Abstract
Antibiotics and immunotherapies possess unavoidable adverse effects that hinder sepsis management. Herbal drugs have demonstrated potential immunomodulatory properties vital for sepsis treatment. We hypothesized in the present study that the use of Carica papaya leaves extract had the potential to improve survival and modulate immune cytokine release during sepsis. Animals were subjected to cecal ligation and puncture (CLP) to induce sepsis. Septic rats divided into 10 groups received ethanol extract of C. papaya leaves (50 and 100 mg/kg), imipenem (120 mg/kg) and cyclophosphamide (CP, 10 mg/kg). To investigate the immunomodulatory potentials of EE, cytokine levels like interleukin (IL-6), tumor necrosis factor (TNF-α), and IL-10 along with hematological and biochemical parameters were analyzed. Our results exhibited improved survival rates concerning ethanol extract treatment alone and in combination with imipenem and CP (100%) as compared to the CLP group (33.3%) on day 7 post-surgery. The combination treatment of ethanol extract with imipenem and CP significantly (P < 0.001) ameliorated cytokine levels and hematological and biochemical parameters in septic rats. A histopathological examination suggested improved liver and kidney tissue condition after combination treatment as compared to the CLP group. Therefore, it was concluded that combination therapy of extract with imipenem and CP improved survival rates and marked immunomodulatory potential in septic rats compared to monotherapy. The findings suggested the use of a mixture of these drugs in clinical settings to treat sepsis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a congregation of physiological, pathological, and biochemical reactions caused by the invasion of microbes (bacteria, fungi and virus) or trauma, resulting in the activation of immune response (Huang et al. 2019). It is a leading cause of mortality and morbidity which accounts for 49 million cases and 11 million deaths globally, as reported by the Global Burden of Disease in 2017. Sepsis is a hyperinflammatory immune response manifested by abnormal secretion of pro-inflammatory and anti-inflammatory cytokines due to microbial insult (Christaki et al. 2011). Dysregulated release of free radical species causing oxidative stress, uncontrolled functioning of coagulation cascade inhibiting fibrinolysis and producing thrombosis contribute to organ dysfunction and mortality in sepsis (Usmani et al. 2021). Activation of platelets leads to inflammation of vessels and further contributes to sepsis (Dewitte et al. 2017). The liver and kidney are two prominent abdominal organs afflicted by dysfunction caused by sepsis (Sapin et al 2017).
Therapies capable of modulating the immune system have gained much attention in the treatment of sepsis. Drugs like doxycycline, tetracycline, and azithromycin claim to hold clinical benefits by suppressing cytokine and chemokines production (Shapira et al. 1996; D’Agostino et al. 1998; Patel et al. 2018). Anti-infective therapies and supportive care are the primordial therapy against sepsis (Rhodes et al. 2017). However, complications related to sepsis continue to grow (Gaieski et al. 2013). Also, antibiotic resistance may develop due to repeated and unnecessary drug administration (Zilahi et al. 2016). Taking into consideration the pathophysiology involved in sepsis, immunotherapy has taken a quantum leap in sepsis treatment (Hotchkiss and Opal 2010). However, previous studies reported the utilization of immunostimulatory drugs in clinical practice has not shown promising outcomes (Zeni et al. 1997; Weighardt et al. 2000; Watanabe et al. 2018). Therefore, therapeutic approaches against sepsis require to be renewed in order to minimize the mortality rate and enhance immunity.
Drugs of herbal origin exhibit immune system-altering properties by diverse mechanisms. Medicinal plants have reportedly mediated the release of inflammatory cytokines, along with the restriction of the cell proliferation, production of nitric oxide, and stimulation of antioxidant enzyme activities thereby ameliorating the diseased condition (Mukherjee et al. 2014; Jantan et al. 2018; Upadhyay et al. 2021). In particular, Carica papaya leaves tend to possess many active phytocomponents that are responsible to ameliorate oxidative stress, increase platelets and modulate the immune response to infection (Usmani et al. 2021).
Therefore, in the present study, we hypothesized that the C. papaya leaves combined with imipenem and CP could alleviate inflammation and impair organs of the body affected by sepsis. The effect of leaf extract on the survival rate in septic rats was also explored.
Material and methods
Animal procurement
The experiment was carried out on albino rats of either sex, weighing 250–350 g, and 8–10 weeks old. Animals were procured from Laboratory Animal Breeding and Research Centre, Jamia Hamdard University, New Delhi after the protocol was approved by the university’s Institutional Animal Ethics Committee (IAEC) (protocol number 1645). The animals were housed in polypropylene cages (4 per cage) with husk as bedding material under laboratory conditions with a controlled environment of temperature 22 ± 3 °C, humidity (60 ± 10%), and 12 h light/dark cycle. They were fed with a standard rodent pellet diet (from Lipton India) and drinking water.
Cecal ligation and puncture-induced sepsis model
Animals were weighed and anesthetized with Ketamine (80 mg/kg) and Xylazine (10 mg/kg) injected intraperitoneally (i.p.). The experiment was performed aseptically in a laminar flow cabinet. The animals were placed in an upright position in the working area and fixed the paws with adhesive tape. The abdominal area was disinfected and shaved. Approximately 2 cm long midline abdominal incision was made and 2/3rd part of the cecum was exposed. A 4–0 silk suture was used to ligate the cecum and punctured at three different points with the help of a 21 gauge needle. The cecum was squeezed to ooze out the waste material into the peritoneal cavity and the abdomen was closed in two layers with 4–0 sutures. A pre-warmed normal saline (1 ml) was injected subcutaneously into all animals immediately after performing surgery. Animals were observed for 30 min post-surgery (Kalechman et al. 2002). The rats that showed lethargy with no improvement or moribund behavior were euthanized.
Drugs and chemicals
Imipenem was procured from Glenmark Pharmaceutical LTD., Mumbai, India and cyclophosphamide was obtained from Getwell Pharma India Private Limited. Haryana, India. Hematoxylin and Eosin, and ethanol, were bought from the company of Sigma–Aldrich (St Louis, MO, USA). Analytical grade chemicals were used and distilled water was used for their solubilisation.
Plant collection and extraction
C. papaya leaves were purchased from the Jamia Hamdard campus located in New Delhi, India. A botanist from the Department of Botany, School of Chemical and Life Sciences, Jamia Hamdard, New Delhi authenticated the plant, where a voucher specimen (BOT/DAC/2021/06) was deposited for record purposes.
For the preparation of extract, soxhlet extraction was carried out which is a temperature-controlled method and requires less amount of solvent. Also, dry and fine solid samples can be extracted using this method (Bryda and Stadnytska 2021). C. papaya leaves were washed in distilled water to remove dust particles and shade dried for 2–3 days. Then the dried plant material was crushed to ground it to powder. The powdered material (58 g) was then extracted for 24 h in the soxhlet apparatus using 500 ml ethanol with intermittent shaking. This procedure was carried out at 78 °C and the solvent was allowed to dry using a rotary evaporator at 65 °C. The prepared extract was oven dried at 64 °C, till crude extract is obtained. The resultant dried extract was stored at 2–4 °C until further use.
Treatment regimen
The animals were divided into ten groups consisting of 6 animals each. The rats in group I were administered with dimethyl sulfoxide (DMSO) as vehicle control, while group II animals were considered as toxic control and underwent CLP with no drug treatment. Group III remained EE Per se (100 mg/kg) extract as no CLP was performed. Group IV and group V animals were injected with 50 mg/kg ethanol extract (EEI) and 100 mg/kg ethanol extract (EEII), respectively. Imipenem (120 mg/kg) was injected into animals in group VI. Animals in group VII and group VIII were given Imipenem (120 mg/kg) + EEI(50 mg/kg) and Imipenem (120 mg/kg) + EEII(100 mg/kg), respectively, whereas, group IX and X animals were injected with Imipenem (120 mg/kg) + EEI(50 mg/kg) + CP (10 mg/kg, dissolved in saline) and Imipenem (120 mg/kg) + EEII(100 mg/kg) + CP (10 mg/kg), respectively.
All the drugs were injected (i.p.), 6 h post-surgery, every 12 h for 7 days. For the survival study, experimental rats were monitored for 7 days.
At the end of the experiment (on day eight, 12 h after the last dose of the drug) animals were euthanized and blood was collected via cardiac puncture. Blood samples were then centrifuged at 2000 rpm for 15 min to separate the serum. Serum was collected in EP tubes for inflammatory and biochemical markers estimation, and stored at – 80 ℃ till further use. Tissue samples of the liver and kidney were collected, washed with normal saline, and fixed in 10% formalin for further histopathological examination.
Cytokine analyses
IL-6, TNF-α, and IL-10 serum levels were detected by the enzyme linked-immunosorbent assay (ELISA) method in accordance with the manufacturer’s instructions. The IL-6 and TNF-α ELISA kits were purchased from Krishgen Biosystems, Mumbai, India, and the IL-10 ELISA kit was purchased from Fine Biotech Co., LTD., China.
Biochemical estimation
Kidney function parameters include serum creatinine (SC), blood urea nitrogen (BUN), albumin, and liver function parameters like an alanine aminotransferase (ALT), and alkaline phosphatase (ALP) were performed in VETLAB, South Delhi, India (Nnaemeka et al. 2023). Antioxidant parameters such as lactate dehydrogenase (LDH), and creatinine kinase (CK) were performed by using assay kits purchased from Elabscience, New Delhi as directed by the manufacturer (Mannaa et al. 2014). Superoxide dismutase (SOD) was determined by the method of Resim et al. 2015 and lipid peroxidase was measured as using the method described by Petronilho et al. 2016. Glutathione (GSH) was measured as previously described by Lee et al. (2017).
Hematological estimation
Blood samples for Prothrombin time (PT) and Plasma fibrinogen were collected in sodium citrate vials while plain vials contained blood samples for haemoglobin (Hb), complete blood count (CBC) measurement, and EDTA vial was used for collecting blood for erythrocyte sedimentation rate (ESR) estimation. The blood samples were analyzed by VETLAB, South Delhi, India (Somayaji et al. 2016).
Liver and kidney histopathology
After 7 days of drug therapy and post-CLP, liver and kidney tissues were collected, subsequently flushed with PBS, and kept in 10% formalin for 24–48 h. The tissues were sliced and deparaffinised in ethanol. After fixation, H&E staining was applied at room temperature. Histopathological evaluation was carried out by a pathologist under the light microscope at 100X.
Statistical analysis
All the readings are expressed as mean ± standard deviation in three replicates. The survival study was analyzed using the Log-rank test. The mean weight of all groups was statistically analyzed by the one-way analysis of variance (ANOVA) method. Data from multiple groups of treatment were analyzed using Tukey’s multiple comparison test. A statistically significant difference was expressed as P < 0.05 between toxic and treatment groups. All the statistical examination was performed using GraphPad Prism software (Version 5.01; GraphPad Software Inc.).
Results
Effect of Carica papaya leaves extract, imipenem, and cyclophosphamide on survival of septic rats
The survival rate was estimated to study the effect of imipenem and CP along with papaya leaf extract at the end of relevant treatments. The animals in CLP groups exhibited 100% survival on day 1 which decreased to 83.3% on day 3, 50% on day 4, and 33.3% on day 6 and day 7. However, a combination group of Imipenem + EE I + CP and Imipenem + EE II + CP exhibited 100% survival on day 7 post-surgery. This was significant (P < 0.01) higher as compared to the CLP group. Figure 1 shows the survival curve of experimental rats.
The survival distribution of experimental rats in each group. DMSO, dimethyl sulfoxide (vehicle control); CLP, cecal ligation and puncture (toxic group, no treatment given); EE Per se, ethanol extract of C. papaya leaves (100 mg/kg); EE I, ethanol extract of C. papaya leaves (50 mg/kg); EE II, ethanol extract of C. papaya leaves (100 mg/kg); CP, cyclophosphamide
Estimation of Immunomodulatory potential of Carica papaya leaves extract, imipenem, and cyclophosphamide in septic rats
The serum levels of IL-6, TNF-α, and IL-10 are significantly higher in CLP groups when compared to each group. The cytokines levels were reduced potentially (P < 0.05) in the EE groups alone and in combination with imipenem and CP. However, the cytokine levels in combination groups of EEI and EEII + imipenem + CP marked a statistical significance but at similar non-differentiating levels (P < 0.05). This signifies that ethanol extract in combination with other standard drugs reduces the cytokine levels producing a synergistic effect. Thus, exhibiting immunomodulatory potentials by modulating the immune response to microbial insult. Figure 2 shows the expressions of cytokine levels in rats.
The effect of Carica papaya leaves extract, Imipenem and Cyclophosphamide (CP) on the expression of serum cytokine levels of IL-6 (A), TNF-α (B), and IL-10 (C). The levels of each group were expressed as mean ± SD with statistical significance *P < 0.05 when compared to CLP groups. DMSO, dimethyl sulfoxide (vehicle control); CLP, cecal ligation and puncture (toxic group, no treatment given); EE Per se, ethanol extract of C. papaya leaves (100 mg/kg); EE I, ethanol extract of C. papaya leaves (50 mg/kg); EE II, ethanol extract of C. papaya leaves (100 mg/kg); CP, cyclophosphamide
Estimation of biochemical markers
Kidney parameters
The measurement of SC levels after the administration of EEI and EEII was found to produce a significant difference (P ≤ 0.001) by reducing the CLP-induced increased SC level in rats administered with a cocktail therapy of extract (EEI, and EEII) with imipenem and CP. However, the induction of DMSO, EEI alone, and imipenem showed no significant (P > 0.05) difference in SC levels (Fig. 3A).
The effect of Carica papaya leaves extract, Imipenem and Cyclophosphamide on levels of kidney parameters of rats in each group. A Serum creatinine, B BUN; blood urea nitrogen, and C Albumin in each group were indicated. The threshold significance levels were expressed as nsP > 0.05 (non-significant), *P < 0.05, **P < 0.01, ***P < 0.001 in CLP v/s other groups. DMSO, dimethyl sulfoxide (vehicle control); CLP, cecal ligation and puncture (toxic group, no treatment given); EE Per se, ethanol extract of C. papaya leaves (100 mg/kg); EE I, ethanol extract of C. papaya leaves (50 mg/kg); EE II, ethanol extract of C. papaya leaves (100 mg/kg); CP, cyclophosphamide
Figure 3B represented that the increased BUN levels due to CLP surgery were markedly reduced by the administration of ethanol extracts alone, imipenem, and combinational drug therapy of EEI and EEII along with imipenem and CP (P ≤ 0.001). On the other hand, DMSO and EEI showed less significant (P ≤ 0.01) difference in the reduction of BUN levels.
Also, albumin levels were significantly (P ≤ 0.001) increased in rats who received a combination of EE, imipenem, and CP producing a synergistic effect in comparison to CLP-induced low level of albumin (Fig. 3C).
Liver parameters
Figure 4 exhibited the effect of ethanol extracts, imipenem, and CP on the liver function parameters of rats. CLP-induced increased levels of ALT, and ALP were significantly (P < 0.001) reduced by the administration of a mixture of EEII + imipenem + CP, whereas, the combination of EEI with imipenem and CP produced a less significant (P < 0.05) reduction of ALT and ALP levels. Also, monotherapy of EE (I and II) was found to be effective in improving the liver function parameters (P < 0.001).
The effect of Carica papaya leaves extract, Imipenem and Cyclophosphamide on levels of liver parameters of rats in each group. A ALT; alanine transferase, and B ALP; alkaline phosphatase were indicated in each grouped animal. The threshold significance levels were expressed as *P < 0.05, ***P < 0.001 in CLP v/s other groups. DMSO, dimethyl sulfoxide (vehicle control); CLP, cecal ligation and puncture (toxic group, no treatment given); EE Per se, ethanol extract of C. papaya leaves (100 mg/kg); EE I, ethanol extract of C. papaya leaves (50 mg/kg); EE II, ethanol extract of C. papaya leaves (100 mg/kg); CP, cyclophosphamide
Antioxidant parameters
The effect of administration of ethanol extract of C. papaya leaves, imipenem and CP on antioxidant parameters were analyzed and presented in Fig. 5.
The effect of Carica papaya leaves extract, Imipenem and Cyclophosphamide on antioxidant parameters of rats in each group. A GSH; glutathione, B Creatine Kinase, C LDH; lactate dehydrogenase, D MDA; malondialdehyde, and E SOD; superoxide dismutase in each group were indicated. The threshold significance levels were expressed as nsP > 0.05 (non-significant), *P < 0.05, **P < 0.01, ***P < 0.001 in CLP v/s other groups. DMSO, dimethyl sulfoxide (vehicle control); CLP, cecal ligation and puncture (toxic group, no treatment given); EE Per se, ethanol extract of C. papaya leaves (100 mg/kg); EE I, ethanol extract of C. papaya leaves (50 mg/kg); EE II, ethanol extract of C. papaya leaves (100 mg/kg); CP, cyclophosphamide
The CLP-induced reduced levels of GSH are significantly (P ≤ 0.001) increased by the administration of EEII along with imipenem and CP. A non-significant (P > 0.05) difference was reported by DMSO, EEI alone, and EEI + imipenem groups, as shown in Fig. 5A.
A marked (P ≤ 0.001) reduction of CK levels were seen in septic rats administered with EEII alone, imipenem, and combination therapy of EEII+imipenem + CP as compared to the CLP group, whereas, the non-significant (P > 0.05) difference was observed in DMSO, EEIalone and EEI + imipenem groups. This indicates the synergistic potential of ethanol extract at a higher dose with other drugs (Fig. 5B).
Similarly, from Fig. 5C, it was observed that administering EEII, imipenem and combination therapy of extract and other standard drugs significantly (P ≤ 0.001) decreased the elevated levels of LDH in the CLP rat model.
The determination of MDA (malondialdehyde), an indicator of lipid peroxidation is shown in Fig. 5D. A statistically significant (P ≤ 0.001) difference in MDA levels was observed in septic rats administered with a combination of ethanol extract (50 and 100 mg/kg), imipenem and CP and a combination of ethanol extract (50 and 100 mg/kg), and imipenem when compared to the CLP group. It can be observed that the CLP-induced increased levels of MDA were reduced by the administration of ethanol extract. However, EEI resulted in a slight significance (P ≤ 0.05) reduction in MDA level in comparison to the EEII, indicating the effectiveness of extract at 100 mg/kg dose. On the other hand, DMSO administration produced a slight significant (P ≤ 0.05) reduction in MDA levels when compared to the CLP group.
A statistically significant (P ≤ 0.001) difference was indicated in Fig. 5E with an elevation of SOD levels in the EE II + imipenem + CP combination group, when compared to the CLP group. However, non-significant (P > 0.05) increased levels were observed in DMSO, EE Per se, EEI, imipenem and EEI + imipenem groups of animals.
Estimation of hematology parameters
Table 1 showed the effect of the treatment of ethanol extracts, imipenem and CP on hematology parameters. CLP-induced increased levels of ESR, and PT were significantly (P < 0.001) reduced in animals treated with the combination of EE (I and II) + Imipenem + CP and decreased fibrinogen level was increased in animals treated with the combination of EE (I and II) + Imipenem + CP. A similar trend was followed by EEI except for a non-significant (P > 0.01) fibrinogen level (118 ± 16.4) and EEII treatment groups. However, DMSO-treated rats displayed a non-significant (P > 0.01) level of ESR, fibrinogen and PT and imipenem group rats showed a less significant reduction in the parameters comparatively.
CLP-induced elevated levels of mean corpuscular hemoglobin (MCH) and white blood cell (WBC) levels in an animal model were reduced significantly (p < 0.001) by the administration of ethanol extract alone and in combination with imipenem and CP exhibiting a synergistic value to the treatment (Table 2). Statistical threshold significant (p < 0.001) increase was observed in the levels of hemoglobin, platelets, mean corpuscular volume (MCV), red blood cell (RBC) and haematocrit (HCT) by the treatment of combined therapy of ethanol extracts (I and II) with imipenem and CP in rats. However, EEI and imipenem groups displayed a non-significant (p > 0.05) reduction in MCV levels in animals.
Histopathological analysis
The hematoxylin and eosin (H&E) stained tissues of the liver and kidney of ethanol extract, imipenem and CP treated rats were used for histopathological examination (Fig. 6). The changes in the liver and kidney morphology of septic rats were displayed in Fig. 6. The liver tissue section of the DMSO group demonstrated focal degeneration of hepatocytes with mild inflammation, indicated by a black arrow around the portal triad, as indicated by the red arrow, and focally dilated sinusoids (Fig. 6A1). The kidney tissue section showed focal degeneration of tubular epithelial cells (red arrow) with normal appearing glomeruli (black arrow) as compared to the CLP group (Fig. 6A2). Photomicrographs from the liver tissue of CLP-grouped rats displayed a widening of the portal triad with the presence of dilated and congested portal vein (black arrow) and dilatation of sinusoids. Mild lymphocytic infiltration was also seen in the portal triad. There was elongation and congestion of portal veins with central to central (red arrow) and central to portal fibrosis (Fig. 6B1). The kidney section showed destruction of glomeruli in different stages with one of the glomeruli (Black arrow) completely replaced by proteinaceous/necrotic material (Fig. 6B2). Furthermore, the liver and kidney sections from the EE Per se group displayed normal central vein (red arrow) with portal triads (black arrow) and intervening strands of normal hepatocytes and normal glomeruli and tubules (Fig. 6C1, 2). Section from the liver show dilated and congested sinusoids, whereas, kidney tissue showed single abnormal glomeruli with fibrin deposition (black arrow) along with degeneration of tubular epithelial cells and mild peri-glomerular lymphocytic infiltrate (red arrow) were observed by EEItreated rats (Fig. 6D 1, 2). Animals treated with EEIIdemonstrated a normal portal triad (red arrow) with cords of hepatocytes and normal glomeruli and tubules (black arrow) (Fig. 6E 1, 2). The liver section of imipenem-treated rats exhibited a congested central vein (black arrow) with dilated and congested sinusoids (red arrow) (Fig. 6F1) while kidney tissue showed normal glomeruli and tubules (red arrow) with few congested capillaries (black arrow) (Fig. 6F2). In the combination of EEIand imipenem, liver and kidney tissues displayed dilated and congested sinusoids (black arrow) and show single normal glomeruli with mild peri-glomerular lymphocytic infiltrate (red arrow) (Fig. 6G 1, 2). From Fig. 6H 1, 2, it was observed that the liver showed a normal central vein (red arrow) with mild dilation of sinusoids (black arrow) and kidney sections showed normal glomerulus and tubules (red arrow). Moreover, the combination treatment of extracts IIwith imipenem and CP was reported to produce show mildly congested central vein (black arrow) with mild dilation of sinusoids (red arrow) from the liver section and normal glomerulus (black arrow) and tubules from kidney tissue were observed (Fig. 6I1, 2, J1, 2). Furthermore, the liver tissue of the combination treatment of extract IIwith imipenem and CP showed normal portal triad (red arrow) with mild dilation of sinusoids and kidney tissue displayed normal glomerulus and tubules (red arrow).
Histopathological examination of liver and kidney tissues of experimental rats by H&E staining (magnification, X100). A DMSO B CLP C Per se (C) CLP D Ethanol extract; EE IE EE IIF Imipenem, G EE I + Imipenem H EE II + Imipenem I EE I + Imipenem + CP J EE II + Imipenem + CP. DMSO, dimethyl sulfoxide; CLP, cecal ligation and puncture; EE I (50 mg/kg ethanol extract; EE II (100 mg/kg ethanol extract); CP, cyclophosphamide. Figure 1 in each group represented liver tissue and Fig. 2 represented kidney tissue of each group
Discussion
The main objective of our study was to analyze the immunomodulatory activity in septic rats following treatment with CP leaf extract. Our results demonstrated the positive outcome by producing a modulatory effect of plant extract toward a compromised immune system due to sepsis. The immune system in sepsis is activated by the attack of bacteria, triggering macrophages, monocytes, T cells, polymorphonuclear leukocytes (PMNLs), free radical species, and nitric oxide production and coagulation pathway. This allows the release of proinflammatory cytokines namely, TNF, interleukins, products of arachidonic acid and complement (Herwald 2011). During the series of events activation of the coagulation system and platelets inhibit fibrinolysis and followed by endothelial dysfunction, microvascular damage and disrupted circulatory system (Bone 1992a; Fourrier et al. 1992). The production of these cytokines gives rise to systemic inflammatory response syndrome (SIRS) manifested as early sepsis followed by compensatory anti-inflammatory response syndrome (CARS) characterized by severe sepsis (hyperinflammatory) and death (Bone 1992b; Iba et al. 2021). In the case of severe sepsis, multi-organ dysfunction is evident, this may lead to septic shock causing cardiovascular collapse, failure to fluid therapy, and vasopressor agents (Faix 2013). The imbalance of SIRS and CARS response will produce mixed antagonist response syndrome (MARS). Increased pre-dominance of SIRS response causes higher chances of organ dysfunction and overproduction of pro-inflammatory cytokines. Contrary, to this, the predominance of CARS will overburden the release of anti-inflammatory cytokines leading to a high propensity to develop an immunocompromised state (Bone 1992a).
The clinical applications of antibiotics and supportive care are the sole therapy for treating sepsis. However, the use of these therapies is limited due to associated adverse effects (Zilahi et al. 2016). The idea of implementing immunotherapy for managing sepsis and related complications in healthcare settings has emerged as a promising approach. A previous study revealed that the treatment of sepsis with antibiotics and G-CSF and antimicrobial peptide LL-37 increased survival rates in a mouse model (Cirioni et al. 2008). In contrast to this, the use of IgG antibody obtained from plasma of E. coli immunized volunteers, exhibited no significant difference in mortality between patients who received IgG antibody and standard IgG preparations (Calandra et al. 1988). The administration of anti-TNF-α monoclonal antibodies may be potentially beneficial against gram-negative and gram-positive bacteria in sepsis. Though, associated factors like the short half-life of TNF- α in humans rendering too early or much-delayed administration of anti-TNF-α monoclonal antibodies, insufficiency of high TNF- α levels to produce shock and capability of anti-TNF-α antibodies to treat all underlying causes of sepsis pour unfavorable responses to drug use. Furthermore, immunostimulatory agents like interferon (INF)-γ and anti-inflammatory drugs such as interleukin (IL)-1 receptor antagonists have not displayed effective responses after clinical use (Zeni et al. 1997). On the other hand, another immunomodulatory component namely, IL-1Ra reportedly improves survival rates, reduced mean arterial pressure and cardiac output alleviating inflammation and incidences of organ failure (Bone 1991). Antimicrobial agents have also been in practice to treat sepsis. For instance, the use of imipenem along with CP demonstrated an increase in survival rates of septic rats (Guo et al. 2018). Supportively, a finding from another study demonstrated diminished cytokine levels, improved intestinal barrier function and restricted epithelial cell apoptosis along with enhanced survival rates by the concomitant administration of imipenem, normal saline and CP as immunosuppressant drugs (Yang et al. 2018). Therefore, the use of immunomodulating agents to treat sepsis remains unclear due to the associated numerous limitations and this would do more harm than good.
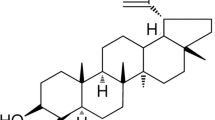
Looking upon the complexity of sepsis and the availability of limited therapies available, we hypothesized that immunosuppression of host cells affected by the microbial insult during sepsis by the implication of herbal drugs might be able to overcome the challenges associated with previously available anti-infective therapies and immunomodulators. Drugs of herbal origin efficiently reduce the production of free radical species thereby inhibiting oxidative stress, moderating the process of inflammation followed by immunosuppression, and elevating platelets and other hematological parameters (Scartezzini and Speroni 2000; Patil et al. 2012; Ansari et al. 2021; Usmani et al. 2021). C. papaya is a herbaceous rapid-growing plant, anciently been used for the treatment of several diseases like malaria, dengue, jaundice, viral and bacterial infections, and immune-compromised conditions. The leaves are an essential part of the plant enriched with flavonoids, saponins, glycosides, phenolic compounds, and alkaloids responsible for possessing high medicinal value like hepatoprotective, wound healing, antibacterial, anticancer, antithrombocytopenic, hypoglycemic, antiulcer properties (Rahmani and Aldebasi 2016; Ajiboye and Olawoyin 2020). Accordingly, a study performed on mice showed the analgesic activity of hexane, methanol ethanol and ethyl acetate extracts of papaya leaves (Hasimun et al. 2014). Another study was conducted to study the antibacterial activity of aqueous, and chloroform extract of leaves and aqueous, and methanol extract of seeds. The results revealed that aqueous and methanol extracts of seeds inhibited the bacterial pathogens, whereas the chloroform extract of the leaves failed to inhibit the bacteria invasion and the aqueous leaf extract potentially inhibit them (Peter et al 2014).
From a previous study, it was found that CP, an immunosuppressant, in combination with imipenem improves survival rates in septic animals (Brown et al. 2015). Similar findings from our model of sepsis revealed that CP together with imipenem and ethanol extract enhances survival in septic rats 7 days post-surgery. It is also evident that ethanol extract alone is not sufficient enough to protect immune cells from mortality due to severe sepsis. However, combinational therapy showed revamped survival rates. It can be concluded that the presence of phytoconstituents in the extract help in moderating mortality in septic animals through immune-modulating potentials. A key to identifying the difference in our study is the inclusion of herbal ingredients with the additional benefit of causing minimum side effects (Lin et al. 2020).
Findings from pre-clinical and clinical studies suggested that high IL-6 levels mark increased mortality (Remick et al. 2002; Coopersmith et al. 2003). Contrary to this, another report stated that the targeted antibody therapy, which decreases IL-6 levels greater than five-fold, failed to improve survival or change elevated IL-6 levels in mice (Vyas et al. 2005). We observed from our study that rats treated with imipenem displayed a decrease in TNF-α, IL-6, and IL-10 levels as compared to the CLP group but when compared to C. papaya extract-treated animals the levels of cytokines were slightly higher. This suggested that the administration of ethanol extract of C. papaya leaves in septic rats significantly decreases CLP-induced surge of pro-inflammatory and anti-inflammatory cytokines (TNF-α, IL-6, IL-10). Moreover, the ethanol extract together with imipenem and CP exhibited a strong synergistic effect rendering its potentiality for sepsis treatment.
We also analyzed the biochemical parameters in our study to further explore the effect of the extract on liver, kidney and antioxidant markers. Reports from previous studies stated that during severe injury to the immune cells in sepsis, marked dysregulated levels of kidney and liver parameters are observed which ultimately disturb the pathological mechanism of the host body (Wang et al. 2014). The excess free radicals production and unbalanced natural scavenging pathways may lead to microvascular dysfunction followed by organ dysfunction during sepsis (Coskun et al. 2011). It was observed from previous studies that the maintenance of protein and lipid integrity is regulated by GSH and provides protection against oxidative stress (Ross 1988). In contrast to increased MDA levels, GSH level is increased in kidney tissues and decreased in lung, liver and heart tissues while MDA levels are increased. The attenuation of liver GSH triggered endotoxins induced oxidative stress in rats causing enhanced plasma lipid peroxide (LPO) levels (Carbonell et al. 2000; Ansari et al. 2016). A study by Ritter et al. (2003), clarified that plasma SOD levels remain a potent antioxidant marker of early mortality in septic rats. This may correspond to our present study explaining the reduced SOD activity by CLP operation in rats. The elevated levels of Creatine Kinase, LDH and MDA were attenuated by ethanol extract treatment CLP-induced low GSH and SOD levels were significantly enhanced by CPL extract treatment. We also observed that CLP-induced increased expression of kidney parameters like SC and BUN levels were reduced by the administration of ethanol extract of CPL in septic rats, however, more reduced levels were observed by the combination therapy of extract and imipenem and CP. The reduced level of albumin after CLP surgery was significantly elevated by the concomitant use of extract combination with imipenem and CP. Liver enzymes like ALT and AST were significantly increased in the sepsis group (Wang et al. 2014). Our study supports this data by exhibiting attenuation of ALT and ALP levels reduced by combination therapy of extract with imipenem and CP in septic rats. Therefore, the hepatic and renal protective effects of CPL extract were evident by reducing inflammatory cytokines levels and regulating antioxidant enzymes. Our findings complement the previous studies performed on septic models to elucidate the effect of drugs on the liver and kidney (Coskun et al. 2011; Arulkumaran et al. 2018; Lee and Bae 2019).
In this study, we also analyzed the hemostatic alterations that occur during sepsis in response to the overproduction of cytokines like IL-6, IL-10 and TNF-α. The released cytokines are responsible for causing a dysregulated mechanism of procoagulant and anticoagulant arms leading to hemostatic imbalance. This ends up with the occurrence of endothelial injury and thrombosis associated with multiple organ dysfunction and death (Satran and Almog 2003). Previous studies by Esmon (2005), and Lupu et al. (2020) demonstrated the secretion of inflammatory mediators elevate platelet production. Activation of platelets leads to inflammation of vessels and further contributes to sepsis. It is stated in a clinical report that low levels of hemoglobin are associated with the condition of septic shock (Jung et al. 2019). Thrombocytopenia was observed in patients with sepsis and severe sepsis (Guclu et al. 2013). A previous study indicated that there is a significant relationship between ESR with inflammation (Ita et al. 2016; Ahn et al. 2018). The findings from our study are in line with the previously published studies that reported the alteration of CBC, prothrombin time, fibrinogen and ESR levels due to sepsis (Aird 2003; Barati et al. 2008; Hassaan et al. 2015; Pereira et al. 2017; Sinha et al. 2021). We concluded from our results that the ingestion of a mixture of ethanol extract with imipenem and CP has the potential to ameliorate CLP-induced hematological alterations and progression of sepsis severity.
Hepatotoxicity and nephrotoxicity were further confirmed by histopathological examinations. Our findings showed prominent signs of the development of infection in animals that underwent CLP marked by the widening of the portal triad and dilatation of sinusoids, mild lymphocytic infiltration, elongation, and congestion of portal veins with fibrosis in liver tissues. The kidney section showed destruction of glomeruli in different stages with replacement by proteinaceous/necrotic material. The cocktail therapy of ethanol extract with imipenem and CP, indeed, improved the severity of sepsis by displaying a mild periportal inflammation with mild dilation of sinusoids from the liver section and normal glomeruli and tubules from kidney tissue. In contrast to the results from a study by Guo et al. (2018), the effect of ethanol extract and combination therapy on the GI tract may also reveal important aspects in addition to the effect on the kidney and lungs. This supports the fact that C. papaya leaves extract potentially ameliorates the septic infection in conjunction with minimum adverse effects. However, our study has some limitations. To begin with, microbial culture was not carried out which could provide an insight into the presence of different types of bacteria in sepsis. Additionally, the effect of CLP on other vital organs were not included in this study which could profoundly explicit an in-depth analysis of ethanol extract of CPL on septic animals. Considering the results of our study we concluded that future investigations should be carried out to evaluate the effect of ethanol extract from C. papaya leaves in a large clinical set-up for better management of sepsis.
Conclusion
The rat model of sepsis was successfully replicated in our study mimicking the sepsis and sepsis-related complications in humans. The administration of ethanol extract from C. papaya leaves in combination with imipenem and CP have significantly displayed infection-reducing potentials by modulating the immune response to injury, regulating biological and hematological pathways involved in sepsis occurrence. However, there are some limitations to our study, foremost, we could not express this effect further due to a lack of clinical approach. Also, in-depth immunohistochemistry estimations and gene expression analysis were not included which may complement with the available studies. Moreover, we did not examine organs like lungs and GI tract that are impacted in the early stage of sepsis and functional changes can be observed due to cyclophosphamide intake. Further studies on the isolated organ tissues would be revealing.
Our findings further promote the use of C. papaya leaves for future investigations in clinical settings with a view to twirling the availability of limited therapeutic options for sepsis treatment globally.
Data availability
Available upon request.
References
Ahn HK, Koo KC, Chung BH, Lee KS (2018) Comparison of the delta neutrophil index with procalcitonin, erythrocyte sedimentation rate, and C-reactive protein as predictors of sepsis in patients with acute prostatitis. Prostate Int 6:157–161. https://doi.org/10.1016/J.PRNIL.2018.05.001
Aird WC (2003) The hematologic system as a marker of organ dysfunction in sepsis. Mayo Clin Proc 78:869–881. https://doi.org/10.4065/78.7.869
Ajiboye AE, Olawoyin RA (2020) Antibacterial activities and phytochemical screening of crude extract of Carica papaya leaf against selected pathogens. Glob J Pure Appl Sci 26:165–170. https://doi.org/10.4314/gjpas.v26i2.8
Ansari MN, Bhandari U, Pillai KK (2016) Protective role of curcumin in myocardial oxidative damage induced by isoproterenol in rats. 26:933–938. https://doi.org/10.1177/0960327107085835
Ansari MN, Saeedan AS, Bajaj S, Singh L (2021) Evaluation of antidiabetic and hypolipidemic activity of Barleria cristata Linn. leaves in alloxan-induced diabetic rats. 3 Biotech 114:1–11. https://doi.org/10.1007/S13205-021-02728-5
Arulkumaran N, Sixma ML, Pollen S, et al (2018) P2X 7 receptor antagonism ameliorates renal dysfunction in a rat model of sepsis. Physiol Rep 6:e13622. https://doi.org/10.14814/PHY2.13622
Barati M, Alinejad F, Bahar MA et al (2008) Comparison of WBC, ESR, CRP and PCT serum levels in septic and non-septic burn cases. Burns 34:770–774. https://doi.org/10.1016/J.BURNS.2008.01.014
Bone RC (1991) A critical evaluation of new agents for the treatment of sepsis. JAMA J Am Med Assoc 266:1686–1691. https://doi.org/10.1001/JAMA.1991.03470120088038
Bone RC (1992) Modulators of coagulation: a critical appraisal of their role in sepsis. Arch Intern Med 152(7):3
Bone RC (1992) Modulators of coagulation: a critical appraisal of their role in sepsis. Arch Intern Med 152(7):1
Brown I, Bellevue O, Shawo A et al (2015) Low dose cyclophosphamide improves survival in a murine treatment model of sepsis. Shock 43:92. https://doi.org/10.1097/SHK.0000000000000263
Bryda O, Stadnytska N (2021) Extraction methods of extractive substances from medicinal plant raw materials: advantages and limitations. Ann Rom Soc Cell Biol 25:1737–1751
Calandra T, Glauser MP, Schellekens J, Verhoef J (1988) Treatment of gram-negative septic shock with human IgG antibody to Escherichia coli J5: a prospective, double-blind, randomized trial. J Infect Dis 158:312–319. https://doi.org/10.1093/INFDIS/158.2.312
Carbonell LF, Nadal JA, Llanos MC et al (2000) Depletion of liver glutathione potentiates the oxidative stress and decreases nitric oxide synthesis in a rat endotoxin shock model. Crit Care Med 28:2002–2006. https://doi.org/10.1097/00003246-200006000-00054
Christaki E, Anyfanti P, Opal SM (2011) Immunomodulatory therapy for sepsis: an update. Expert Rev Anti Infect Ther 9:1013–1033
Cirioni O, Ghiselli R, Tomasinsig L et al (2008) Efficacy of LL-37 and granulocyte colony-stimulating factor in a neutropenic murine sepsis due to Pseudomonas aeruginosa. Shock 30:443–448. https://doi.org/10.1097/SHK.0B013E31816D2269
Coopersmith CM, Amiot DM, Stromberg PE et al (2003) Antibiotics improve survival and alter the inflammatory profile in a murine model of sepsis from Pseudomonas aeruginosa pneumonia. Shock 19:408–414. https://doi.org/10.1097/01.SHK.0000054370.24363.EE
Coskun AK, Yigiter M, Oral A et al (2011) The effects of montelukast on antioxidant enzymes and proinflammatory cytokines on the heart, liver, lungs, and kidneys in a rat model of cecal ligation and puncture-induced sepsis. Sci World J 11:1341–1356. https://doi.org/10.1100/TSW.2011.122
D’Agostino P, La Rosa M, Barbera C et al (1998) Doxycycline reduces mortality to lethal endotoxemia by reducing nitric oxide synthesis via an interleukin-10-independent mechanism. J Infect Dis 177:489–492. https://doi.org/10.1086/517383
Dewitte A, Lepreux S, Villeneuve J et al (2017) Blood platelets and sepsis pathophysiology: a new therapeutic prospect in critical ill patients? Ann Intensive Care 71(7):1–18. https://doi.org/10.1186/S13613-017-0337-7
Esmon CT (2005) The interactions between inflammation and coagulation. Br J Haematol 131:417–430. https://doi.org/10.1111/J.1365-2141.2005.05753.X
Faix JD (2013) Biomarkers of sepsis. Crit Rev Clin Lab Sci 50:23–36. https://doi.org/10.3109/10408363.2013.764490
Fourrier F, Chopin C, Goudemand J et al (1992) Septic shock, multiple organ failure, and disseminated intravascular coagulation. Compared patterns of antithrombin III, protein C, and protein S deficiencies. Chest 101:816–823. https://doi.org/10.1378/CHEST.101.3.816
Gaieski DF, Edwards JM, Kallan MJ, Carr BG (2013) Benchmarking the incidence and mortality of severe sepsis in the united states. Crit Care Med 41:1167–1174. https://doi.org/10.1097/CCM.0B013E31827C09F8
Guclu E, Durmaz Y, Karabay O (2013) Effect of severe sepsis on platelet count and their indices. Afr Health Sci 13:333–338. https://doi.org/10.4314/AHS.V13I2.19
Guo P, Zhang SW, Zhang J et al (2018) Effects of imipenem combined with low-dose cyclophosphamide on the intestinal barrier in septic rats. Exp Ther Med 16:1919. https://doi.org/10.3892/ETM.2018.6373
Hasimun P, Suwendar EGI (2014) Analgetic activity of papaya (Carica papaya L.) leaves extract. Procedia Chem 13:147–149. https://doi.org/10.1016/J.PROCHE.2014.12.019
Hassaan PS, Mehanna RA, Dief AE (2015) The potential role of hemopexin and heme oxygenase-1 inducer in a model of sepsis. Physiol J 2015:1–10. https://doi.org/10.1155/2015/208485
Herwald HEA (2011) Sepsis-pro-inflammatory and anti-inflammatory responses. Contrib Microbiol. Basel; Karger: 1–11
Hotchkiss RS, Opal S (2010) Immunotherapy for sepsis–a new approach against an ancient foe. N Engl J Med 363:87–89. https://doi.org/10.1056/NEJMCIBR1004371
Huang M, Cai S, Su J (2019) The pathogenesis of sepsis and potential therapeutic targets. Int J Mol Sci 20:5376. https://doi.org/10.3390/IJMS20215376
Iba T, Umemura Y, Wada H, Levy JH (2021) Roles of coagulation abnormalities and microthrombosis in sepsis: pathophysiology, diagnosis, and treatment. Arch Med Res 52:788–797. https://doi.org/10.1016/J.ARCMED.2021.07.003
Ita SO, Akpanyung EO, Robert AS et al (2016) Evaluation of some inflammatory biomarkers in male albino wistar rats following ingestion of crude oil and the role of bee honey, vitamins C and E. Mod Res Inflamm 05:55–62. https://doi.org/10.4236/MRI.2016.53006
Jantan I, Ahmad W, Science SB-F in P, 2018 U (2018) Corrigendum: Plant-derived immunomodulators: An insight on their preclinical evaluation and clinical trials. frontiersin.org 9:1178:
Jung SM, Kim YJ, Ryoo SM, Kim WY (2019) Relationship between low hemoglobin levels and mortality in patients with septic shock. Acute Crit Care 34:141–147. https://doi.org/10.4266/ACC.2019.00465
Kalechman Y, Gafter U, Gal R et al (2002) Anti-IL-10 therapeutic strategy using the immunomodulator AS101 in protecting mice from sepsis-induced death: dependence on timing of immunomodulating intervention. J Immunol 169:384–392. https://doi.org/10.4049/JIMMUNOL.169.1.384
Lee IC, Bae JS (2019) Pelargonidin protects against renal injury in a mouse model of sepsis. J Med Food 22:57–61. https://doi.org/10.1089/JMF.2018.4230
Lee W, Lee Y, Jeong GS et al (2017) Cudratricusxanthone A attenuates renal injury in septic mice. Food Chem Toxicol 106:404–410. https://doi.org/10.1016/J.FCT.2017.06.009
Lin SR, Chang CH, Hsu CF et al (2020) Natural compounds as potential adjuvants to cancer therapy: preclinical evidence. Br J Pharmacol 177:1409–1423. https://doi.org/10.1111/BPH.14816
Lupu F, Kinasewitz G, Dormer K (2020) The role of endothelial shear stress on haemodynamics, inflammation, coagulation and glycocalyx during sepsis. J Cell Mol Med 24:12258–12271. https://doi.org/10.1111/JCMM.15895
Mannaa FA, Abdel-Wahhab KG, Abdel-Wahhab MA (2014) Prevention of cardiotoxicity of aflatoxin B1 via dietary supplementation of papaya fruit extracts in rats. Cytotechnology 66:327–334. https://doi.org/10.1007/S10616-013-9579-X/TABLES/2
Mukherjee PK, Nema NK, Bhadra S et al (2014) Immunomodulatory leads from medicinal plants. Indian J Tradit Knowl 13:235–256
Nnaemeka UM, Ugwu, Ukamaka IA, et al (2023) Comparative study of aqueous, methanol and petroleum ether extracts of unripe Carica papaya seed on liver and kidney function in streptozotocin-induced diabetic rats. GSC Biol Pharm Sci 22:038–047. https://doi.org/10.30574/gscbps.2023.22.1.0488
Patel A, Joseph J, Periasamy H, Mokale S (2018) Azithromycin in combination with ceftriaxone reduces systemic inflammation and provides survival benefit in a murine model of polymicrobial sepsis. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.00752-18
Patil US, Jaydeokar AV, Bandawane DD (2012) Immunomodulators: a pharmacological review. Int J Pharm Pharm Sci 4:30–36
Pereira RS, Bertoncheli CM, Adefegha SA et al (2017) Sepsis induced by cecal ligation and perforation (CLP) alters nucleotidase activities in platelets of rats. Microb Pathog 111:345–351. https://doi.org/10.1016/J.MICPATH.2017.08.047
Peter JK, Kumar Y, Pandey P et al. (2014) Antibacterial activity of seed and leaf extract of Carica Papaya var. Pusa dwarf Linn. Sci J pharm Biol 9(2):29–37
Petronilho F, Florentino D, Danielski LG et al (2016) Alpha-lipoic acid attenuates oxidative damage in organs after sepsis. Inflammation 39:357–365. https://doi.org/10.1007/S10753-015-0256-4
Rahmani AH, Aldebasi YH (2016) Potential role of carica papaya and their active constituents in the prevention and treatment of diseases Implication of PTEN, akt and bcl2 expressions and its co-relation with apoptotic pathways in oral squamous cell carcinoma View project Natural product. Int J Pharm Pharm Sci 8:11–15
Remick DG, Bolgos GR, Siddiqui J et al (2002) Six at six: interleukin-6 measured 6 h after the initiation of sepsis predicts mortality over 3 days. Shock 17:463–467. https://doi.org/10.1097/00024382-200206000-00004
Resim S, Kurutas EB, Gul AB et al (2015) The levels of oxidative stress biomarkers in rats as a response to different techniques of testicular biopsy. Indian J Surg 77:310–313. https://doi.org/10.1007/S12262-013-0808-5
Rhodes A, Evans LE, Alhazzani W et al (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 433(43):304–377. https://doi.org/10.1007/S00134-017-4683-6
Ritter C, Andrades M, Frota MLC et al (2003) Oxidative parameters and mortality in sepsis induced by cecal ligation and perforation. Intensive Care Med 29:1782–1789. https://doi.org/10.1007/S00134-003-1789-9
Ross D (1988) Glutathione, free radicals and chemotherapeutic agents. Mechanisms of free-radical induced toxicity and glutathione-dependent protection. Pharmacol Ther 37:231–249. https://doi.org/10.1016/0163-7258(88)90027-7
Sapin F, Biston P, Piagnerelli M (2017) Predictive value of C-reactive protein in critically ill patients after abdominal surgery. Clinics
Satran R, Almog Y (2003) The coagulopathy of sepsis: pathophysiology and management. Isr Med Assoc J 5:516–520
Scartezzini P, Speroni E (2000) Review on some plants of Indian traditional medicine with antioxidant activity. J Ethnopharmacol 71:23–43. https://doi.org/10.1016/S0378-8741(00)00213-0
Shapira L, Aubrey Soskolne W, Houri Y et al (1996) Protection against endotoxic shock and lipopolysaccharide-induced local inflammation by tetracycline: correlation with inhibition of cytokine secretion. Infect Immun 64:825–828. https://doi.org/10.1128/iai.64.3.825-828.1996
Sinha H, Maitra S, Anand RK et al (2021) Epidemiology and prognostic utility of cellular components of hematological system in sepsis. Indian J Crit Care Med 25:660. https://doi.org/10.5005/JP-JOURNALS-10071-23874
Somayaji YT, Vidya V, Rao S et al (2016) Modulatory effects of Carica papaya ( Linn.) on electron beam radiation induced hematological suppression and biochemical alterations in swiss albino mice. J Biochem Technol 7:1044–1050
Upadhyay G, Tiwari N, Maurya H, et al (2021) In vivo wound-healing and antioxidant activity of aqueous extract of Roylea elegans leaves against physically induced burn model in Wistar albino rats. 3 Biotech 1110(11):1–10. https://doi.org/10.1007/S13205-021-02993-4
Usmani J, Khan T, Ahmad R, Sharma M (2021) Potential role of herbal medicines as a novel approach in sepsis treatment. Biomed Pharmacother 144:112337
Vyas D, Javadi P, Di Pasco PJ, et al (2005) Early antibiotic administration but not antibody therapy directed against IL-6 improves survival in septic mice predicted to die on basis of high IL-6 levels. Am J Physiol Regul Integr Comp Physiol. https://doi.org/10.1152/AJPREGU.00312.2005
Wang D, Yin Y, Yao Y (2014) Advances in sepsis-associated liver dysfunction. Burn Trauma 2:97–105. https://doi.org/10.4103/2321-3868.132689
Watanabe E, Thampy LK, Hotchkiss RS (2018) Immunoadjuvant therapy in sepsis: novel strategies for immunosuppressive sepsis coming down the pike. Acute Med Surg 5:309–315. https://doi.org/10.1002/AMS2.363
Weighardt H, Heidecke CD, Emmanuilidis K et al (2000) Sepsis after major visceral surgery is associated with sustained and interferon-gamma-resistant defects of monocyte cytokine production. Surgery 127:309–315. https://doi.org/10.1067/MSY.2000.104118
Yang J, Zhang S, Wu J et al (2018) Imipenem and normal saline with cyclophosphamide have positive effects on the intestinal barrier in rats with sepsis. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 162:90–98. https://doi.org/10.5507/BP.2018.032
Zeni F, Freeman B, Natanson C (1997) Anti-inflammatory therapies to treat sepsis and septic shock: a reassessment. Crit Care Med 25:1095–1100. https://doi.org/10.1097/00003246-199707000-00001
Zilahi G, McMahon MA, Povoa P, Martin-Loeches I (2016) Duration of antibiotic therapy in the intensive care unit. J Thorac Dis 8:3774. https://doi.org/10.21037/JTD.2016.12.89
Funding
This research received no funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, JU, RA; Data curation, JU; Formal analysis, JU, MW, RA; Investigation, JU, MW, MH, RA; Methodology, JU, RA; Project administration, JU, RA; Resources, JU, MNA, MH, MJ, RA; Supervision, MNA, MH, MJ, RA; Validation, RA; Visualization, JU, RA; Writing—original draft, JU, MW, MNA, MJ, RA; Writing—review and editing, JU, MW, MNA, MH, MJ, RA.
Corresponding author
Ethics declarations
Conflict of interest
The authors of the present study declare no conflict of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Usmani, J., Wasim, M., Ansari, M.N. et al. Potential therapeutic effect of Carica papaya leaves extract on immune response, biochemical and hematological mechanisms on cecal ligation and puncture model of sepsis in rats: an in vivo study. 3 Biotech 13, 151 (2023). https://doi.org/10.1007/s13205-023-03567-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13205-023-03567-2