Abstract
Background
Controlled ovarian hyperstimulation (COH) for in vitro fertilization (IVF) is essential in improving the pregnancy rate, but supraphysiologic levels of estradiol (E2), which are attained during COH and which affect the outcome of IVF, have remained unclear. The aim of this study was to evaluate the association of E2 levels on the day of hCG with embryo quality and pregnancy rates in long protocol in IVF.
Materials and Methods
We retrospectively reviewed 128 IVF cycles. All the patients were stimulated with long protocol. The patients were categorized into three groups according to the serum E2 levels on hCG administration day (group 1; <1500 pg/ml, group 2; 1500–3500 pg/ml, group 3; >3500 pg/ml).
Results
Of the 128 cycles, 23 (18 %) cycles resulted in pregnancy. There were no statistically significant differences between mean age, duration of infertility, BMI and FSH on cycle day 3 in three groups. The number of the retrieved oocytes, the number of obtained embryos, the number of transferred embryos, and pregnancy rates were gradually increased from group 1 to 3 as estradiol levels increased, and these values were statistically significant (P < 0.05). In addition, the correlation between age and IVF outcome was found. Mean age in patients with positive pregnancy test was lower than that in patients with negative pregnancy test, and this difference was statistically significant.
Conclusion
This study shows that there is a positive association between estradiol level on hCG administration day and pregnancy rates in IVF cycles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infertility means inability to attain pregnancy even after 1 year of regular intercourse without the use of contraceptive method [14]. Some infertile patients are candidates for assisted reproductive technology (ART) [1]. An important part of ART is controlled ovarian hyperstimulation which produces multifollicular development and subsequent supraphysiological estradiol hormone [10]. The estradiol level may be increased by more than tenfold in comparison with natural cycle [3].
Because the endometrial preparation for embryo implantation is regulated by ovarian hormones, it has been hypothesized that high levels of estradiol are likely to affect endometrial receptivity. In recent years, numerous studies have reported conflicting results. Simon et al. [11] have reported that high levels of estradiol lead to reduced endometrial receptivity, but do not affect the quality of oocytes and embryos. In vitro studies have shown that high levels of estradiol induce a toxic effect on the cleavage stage embryos [12]. Kosmas et al. [6] in their systematic review reported the levels of E2 do not affect the outcome of pregnancy.
The aim of present study was to evaluate the association of E2 levels on the day of hCG administration with embryo quality and pregnancy rates in a GnRH agonist and HMG protocol.
Materials and Methods
Patient Population
In this retrospective cohort study, all women aged from 19 to 45 years who underwent IVF cycles at Shahid Beheshti Hospital in Kashan, Isfahan Province, central part of Iran between 2007 and 2013 were identified. We excluded those cycles without accurate medical record. Analysis was limited to 128 cases for which complete clinical data on pregnancy outcomes were available. For an expected pregnancy rate of 14 % for patients with minimum estradiol level and 45 % for patients with maximum estradiol level, a sample size of 40 patients per group was required for a statistical power of 90 % at a P level of 0.05 using this formula:
Ovarian Stimulation
In this study, the patients underwent the standard down-regulation using GnRH agonist (Superfact, Aventis, Frankfurt, Germany). A dosage of 0.5 mg subcutaneous daily was started on the 21st day of the previous cycle. When pituitary desensitization was confirmed (endometrial thickness <5 mm and serum estradiol level <50 pg/ml), the dose of Superfact was reduced to 25 µg.
Ovarian stimulation was started with a dose of 75 IU, 150 IU or 225 IU HMG (Merional, IBSA, Switzerland). It was continued until the day of ovulatory hCG administration according to the ovarian response. When at least two follicles were greater than 18 mm, 10,000 IU urinary hCG intramuscularly (Choriomon, IBSA, Lugano, Switzerland) was administered for ovulation and oocyte retrieval was performed 34–36 h later. Obtained oocytes were injected by ICSI. The first evolution was done at 18–24 h and another at 48 h after fertilization, after which four cells’ embryos were transferred to uterus.
Luteal Supplementation
The patients used progesterone suppositories (Cyclogest, 400 mg BD vaginally, Alpharma, England).
Outcome Measures
The sign of chemical pregnancy (positive β-hCG test, i.e., >25 IU/ml) was considered as outcome measure. The quantitative serum β-hCG level analysis after 14 days of progesterone administration was performed for pregnancy test. On the day of hCG injection, serum estradiol level of the patient was measured by the same laboratory and based on the level, the patients were divided into three groups: group 1 (estradiol <1500 pg/ml), n = 45; group 2 (estradiol 1500–3500 pg/ml), n = 35; group 3 (estradiol >3500 pg/ml), n = 48.
Ethical Considerations
The Ethics Committee of the Kashan Medical University approved the study.
Statistical Analysis
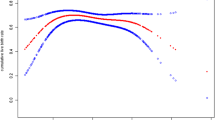
Sociodemographic characteristics of the participants were stated as mean ± SD or case (percentage) elsewhere. The data were compared using one-way analysis of variance (One-Way ANOVA) and cochran tests and linear regression. The chemical pregnancy was compared between groups by cochran test. Data analysis was carried out using SPSS, version 16. P values were set as 0.05 for all analyses.
Results
We included 128 cases in the present study, who had accurate medical record. The sociodemographic characteristics between groups were compared according to age, duration of infertility, FSH on 3rd day of menstruation, and BMI (Table 1). No significant differences are seen with respect to age, FSH level, and BMI in subgroups based on estradiol level.
There is a significant relation between estradiol level on hCG injection day and pregnancy outcome; participants with higher estradiol level had higher pregnancy rate compared with other groups. Retrieved oocytes, obtained embryos, and transferred embryos are significantly increased in patients in high estradiol level group. Pregnancy rate was significantly increased in high estradiol group (31.2 %) compared with low estradiol group (8.9 %) (Table 2).
Discussion
Our data have shown that there are positive associations between estradiol level on hCG administration and retrieved oocytes, obtained embryos, transferred embryos, and pregnancy rate. These findings are consistent with Kara et al’s [5] study which reported the positive correlations between E2 level on hCG administration day and retrieval of oocytes, availability of blastocysts, and pregnancy rates [5]. Moreover, Blazer et al. [2] have shown certain findings consistent with our results. It is important to note that, estradiol is a hormone which is produced by granulosa cells by aromatization of androstendione to estradiol in follicular phase, and elevated E2 peak enhanced the oocytes maturation by increasing meiotic competency [2]. In addition, the peak E2 sustains the optimal levels of progesterone during embryo implantation and the luteal phase of the female cycle. E2 and progesterone regulate local production of growth factors, cytokines, and cyclooxygenase-derived prostaglandins through autocrine and paracrine pathways [2].
On the contrary, some studies have suggested that there is no association between pregnancy achievement and E2 serum level on hCG day. Kyrou [7] have reported a lack of association in antagonist cycles and basal FSH [7]. Ozcakir et al. [9] have evaluated this association after use of clomiphene citrate and HMG followed by intrauterine insemination of 180 patients and reported that there is no correlation between E2 level and clinical pregnancy [9]. Also, Mitwally et al. [8] have investigated the association of E2 level during COH and peak E2 pregnancy outcome in 270 patients and reported the positive correlation between estradiol during COH and pregnancy outcome, but not between E2 on hCG administration day and pregnancy outcome. In their study, they used GnRH agonist and gonadotropin [8]. E2 level in IVF procedure is subject of GnRH agonist and antagonist for down-regulation of ovary controlled by COH. In COH protocol, E2 increased tenfold in natural cycle; however, significant deviation from the physiologic level of E2 has detrimental effect on endometrium, embryo implantation, and subsequently on pregnancy rate [4].
As mentioned above, there are some controversies in different studies; this is due to different stimulation protocols in comparison to our study. However, similar to our study, a recent study by Wu et al. [13] on infertile women undergoing a short or long protocol GnRH agonist/recombinant FSH or HMG treatment also demonstrated that high serum estradiol concentration on hCG day did not affect the IVF pregnancy outcome [13]. Another hypothesis is proposed that these controversies are subject to sample size, which implies that there is no positive correlation in studies with greater sample size. Estrogen increases endometrial proliferation and uterine perfusion which improves the chance of pregnancy. E2 may disrupt the implantation process through endometrial damage which is responsible for the negative effect of E2 on IVF–ICSI outcome [9].
Despite the well-designed structure, the present study possesses some limitations, as follows (i) the number of included subjects was small (ii) no follow-up of patients for clinical pregnancy and live birth rate.
Conclusion
Retrieved oocytes, obtained embryos, and transferred embryos are significantly higher in the presence of high E2 levels on the day of hCG administration, which has a positive association with pregnancy rates in IVF with long protocol. However, there is risk of OHSS. COH for IVF should lead to an optimum rather than maximum number of oocytes without compromising uterine receptivity or embryo implantation.
References
Agarwal A, Gupta S, Sharma RK. Role of oxidative stress in female reproduction. Reprod Biol Endocrinol. 2005;3:28.
Blazar AS, Hogan JW, Frankfurter D, et al. Serum estradiol positively predicts outcomes in patients undergoing in vitro fertilization. Fertil Steril. 2004;81:1707–9.
Fisher S, Grin A, Paltoo A, et al. Falling estradiol levels as a result of intentional reduction in gonadotrophin dose are not associated with poor IVF outcomes, whereas spontaneously falling estradiol levels result in low clinical pregnancy rates. Hum Reprod. 2005;20:84–8.
Friedler S, Zimerman A, Schachter M, et al. The midluteal decline in serum estradiol levels is drastic but not deleterious for implantation after in vitro fertilization and embryo transfer in patients with normal or high responses. Fertil Steril. 2005;83:54–60.
Kara M, Kutlu T, Sofuoglu K, et al. Association between serum estradiol level on the hCG administration day and IVF-ICSI outcome. Iran J Reprod Med. 2012;10:53–8.
Kosmas IP, Kolibianakis EM, Devroey P. Association of estradiol levels on the day of hCG administration and pregnancy achievement in IVF: a systematic review. Hum Reprod. 2004;19:2446–53.
Kyrou D, Popovic-Todorovic B, Fatemi HM, et al. Does the estradiol level on the day of human chorionic gonadotrophin administration have an impact on pregnancy rates in patients treated with rec-FSH/GnRH antagonist? Hum Reprod. 2009;24:2902–9.
Mitwally MF, Bhakoo HS, Crickard K, et al. Estradiol production during controlled ovarian hyperstimulation correlates with treatment outcome in women undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2006;86:588–96.
Ozcakir HT, Goker EN, Terek MC, et al. Relationship of follicle number, serum estradiol level, and other factors to clinical pregnancy rate in gonadotropin-induced intrauterine insemination cycles. Arch Gynecol Obstet. 2002;266:18–20.
Rosen MP, Shen S, Rinaudo PF, et al. Fertilization rate is an independent predictor of implantation rate. Fertil Steril. 2010;94:1328–33.
Simon C, Cano F, Valbuena D, et al. Clinical evidence for a detrimental effect on uterine receptivity of high serum oestradiol concentrations in high and normal responder patients. Hum Reprod. 1995;10:2432–7.
Valbuena D, Martin J, de Pablo JL, et al. Increasing levels of estradiol are deleterious to embryonic implantation because they directly affect the embryo. Fertil Steril. 2001;76:962–8.
Wu Z, Li R, Ma Y, et al. Effect of HCG-day serum progesterone and oestradiol concentrations on pregnancy outcomes in GnRH agonist cycles. Reprod Biomed Online. 2012;24:511–20.
Zegers-Hochschild F, Adamson GD, de Mouzon J, et al. The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology, 2009. Hum Reprod. 2009;24:2683–7.
Acknowledgments
We thank the staff of the Department of Infertility at the Kashan University of Medical Sciences.
Compliance with ethical requirements and Conflict of interest
The Ethics Committee of the Kashan Medical University approved the study. The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Foroozanfard, F., Moraveji, S.A., Taghavi, S.A. et al. Association Between Serum Estradiol Level on the Day of hCG Administration and IVF–ICSI Outcome. J Obstet Gynecol India 66, 170–173 (2016). https://doi.org/10.1007/s13224-015-0687-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-015-0687-8