Abstract
Study Objectives
This meta-analysis was performed to compare the outcomes between NACT-S and RT for locally advanced cancer cervix. The primary end points were survival benefits.
Searching Method
The data sources for the search included medline, national library of medicine, and the embase search engines. Inclusion criteria included studies published between 2000 and 2012, and FIGO stages IB2 to IVA. Studies had to be properly randomized, prospective, or retrospective and only phase III. Further, the studies had to be with two arms, including one arm for neoadjuvant chemotherapy then-surgery (NACT-S), and the other arm for radiotherapy (RT).
Results
Data were collected from 1171 patients enrolled in seven phase III trials. The 5-year PFS (progression-free survival) for NACT-S and RT were 62 and 45.5 %, respectively. The 5-year OS for NACT-S and RT were 66 and 49 %, respectively. NACT-S was associated with better late toxicities compared to RT.
Conclusion
NACT-S is a reasonable treatment option for locally advanced cancer cervix. It achieved better results than RT, especially for stages from IB2 to IIB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cervical cancer is the most prevalent gynecological malignancy in many developing countries [1].
Since 1999, concurrent chemoradiotherapy (CCRT) has been considered the standard treatment for locally advanced cancer cervix (Féderation Internationale de Gynécologie et d’Obstétrique (FIGO) stages from IB2 bulky (tumor > 4.0 cm) to stage IVA (tumor spreading to adjacent organs) [2, 3].
Many trials have shown the benefits of CCRT over radiotherapy (RT) in terms of local control and survival [4].
However, recent trials showed that, CCRT is associated with quiet significant toxicities, especially late toxicities—in particular grade 3, 4 urinary, and bowel late toxicities ranging from 16 to 18 % [5, 6].
As one of the treatment strategies for cervical cancer, neoadjuvant chemotherapy then surgery (NACT-S) is an attractive option as chemotherapy administered prior to surgery and has advantages such as ability to reduce tumor size, expeditious micrometastasis treatment, improved operability and surgical downstaging, and leading to improvement in overall survival (OS) [7, 8].
A recent systemic review was performed by the author to show the efficacy of NACT-S in locally advanced cancer cervix. The systemic review included data from 30 phase II and III trials. The study showed that NACT-S was associated 5-year progression-free survival (PFS) and overall survival (OS) of 61.9 and 72.8 %, respectively. Further, NACT-S was associated with mild toxicity profile including mild late toxicities [9, 10].
Study Objectives
This meta-analysis was performed to compare the outcome measures between NACT-S and RT for locally advanced cancer cervix. The primary end points were OS and PFS benefits. The secondary end points were treatment response and toxicities.
Method
Randomized trials identified through searches of the medline search engine @ http://clinicaltrials.gov/ct2/search/advanced, the national library of medicine search engine @ http://www.ncbi.nlm.nih.gov/pubmed, and the embase search engine @ http://www.embase.com.
Inclusion Criteria
Inclusion criteria included studies published between January 1, 2000 and December 31, 2012, and FIGO stages IB2 to IVA. Histologies included either squamous cell, adeno, or adenosquamous carcinoma. Studies had to be properly randomized, prospective, or retrospective and only phase III (based on comparison). Patients included should be chemotherapy naïve or cancer cervix chemotherapy naïve. Studies had to be with two arms including one arm for neoadjuvant chemotherapy then surgery (NACT-S) and the other arm for definitive RT.
Exclusion Criteria
Exclusion criteria included metastatic cancer cervix (FIGO stage IVB), phase 1, 2 trials, and case presentations. Studies included rare pathological variants; for example, small cell and clear cell were further excluded. Trials which included RT at neoadjuvant setting were also excluded, as well as studies that are not well randomized.
Outcome Measures
Response to neoadjuvant chemotherapy was defined based on WHO criteria. Complete Response (CR) which means complete disappearance of the tumor, Partial Response (PR) meaning 50 % or more reduction in the tumor, Disease Progression (DP) which means at least 25 % increase in the tumor, and stable disease (SD) which included all other situations.
PFS was defined as the time from start of treatment till progression, relapse, recurrence, death, or the date of last follow up. OS was defined as the time from start of treatment till death or the date of last follow up of the study [11].
Statistical Analysis
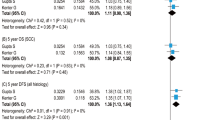
All statistical Analysis was performed using prism 6 software. The study applied mean, median, average, and 95 % confidence interval to analyze included data. Publication bias was assessed funnel plots visual inspection. Forest plot was applied for comparison of survival data. Statistical heterogeneity was analyzed by either X 2, or I 2 test. p value > 0.1 for X 2 test and I 2 value < 25 % were interpreted as signifying low levels of heterogeneity.
Results
Searching for phase III trials on the above scientific engines by typing some or all of the following phrases: “neoadjuvant chemotherapy versus RT in locally advanced cancer cervix,” for trials published between January 1, 2000 and December 31, 2012 identified seven studies. All of the included trials fit with the current meta-analysis inclusion criteria. The trial designs are shown in Table 1.
Data were collected from 1171 patients. Of them, 674 underwent NACT-S, and 497 underwent definitive RT. (57.5 and 42.5 %, respectively). Patients’ characteristics are summarized in Table 2.
For the NACT-S arm, response to chemotherapy was checked in 90 % of patients. Of them, 103 patients (17 %) achieved CR; 286 patients (48 %) achieved PR; and 182 patients (30 %) had SD. The remaining 34 patients (5 %) had disease progression.
Data were included for pathological evaluation of surgery specimen in three trials for those who achieved CR, where 45 % patients of them who had clinical CR were found to have pathological CR, and 55 % of the clinical CR patients had pathological partial remission (microscopic residual disease).
Survival Results
The survival data were included in all the seven trials. The trial of Kornovski and Gorchev [16] included only 2-year survival data, with no further data. The study of Choi et al. [15] included survival data for 5 and 10 years also.
The overall 5-year PFS for NACT-S, and RT were 62, and 45.5 %, respectively. The overall 5-year OS for NACT-S and RT were 66 and 49 %, respectively. Further, the 10-year OS for NACT-S and RT were 60.4 and 25 %, respectively.
Three studies included data about survival grouped by staging. The 5-year OS of stages IB2 to IIA for NACT-S and RT were 72 and 60 %, respectively. The 5-year OS of stages IIB for NACT-S and RT were 62 and 53 %, respectively. The 5-year OS of stages III for NACT-S and RT were 45 and 40 %, respectively. (Figs. 1, 2).
Further, the study of Kornovski and Gorchev [16], reported more pelvic recurrence in the RT arm. The study of Yin et al. [18], reported better 5-year OS with paclitaxel and cisplatin versus cisplatin, vincristine, bleomycin (improvement by 15 %).
Toxicity Profiles
Toxicity included early and late toxicity. Early toxicity was defined as that occurred since treatment till 6–8 weeks post chemotherapy. Late toxicity referred to that happened >8 weeks after treatment. (Table 3).
For arm A, Delay of chemotherapy cycles for 1–2 weeks occurred in 25 % of cycles. No documented deaths occurred related to chemotherapy side effects.
The relative risk of early grade 3, 4 toxicities for NACT-S versus RT was 1.3 (p value 0.1). The relative risk of late grade 3, 4 toxicities for NACT-S versus RT was 0.33 (p value 0.15).
Discussion
The role of NACT-S in locally advanced cancer cervix is still unclear. Few trials included such treatment probably because of the fact that a standard treatment is available with considerable efficacy. The aim of the current meta-analysis was to explore the benefits of NACT-S by comparing it with the available treatments in phase III trials (RT), taking into account the fact that, there are no published phase III trials compared between NACT-S and CCRT yet. Comparing NACT-S with surgery might be beneficial only for early stages IB2-IIA. However, for higher stages, the data about surgery are very few and unclear [19].
CCRT is the standard treatment of locally advanced cancer cervix based on many trials. A meta-analysis of 13 trials compared between CCRT and radiotherapy observed 6 % improvement in 5-year OS with CCRT, improved 5-year PFS by 10 %, and reduced local and distant recurrence [20].
Another important evidence for the CCRT is the study of Morris et al. [21]. The authors compared outcome measures between CCRT using cisplatin and 5 fluorouracil, and RT. They observed 5-year OS of 73 and 58 %, respectively. Further, the corresponding values for 5-year PFS were 67 and 40 %, respectively [21].
On comparing the current results with those of the above trials, NACT-S seemed to achieve comparable results with CCRT in terms of OS and PFS.
When looking for the early toxicities, the study of Morris et al. [21] showed that the early side effects occurred in 64 % of the group that underwent CCRT, with hematological toxicities being the highest (37 %). The current meta-analysis showed lower early toxicity profile (35.5 %). When considering the late toxicities, the study of Morris et al. [21] reported grades 3 and 4 late toxicities in 12 % of their patients. In the current meta-analysis, the grades 3 and 4 late toxicities were found in 8.9 % of the patients.
Further, the high rate of early toxicity in the current meta-analysis can be attributed to the chemotherapy regimens used. The commonly used combination was that of cisplatin, vincristine, and bleomycin, which was associated with significant toxicities. This chemotherapy regimen is not currently the standard for adjuvant/neoadjuvant settings in cancer cervix, but rather the combinations of cisplatin, paclitaxel, or cisplatin, and 5 flurouracil [22, 23].
A systemic review was conducted through Cochrane database, which included 872 patients from five trials to compare outcome measures between NACT-S and RT, and those authors cited above observed better results with NACT-S, with some degrees of heterogeneity. The current meta-analysis was based on higher numbers of patients, from larger numbers of trials, over shorter duration, and with lower level of heterogeneity [24].
Heterogeneity is the major problem that is encountered by researchers conducting meta-analysis. The current meta-analysis was based only on phase III trials, and was conducted through relatively short duration in order to minimize heterogeneity.
When looking for the survival differences by stages, it is reasonable to say that NACT-S achieved better survival results for stages IB2-IIB than stage III. Clinical studies are still needed to explore this ambiguous point. Further, the current trial included many chemotherapy regimens. All of them included cisplatin. However, it failed to show the best regimen with better results. Probably the answer to this question came from the trial of Yin et al. [18], which showed improved survival results with paclitaxel and cisplatin versus cisplatin, vincristine, bleomycin, by 15 %.
However, this question needs to be explored from further clinical trials.
Conclusion
NACT-S is a reasonable treatment option for locally advanced cancer cervix. It achieved better results than RT, especially for stages from IB2 to IIB. Further studies are needed to clarify the best chemotherapeutic regimen and identify the definite role of NACT-S in stage III cancer cervix.
References
Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer. 1999;80:827–41.
Rose PG, Bundy BN, Watkins EB, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999;340:1144–53.
Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009;105(2):103–4.
Green JA, Kirwan JM, Tierney JF, et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systematic review and meta-analysis. Lancet. 2001;358:781–6.
Tan LT, Zahra M. Long-term survival and late toxicity after chemoradiotherapy for cervical cancer d the Addenbrooke’s experience. Clin Oncol. 2008;20:358–64.
Monk BJ, Tewari KS, Koh WJ. Multimodality therapy for locally advanced cervical carcinoma: state of the art and future directions. J Clin Oncol. 2007;25(20):2952–65.
Kigawa J, Minagawa Y, Ishihara H, et al. The role of neoadjuvant intraarterial infusion chemotherapy with cisplatin and bleomycin for locally advanced cervical cancer. Am J Clin Oncol. 1996;19:255–9.
Panici PB, Scambia G, Baiocchi G, et al. Neoadjuvant chemotherapy and radical surgery in locally advanced cervical cancer. Prognostic factors for response and survival. Cancer. 1998;67(2):372–9.
Osman M: The role of neoadjuvant chemotherapy in management of locally advanced cancer cervix: a systemic review. Oncology reviews. 2014; 8(2):60–6. (Part of this trial was discussed in the ESMO (European society of medical oncology) meeting 2014, Madrid, Spain)
Patrick T, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. (Special alert). J Natl Cancer Inst. 2000;92(3):205–16.
World Health Organization. WHO handbook for reporting results of cancer treatment, vol. 48. Geneva: World Health Organization; 1979. p. 22–7.
Chang TC, Lai CH, Hong JH, et al. Randomized trial of neoadjuvant cisplatin, vincristine, bleomycin, and radical hysterectomy versus radiation therapy for bulky stage IB and IIA cervical cancer. J Clin Oncol. 2000;18(8):1740–7.
Benedetti-Panici P, Greggi S, Colombo A, et al. Neoadjuvant chemotherapy and radical surgery versus exclusive radiotherapy in locally advanced squamous cell cervical cancer: results from the Italian multicenter randomized study. J Clin Oncol. 2002;20(1):179–88.
Napolitano U, Imperato F, Mossa B, et al. The role of neoadjuvant chemotherapy for squamous cell cervical cancer (Ib-IIIb): a long-term randomized trial. Eur J Gynaecol Oncol. 2003;24(1):51–9.
Choi YS, Sin J, Kim J, et al. Survival benefits of neoadjuvant chemotherapy followed by radical surgery versus radiotherapy in locally advanced chemoresistant cervical cancer. J Korean Med Sci. 2006;21:683–9.
Kornovski Y, Gorchev G. Neoadjuvant chemotherapy followed by radical surgery and radiotherapy vs. pelvic irradiation in patients with cervical cancer FIGO stage IIB—IVA. J BUON. 2006;11(3):291–7.
Yamauchi N, Sameshima H, Fukushima K, et al. A randomized trial of neoadjuvant chemotherapy followed by radical surgery versus radiotherapy alone in Stage IIIb carcinoma of the uterine cervix. J Gynecol Surg. 2010;26(2):105.
Yin M, Zhao F, Lou G, et al. The long-term efficacy of neoadjuvant chemotherapy followed by radical hysterectomy compared with radical surgery alone or concurrent chemoradiotherapy on locally advanced-stage cervical cancer. Int J Gynecol Cancer. 2011;21(1):92–9.
Rydzewska L, Tierney J, Vale CL, et al. Neoadjuvant chemotherapy plus surgery versus surgery for cervical cancer. Cochrane Database Syst Rev. 2010. doi:10.1002/14651858.
Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: a systematic review and meta-analysis of individual patient data from 18 randomized trials. J Clin Oncol. 2008;26(35):5802–12.
Morris M, Eifel PJ, Lu J, et al. Pelvic radiation with concurrent chemotherapy versus pelvic and para-aortic radiation for high-risk cervical cancer: a randomized Radiation Therapy Oncology Group clinical trial. N Engl J Med. 1999;340:1137–43.
Lorusso D, Petrelli F, Coinu A, et al. A systematic review comparing cisplatin and carboplatin plus paclitaxel-based chemotherapy for recurrent or metastatic cervical cancer. Gynecol Oncol. 2014;133(1):117–23.
Whitney CW, Sause W, Bundy BN, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: gynecologic oncology group and southwest oncology group study. J Clin Oncol. 1999;17(5):1339–48.
Neoadjuvant Chemotherapy for Cervical Cancer Meta-Analysis Collaboration (NACCCMA). Neoadjuvant chemotherapy for locally advanced cervix cancer. Cochrane Database Syst Rev. 2004;(2): CD001774.
Compliance with ethical requirements and Confilct of interest
The author declare that all the included seven trials included data that they did not receive any financial support from pharmaceutical companies. One trial received support from Cancer Research Campaign of the UK. All the studies included a statement related to no potential conflicts of interest. Four trials included data that they were approved from their local ethical committees.
Author information
Authors and Affiliations
Corresponding author
Additional information
Mohammed A. Osman is a Consultant at General Organization for Teaching Hospitals, Institutes.
Rights and permissions
About this article
Cite this article
Osman, M.A. Defining the Role of Neoadjuvant Chemotherapy Followed by Surgery in Locally Advanced Cancer Cervix: A Meta-analysis of Phase III Trials. J Obstet Gynecol India 66, 352–357 (2016). https://doi.org/10.1007/s13224-015-0696-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-015-0696-7