identifier NCT01090947). The study was approved by the Danish Data Protection Agency (H-1-2009-142), the Regional Ethics Committee, and followed the principles in the declaration of Helsinki. Consent was obtained from all patients before participation. The population was randomly dived into a training group used for development of the algorithm and a validation group for blinded validation of the algorithm.
Study Population
The initial population included 463 patients. Patients were recruited consecutively by the hospital staff prior to the CAG examination. The inclusion criteria were: age larger than eighteen years, referred to a diagnostic CAG examination due to suspected CAD, in a stable condition. The initial exclusion criteria were: patients with acute coronary syndrome, previous coronary artery bypass grafting, heart transplanted, or pregnancy. To simplify the signal analysis, we further excluded patients with arrhythmias (N = 58), mitral valve stenosis and aortic incompetence which all causes diastolic murmurs (N = 26), those with previous biological or mechanical valve surgery (N = 9) and patients suffering severe chronic obstructive pulmonary disease (N = 38). Furthermore, to reduce complexity, we excluded patients with recordings classified as noisy in a manual review or by the algorithm internal quality control (N = 77), and recordings where the diastasis period, defined as the period between the third and the fourth heart sound, was shorter than 100 ms (N = 30). A few with insufficient clinical data or interpretable angiograms (N = 7) were excluded.
The remaining 218 patients were randomly (60%:40%) divided into a training group (N = 127) and a validation group (N = 91). The validation group was blinded to the authors under the development and test of the method.
Recording of Heart Sounds
Heart sounds were recorded at the hospital department prior to invasive CAG examination with a novel acoustic sensor (Acarix®), and a dedicated acquisition system, see the Fig. 1.12,33 Recordings were performed at the chest wall from the left 4th intercostal space with patients placed in a supine position. To make the recording procedure more robust and less depended on the operator, the acoustic sensor was attached with a double adhesive patch to the chest wall. A recording lasted 3 min. The first minute was used to ensure steady state. The patient was then asked to hold the breath in 4 recording periods of 8 s to limit respiration noise. Between each respiration pause, the patient rested in 20 s. Only the 4 periods without respiration were used in the further analysis.
Visualizations of the steps in the estimation of the CAD-score. (a) A dedicated system to acquire Heart sounds. (b) Hearts segmented into individual heart beats and aligned to S2. (c) Diastolic power spectrums of a non-CAD and an obstructive CAD patient (PSD = power spectrum density). (d) The equation for estimation of the CAD-score from the Diastolic power spectrums. (e) Distribution of the CAD-score in the training group and validation group.
Algorithm for Pre-Processing of Heart Sounds
A dedicated signal processing and classification algorithm was developed in MATLAB, (The MathWorks Inc., Massachusetts, US). Since the coronary flow usually peaks in the diastolic period, the diastolic heart sounds were the focus of the algorithm. To limit the analysis to the diastolic period, the recordings were automatically segmented into diastolic and systolic periods using an automatic segmentation method.22 The beats were then aligned according to the second heart sound (S2) using cross correlation, see the central figure. The diastolic periods were then high-pass filtered with a 4th order Butterworth filter with cut-off frequencies at 10 Hz. To limit the influence of ambient noise, noisy diastoles were discharged automatically using the approach described in by Schmidt et al.21 Recordings with less than 8 remaining beats were excluded as noisy recordings as previously mentioned.
The Acoustic CAD-Score
The previous study of heart sounds from an electronic stethoscope24 and an initial analysis of the recordings in the training group showed an increased power of the diastolic heart sound at frequencies below 100 Hz in CAD patients compared to non-CAD patients.21 This increase was observed approximately 200 ms after the onset of S2 and continued through most of the diastole. To quantify these changes, we estimated the power spectrum density (PSD) of the diastasis period using the Welch's method. The diastasis period was automatically identified as the silent period between the third heart sound (S3) and the fourth heart sound (S4). A whitening filter, that makes the PSD of the average non-CAD patient from the training group flat, was applied to reduce spectral leakage. Since the absolute amplitude of heart sounds is influenced by several factors, the low frequency power in the 10–90 Hz range is divided by the power in the 90–300 Hz range, see the central figure and formula (1). The 10, 90 and 300 Hz limits were identified using an empirical approach in the training data. To ensure a normal distribution, the power ratio was log transformed.
Correction for Age, Gender and BMI
It is known from other technologies related to cardiac vibration, such as ballistocardiography, that there is a relationship between the low frequency chest vibrations and age. Furthermore, it is likely that the distance between the heart and the microphone influences the power ratio. Without correction, the power ratio correlated with gender (r = 0.29), age (r = 0.03) and BMI (r = − 0.26). The power ratio was therefore corrected using multivariate regression. Since the age of the patient population is rather high, we expanded the age variation by including heart sounds recorded from 30 younger asymptomatic patients (mean age 27.4 years and STD: 9.1). This population is considered a low-risk population. Before correction, the ratio was correlated with gender (r = 0.29), age (r = 0.03) and BMI (r = − 0.26). The corrected power ratio was then scaled as a score which covered a range between 0 and 100. The scale was adjusted such that 25 was the optimal threshold according to a Bayesian Classification criterion. The acoustic CAD-score is described in formula (1) where CBMI,Age,Gender is the correction factor related to BMI, age and gender.
Coronary Angiography
The coronary angiography images were analysed with quantitative coronary angiography (QCA) by an independent core-lab. Patients with at least one diameter reduction ≥ 50% were defined as patients with obstructive CAD. Patients, where the most extensive identified stenosis had a diameter reduction less than 50%, but higher than 25%, were defined as non-obstructive CAD. Patients without any identified stenosis above 25% in the QCA analysis were defined as non-CAD patients.
Statistical Analysis
The statistical difference across the three groups (non-CAD, non-obstructive CAD and obstructive CAD) was evaluated using analysis of variance (ANOVA), and the classification performances were measured using the area under the receiving operator characteristic curve (AUC). Sensitivity and specificity were estimated when the CAD-score was used as a binary classifier (CAD-score ≥ 25 = high risk, CAD-score < 25 = low risk).
Logistic regression analysis was used to compare the CAD-scores to other risk factors. A logistic regression model was built to classify non-CAD patients from obstructive CAD patients using the CAD-score, gender, age, hypertension, BMI and diabetes as independent variables. Hypertension was defined as a systolic blood pressure above 140, or if the patient received medication for high blood pressure. The independent variables were standardized to zero mean and a standard deviation at one. The standardized coefficients were used to rank the influence of each variable and t-statistics were used to estimate the significance of each variable. All statistical analyses were conducted in MATLAB (The MathWorks Inc., Massachusetts, US).
To test if the location of the stenosis and the number of diseased vessels influence the CAD-score, patients were grouped according to the number of diseased vessels (1, 2 or 3). Patients with single vessel disease were further grouped as right coronary artery (RCA), left anterior descending (LAD) or left circumflex artery (LCX) depend on the location of the significant stenosis. Left main was included in LAD. The sensitivity and the mean CAD-score were estimated in each group, and a potential difference between the vessel groups was validated using ANOVA.
Results
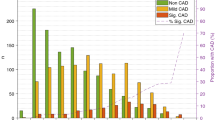
The QCA analysis of the training group identified 79 obstructive CAD patients, 33 non-CAD patients and 15 patients with non-obstructive CAD, whereas the validation group included 58 obstructive CAD patients, 25 non-CAD patients and 8 patients with non-obstructive CAD. The baseline characteristics and CAD-score can be seen in Table 1. The CAD-score differed significantly across the three groups (non-CAD, non-obstructive CAD and obstructive CAD) in both the training and the validation group. The CAD-score was significantly lower in non-CAD patients compared to obstructive CAD patients in both datasets. The mean CAD-score was 21.6 ± 10 and 32.4 ± 11 in non-CAD and obstructive CAD patients, respectively, in the validation group (p < 0.0001), and 21.8 ± 7.3 and 32.2 ± 12 respectively, in the training group (p < 0.00001). However, the non-obstructive CAD patients did not differ significantly from the obstructive CAD patients in either dataset (p = 0.79 and p = 0.19), but this group did differ significantly from the non-CAD patients in the training group (p = 0.004), but not in the validation group (p = 0.25). There was no statistically significant difference between the CAD-score in the training group and validation group (p = 0.79). The distribution of the score in both the training and the validation group are seen in the central figure.
The mean PSD’s from obstructive CAD and non-CAD patients are seen in Fig. 1 from both the training and the validation group. A clear increase in energy below 100 Hz in obstructive CAD patients is observed in both datasets.
Diagnostic Accuracy of the CAD-Score
When the CAD-score was used to separate the non-CAD patients from obstructive CAD patients the AUC was 78% (95% CI 68–88) in the training group, and 77% (95% CI 63–91) in the validation group (Fig. 2). The sensitivity and specificity of the CAD-score were 73% (95% CI 64–83%) and 76% (95% CI 61–90%), respectively, in the training group, and 71% (95% CI 59–82%) and 64% (95% CI 45–83%), respectively, in the validation group. Combining patients classified as non-obstructive CAD (25 to 50% reduction in diameter stenosis) with the non-CAD patients, the AUC drops to 71 (95% CI 61–80%) in the training group and 73 (95% CI 62–84%) in the validation group (Fig. 3).
The diastolic power spectrums for obstructive CAD (red) and non-CAD patients (green) in the training and the validation group. The full line is the average power spectrum density (PSD) from all obstructive CAD patients and the dashed line is the average PSD from all non-CAD patients. As seen is the energy of sound higher at frequencies below 100 Hz in the obstructive CAD-patients.
The CAD-Score and Subgroups
The training group and the validation group were pooled to one dataset to further analyse the CAD-score. The classification performance of the CAD-score was similar in females, AUC = 77% (95% CI 65–89), and males, AUC = 77% (95% CI 67–87). As seen in Table 2 the CAD-score was numerically more sensitive in patients with 3-vessel disease compared to 2-vessel or single vessel disease, however not reaching statistically significance (p = 0.31). There was a similar sensitivity for detection of CAD between the 3 major coronaries (p = 0.44). Dividing the stenosis location into either distal, mid or proximal show a slightly lower CAD-score when the stenosis was placed distal, but this was not statistically significant (p = 0.86).
Multivariate Analysis
As seen in Table 1, both age and the proportion of patients with high blood pressure differed significantly between the non-CAD, non-obstructive CAD and the obstructive CAD patients. However, the CAD-score was clearly the domination predictor of obstructive CAD in the multiple regression analysis, see Table 3. Only the CAD-score and hypertension contributed significantly to identification of obstructive CAD patients in the logistic regression analysis.
Discussion
The robust difference between the CAD-score in the obstructive CAD patients and non-CAD patients in both the training group and the blinded test/validation dataset confirms a change in the low frequency distribution of diastolic heart sounds in obstructive CAD patients. Thereby the initial findings observed with an electronic stethoscope24 are confirmed by the current study. The data obtained in the current study with the prototype device was used for further development of the CAD-score algorithm, e.g. by inclusion of adaptive noise cancelation to remove noise from the audio recordings. Furthermore, the current study underlines the findings of the recent studies based on fully developed systems.5,31 The contribution of the current paper is the demonstration that low frequency diastolic heart sound is increased in subjects with CAD and that a simple quantification of the diastolic frequency spectrum can provided valuable information in the assessment of patients with suspected CAD.
Diagnostic Potential
The diagnostic performance showing an AUC at 73% (95% CI 62–85%) in discrimination obstructive CAD patients from other patients, significantly exceeds most AUC values (56–73%) reported from ECG stress testing using the Duke score.9,11,16,32 Compared to ECG stress testing and other test modalities an Acoustic CAD-score system has several advantages. Examinations with the Acoustic CAD-score are very fast, less than 15 min in total, and a test will be easy to use for medically trained personal. In addition, the CAD-score examination does not cause any risk to the patient as other modalities.9,14 The relatively simple hardware, a good microphone and a micro processer might facilitate low cost examinations. These characteristics make the CAD-score suited for use outside major hospitals, for instance in the doctor’s office in primary care, thereby the CAD-score test might already be used at the first patient encounter for risk stratification in symptomatic patients. Combined with risk stratification based on traditional risk factors and symptoms, the CAD-score might be used to guide if further examinations are necessary.
The study demonstrates that the CAD-score in non-obstructive CAD patients (25–50% stenosis) does not differ significantly from the obstructive CAD patients. Thereby the CAD-score’s capability shown in this study is more to identify changes in the coronary arteries than identifying stenosis that are exactly above 50% diameter reduction.
Signal Source
Previous heart sound algorithms have used the high frequency analysis of coronary artery murmurs. In the current study we did not include high frequency features due to noise contamination of the higher frequency bands. The cause of the low frequency change is unidentified, but the low frequency sound is likely due to oscillations in the myocardium. These oscillations might be due to altered diastolic filling patterns or changes in resonate frequencies of the coronary artery system due to stiffening of the arteries. The final hypothesis is in line with Jin-Zhao et al.’s findings that a stenosis in the coronary arteries will cause a low frequency component to shift to lower frequencies.13 However, recently Becker et al. demonstrated that temporal occlusion of the coronary arteries also caused a shift towards lower frequencies,6 which might indicate that the contraction patterns influence the low frequency heart sounds.
Study Limitations
In the current study a large number of patients were excluded (28%) due to comorbidities like arrhythmia, valve disease and chronic obstructive pulmonary disease. Furthermore, patients with poor audio recordings due to noise and patients with short diastases were excluded (25%). Thereby the current results might not be descriptive of broader clinical populations and a device where less than 50% of the patients qualified for analysis might be of low clinical value. A recent system30,31 has used adaptive noise cancelation to remove noise from the audio recordings, this allowed the acoustic score to be calculated in more than 90% of the patients.31 In the current study we did not control either patient medication or coffee intake before the acoustic measurements. We did not see a significant difference in CAD-score across the number of diseased vessels, however, post hoc power analysis showed a relative weak power at only 47% for this analysis.
Concluding Remarks
The results of this early clinical study suggest that CAD alters the diastolic heart sound and increases the relative power of the low frequency heart sound. In a controlled population, the current study demonstrates a diagnostic potential of the acoustic CAD-score, and that the CAD-score provides substantial information in addition to traditional risk factors such as age, high blood pressure and gender. Therefor the CAD-score might provide a diagnostic test for CAD. In contrast to the existing diagnostic modalities, the heart sound method is low cost, easy to train and use with the potential to available in the general physician office or provide more widespread CAD diagnostic capabilities in low-income countries.
References
Akay M. Automated noninvasive detection of coronary artery disease using wavelet-based neural networks. Artificial Neural Networks in Engineering–Proceedings (ANNIE’94). 1994;4:517–522.
Akay, M., Y. M. Akay, D. Gauthier, et al. Dynamics of diastolic sounds caused by partially occluded coronary arteries. IEEE Trans. Bio-med. Eng. 56:513–517, 2009.
Akay, Y. M., M. Akay, W. Welkowitz, et al. Noninvasive acoustical detection of coronary artery disease: a comparative study of signal processing methods. IEEE Trans. Bio-med. Eng. 40:571–578, 1993.
Akay, M., J. L. Semmlow, W. Welkowitz, et al. Noninvasive detection of coronary stenoses before and after angioplasty using eigenvector methods. IEEE transactions on bio-medical engineering. 37:1095–1104, 1990.
Azimpour, F., E. Caldwell, P. Tawfik, et al. Audible coronary artery stenosis. Am. J. Med. 129:S15-21, 2016.
Becker, M., A. B. Roehl, U. Siekmann, et al. Simplified detection of myocardial ischemia by seismocardiography. Differentiation between causes of altered myocardial function. Herz. 39:586–592, 2014.
Cohn, P. F., P. S. Vokonas, R. A. Williams, et al. Diastolic heart sounds and filling waves in coronary artery disease. Circulation [Internet] 44:196–202, 1971. Available from: http://ahajournals.org.
Dock, W., and S. Zoneraich. A diastolic murmur arising in a stenosed coronary artery. Am. J. Med. 42:617–619, 1967.
Fearon, W. F., A. J. Gauri, J. Myers, et al. A comparison of treadmill scores to diagnose coronary artery disease. Clin. Cardiol.. 25:117–122, 2002.
Gauthier, D., Y. M. Akay, R.G. Paden, et al. Spectral analysis of heart sounds associated with coronary occlusions. Information Technology Applications in Biomedicine, 2007 ITAB 2007 6th International Special Topic Conference on. 2007. pp. 49–52.
Greulich, S., O. Bruder, M. Parker, et al. Comparison of exercise electrocardiography and stress perfusion CMR for the detection of coronary artery disease in women. J. Cardiovasc. Magn. Reson. 14:36, 2012.
Hansen, J., N. H. Zimmermann, S. Schmidt, et al. System for acquisition of weak murmurs related to coronary artery diseases. Comput. Cardiol. 38:213–216, 2011.
Jin-Zhao, W., T. Bing, W. Welkowitz, et al. Modeling sound generation in stenosed coronary arteries. IEEE Trans. Biomed. Eng.. 37:1087–1094, 1990.
Knuuti, J., F. Bengel, J. J. Bax, et al. Risks and benefits of cardiac imaging: an analysis of risks related to imaging for coronary artery disease. Eur. Heart J. 35:633–638, 2014.
Knuuti, J., W. Wijns, S. Achenbach, et al. ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J., 2019. https://doi.org/10.1093/eurheartj/ehz425.
Lai, S., A. Kaykha, T. Yamazaki, et al. Treadmill scores in elderly men. J. Am. Coll. Cardiol. 43:606–615, 2004.
Makaryus, A. N., J. N. Makaryus, A. Figgatt, et al. Utility of an advanced digital electronic stethoscope in the diagnosis of coronary artery disease compared with coronary computed tomographic angiography. Am. J. Cardiol. 111:786–792, 2013.
Marcus, G. M., I. L. Gerber, B. H. McKeown, et al. Association between phonocardiographic third and fourth heart sounds and objective measures of left ventricular function. J. Am. Med. Assoc. [Internet] 293:2238–2244, 2005. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.293.18.2238.
Padmanabhan Semmlow, J. L., and W. V. Welkowitz. Accelerometer type cardiac transducer for detection of low-level heart sounds. IEEE Trans. Bio-med. Eng. 40:21–28, 1993.
Pathak, A., K. Mandana, and G. Saha. Ensembled transfer learning and multiple kernel learning for phonocardiogram based atherosclerotic coronary artery disease detection. IEEE J. Biomed. Health Inf. 2022. https://doi.org/10.1109/JBHI.2022.3140277.
Schmidt, S. E., J. Hansen, H. Zimmermann, et al. Coronary artery disease and low frequency heart sound signatures. Comput. Cardiol. 2011:481–484, 2011.
Schmidt, S. E., C. Holst-Hansen, C. Graff, et al. Segmentation of heart sound recordings by a duration-dependent hidden Markov model. Physiol. Meas. [Internet] 31:513–529, 2010. Available from: http://www.scopus.com/inward/record.url?eid=2-s2.0-77949781513&partnerID=40&md5=09f35a9ab11f14d6b93e879e16a877ae.
Schmidt, S. E., C. Holst-Hansen, C. Graff, et al. Detection of coronary artery disease with an electronic stethoscope. Comput. Cardiol. 2007. https://doi.org/10.1109/CIC.2007.4745596.
Schmidt, S. E., C. Holst-Hansen, J. Hansen, et al. Acoustic features for the identification of coronary artery disease. IEEE Trans. Biomed. Eng. [Internet] 62:2611–2619, 2015. Available from: http://ieeexplore.ieee.org/document/7105874/.
Schmidt, S. E., E. Toft, C. Holst-Hansen, et al. Noise and the detection of coronary artery disease with an electronic stethoscope. 2010 5th Cairo International Biomedical Engineering Conference. Sønderborg, Denmark: IEEE; 2010. pp. 53–56.
Schmidt, S. E., S. Winther, B. S. Larsen, et al. Coronary artery disease risk reclassification by a new acoustic-based score. Int. J. Cardiovasc. Imaging. 35:2019–2028, 2019.
Semmlow, J., and K. Rahalkar. Acoustic detection of coronary artery disease. Annu. Rev. Biomed. Eng. 9:449–469, 2007.
Semmlow, J., W. Welkowitz, J. Kostis, et al. Coronary artery disease–correlates between diastolic auditory characteristics and coronary artery stenoses. IEEE Trans. Bio-med. Eng. 30:136–139, 1983.
Therming, C., S. Galatius, M. Heitmann, et al. Low diagnostic yield of non-invasive testing in patients with suspected coronary artery disease: results from a large unselected hospital-based sample. Eur. Heart J. 4:301–308, 2018.
Winther, S., L. Nissen, S. E. Schmidt, et al. Diagnostic performance of an acoustic-based system for coronary artery disease risk stratification. Heart [Internet] 104:928–935, 2018. Available from: http://heart.bmj.com/lookup/doi/10.1136/heartjnl-2017-311944.
Winther, S., S. E. Schmidt, N. R. Holm, et al. Diagnosing coronary artery disease by sound analysis from coronary stenosis induced turbulent blood flow: diagnostic performance in patients with stable angina pectoris. Int. J. Cardiovasc. Imaging. 32:235–245, 2016.
Wu, E. B., F. Hodson, and J. B. Chambers. A simple score for predicting coronary artery disease in patients with chest pain. QJM. 98:803–811, 2005.
Zimmermann, N. H., S. Schmidt, J. Hansen, et al. Acoustic coupler for acquisition of coronary artery murmurs. Comput. Cardiol. 3:209–212, 2011.
Author Contributions
SES developed the algorithm, drafted the manuscripts. LHM did the data collection and reviewed the manuscript, JH, HZ and DH developed the data acquisition system and reviewed the manuscript. KH did the analyse of the QCA analyse. ET and JJS reviewed the protocol and manuscript. PC was the principal investigator, drafted the study protocol and reviewed the manuscript.
Funding
The current study was sponsored by the Danish high technology foundation and Coloplast A/S.
Conflict of interest
SES holds shares in Acarix, works significantly as Expert Witness and consultant for Acarix and received institutional research grants from Acarix.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Scott C Corbett oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schmidt, S.E., Madsen, L.H., Hansen, J. et al. Coronary Artery Disease Detected by Low Frequency Heart Sounds. Cardiovasc Eng Tech 13, 864–871 (2022). https://doi.org/10.1007/s13239-022-00622-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-022-00622-6