Abstract
Introduction and Objective
Fetal choroid plexus cysts (CPC) are often detected on prenatal ultrasounds and pose a need to formulate protocol for management and counseling.
Methodology
A total of 1024 unselected cases between gestational ages 11 and 20 weeks were sonologically screened for CPC in 1-year period. On ultrasound, CPC are seen as sonolucent spaces in the echogenic choroid plexus of lateral ventricles of brain measuring at least 2–3 mm in diameter. Those diagnosed with CPC were subjected to thorough anomaly scan. Prenatal karyotype was offered in cases of associated anomalies.
Results
The incidence of CPC is 1% (10/1024) in this study. Associated anomalies were found in 20% (2/10) of cases, which were offered invasive testing for fetal karyotype. All the cases with isolated CPC had good outcome.
Conclusions
Isolated CPC with low-risk biochemical screening for aneuploidies are now considered normal variants rather than a pathology, need no invasive testing and carry a good prognosis. CPC associated with other anomalies warrant invasive testing and are more likely to be associated with Trisomy 18.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fetal choroid plexus cysts detected during the prenatal ultrasounds incur a need to formulate a protocol on what else to be done, how to counsel the parents and when to offer invasive genetic testing. This study in an Indian scenario aims to answer these questions.
Methods
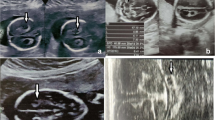
This study is a prospective study including a total of 1024 unselected cases between gestational ages 11 and 20 weeks during 1-year period (April 2016–March 2017). The ultrasound was carried out by FMF, UK (Fetal medicine foundation) certified sonographer on WS80A, Samsung. The criteria for diagnosing choroid plexus cysts (CPC) were 1) sonolucent spaces within the echogenic choroid plexus of lateral ventricles, with well-defined walls 2) measuring at least 2–3 mm in mid trimester 3) usually found at the level of atria, infrequently in the body or anterior part of choroid plexus [1]. Ten cases were reported to have unilateral or bilateral choroid plexus cysts. Out of ten cases of CPC, only one was located in anterior part of choroid plexus. Rest all were located at the level of atria, the usual location.
All the cases wherein CPC were reported were thoroughly scanned for other markers of Trisomy 18 like strawberry head, clenched hands, cardiac abnormalities, talipes, early fetal growth restriction (FGR) and polyhydramnios. The biochemical screening risks (Dual marker or Quadruple marker as per gestation) for aneuploidies were also reviewed in all ten cases. Two cases out of 10 had associated anomalies. One had clenched hands, early FGR and polyhydramnios and Trisomy 18 were suspected in this case, but parents denied any chromosomal analysis and intrauterine fetal death occurred at 28 weeks. Another case had polyhydramnios and single umbilical artery as associated anomalies, and fetal karyotype was normal in this case. The case was followed up routinely until delivery of a female 3.2 kg. The newborn was examined by the neonatologist, and no peculiar features of genetic syndromes were noted by him. Biochemical screening was low risk for aneuploidies in both the cases.
All the patients with isolated CPC were counseled about the excellent prognosis and disappearance of cysts with advancing gestation. All eight isolated cases were followed up at routine growth scans (32 or 36 weeks), and cysts had already disappeared in all of these (Figs. 1, 2).
Results
The median age of the women included was 27.5 years. All women belonged to South Asian ethnicity. None of the cases with CPC had a significant family history of genetic/chromosomal disorders. The incidence of CPC in our study is 1%. The incidence of associated anomalies is 20% in our study. Invasive testing was carried out in one of the two cases with associated anomalies as one couple denied the invasive and carried the pregnancy expectantly. Postnatal examinations of neonates having isolated CPC antenatally were normal which reiterates good prognosis in isolated cases. The association with chromosomal abnormalities could not be confirmed in our study which is a shortcoming.
Discussion
Fetal choroid plexus cysts are most frequently transient and benign findings, and therefore, there is a lack of pathological studies. The ultrasound appearance suggests that a collection of fluid surrounded by choroid plexus tissue [1]. Choroid plexus cysts are identified in approximately 1–2% of fetuses in the second trimester, and they occur equally in male and female fetuses [2]. The real incidence is probably dependent upon the resolution of the ultrasound equipment and the alertness of the operator. The common differential being intraventricular clot, but this is usually less regular than CPC and associated with ventriculomegaly. Another difficulty arises when cyst is located in anterior part of the body or is unusually large. Transvaginal scan when fetus is in cephalic position or a follow-up scan to see the trend and ruling out associated anomalies is helpful. Sometimes there is no well-defined cyst, but the choroid plexus appears heterogenous. This usually will be a benign finding in isolation [1].
Isolated CPC in prenatal period after thorough targeted anomaly scan are considered normal variants and not an abnormality. Ninety percent of CPC usually disappear by third trimester (28 weeks) and rarely persist postnatally. So far, no evidence in the literature suggests proven neurological damage or affected cognitive/motor behavior by CPC per se. A note is made in neurosurgical literature of very large cysts of the choroid plexuses causing intracranial hypertension postnatally, but these represent probably a separate clinical entity [1]. The likelihood of isolated CPC being associated with Trisomy 18 is 7(2.5) and for Trisomy 21 is 1.9 [3, 4]. No invasive genetic testing is needed in these cases after thorough targeted anomaly scan and biochemical screen review. The overall counseling in case of isolated CPC should be of excellent prognosis, and the parents be reassured. No difference in obstetric management is required in these cases. Follow-up ultrasound is not necessary for isolated CPCs [4].
In those with associated anomalies, aneuploidies are likely to be detected in 2.1% cases [1] and are Trisomy 18 in usually all cases [1]. An invasive testing is justified in these cases before offering termination of pregnancy. Noninvasive prenatal test (NIPT) is not the best reliable option for Trisomy 18 detection due to low fetal fraction and lower detection rate [5]. The presence of a choroid plexus cyst does not alter the risk of Trisomy 21, and the finding should not be used to modify a patient’s risk of Trisomy 21(2).
Flowchart of protocol for prenatally diagnosed CPC

Conclusion
CPC detected prenatally warrants thorough search of associated anomalies especially markers of Trisomy 18, in absence of which they are considered as normal variants and hold excellent prognosis. A review of biochemical screening risks is prudent, but low risk does not defer targeted anomaly scan. Invasive genetic testing is justified in presence of associated anomalies only or high risk for Trisomy 21/Trisomy 18 on biochemical screening. NIPT as an alternative to invasive genetic testing in case of associated anomalies is not reliable.
References
Pilu G. Choroid plexus cysts. Vis Encycl Ultrasound Obstet Gynecol. www.visuog.org. August 2013.
Fuchs KM. Isolated fetal choroid plexus cysts. Their implications and outcomes 2013. www.ContemporaryOBGYN.modernmedicine.com.
Goetzinger KR, Stamilio DM, Dicke JM, et al. Evaluating the incidence and likelihood ratios for chromosomal abnormalities in fetuses with common central nervous system malformations. Am J Obstet Gynecol. 2008;199(3):285.e1–6.
Van den Hof MC, Wilson RD, Diagnostic Imaging Committee. Fetal soft markers in obstetric ultrasound. SOGC Clinical Practice Guidelines No. 162, June 2005. J Obstet Gynaecol Can. 2005;27:592–636.
Benn P, Borrell A, Chiu R et al. Position statement from the chromosome abnormality screening, International Society of Prenatal Diagnosis April 8, 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical Statements
The study was approved by the Ethics Committee, Paras Hospitals and written informed consents were taken from the patients included.
Additional information
Dr. Nupur Shah is Consultant Fetal Medicine at Paras Bliss Hospital Fetal Medicine Centre, Panchkula, Haryana (near Chandigarh), India.
Rights and permissions
About this article
Cite this article
Shah, N. Prenatal Diagnosis of Choroid Plexus Cyst: What Next?. J Obstet Gynecol India 68, 366–368 (2018). https://doi.org/10.1007/s13224-017-1047-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-017-1047-7