Abstract
Background
Genital tuberculosis is one of the leading causes of female infertility. Paucibacillary nature of the disease in the female genital system often makes its diagnosis difficult. No single test has been able to accurately diagnose genital tuberculosis. In this study we aim to compare conventional diagnostic tests for tuberculosis like Acid Fast Bacilli (AFB) Staining, Lowenstein Jensen (LJ) Culture and Histopathology with newer tests like PCR, MGIT 960, GeneXpert.
Methods
This study included 67 infertile women from Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi. They were subjected to detailed history and routine investigations, namely Haemogram, ESR, Mantoux test, Chest X-ray and pelvic ultrasound to look for the findings of tuberculosis. A premenstrual endometrial aspirate was taken and was subjected to the AFB Staining, LJ Culture, Histopathology, PCR, MGIT 960, Gene Xpert, and the test results were compared.
Result and Conclusion
35.8% (24/67) of women were diagnosed with genital tuberculosis using the diagnostic criteria. With culture as the gold standard, the positivity of genital TB was 19.4% (13/67). Majority of infertile patients with low index of suspicion clinically were positive for genital tuberculosis. Therefore, all the patients of infertility should be routinely evaluated for genital tuberculosis. PCR and MGIT 960 have shown promising results in the newer methods. LJ culture and histopathology are still the most reliable and available diagnostic methods. The usefulness of AFB Staining and GeneXpert remains questionable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infertility is defined as inability of a couple to conceive even after 1 year of unprotected intercourse. In women who are more than or equal to 35 years, this time is further reduced to 6 months.
Female genital tuberculosis (FGTB), primarily an asymptomatic disease, is one of the most important causes of female infertility in developing countries [1]. Genitourinary tuberculosis is the most common form of extra-pulmonary tuberculosis [2]. In developing countries, its prevalence is approximately 28%, while it is only < 1% in developed countries [1]. In India it is reported to be 18–19% among infertile women [3]. The organs most commonly affected are fallopian tubes (92–100%), followed by the endometrium (50%), ovaries (10–30%), cervix (5%), and rarely vagina/ vulva (< 1%). Presenting symptoms are generally varied with infertility being the most common presentation. Other clinical symptoms include pelvic pain, menstrual irregularities, dyspareunia, dysmenorrhea [1].
The early diagnosis of FGTB is critical to prevent its sequelae. Due to paucibacillary nature of the disease, there has been no satisfactory diagnostic modality. Lack of an accurate diagnostic test has led to either underdiagnosis or an indiscriminate use of antitubercular treatment in infertile women along with the risk of developing resistance to ATT (anti-tubercular treatment).
Conventional methods for detection of genital tuberculosis are Acid Fast Bacilli(AFB) Staining, AFB Culture by Lowenstein Jensen(LJ) method and Histopathology.
Newer diagnostic modalities are Real-Time Polymerase Chain Reaction (PCR), GeneXpert, Automated TB Culture.
Real-Time PCR is a Nucleic Acid Amplification Test which is used to amplify DNA segments with a high specificity to rapidly identify microorganisms in a specimen. False positives may occur due to contamination of specimens with Mycobacterium tuberculosis (MTB) DNA product from the PCR laboratory. The inability to differentiate between viable and nonviable organisms is one of the major disadvantages. Therefore, the test can remain positive for longer periods in patients who are on ATT or who have completed TB treatment. False-negative results may occur because of the inefficient extraction of the DNA due to low mycobacterial numbers or the presence of PCR inhibitors.
GeneXpert is a cartridge-based, semi-automated, rapid molecular assay, which allows rapid TB diagnosis through the detection of the mycobacterial DNA and simultaneous identification of rifampicin resistance (Multi Drug Resistant TB). However, its use in extrapulmonary TB (other than lymph node aspirate, CSF) is still not fully established [3].
Automated TB culture (e.g. Mycobacterium Growth Indicator Tube (MGIT) 960) is a rapid liquid culture method which senses carbon dioxide production or oxygen reduction in the culture media, a portion of which is then centrifuged and stained with ZN stain to identify MTB. Positive cultures are reported usually within 10–12 days [3].
Materials and Methods
This study was conducted in the Department of Obstetrics and Gynaecology in conjunction with Department of Microbiology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi and included 67 infertile women who were enrolled over a period of 18 months.
Type of study: Cross-sectional study.
Inclusion criteria: All women, less than 38 years of age, attending infertility OPD at Safdarjung Hospital, New Delhi.
Exclusion criteria:
-
1.
Presence of moderate to severe endometriosis.
-
2.
Presence of documented uterine factor in the form of polyps or fibroids, requiring immediate treatment.
-
3.
History of being treated for tuberculosis.
After obtaining written informed consent from the females, they were subjected to detailed history and clinical examination. Routine investigations were done, namely Haemogram, ESR, Mantoux test, Chest X-ray and pelvic ultrasound to look for the findings of tuberculosis.
ESR of > 20 mm/h was considered raised, and an induration of > 20 mm was considered as positive Mantoux test for tuberculosis.
In the pelvic ultrasound findings such as endometrial or sub-endometrial calcification, bands, inhomogeneity, thin endometrium or diffuse variable thickening, cornual obliteration, tubal fluid, free/loculated peritoneal fluid, adenexal fixity, follicles with echogenic rims were considered suggestive of genital tuberculosis.
Socioeconomic status of the study subjects was assessed by Modified Kuppuswami Scale 2019 [4].
Endometrial aspirate: A premenstrual endometrial aspirate was taken and was subjected to the following tests after processing. Sample was emulsified in sterile saline and processed by vortexing for further use. For culture, sample was centrifuged and further processed by Modified Petroff”s method.
Conventional tests
AFB Staining: Smears were prepared stained using Ziehl–Neelsen(ZN) staining method and examined using light microscope under oil field immersion (100X) lens for presence of pink-bright red curved, beaded rods arranged singly or in clumps. Presence of even single bacteria was reported as positive for extrapulmonary TB.
AFB Culture by Lowenstein Jensen (LJ) method: The processed sample was inoculated into the Lowenstein Jensen medium and was then incubated at 370 C. The media were reexamined within 5–7 days and weekly thereafter for 8 weeks and any growth noted. The growth such obtained was confirmed for AFB by microscopic examination.
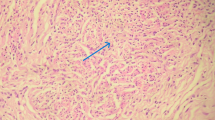
Histopathological examination: A part of endometrial aspirate was also sent for histopathological examination and findings noted. The presence of caeseating granulomas surrounded by epitheloid cells, giant cells, lymphocytes, plasma cells was considered positive for genital tuberculosis.
Newer tests
GeneXpert
1 µl of decontaminated sample was diluted in 2 µl of sample buffer given with the assay kit. Solution was vortexed for 15 s and left undisturbed for 15 min. It was vortexed for 15 s halfway through. Using a calibrated pipette, a specific volume was collected and transferred to the cartridge and the cartridge inserted into the GeneXpert instruments.
Automated TB culture
The culture method used was MGIT 960.The MGIT 960 culture tubes contain 7 ml of Middlebrook 7H9 broth base. After inoculation of each tube with 0.5 ml of the processed specimen, they were entered into the MGIT 960 instrument. The vials were incubated at room temperature and monitored automatically every 60 min for increase in fluorescence for a maximum of 6 weeks. Any sample, which was identified as positive, was removed from the instrument and prepared for examination of AFB.
Real-time TB-PCR
DNA extraction method (QIAamp DNA minikit)
DNA was extracted prior to performing PCR.
Real-time PCR (Qiagen Rotor gene 6000)
PCR result interpretation:
-
Signal in flourescence channel Cycling A.FAM - MTb Complex DNA positive.
-
Signal in flourescence channel Cycling A.Green- MTb Complex DNA positive.
On the basis of results of ESR, Mantoux, Chest X-ray and ultrasonography, women were divided into high index and low index of suspicion of female genital tuberculosis clinically. High index of suspicion was those with all 3 having positive findings suggestive of GTB i.e. on ultrasound or Chest X-ray, raised ESR and positive Mantoux.
Diagnosis of female GTB was based on one of the followings [5, 6]:
-
1.
Positive on histopathological examination.
-
2.
Positive on culture (LJ and/or MGIT 960).
Comparison of all the conventional and newer tests was done with the above diagnostic criteria.
Statistical analysis
Analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Observations and results
Out of the total 67 patients, 50 (74.6%) belonged to 21–30 years of age group and 17 (25.4%) to 31–40 years. In this study, 47 (70.15%) patients were having primary infertility and 20 (29.85%) were having secondary infertility. The mean duration of infertility was 5.31 ± 2.52 years.
The socioeconomic status of the participants was assessed according to Modified Kuppuswamy Scale 2019. Majority (58.21%) of study participants belonged to upper lower socioeconomic class.
Apart from infertility, 19 (28.36%) patients presented with menstrual disturbances and 7 (10.45%) with chronic pelvic pain and backache and majority of them were asymptomatic (62.69%).
On investigations, 26 (38.81%) showed raised ESR and 48 (71.64%) had positive Mantoux test. Fourteen (20.90%) depicted findings suggestive of genital tuberculosis in pelvic ultrasonography and only 2 (2.99%) showed findings suggestive of tuberculosis on chest X-ray. However, only nine (13.44%) patients had all the three findings: raised ESR, positive Mantoux and ultrasound/X ray findings. These nine patients therefore had high index of suspicion clinically and rest 58 (86.56%) had low index of suspicion for genital tuberculosis.
Out of the 67 patients, 24 (35%) were found to be having genital tuberculosis i.e. positive on any culture or histopathology. 8 (11.94%) showed positivity on conventional LJ culture method, whereas only 5 (7.46%) were positive on newer MGIT 960 culture method. A total of 13 patients (19.40%) showed positivity on either LJ or MGIT 960 but none of the LJ culture positive patients showed positivity on MGIT 960 culture and vice versa. Histopathology was positive in 11 (16.42%) patients.
PCR was positive in 15 (22.39%) patients. None of the samples tested positive by AFB-ZN staining and GeneXpert.
Out of the 9 (13.44%) patients having high index of suspicion, 6 (8.96%) were symptomatic and out of 58 (86.56%) patients with low suspicion, majority 39 (58.21%) were asymptomatic.
Out of the 9 (13.44%) patients with clinically high index of suspicion for genital tuberculosis, only one (1.49%) was positive by LJ culture, 2 (2.99%) patients showed positivity by PCR and none of them was positive on MGIT 960 culture. These results were statistically insignificant which means there was no significant difference between high and low suspicion groups. However, 5 (7.46%) patients showed positivity on histopathological examination and this result was statistically significant with p value of 0.001.
Comparison of tests
Out of 15 (22.39%) patients positive for PCR, 8 (11.94%) came out to be positive on LJ/MGIT culture and out of 52 (77.61%) PCR negative patients, 5 (7.46%) came out to be positive on LJ/MGIT culture. There was moderate and significant agreement (kappa = 0.459, p < 0.001) between the tests.
Out of 15 (22.39%) patients positive on PCR, only 2 (2.99%) were positive on histopathology and out of 52 (77.61%) patients negative on PCR, 9 (13.43%) patients showed findings of FGTB on histopathological examination. However, there was poor agreement between the tests (p value = 0.714, kappa = − 0.044). All patients positive on histopathology tested negative by both LJ and MGIT cultures (Table 1).
With culture as the gold standard, the prevalence of genital TB was 19.4% (13/67). PCR had moderate sensitivity and PPV and high specificity and NPV. If we use PCR for diagnosis of genital TB we will miss 38% of the cases and of those who test positive only 47% will have the disease. None of the cases of genital TB was identified by AFB stain, GeneXpert and histopathology (Table 2).
Please check and confirm the inserted citation of Tables 1 and 2 are correct. If not, please suggest an alternative citation. Please note that tables should be cited in sequential order in the text.it is okay
PCR had low sensitivity and PPV and high specificity and NPV. If we use PCR for diagnosis of genital TB we will miss 82% of the cases and of those who test positive only 13% will have the disease.
Discussion
In the present study, 67 infertile females were enrolled. The mean age of the patients was 28.52 years, and mean of duration of infertility was 5.31 years. 70% were having primary infertility and 30% secondary infertility. Majority of my subjects belonged to Upper Lower socioeconomic class. Most of the patients were asymptomatic (62.69%). 35.8% (24/67) of women were diagnosed with genital tuberculosis using the diagnostic criteria. With culture as the gold standard, the positivity of genital TB was 19.4% (13/67).
ZN Staining: AFB ZN staining scored negative in our study. This could be due to direct staining of the specimens as for ZN staining to be positive, it requires 104–106 bacilli per ml and moreover it cannot differentiate mycobacterium tuberculosis pathogen from nontuberculous mycobacteria. So, for a disease like FGTB with a small organism burden, AFB ZN is not an appropriate test.
Goel et al. [7] showed 0.18% positivity on AFB smear and Bhanu et al. [8] showed 1.6% positivity on AFB smear. These results are comparable to the present study.
LJ culture, MGIT 960 and histopathology
There must be 10–100 bacilli/ml of the specimen for LJ culture to be positive.
In the present study, LJ culture, MGIT 960 culture and Histopathology showed 11.94%, 7.46% and 16.42% positivity for GTB, respectively. None of the samples tested positive by all the above three tests. Moreover, LJ conventional method missed out all the 5 cases positive on newer MGIT method and MGIT failed to detect all 8 patients positive on conventional culture.
Seven out of 8 patients positive on LJ and all 5 patients positive on MGIT culture were had low index of suspicion clinically. Therefore, inspite of low/no suspicion clinically both LJ and MGIT culture should be included in the routine battery of investigations for infertility. Six out of 11 patients positive on histopathology had low index of suspicion for genital tuberculosis clinically. This means majority i.e. 18 out of 24 patients diagnosed with genital tuberculosis had low index of suspicion clinically.
None of culture positive patient was positive by histopathology and vice versa. This is possibly due to tuberculosis being a chronic disease, positive histopathology signifies healed or latent lesions or due to the cyclical shedding of the endometrium having granulomas and new ones take time to form.
Goel at al. [7] showed 1.83% positivity on LJ medium. Thangappah et al. [9] showed 5.6% and 6.9% positivity on LJ and Histopathological Examination (HPE), respectively. Kumar et al. [10] showed 4.6% culture positivity and 3.2% HPE positivity. Jindal et al. [11] showed 46.7%, 3.3% and 33.3% positivity on MGIT 960, LJ and HPE, respectively. Smaoui et al. [12] showed 22.4% and 6.1% positivity on MGIT and LJ medium, respectively.
However, in the present study, LJ had a better detection rate than MGIT. This might be due to the fact that our choice of sample was endometrial tissue so a solid culture LJ medium was able to detect more than liquid culture MGIT 960.
Also, histopathology and culture methods supplement each other and should be used in combination. This is due to the fact that culture identifies active disease, whereas histopathology also detects healed and latent lesions.
Polymerase chain reaction
In the present study, PCR was positive in 15 (22.39%) patients which was comparable to study conducted by Thangappah et al. [9] (36.7%), Kumar et al. [10] (38.9%) and Goel et al. [7] (22.22%).
However, Srivastva et al. [13] showed 86% positivity of TB PCR. Bhanu et al. [8] showed positivity of 56% with PCR. These results were not in agreement with the present study.
Among 9 patients with clinically high index of suspicion, only 2 were positive by PCR. Conversely, 13 out of 15 patients positive on PCR had low index of suspicion clinically.
Among the conventional and newer diagnostic methods, PCR had the maximum positivity rate. Eight (11.94%) of the total patients were positive both on PCR and culture (LJ or MGIT). PCR had failed to detect 5 (7.46%) patients which were positive on either of the two cultures. This might be likely due to the presence of PCR inhibitors or blood in the specimen. Also, DNA amplification gets compromised if human: bacterial genome ratio is more than 190:1 which could be possible due to paucibacillary nature of genital TB.
Seven Patients (10.45%) who were positive on PCR were negative on either of the two culture methods. This might be due to the fact that PCR detects even dead bacilli.
Out of 15 positive patients on PCR, only 2 were positive by histopathology. This also means that histopathology missed 13 patients positive on PCR. This might be due to the fact that histopathology just detects the caeseating granulomas which may or may not harbour the TB bacilli and the granulomas might have been shed with the endometrium and new granulomas take weeks to months to form.
Therefore, PCR failed to detect total of 14 out of 24 patients diagnosed with genital TB in the present study.
Using culture as the gold standard, sensitivity, specificity, PPV and NPV of PCR came out to be 61.54%, 87.04%, 53.33% and 90.38%. This result was comparable to Thangappah et al. [9] who showed sensitivity of PCR to be 57.1% and VCC Cheng et al. [14] who showed 72% sensitivity of PCR for extrapulmonary samples.
GeneXpert
In the present study, none tested positive for GeneXpert.
Garg et al. [15] showed 0% positivity of GeneXpert for endometrial samples. Another study showed 1.6% positivity [16]. A meta-analysis conducted by Penz et al. [17] who concluded that GeneXpert has a high specificity but limited sensitivity for detection of extrapulmonary TB. These results were comparable to the present study.
Therefore, GeneXpert has not been much useful for detection of tuberculosis in endometrial samples. This could be due to faulty method of sample processing which was unable to extract bacterial DNA from the endometrial sample.
Kim et al [18] showed sensitivity, specificity, PPV and NPV of GeneXpert to be 67.7%, 98.1%, 60% and 98.6%, respectively, using culture as the gold standard. Similarly, another study showed 100% sensitivity and 20% specificity for acid fast bacilli smear positive extrapulmonary specimen [19]. This was much higher than the present study. On the other hand, the same study showed only 28% sensitivity and 99% specificity for smear negative extrapulmonary specimens [19] similar to the present study.
Conclusion
No single test was appropriate for diagnosing GTB. Hence, clinical evaluation along with conventional and newer methods should be used for evaluating the infertile females. PCR and MGIT 960 have shown promising results in the newer methods. LJ culture and histopathology are still the most reliable and available diagnostic methods.
Majority of infertile patients with low index of suspicion clinically were positive for genital tuberculosis. Therefore, all the patients of infertility should be routinely evaluated for genital tuberculosis by ESR, Mantoux, pelvic ultrasound, LJ along with MGIT culture and histopathology on endometrial tissue.
In this study, conventional methods performed better than newer diagnostic modalities.
Recommendations
-
1.
Apart from endometrial aspirate, menstrual blood, fluid from Pouch of Douglas, multiple intraabdominal biopsies from adhesions should also be sent for evaluation, especially in clinically suspected cases. Hysterolaproscopy and Hystersalpingography findings should also be taken into consideration in diagnosing GTB.
-
2.
Better methods of sample handling, processing and DNA extraction should be evaluated.
-
3.
An appropriate diagnostic test or criteria is to yet to be found which is feasible, affordable, both sensitive and specific and provides early diagnosis.
References
Naredi N, Talwar P, Narayan N, et al. Spontaneous conception following anti-tubercular treatment for sub-fertile women with multiple imaging markers suggesting genital tuberculosis. Fertil Sci Res. 2014;1:44–9.
Das P, Ahuja A, Gupta SD. Incidence, etiopathogenesis and pathological aspects of genitourinary tuberculosis in India: a journey revisited. Indian J Urol. 2008;24:356–61.
Mahajan N, Naidu P, Kaur SD. Insight into the diagnosis and management of subclinical genital tuberculosis in women with infertility. J Human Reprod Sci. 2016;9:135–44.
Saleem SM. Modified Kuppuswamy socioeconomic scale updated for the year 2019. Indian J Forensic Community Med. 2019;6:1–3.
Global tuberculosis report [Internet]. World Health Organization. 2016 [cited 17 September 2017]. http://www.who.int/tb/publications/global_report/en/
Index TB guidelines. Guidelines for extrapulmonary tuberculosis in India. [internet]. 2016 [cited 23 April 2019]. http://www.icmr.nic.in/sites/default/files/guidelines/Index-TB%20Guidelines%20-%20green%20colour%202594164.pdf
Goel G, Khatuja R, Radhakrishnan G, et al. Role of newer methods of diagnosing genital tuberculosis in infertile women. Indian J Pathol Microbiol. 2013;56:155–7.
Bhanu NV, Singh UB, Chakraborty M, et al. Improved diagnostic value of PCR in the diagnosis of female genital tuberculosis leading to infertility. J Med Microbiol. 2005;54:927–31.
Thangappah RBP, Paramasivan CN, Narayanan S. Evaluating PCR, culture & histopathology in the diagnosis of female genital tuberculosis. Indian J Med Res. 2011;134:40–6.
Kumar P, Shah NP, Singhal A, et al. Association of tubercular endometritis with infertility and other gynecological complaints of women in India. J Clin Microbiol. 2008;46:4068–70.
Jindal N, Gainder S, Dhaliwal LK, et al. The role of MGIT 960 culture medium in resolving the diagnostic dilemma for genital tuberculosis patients presenting with infertility. J Obstet Gynaecol India. 2018;68:123–8.
Smaoui S, Kammoun S, Marouane C, et al. Evaluation of the BACTEC MGIT 960 TB with solid media for recovery of mycobacteria from extrapulmonary specimens in South Tunisia. J Med Diagn Meth. 2015;4:171. https://doi.org/10.4172/2168-9784.1000.171.
Shrivastava G, Bajpai T, Bhatambare GS, et al. Genital tuberculosis: Comparative study of the diagnostic modalities. J Hum Reprod Sci. 2014;7:30–3.
Cheng VCC, Yam WC, Hung IFN, et al. Clinical evaluation of the polymerase chain reaction for the rapid diagnosis of tuberculosis. J Clin Pathol. 2004;57:281–5.
Garg R, Agarwal N, Gupta M. Gene Xpert test and endometrial histological findings in infertile women. Int J Reprod Contracept Obstet Gynecol. 2018;7:1480–3.
Saxena R, Shrinet K, Jain M. Comparative study of genital tuberculosis diagnosis in women with infertility. Int J Sci Res. 2017;7:817–9.
Penz E, Boffa J, Roberts DJ, et al. Diagnostic accuracy of the Xpert MTB/RIF assay for extrapulmonary tuberculosis: a meta-analysis. Int J Tuberc Lung Dis. 2015;19:278–84.
Kim YW, Kwak N, Seong MW, et al. Accuracy of the Xpert MTB/RIF assay for the diagnosis of extrapulmonary tuberculosis in South Korea. Int J Tuberc Lung Dis. 2015;19:81–6.
Ozkutuk N, Surucuoglu S. Evaluation of the Xpert MTB/RIF assay for the diagnosis of pulmonary and extrapulmonary tuberculosis in an intermediate prevalence setting. Mikrobiyol Bul. 2014;48:223–32.
Funding
Nil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of V.M.M.C & Safdarjung Hospital, New Delhi (S. No. IEC/VMMC/SJH/Thesis/October/2017–107) and performed in accordance with the principles of the Declaration of Helsinki, 1964 or comparable standards. The research involved human participation and no animal participation.
Consent to participate
Written informed consents were obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Study conducted in: Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
Rights and permissions
About this article
Cite this article
Sethi, A., Bajaj, B., Nair, D. et al. Comparison of Conventional Methods with Newer Diagnostic Modalities to Detect Genital Tuberculosis in Infertile Women. J Obstet Gynecol India 72, 426–432 (2022). https://doi.org/10.1007/s13224-022-01629-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-022-01629-8