Abstract
Background
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorder having most impact on women of reproductive age group, affecting their quality of life (HRQOL) and psychological well-being.
Objective
This paper aims to determine QOL among women affected with PCOS attending a multidisciplinary clinic using PCOSQ tool and its association with socio-economic status, phenotypes, anxiety, depression and metabolic comorbidities and evaluate the coping strategies adapted by these women.
Design
Retrospective study.
Setting
Integrated multidisciplinary PCOS clinic.
Patient(s)
Two hundred and nine women diagnosed with PCOS as per Rotterdam criteria.
Results
Infertility was an important condition for reduced HRQOL and psychological morbidity across all socio-economic status and phenotypes. The poor psychological status and obesity were identified as determinants of HRQOL among women affected with PCOS. Those who suffered from anxiety, depression and showed lower HRQOL used emotional maladaptive coping strategies.
Conclusion
Results reveal that HRQOL of PCOS women is worsened in the presence of comorbidities. Maladaptive and disengagement coping strategies used by women may worsen their psychological status. Holistic assessment of comorbidities and its management can help improve HROL of affected women. Personalised counselling based on the assessment of coping strategies used by women could empower women to cope better with PCOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorder affecting women from adolescence to menopause impacting reproductive health and general well-being [1]. Studies on PCOS in India report varied prevalence ranging from 3.7 to 22.5% [2]. Most common symptoms of PCOS are menstrual irregularities, infertility, hirsutism, acne vulgaris, acanthosis nigricans and androgenetic alopecia [1]. Many women diagnosed with PCOS also present with features of metabolic syndrome (MS) [3].
There are various reports linking specific features of PCOS with decreased psychological well-being. This is often due to negative body image not conforming to the societal norms of physical and cosmetic appearance and hence lowering the self-esteem of these women [4]. Irrespective of severity of symptoms, studies have shown that this may result in anxiety and depression and have a negative impact on health-related quality of life (HRQOL) in women with PCOS including adolescents [5,6,7,8,9,10,11,12]. Hence, guidelines [13, 14] recommend screening for psychological well-being in all women with PCOS.
Not much is known about how women in India cope with PCOS and how it affects their psychological well-being and HRQOL. Studies on HRQOL and PCOS have used generalised tools such as SF 36 [5, 6, 9] and WHOQOL BREF [10, 12]. However, Polycystic Ovarian Syndrome Questionnaire (PCOSQ) is a very specific tool [15] that has been developed based on signs and symptoms affecting women with PCOS. Very few studies in Indian context have used PCOSQ [16, 17] and studied their association with phenotypes and associated morbidities.
Coping strategies (CS) form an important link between a stressful situation and the resulting psychological response of the person towards it [18]. An illness and its subsequent sequelae can bring about stressful reactions in people [19]. The process of successful or unsuccessful coping can affect their health behaviour, choices and outcomes including psychological well-being and HRQOL. [19, 20]. Successful use of adaptive CS helps in reducing psychological problems in women with PCOS [18, 21].
This paper aims to determine HRQOL among women affected with PCOS attending a multidisciplinary clinic using PCOSQ tool and its association with socio-economic status (SES), phenotypes, anxiety, depression and MS and evaluate the CS adapted by these women.
Methods
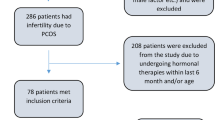
This is a retrospective analysis of case record forms, of 209 women between 15 and 40 years of age, who presented to an integrated multidisciplinary PCOS clinic at Indian Council of Medical Research—National Institute for Research in Reproductive and Child Health (ICMR-NIRRCH) Mumbai, India, from May 2016 to February 2020. They were diagnosed with PCOS as per Rotterdam Criteria [14] and after ruling out other differential diagnosis conditions [22]. PCOSQ, DSM-5 [23] and the Coping Strategy Inventory (CSI) [24] are used routinely at the clinic to offer holistic management for PCOS and are administered by the counsellors at the clinic. Permission for publication of the retrospective data was obtained from the institute’s ethics committee, and all data were anonymized for analysis.
BG Prasad 2019 classification [25] was used to determine the SES of the participants. Diagnosis of MS was done according to the NCEP ATP III definition [26].
PCOSQ was used to measure HRQOL which is a 26-item Questionnaire subdivided into five domains, namely emotional, body hair, weight, infertility and menstruation answered on a 7-point Likert scale,. The mean scores for each domain reflect the respondent’s feelings in the preceding 2 weeks with higher values indicating better HRQOL. PCOSQ scoring provides separate domain scores for each of the five domains, as the numeric mean as well as a global score, as the mean of the five domain scores. Copyright permission to use the PCOSQ was obtained. (Order No.501312418). Total HRQOL Scores above Mean + SD were considered as better QOL.
The DSM-5 self-rated level 1 cross-cutting symptom measure-Adult was used to assess the psychological status of women with PCOS. It has 23 questions assessing participant’s feelings about certain situation across 13 psychiatric domains, measured on a 5-point Likert scale with mean score ranging from 0 to 4. The presence of anxiety and depression was considered if the mean score was 2 and above in the respective domains.
The CSI was used to assess the CS used by women with PCOS. It is a 72-item questionnaire assessing eight primary CS and further broadly assessed as adaptive/ engagement CS and maladaptive/ disengagement CS, mentioned in detail in Table 3. Mean score is calculated for each subscale and ranges from 1 to 5, where higher mean value indicates better response in the particular CS.
Scoring and analysis of each questionnaire was done as per their respective manuals. SPSS for Windows, Version 23, Chicago, SPSS Inc., was used to analyse the data. Descriptive statistics was used for all categorical data. Comparing PCOSQ and CSI scores between different groups was done using the independent t tests.
The magnitude of the association between HRQOL and selected independent variables was measured by odds ratio (OR) and their 95% confidence intervals (CI) obtained with simple logistic regression (LR) models. All variables that were significant at a P value of < 0.05 were entered in univariate analysis. The step-up model was used for multivariate analysis.
Results
Socio-demographic Profile and Clinical Profile
The mean age of the participants was 26.27 ± 4.9 years. Socio-demographic and clinical characteristics of the women with PCOS are given in Table 1. Majority were married, housewives belonging to higher or middle socio-economic strata.
Nearly half (48.8%) presented with oligo menorrhoea as chief complaint, and a third of women (31.1%) presented with amenorrhoea. A large majority (88.53%) from the 157 married females presented with infertility. More than half (62.2%) had hirsutism score more than 8 and BMI above 25 (58.9%). Hormonal analysis revealed that 69.4% women had hyperandrogenism and 10.52% had hyperinsulinemia. Polycystic ovarian morphology on ultrasound was observed among almost all women (96.7%). When categorised into different phenotypes as per the International Evidence-based guidelines for the assessment and management of PCOS, 2018 [14], 68.89% were Phenotype A, 71.77% were Phenotype B, 81.33% presented as Phenotype C and 85.64% were Phenotype D. About a third of women with PCOS (36.84%) were diagnosed with MS.
PCOSQ revealed that maximum score was present in the hair domain (5.70 ± 1.79) followed by weight (4.76 ± 2.01), menstrual (4.53 ± 1.38) and emotional (4.44 ± 1.42) domains. The least score was obtained in the infertility (3.85 ± 1.86) domain indicating that it affected HRQOL the most.
Symptoms of anxiety and/or depression were present in 68.9% of the respondents, out of which 61.7% had anxiety, 39.2% had depression, while 32.05% had both. No significant difference was noted in the prevalence of anxiety and depression based on the different phenotypes.
Association of HRQOL scores with Socio-economic profile, PCOS Phenotypes, Comorbidities and Anxiety, Depression
Mean values of PCOSQ scores were found to be higher in Class 3 and 4 of socio-economic classes, across all domains. Infertility scores were the lowest in all the socio-economic groups (Table 2). No significant difference was observed in the mean scores of PCOSQ across the different phenotypes.
The mean scores of the group with anxiety and depression symptoms in all the domains and the total HRQOL was found to be low and statistically significant compared to the group without anxiety and depression symptoms, indicating a lower HRQOL in the group with anxiety and depression symptoms. (Table 2).
The mean scores of the group with MS in all domains (except Hair) and the total HRQOL was found to be low compared to the group without MS. This difference was found to be statistically significant across the emotional and weight domains and the total HRQOL (Table 2).
Coping Strategies and its Association with Anxiety, Depression and HRQOL
Mean score 3 and above was observed in 28.7% women for engagement CS alone and in 7.2% women for disengagement CS. However, majority (63.6%) of them scored above mean in both engagement and disengagement CS (Table 3).
Comparison of mean scores of different CS was done between groups with and without anxiety and depression symptoms. The mean scores of the group with anxiety and depression was higher and statistically significant across all domains of maladaptive CS indicating that it was most used by those with psychological morbidity (Table 3).
The total HRQOL score was divided into two groups considering the mean + SD score of 5.87. Those who scored above this value were presumed to have a better HRQOL than those who scored below. Comparison of mean scores of CS was done between the two groups. The mean scores across disengagement or maladaptive CS were higher and statistically significant among the lower HRQOL score group (Table 4).
Determinants of HRQOL
LR was performed to ascertain the effects of several independent variables such as marital status, infertility, obesity, MS, psychological morbidity, SES and CS on better HRQOL. Table 5 shows that non-obese PCOS women have better HRQOL (U.O.R = 7.25, AOR = 8.02) compared to obese women. Similarly, those without psychological morbidity have three times better HRQOL. PCOS women without MS were found to have better HRQOL (U.O.R = 2.53) as compared to those who had; however, the adjusted odds were not significant. Post hoc assessment of model fit (Hosmer and Lemeshow test, P = 0.48) showed good fit of the mathematical model.
Discussion
Clinicians often are more objective in treating PCOS such that they focus on clinical and laboratory parameters to treat physical health parameters. This paper aims to highlight the importance of addressing HRQOL and CS that are less addressed in clinical practice.
HRQOL is a very subjective concept and is determined by a number of measurable and non-measurable aspects of how a woman, her family and society perceives the symptoms and associated comorbidities. Many tools have been used to measure HRQOL. Qualitative interviews with women with PCOS have demonstrated that generic questionnaires can underestimate the full impact of PCOS on their HRQOL, as they do not explore issues specific to PCOS. [27] However, PCOSQ is specifically developed tool to assess HRQOL in PCOS women.
Indian studies using SF 36 and WHO BRIEF [12, 28] to evaluate HRQOL in women with PCOS have also reported lower HRQOL scores across different domains like social and interpersonal relationships, physical, environmental, financial, psychological, etc., as compared to healthy controls. Having used PCOSQ, we have reported reduced HRQOL in women with PCOS in domains like emotion, hair, menstruation, weight and infertility which are more specific to PCOS. Our findings reveal infertility affected HRQOL the most. A strong association is reported between infertility and emotional well-being of women with PCOS in another study done in North India [17] using PCOSQ. It is obvious as infertility is a socially stigmatising problem less addressed through the public health system in India. This finding is also supported by other studies using SF 36 and WHO BRIEF [10, 12, 28]. The WHO BRIEF study also found that patients with hirsutism had lower HRQOL scores [10]. Study done in Hyderabad [16] using PCOSQ reported menstruation affected HRQOL the most, different from our finding, probably due to majority of the study population being unmarried girls, and pregnancy not being a priority. This reveals that health priorities differ in different age groups and affect different dimensions or domains of HRQOL.
Our finding, that higher the SES, better the HRQOL, resonates with the findings published from Poland [29]. This is one very strong pointer of how PCOS is a social and economic issue irrespective of the phenotypes women present with as also seen in a study from Iran [30].
Poor HRQOL, psychological status such as anxiety, depression, and use of improper CS are interdependent factors that need a holistic assessment and care using a multidisciplinary approach. The meta-analysis [4] published in 2012 on prevalence of anxiety in PCOS women suggested that hirsutism, obesity and infertility are triggers for psychological distress, unfortunately it did not include any studies from India that have also reported prevalence of psychological disorders [12, 27, 31] among women with PCOS much higher as compared to controls [12, 27, 32]. Our analysis reported that about two-third (68.9%) women had anxiety and depression, which are the most commonly reported psychological disorders associated with PCOS [8]. However, the prevalence was higher than that reported in another study from Mumbai, India, that used HADS tool and reported 38.6% prevalence for anxiety disorders and 25.7% for depressive disorders [12]. The prevalence of anxiety and depression in our subjects may be higher as a large proportion (88%) of our participants were suffering from infertility unlike the study in Mumbai, where infertility was reported by less than a quarter of total sample. Another Indian study from Kashmir [32] reported prevalence of generalised anxiety disorder to be 15.5% and 23% had depression on using a DSM-IV tool.
The presence of anxiety and depression was correlated with specific PCOSQ domains which has not been reported earlier, to our knowledge. Results revealed that women with anxiety and depression scored significantly poor on all the PCOSQ domains and total HRQOL score, as compared to those who did not. Further analysis revealed that among all independent variables, obesity and psychological status affected HRQOL significantly. As expected, infertility greatly affected psychological status. Thus, addressing infertility is an important strategy to facilitate PCOS women improve their HRQOL.
Research studies have found individuals using problem-oriented CS are better suited to handle stressful situations and that has positive effect on the HRQOL [33]. Negative impact of stress can reduce individual’s resilience, and leave long-term adverse health impacts, thus emphasising that CS adopted by individuals is critical [34, 35].
Our findings suggest that mostly a combination of both engagement and disengagement CS was used. However, those who had lower HRQOL and anxiety and depression used disengagement CS, which was statistically significant similar to a study done in Turkey [36]. Some of the earlier studies report disengagement CS to be positively correlated with psychological morbidity [21, 37] and inversely correlated with the HRQOL [21, 38].
Women generally tend to use emotion focused CS [34, 39]. Improper CS severely affects the HRQOL of women affected with PCOS [37]. High level of stress and a feeling that the situation is not under their control makes it difficult to use problem focused CS [40]. Given that our study population constituted of a large number of women with infertility, which is a very stressful condition, emotion focused disengagement CS approach was seen extensively used in our study.
This study has the limitation due to the absence of a control group. Intervention studies using multidisciplinary approach are needed to assess impact of various therapeutic drugs, biofeedback strategies, cognitive therapies and involvement of marital partners, families and social support groups to provide an enabling environment that could help avert these morbidities among women affected with PCOS.
Conclusion
Data reveal that HRQOL of PCOS women is worsened in the presence of comorbidities. Maladaptive and disengagement coping strategies used by women may worsen their psychological status. Holistic assessment of comorbidities and its management can help improve HROL of affected women. Personalised counselling based on the assessment of coping strategies used by women could empower women to cope better with PCOS.
References
Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO. The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab. 2004;89(6):2745–9.
Ganie MA, Vasudevan V, Wani IA, Baba MS, Arif T, Rashid A. Epidemiology, pathogenesis, genetics and management of polycystic ovary syndrome in India. Indian J Med Res. 2019;150(4):333–44. https://doi.org/10.4103/ijmr.IJMR_1937_17.
Wild RA, Carmina E, Diamanti-Kandarakis E, Dokras A, Escobar-Morreale HF, Futterweit W, Lobo R, Norman RJ, Talbott E, Dumesic DA. Assessment of cardiovascular risk and prevention of cardiovascular disease in women with the polycystic ovary syndrome: a consensus statement by the Androgen Excess and Polycystic Ovary Syndrome (AE-PCOS) Society. J Clin Endocrinol Metab. 2010;95(5):2038–49.
Dokras A, Clifton S, Futterweit W, Wild R. Increased risk for abnormal anxiety scores in women with polycystic ovary syndrome: a systematic review and meta-analysis. Fert Steril. 2012;97(1):225–30.
Coffey S, Bano G, Mason HD. Health-related quality of life in women with polycystic ovary syndrome: a comparison with the general population using the Polycystic Ovary Syndrome Questionnaire (PCOSQ) and the Short Form-36 (SF-36). Gynecol Endocrinol. 2006;22:80–6.
Khomami MB, Tehrani FR, Hashemi S, Farahmand M, Azizi F. Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Ira- nian women. PLoS ONE. 2015;10:e0123608.
Schmid J, Kirchengast S, Vytiska-Binstorfer E, Huber J. Infertility caused by PCOS—health-related quality of life among Austrian and Moslem immi- grant women in Austria. Hum Reprod. 2004;19:2251–7.
Trent ME, Rich M, Austin SB, Gordon CM. Quality of life in adolescent girls with polycystic ovary syndrome. Arch Pediatr Adolesc Med. 2002;156(6):556–60.
Elsenbruch S, Hahn S, Kowalsky D, Öffner AH, Schedlowski M, Mann K, Janssen OE. Quality of life, psychosocial well-being, and sexual satisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2003;88(12):5801–7.
Prathap A, Subhalakshmi TP, Varghese PJ. A cross-sectional study on the proportion of anxiety and depression and determinants of quality of life in polycystic ovarian disease. Indian J Psychol Med. 2018;40(3):257.
Greenwood EA, Pasch LA, Cedars MI, Legro RS, Huddleston HG, Network HD, Eunice Kennedy Shriver National Institute of Child Health. Association among depression, symptom experience, and quality of life in polycystic ovary syndrome. Am J Obstet Gynecol. 2018;219(3):2791.
Chaudhari AP, Mazumdar K, Mehta PD. Anxiety, depression, and quality of life in women with polycystic ovarian syndrome. Indian J Psychol Med. 2018;40(3):239.
Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Hassan Murad M, Pasquali R, Welt CK. Diagnosis and treatment of polycystic ovary syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4565–92. https://doi.org/10.1210/jc.2013-2350.
International evidence-based guideline for the assessment and management of polycystic ovary syndrome 2018. https://www.monash.edu/__data/assets/pdf_file/0004/1412644/PCOS_Evidence-Based-Guidelines_20181009.pdf
Cronin L, Guyatt G, Grifrth L, Wong E, Azziz R, Futterweit W, Cook D, Dunaif A. Development of a health-related quality-of-life questionnaire (PCOSQ) for women with polycystic ovary syndrome (PCOS). J Clin Endocrinol Metab. 1998;83:1976–87.
Gollapudi R, Lanke VM, Namilakonda M. Prevalence of depression and quality of life in polycystic ovary syndrome patients at a tertiary care hospital: a cross-sectional study. Int J Reprod Contracept Obstet Gynecol. 2019;8(6):2251–5. https://doi.org/10.18203/2320-1770.ijrcog20192412.
Tabassum F, Sinha HH, Dhar K, Jyoti C, Akhtar MS, Chopra VS. Assessment of psycho-emotional distress due to age, body mass index, and marital status in polycystic ovary syndrome in North Indian population. Int J Women’s Health Reprod Sci. 2020;8(4):368–75. https://doi.org/10.15296/ijwhr.2020.59.
Folkman S. Stress: appraisal and coping. In: Gellman MD, Turner JR, editors. Encyclopedia of behavioral medicine. New York: Springer; 2013. p. 1913–5. https://doi.org/10.1007/978-1-4419-1005-9_215.
Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. San Francisco, CA: Jossey-Bass; 2008. p. 211–36.
Lechner L, Bolman C, van Dalen A. Definite involuntary childlessness: associations between coping, social support and psychological distress. Hum Reprod. 2007;22:288–94.
Benson S, Hahn S, Tan S, Janssen OE, Schedlowski M, Elsenbruch S. Maladaptive coping with illness in women with polycystic ovary syndrome. JOGNN. 2010;39:37–45.
Sheehan MT. Polycystic ovarian syndrome: diagnosis and management. Clin Med Res. 2004;2(1):13–27. https://doi.org/10.3121/cmr.2.1.13.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Tobin, D.L, (2001). User Manual for the Coping Strategies Inventory. https://www.academia.edu/30133319/User_Manual_for_the_COPING_STRATEGIES_INVENTORY
Pandey VK, Aggarwal P, Kakkar R. Modified BG Prasad socio-economic classification, update - 2019. Indian J Commun Health. 2019;31:123–5. https://doi.org/10.47203/IJCH.2019.v31i01.025.
National Cholesterol Education Program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). Circulation. 2002;106(25):3143–421.
Bhattacharya SM, Jha A. Prevalence and risk of depressive disorders in women with polycystic ovary syndrome (PCOS). Fertil Steril. 2010;94(1):357–9.
Tabassum F, Jyoti C, Sinha HH, Dhar K, Akhtar MS. Impact of polycystic ovary syndrome on quality of life of women in correlation to age, basal metabolic index, education and marriage. PLoS ONE. 2021;16(3):e0247486. https://doi.org/10.1371/journal.pone.0247486.
Rzońca E, Bień A, Wdowiak A, Szymański R, Iwanowicz-Palus G. Determinants of quality of life and satisfaction with life in women with polycystic ovary syndrome. Int J Environ Res Public Health. 2018;15(2):376. https://doi.org/10.3390/ijerph15020376.
Fatemeh B, Shahideh JS, Negin M. Health related quality of life and psychological parameters in different polycystic ovary syndrome phenotypes: a comparative cross-sectional study. J Ovarian Res. 2021;14:57. https://doi.org/10.1186/s13048-021-00811-2.
Sundararaman PG, Sridhar GR. Psychosocial aspects of women with polycystic ovary syndrome from south India. J Assoc Phys India. 2008;56:945–8.
Hussain A, Chandel RK, Ganie MA, Dar MA, Rather YH, Wani ZA, Shiekh JA, Shah MS. Prevalence of psychiatric disorders in patients with a diagnosis of polycystic ovary syndrome in kashmir. Indian J Psychol Med. 2015;7(1):66–70. https://doi.org/10.4103/0253-7176.150822.
Graven LJ, Grant JS. Coping and health-related quality of life in individuals with heart failure: an integrative review. Heart Lung. 2013;42(3):183–94. https://doi.org/10.1016/j.hrtlng.2012.12.002.
Morshedi T, Salehi M, Farzad V, Hassani F, Shakibazadeh E. The status of relationship between coping strategies and quality of life in women with polycystic ovary syndrome. J Educ Health Promot. 2021;10(1):185. https://doi.org/10.4103/jehp.jehp_1008_20.
Nedaei A, Paghoosh A, Sadeghi-Hosnijeh A. Relationship between coping strategies and quality of life: mediating role of cognitive emotion regulation skills. J Clin Psychol. 2016;8(4):35–48. https://doi.org/10.22075/jcp.2017.2252.
Özenli Y, Haydardedeoğlu B, Micozkadıoğlu İ, Şimşek E, BulganKılıçdağ E, Bağış T. Anxiety, depression and ways of coping skills in women with polycystic ovary syndrome: a controlled study. J Turk Ger Gynecol Assoc. 2008;9:190–3.
Carron R, Kooienga S, Boyle DK, Alvero R. Coping in women with polycystic ovary syndrome: implications for practitioners. J Nurs Pract. 2017;13(10):700–7.
Kolahi L, Asemi N, Mirzaei M, Adibi N, Beiraghdar M, Mehr AM. The relationship between quality of life and coping strategies in polycystic ovary syndrome patients. Adv Biomed Res. 2015;4:168.
Kelly MM, Tyrka AR, Price LH, Carpenter LL. Sex Differences in the use of coping strategies: predictors of anxiety and depressive symptoms. Depress Anxiety. 2008;25(10):839–46.
Stephenson E, King DB, DeLongis A. Chapter 44: coping process. Stress: concepts, cognition, emotion, and behavior. Amsterdam: Elsevier Inc; 2016.
Acknowledgements
We acknowledge the encouragement and support provided by Dr. Smita Mahale, Director, Indian Council of Medical Research—National Institute for Research in Reproductive and Child Health (ICMR-NIRRCH). We acknowledge and thank all participants of the survey without whom this was an impossible task.
Funding
This study was conducted as an Intramural project of ICMR-NIRRH, and hence there was no sourced funding agency and no financial conflicts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All necessary ethical approvals were obtained from NIRRCH Ethical Committee for Clinical Studies and use of retrospective data. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this manuscript.
Consent to Participate
Informed written consent for participation in study was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joshi, B., Patil, A., Kokate, P.P. et al. Assessment of Health-Related Quality of Life Using PCOSQ Tool, Its Determinants and Coping Mechanisms Used by Women with Polycystic Ovarian Syndrome Attending Multidisciplinary Clinic in Mumbai, India. J Obstet Gynecol India 73, 172–179 (2023). https://doi.org/10.1007/s13224-022-01723-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-022-01723-x