Abstract
Macrocybe crassa (or Tricholoma crassum) is a nutrient-dense wild edible mushroom native to Thailand. The mushroom extract and its constituents have remarkable biological characteristics, but the influence of the powder on the human gut microbiota is unknown. This study investigated the bioactive composition and modulatory properties of M. crassa powder on gut microbial composition and short-chain fatty acids (SCFA) production. The fermentation of M. crassa powder by human intestinal microbiota released SCFA, mainly acetic acid, propionic acid and butyric acid. M. crassa powder significantly modulated the microbiota by increasing the relative abundances of Bifidobacterium, Lactobacillus/Enterococcus group, Atopobium, Bacteroidaceae/Prevotellaceae, and C. coccoides. F. prausnitzii, Roseburia genus, C. histolyticum and C. cluster IX, similar to that of Fructooligosaccharides (FOS). With M. crassa powder, high content of propionic acid was observed, as well as a number of Bacteroidaceae/Prevotellaceae and C. cluster IX. On the other hand, FOS caused a high acetic acid concentration and a population of Bifidobacterium spp., Atopobium cluster, Bacteroidaceae/Prevotellaceae, and C. coccoides. Therefore, this work will significantly contribute to filling the knowledge gap and revealing the significance of M. crassa in the pharmaceutical industry.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Edible mushrooms consumed for centuries as food and medicine. Recent studies have shown that mushrooms and their extracts have both therapeutic and prebiotic properties (Mahdavi et al. 2021; Ruthes et al. 2021). Indigestible polysaccharides such as pleuran, lentinan, schizophyllan, and β-glucans are major components of mushrooms that play a prebiotic role (Liu et al. 2020; Singdevsachan et al. 2016). Additionally, the gut microbiota may be impacted by other food components like proteins (Madsen et al. 2017), or phenolic and phenolic fibre-rich fractions (Loo et al. 2020), but less is known about the prebiotic properties of entire mushroom powder derived from the fruiting bodies. It is now clear that there are significant differences in bioactivities between mixed and purified compounds. The synergistic effect of a mixture of active constituents in mixed forms such as in a mushroom powder can provide an alternative to the concept of one drug > one target > one disease (Liu et al. 2018). Several studies have demonstrated a similar concept for the development of natural prebiotics from crude polysaccharides found in mushrooms (Hussain et al. 2022). White button (WB) mushrooms (Agaricus bisporus) had a prebiotic effect on both the bacteria metabolism and the host. WB feeding caused changes in the microbiota, including an increase in Bacteroidetes phyla members, particularly Prevotella bacteria, which are known to produce propionic and succinic acid (Tian et al. 2018). Also, P. ostreatus mushroom-powder treatments improved gut microbiota and short-chain fatty acids (SCFA) production (Koutrotsios et al. 2019). According to Ayimbila et al. most of the Lentinus squarrosulus powder evaded digestion under simulated gastric and intestinal conditions, and the resistant hydrolysate decreased the Firmicutes/Bacteroidetes ratio and increased the number of essential immunomodulation bacteria (Ayimbila et al. 2022). Owing to these mushrooms are considered next-generation healthy food components.
Macrocybe crassa or Tricholoma crassum is a wild, edible mushroom native to south and southeast Asia. It has a large fruit body with a fleshy texture and a delicious taste, for which it is highly regarded. It is consumed in significant amounts, for example, consumption in West Bengal was estimated at approximately 3.9 tons annually (Ghosh and Acharya 2022). M. crassa is known in Thailand by a variety of names, including Hed-Tean-Rad (northeast), Hed-Jan (north), Hed-Hua-Sum (south), and Hed Yai or Hed-Tub-Tao-Khao (central) (Inyod et al. 2017; Verma et al. 2017). Similar to other mushrooms, M. crassa has a high nutritional value (Inyod et al. 2016; Payapanon and Srijumpa 2008), and has attracted attention for its pharmacological properties. Methanolic extracts indicated a potential for biomolecule isolation interesting in the treatment of breast cancer (Koutrotsios et al. 2019), and its fruiting bodies contain biological agents such as selenium (Se), which can prevent and reduce the risk of cancer, especially prostate cancer (Saranya et al. 2022). Mushrooms are well-known for their low-fat content, high-quality proteins, dietary fibre, and the presence of nutraceuticals, which are essential for improving host health and well-being. Edible mushrooms are increasingly being used as functional food ingredients to harness nutritional, bioactive, and medicinal properties (Das et al. 2021). However, data on the potential use of M. crassa for prebiotic applications are limited. Prebiotics are microbiota-shaping compounds that act as a carbon source for the growth of beneficial taxa, delivering a specific or selective change that confers host health related to metabolism (Swanson et al. 2020). The International Scientific Association of Probiotics and Prebiotics (ISAPP) defines prebiotics as “a substrate that is selectively utilized by host bacteria imparting a health advantage” (Gibson et al. 2017).
Fructooligosaccharides (FOS), inulin, lactulose and galactooligosaccharides are universally agreed-upon prebiotics (Carlson et al. 2018), which show high fermentability by colonic microbiota related to health benefits. The colonic fermentation of mushroom components thereof, can synergistically stimulate the growth of health-promoting microorganisms and decrease the abundance of opportunistic pathogens, and directly or indirectly improve immune responses through the modulation of the gut microbiota and releasing of short-chain fatty acids (SCFA) (Ma et al. 2017; Ruthes et al. 2021). Lactic acid and SCFA can supply energy to the colonic epithelium, affect cholesterol and lipid metabolism, decrease pathogenic intestinal bacteria, and modulate the immune system (Gibson et al. 2010). The effect of L. squarrosulus powder hydrolysate on the development of beneficial bacteria and the formation of SCFA and branched-chain fatty acids (BCFA) may be due to carbohydrate and protein fraction fermentation (Ayimbila et al. 2022). Certain types of dietary fibre, particularly indigestible oligosaccharides, have been studied for their ability to stimulate the growth and/or activity of beneficial gut bacteria such as bifidobacteria and lactobacilli while inhibiting the development of Clostridium histolyticum, resulting in a concomitant positive effect on colonic health (Gibson et al. 2010; Kang et al. 2022). This has sparked a keen interest in the discovery of new mushrooms with potential prebiotic properties. Most of the research on mushrooms and their prebiotic properties has involved mushroom extracts rather than whole mushrooms in food form (You et al. 2022). For this reason, an understanding of the prebiotic benefits of mushrooms as a whole, natural food is still needed. The whole mushroom powder consists of polysaccharides, proteins and phenols that may offer a synergistic effect in the gut. Because the large intestine is where most gut fermentations occur (Das et al. 2021), it can be targeted to fully reveal the prebiotic properties via synergistic effects of mushroom components. As a result, mushroom powder can be utilized as a functional ingredient in the form of a capsule or tablet or add to stir-fries, soups or shake it up in smoothies. Therefore, this work focused on potential prebiotic effects of M. crassa powder as indicated by SCFA production and modulation of the gut microbial composition. To the best of our knowledge, no research has been conducted on the influence of M. crassa powder on gut microbial ecology to validate and solidify the biological potential of this mushroom for use as a functional food and bioactive component source.
Materials and methods
Materials
Two different types of carbohydrate materials (mushroom powder and Fructooligosaccharides; FOS) and negative control were used as substrates in batch cultures. M. crassa was cultivated on spent mushroom compost, fine rice bran and fine seed corn at a ratio of 80:15:5, yielding 237 g of fresh fruit bodies per 600 g substrate. The mushroom powder was prepared from dried fruit bodies of M. crassa by grinding, blending and sieving to collect particles of < 0.5 mm. The fructooligosaccharide (FOS, Orafti® P95, Beneo, Tienen, Belgium) was used as a prebiotic reference. Sigma Laboratories Gillingham, Dorset, United Kingdom) supplied all of the reagents and chemicals used in this study.
Nutritional analysis
The nutritional components of mushroom powder were analysed at the Thailand Institute of Scientific and Technological Research (TISTR). The carbohydrate, protein, fat, crude fibre, and ash contents were determined using standard methods (AOAC 1995; Manzi et al. 2001). Minerals were analysed using atomic absorption spectrophotometry (Willard et al. 1988), and total phosphorus was analysed using the phosphorus-vanadomolybdate method (Munson and Nelson 1990). The Mushroom and Yeast Glucan Assay Kit (K-YBGL 09/2009; Megazyme International Ireland Ltd.; Bray, County Wicklow, Ireland) was used to determine the glucan content in mushroom powder. The total phenolic content was determined using the Folin–Ciocalteu method (Li et al. 2020) and the data obtained were expressed as mg/g of gallic acid equivalents (GAE) in milligrams per gram (mg GAE/g) of dry sample.
Faecal inocula
Fresh human faecal samples were collected from four healthy human volunteers (average age 30–45 years; three females, one male) who had not taken any prebiotics or antibiotics in the three months leading up to the study. The samples were homogenized in a stomacher (model 6041; Seward Scientific, UK) for 2 min at normal speed after being diluted 1:10 (w/w) in anaerobic 0.1 M phosphate buffered saline (pH 7.0).
In vitro fermentations
The batch-culture fermentation systems were set up in sterile vessels. Each vessel contained 45 mL of sterile basal medium (peptone water 2 g/L (Oxoid), yeast extract 2 g/L (Oxoid), NaCl 0·1 g/L, K2HPO4 0·04 g/L, KH2PO4 0·04 g/L, MgSO4.7H2O 0·01 g/L, CaCl2.6H2O 0·01 g/L, NaHCO3 2 g/L, Tween-80 2 mL (BDH), haemin 0·05 g/L, vitamin K1 10 mL, cysteine. HCl 0·5 g/L, bile salts 0·5 g/L, pH 7·0), and was pre-reduced overnight with oxygen-free nitrogen (15 mL/min). The pH was maintained between 6.7 and 6.9 using a pH controller, and the temperature was kept at 37 °C (Fermac 260; Electrolab, Tewkesbury, UK). The final sample concentration in the vessel supplemented with mushroom powder and FOS (positive control) was 1% (w/v) in a 50 mL working volume (0.5 g). A vessel containing basal medium was used as a negative control group. Each batch culture was inoculated with 5 mL of fresh faecal slurry to give a final concentration of 10% (w/w). The batch reactors were maintained at 37 °C, and 5-mL samples were taken after 0, 10, 24 and 34 h to enumerate bacteria by fluorescent in situ hybridization and analyse short-chain fatty acids. Independent duplicates of these fermentations were performed for different donors.
Bacterial enumeration
Fluorescent in situ hybridization with 16S Ribosomal RNA (rRNA) probes were used to assess human faecal bacterial populations. These probes were synthesized commercially and labelled with the fluorescent dye Cy3 for identification (supplied by Eurogentec Ltd., UK). The selected 16S rRNA probes were specific for the Bifidobacteria group, Lactobacilli/Enterococci group, Atopobium cluster, Bacteroides/Prevotella group, Clostridium histolyticum group and Eubacterium rectale group. The probes used were Bif164, Lab158, Ato291, Bac303, Chis150, Prop853, Erec482, Rrec584 and Fra655 (Table 1). Total bacterial counts were performed using the nucleic acid stain 4′,6-diamidino-2-phenylindole (DAPI). Fermentation samples (375 µL) were fixed for 4 h (4 °C) in 1125 µL of filtered 4% (w/v) paraformaldehyde at each sampling time. Fixed cells were centrifuged at 13,000g for 5 min and washed twice in 1 mL of filter-sterilized PBS. Washed cells were suspended in 150 µL filtered PBS and 150 µL ethanol (99%) and stored at 20 °C for at least 1 h before further analysis. Samples (10 µL) were diluted in PBS and 20 µL of the solution was added to each well of a six-well polytetrafluoroethylene/poly-l-lysine-coated slide (Tekdon Inc., Myakka City, FL). The samples were dried for 15 min in a drying chamber (50 °C) and then were dehydrated using alcohol solutions of 50%, 80%, and 96% ethanol, respectively, for 3 min in each solution. Slides were dried in a drying chamber for 2 min to evaporate ethanol. A hybridization mixture of 50 µL (consisting of 5 µL probe and 45 µL hybridization buffer) was added to each well. Hybridization was carried out at the appropriate temperatures for each probe for 4 h in a hybridization incubator (Grant-Boekel, Cambridge, UK). After hybridization, slides were washed in 50 mL of washing buffer (9 mL of 5 M NaCl, 1 mL of 1 M Tris/HCl (pH 8.0) and 40 mL of deionized water) containing 20 µL DAPI solution (50 mg/mL) for 15 min, then were dipped in cold water for a few seconds and dried with compressed air. Five microliters of ‘antifade’ (Sigma–Aldrich, New Jersey, USA or Geel, Belgium) were added to each well, and a coverslip (20 mm; thickness no. 1; VWR, Lutterworth, United Kingdom) was placed on each slide. Slides were examined using fluorescence microscopy (Eclipse 400; Nikon, Surrey, UK). At least fifteen random fields were counted on each well.
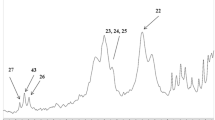
Short-chain fatty acid analyses
One-milliliter samples were obtained from the batch culture fermentation and centrifuged at 13,000g for 5 min. The supernatant was filtered by a 0.22 µm filter unit (Millipore) and 20 µL was injected into a High-Performance Liquid Chromatography (HPLC) system (Model LaChrom by Merck Hitachi, Poole, Dorset, UK) equipped with a pump (L-7100), a refractive index detector (L-7490), and auto-sampling (L-7200). The column used was the ion-exclusion Rezex ROA-Organic Acid H (8%) column (300 × 7.80 mm; Phenomenex, Cheshire, UK). Guard columns were Security Guard Carbo-H + , 4 × 3.0-mm cartridges (Phenomenex). The mobile phase used was 2.5 mM sulfuric acid in HPLC-grade water. The samples were quantified using calibration curves of lactic acid, formic acid, acetic acid, propionic acid, and butyric acid at concentrations of 12.5, 25, 50, 75, and 100 mM, and the results were expressed in mmol/L.
Statistical analysis
The differences between bacterial numbers and SCFA production at 0, 10, 24 and 34 h of fermentation for each batch culture were checked for significance by the paired t-test. The differences were considered significant when P < 0.05 and calculations were done with SPSS for Windows (version 21.0; SPSS, Inc.). One-way ANOVA and post hoc Tukey’s tests were used to determine significant differences in substrates used on bacterial group population and SCFA. All bacterial population and metabolite data (Log10 cell/mL) are expressed as the average of four replications (donors) plus or minus standard deviation.
Results and discussion
Nutritional composition
According to Table 2, M. crassa mushroom powder contained protein (14.3%), carbohydrates (65.3%), fat (4.89%), ash (11.2%), crude fibre (1.67%), beta (β-) glucans (37.6%) and moisture (13.6%). The macronutrient composition in mg per kg dry weight is phosphorus (8600), potassium (35,300), calcium (433) and sodium (930), and the following micronutrients were analysed (mg/kg dry wt.): Fe (420), Zn (85.0), Cu (ND) and Mn (1.09). In addition, the mushroom powder contained phenolic compounds (4.76 ± 0.05 mg GAE/g) and its caloric value was 352 kcal/kg. The nutritional composition of M. crassa was thus comparable to other medicinal mushrooms. Dried L. edodes contains carbohydrates (58–60%), proteins (20–23%), fibre (9–10%), lipids (3–4%), β-glucans and phenolics (4.32 mg GAE/g) (in pileus; 20–40% and stipe; 33–58%) (Carrasco-González et al. 2017; Nie et al. 2020). Pleurotus spp. contain carbohydrates (9.4–75.4%), proteins (10–38.5%), fibre (10.2–20.7%), lipids (0.9–3.5%), β-glucans (25.9–50%) and phenolics (9.02–17.17 mg GAE/150 g) (Raman et al. 2021), and Ganoderma fruit bodies are composed of protein, carbohydrate, fat, ash and phenolic compounds ranging between 15.7 and 24.5 g/100 g dw, 73.31 and 81.90 g/100 g, 0.48 and 1.40 g/100 g and 7.6 and 489 µg/100 g, respectively (Obodai et al. 2017). The fat/lipids content of M. crassa appears to be higher than for these mushrooms, but it does not exceed the 6% limit specified by the Food and Drug Administration (FDA) for low-fat foods (FDA 2013). Polysaccharides (β-glucans), proteins, lipids, and phenolic compounds make up the majority of myco-chemicals, the bioactive compounds found in mushrooms (Cateni et al. 2021), and M. crassa revealed excellent amounts of these compounds. Polysaccharides, especially β-glucans, as well as proteins and phenolics have all been linked to prebiotic and positive health effects, including anti-cholesterol, anti-cancer, antioxidant, and immunomodulator properties, among others (Ayimbila and Keawsompong 2021; Kumar Singh et al. 2019). The findings revealed that M. crassa powder is a high-nutrient food with the potential to stimulate gut microbiota.
In vitro colonic fermentation
During long-term competition and evolution, microbes of the gut became interdependent with the hosts and play an essential role in health, nutrition, disease, metabolism and immune homeostasis (Chen et al. 2018). Consuming different dietary fibres can selectively alter the composition and/or activity of the intestinal bacterial flora, which can have biological significance (Cantu-Jungles et al. 2018). While it is known that mushrooms contain a variety of biologically active compounds that can synergistically affect microbiome composition, most studies have focused on the impact of isolated carbohydrate fractions rather than the entire composition. For this reason, the ability of the entire fruiting body of M. crassa to stimulate human gut microbiota composition was assessed and compared to a negative control as well as to FOS, a known prebiotic. It is important to note that before the performance of in vitro fermentations mushroom powder was submitted to simulated gastrointestinal digestion because it can be made to consume in a capsule or tablet form which can escape hydrolysis by gastric acidity and mammalian enzymes to enable the substrate to reach the colon and be fermented by intestinal microbiota, meeting the requirements for a gut modulation effect. Prebiotics are defined by the International Scientific Association of Probiotics and Prebiotics (ISAPP) as “a substrate that is selectively utilized by host bacteria to confer a health benefit” (Gibson et al. 2017). The few studies that have evaluated the prebiotic potential of mushroom powder using in vitro fermentation have gone through gastrointestinal digestion, making it difficult to determine the true effectiveness of whole compounds and multiple different bioactive components (Ayimbila et al. 2022; Rodrigues et al. 2016) to make the whole mushroom beneficial. During the experimental time course (0, 10, 24, and 34 h), in vitro fermentation of M. crassa powder at 1% (w/v) modified bacterial populations (Table 3) and accumulated lactic acid and SCFA (acetic, propionic, butyric acids) (Table 4) in comparison to well-established prebiotic FOS (positive control) and medium without carbon source (negative control). The non-digestible extracts of five M. crassa strains were reported in a recent study to resist digestion in the stomach and intestine, suppress pathogenic bacteria, and stimulate the growth of lactic acid bacteria (Inyod et al. 2022).
As depicted in Table 3, Bifidobacterium populations in response to all substrates significantly increased at 10 h compared to 0 h (P < 0.01). FOS (8.85 ± 0.03) had the greatest effect on Bifidobacterium populations after 24 h, followed by M. crassa powder (8.79 ± 0.04); however, the impact of these two substrates on Bifidobacterium populations is statistically comparable, confirming a similar stimulatory effect. In addition to this, after 10 h of fermentation, the Lactobacillus/Enterococcus group concentrations were comparable between FOS and M. crassa powder, which increased significantly (P < 0.05) when compared to 0 h. The hydrolysate of five M. crassa strains extracts potentially decrease pathogenic bacteria; Shigella DMST 1511, Staphylococcus aureus TISTR 029, E. coli E010, Salmonella DMST 17,368, but boost the growth of lactic acid bacteria; Lactobacillus, Pediococcus and Enterococcus bacteria (Inyod et al. 2022). In another study, the powder of L. squarrosulus (LP) and its resistant hydrolysate (RH) improved L. crispatus JCM 5810 and L. crispatus JCM 5810 after 16 h, as well as later fecal microbiota fermentation of RH, increased the relative abundance of Lactobacillus in at least one volunteer (Ayimbila et al. 2022). Bifidobacterium and Lactobacillus are two well-known probiotic bacteria found in the intestine, promoting human health by modulating the enteric nervous system, increasing resistance to harmful bacteria, and stimulating the immune system (Wang et al. 2010; Zhang et al. 2020).
The Atopobium cluster increased significantly (P < 0.05) between 10 and 34 h of fermentation with FOS and M. crassa powder. Increased Atopobium abundance was found to have a negative correlation with the inflammation markers hs-CRP and BMI, and a positive correlation with HDL cholesterol, suggesting that it may play a role in the prevalence of T2DM (Sato et al. 2014). Another study found that increasing Atopobium could be one of the underlying mechanisms of Rifaximin-induced bowel inflammation reduction (Maccaferri et al. 2010).
FOS and M. crassa powder significantly increased the Bacteroidaceae/Prevotellaceae group (P < 0.01) between 10 and 34 h of fermentation. FOS recorded the highest impact on the Bacteroidaceae/Prevotellaceae group at 10 h, but from 24 to 34 h of fermentation, it was statistically comparable to M. crassa powder. Obesity and metabolic disturbances have been linked to low Bacteroidaceae/Prevotellaceae prevalence in rural Mexican school-aged children (Aguilar et al. 2020). Similarly, according to the BMI z-score, there was a decrease in Bacteroidaceae in children who were obese (Riva et al. 2017). These genera are known to vary substantially depending on the nature of the diet. Bacteroides and Prevotella genera are organisms that can grow on a variety of different substrates and are major producers of propionic acid. Propionic generation is substantial by 10, 24, and 34 h fermentation, and of the same order of magnitude, for M. crassa powder and the positive control FOS (Table 4). Thus, M. crassa powder may have similar effects to FOS in terms of promoting Bacteroidaceae/Prevotellaceae but not propionic generation. The hydrolysate of L. squarrosulus powder has recently been shown to reduce the ratio of Firmicutes/Bacteroidetes while increasing the relative abundance of key immunomodulators such as Bacteroides, Bifidobacterium, Clostridium cluster XIVa and IV, and Sutterella (Ayimbila et al. 2022).
There were no significant changes between substrates for the growth of C. histolyticum group, Faecalibacterium prausnitzii, and Roseburia genus, which declined but remained much higher than the negative control after 34 h of fermentation (P > 0.05). These essential bacteria must be preserved in a healthy gut microbiota to carry out regular physiological processes and avoid the onset of diseases. These bacteria could be partially maintained using M. crassa powder and FOS. F. Prausnitzii has a critical role in supplying energy for colonocytes as well as the cooperation of anti-inflammatory metabolites for intestinal health. As such, diabetes patients had a deficiency in butyrate-producing members of the Clostridiales family, such as F. prausnitzii, in their gut microbiome (Kwan et al. 2022). Also, in diabetic Chinese subjects, Roseburia and F. prausnitzii, were depleted (Zhang et al. 2013). Interestingly, these bacteria were unable to use M. crassa powder and FOS to growth, which was in a similar manner. F. prausnitzii strains have been shown to partially utilise polysaccharides frequently found in gut (Sun et al. 2022). Nonetheless, F. prausnitzii is well suited for the intestinal environment, where it may be cross-fed by the other intestinal microbiota members (Ferreira-Halder et al. 2017). FOS and M. crassa powder in the gut environment may, therefore, have comparable impacts on the development of these bacteria and their capacity to provide health benefits.
The Clostridium coccoides group increased significantly after 10 and 24 h for both substrates, with significant variations between them (P > 0.05). Remarkably, only M. crassa powder significantly improved the bacterial count at 34 h. The occurrence of C. coccoides decreased in both inflammatory bowel diseases (IBD) and ankylosing spondylitis (AS) (Cardoneanu et al. 2021). All substrates reduced Clostridium histolyticum levels over the course of fermentation, with no significant differences except at 34 h. The faecal flora of autistic spectrum disorders (ASDs) contained a higher incidence of the C. histolyticum group of bacteria than that of healthy children. Furthermore, members of this group are toxin producers, and may contribute towards gut dysfunction, with their metabolic products also exerting systemic effects (Parracho et al. 2005). Diet can influence the gut-brain axis (GBA), and prebiotics such as inulin, blueberry flavonoids (Sagbasan, 2022), and M. crassa powder may be useful in supporting these changes. The results also showed that after 10 h of fermentation between FOS and the mushroom powder, the Clostridium cluster IX population did not significantly decline. However, after 34 h, M. crassa powder caused a significant reduction that was statistically distinct from both the controls (P > 0.05). It was discovered that patients with portal hypertension had considerably lower amounts of Clostridium cluster IX than other patients. Therefore, M. crassa powder may not have a major impact on the proliferation of C. cluster IX in the gut.
Because the fermentation of these substrates led to the generation of acids, five SCFAs such as acetic acid, propionic acid, butyric acid, lactic acid, and formic acid were effectively observed (Table 4). After fermentation for 34 h, the SCFAs concentration in each group (M. crassa powder, negative control, and positive control (FOS) was noticeably increased. In comparison to the negative control group, the total SCFA concentration resulting from bacterial fermentation of M. crassa powder and FOS groups steadily increased from 10 to 34 h. These results suggest that mushroom macronutrients and FOS can gradually regulate the intestinal microenvironment to produce SCFAs, consistent with previous reports (Chen et al. 2019; Cui et al. 2022; Li et al. 2019). It is also important to identified that SCFAs produced in a negative control group were due to protein consumption by putrefactive bacteria in the faecal microflora, with acetic acid, propionic acid and butyric acid as the principal fermentation products (Feng et al. 2022). For M. crassa, the concentrations of acetic acid, propionic acid and butyric acid were 38.6 ± 16.1 mM and 15.59 ± 4.51 mM and 4.52 ± 3.00 at 24 h, respectively. Propionic acid level in M. crassa fermentation was likewise substantially greater than in FOS.
After 34 h, the concentrations of acetic acid induced by M. crassa powder, negative control and FOS were 38.6, 10.40 and 51.3 mM, respectively. Acetic acid is important as a source of energy for intestinal microbiota, activate G protein-coupled GPR41 and GPR43 receptors, which stimulate the intestinal microbiota to produce SCFA and adipose-insulin signalling, accordingly (Kimura et al. 2019). A study of the gut microbiota and obesity in 499 Chinese peri- and postmenopausal women found that high level of Bacteroides fragilis may contribute to obesity by reducing acetic acid levels (Shen et al. 2022). Therefore, using M. crassa powder to promote acetic acid level may offer therapeutic targets for obesity intervention in peri- and post-menopausal women. Also, propionic acid was shown to effectively reduce the level of serum cholesterol, regulates blood lipid levels, improves the sensitivity of insulin tissue, and is immunocompromising (Laparra and Sanz 2010). It has been revealed that indole-3-propionic acid has a positive impact on host health due to its anti-inflammatory and ROS-scavenging properties (Konopelski and Mogilnicka 2022). Additionally, butyric acid has a number of biological effects, including maintaining the morphology and function of the intestinal barrier, as well as anti-cancer and anti-inflammatory effects (Cox and Blaser 2013). Recent data suggest that butyric acid released by sweet tea extract (STE) fermentation may be a key factor in promoting the integrity of the intestinal barrier in ulcerative colitis (UC) mice (He et al. 2022). Moreover, the ratio of some SCFAs in the gut enhances host health. For instance, acetic acid and propionic acid ratio not only provide the liver and surrounding tissues with energy, but also inhibit lipogenesis (Di et al. 2018). Importantly, the ratio of acetic to propionic acid increased considerably after M. crassa and FOS fermentation for 34 h. This increase has been shown to inhibit cholesterol and fatty acid synthesis and regulate blood lipid levels (Clemente et al. 2012). As a result, the amount of SCFAs in the gut generated by a dietary intervention is vital for the prevention of numerous diseases. It was observed that the total SCFA concentrations induced by M. crassa (58.9 ± 18.6), negative control (16.11 ± 0.57), and FOS (73.5 ± 30.1) were significantly different after 34 h. This suggested that M. crassa powder could be degraded and utilized by the gut microbiota, resulting in the production of several SCFAs that could regulate host's health. A current study was consistent with the result of Lentinus squarrosulus powder fermentation by human fecal microbiota that substantial SCFA and some content of branched chain fatty acids (BCFA) were produced (Ayimbila et al. 2022). Again, intestinal flora fermented polysaccharide from Pleurotus eryngii to produce a variety of short-chain fatty acids (SCFAs), which lowered the pH level in fecal culture (Ma et al. 2022). Clearly, mushrooms, particularly M. crassa, provides an essential source of bioactive components that can regulate SCFAs to prevent or control a variety of human disorders.
It is well known that certain gut bacteria can stimulate the growth of others via cross-feeding, resulting in a variety of fermentation products. Acetate production pathways are widely distributed among bacterial classes and reach their peak concentration in the intestinal lumen (Louis and Flint 2017; Saa et al. 2021), unlike propionic acid and butyric acid pathways, which are more conserved and substrate specific (Portincasa et al. 2022). Fermentation intermediates such as lactic acid and formic acid tend to build in faecal fermentations of rapidly fermented substrates such as FOS. Following the fermentation of all the substrates, an increased number of Bifidobacterium spp. and Lactobacillus/Enterococcus groups were identified (Table 3). Lactic acids produced by both bifidobacteria and lactobacilli were considerably higher at 10 h during faecal FOS and M. crassa powder fermentation, showing that these substrates fermented rapidly. Similarly, a study found a link between Bifidobacterium spp. and lactic acid bacteria and lactic acid levels after 10 h of FOS fermentation, but this relationship was lost afterward (Prayoonthien et al. 2019). The results indicate that other bacteria use lactic acid to produce acetic acid, butyric acid, and propionic acid. Meanwhile, the Bacteroidaceae/Prevotellaceae and Clostridium cluster IX are known propionic acid producers (Madsen et al. 2017), with a trend of increasing numbers of these bacteria along with propionic acid concentrations, as noticed during M. crassa fermentation in this study. This shows that M. crassa may trigger propionic acid synthesis more effectively than FOS by increasing the amount of Bacteroidaceae/Prevotellaceae group and Clostridium cluster IX.
In addition, Clostridium histolyticum counts decreased while the acetic acid concentration increased after 10 h of fermentation with all substrates. After 10 h, the populations of Bifidobacterium spp., Atopobium cluster, Bacteroidaceae/Prevotellaceae, and C. coccoides increased in correlation with the concentration of acetic acid. This was most visible with FOS, followed by the mushroom powder. Hence, the decrease in Clostridium histolyticum may be associated with higher acetic acid concentrations (Prayoonthien et al. 2019). Besides, Bifidobacteria can use inulin-type fructans and intricate carbohydrates to produce acetic acid and lactic acid via a pathway known as the “bifid shunt” with fructose 6-phosphate phosphoketolase as the central enzyme (De Vuyst et al. 2014; Tsukuda et al. 2021). Hence, FOS and M. crassa powder promoted a comparable number of Bifidobacterium spp., but FOS fermentation produced higher concentrations of acetic acid and lactic acid. This could be due to FOS's lower degree of polymerization (DP) and higher purity when compared to the mushroom powder. Similarly, M. crassa and FOS stimulated Bifidobacterium, which suggests that M. crassa contains a significant amount of glucose in the form of β-glucans (Mo et al. 2022). Bifidobacterium species, which are frequently thought to be the target of prebiotic action, can utilize polysaccharides found in mushrooms, including β-glucans (González et al. 2021).
The human gut microbiota performs a variety of functions, including the production of various metabolites such as vitamins and short-chain fatty acids (SCFAs), the maintenance of the epithelial barrier, the inhibition of pathogen adhesion to intestinal surfaces, the degradation of previously indigestible carbon sources (such as mushrooms), and immune system modulation and maturation (Sánchez et al. 2017). Alterations in the composition of intestinal microbiota are linked with various diseases, such as obesity, atherosclerosis, chronic kidney disease, diabetes mellitus type 2, heart failure, and high blood pressure (Vijay and Valdes 2022). Various bioactive mushroom compounds have been proven to alter the intestinal microbiota and improve health. Mushroom components (hemicellulose, chitin, α- and β-glucans, mannans, xylans, and galactans) may serve to promote the growth of probiotic bacteria in the intestine and to decrease pathogenic proliferation (Kumari 2020). Therefore, consuming M. crassa mushrooms may improve GI health by stimulating the immune system, reducing bowel inflammation, obesity and metabolic disturbances, hypertension, and preventing toxin-producers that cause gut dysfunction.
Moreover, prebiotic compounds are Gastrointestinal tract (GI) tolerable (pharmacodynamic) in the presence of salivary amylases, gastric juices, or bile extract and retain their capacity to stimulate beneficial microbes to improve health (pharmacodynamic) in the host (Gibson 2022). However, the low bioavailability of phenols and proteins, in particular, due to the impact of GI conditions, may compromise their biological and pharmacological benefits (Nunes et al. 2017). The potential use of M. crassa as a prebiotic was thus shown in this study based on the growth of intestinal bacteria and SCFAs in human excretions. Interestingly, M. crassa powder contains excellent bioactive compounds that can stimulate the composition of the faecal microbiota, and hence, supplying it at a suitable site would overcome the pharmacokinetic limitations of M. crassa powder and improve its pharmacodynamic potential.
Conclusion
Individual health demands have prompted a search for functional foods that can alter the gut flora and improve health. The functional composition of M. crassa powder consists primarily of protein (14.31%), carbohydrates (65.3%), beta (β)-glucan (37.6%), low-fat content (4.89%), and phenolics (4.76 0.05 mg GAE/g). In vitro fermentation revealed that M. crassa powder was fermented by the gut microbiota to produce SCFAs, which increased with time. The principal products of the SCFA were acetic acid, propionic acid and butyric acid. The M. crassa fermentation produced more propionic acid, and less acetic and butyric acids in comparison with FOS fermentation. Also, M. crassa increased the populations of Bifidobacterium, Lactobacillus/Enterococcus group, Atopobium cluster, Bacteroidaceae/Prevotellaceae and C. coccoides. F. prausnitzii, Roseburia genus, C. histolyticum and C. cluster IX counts, on the other hand, were reduced. M. crassa powder apparently increases propionic acid production by increasing the number of the Bacteroidaceae/Prevotellaceae group and C. cluster IX more than FOS. Whereas, Bifidobacterium spp., Atopobium cluster, Bacteroidaceae/Prevotellaceae and C. coccoides populations increased in correlation with the concentration of acetic acid for FOS and M. crassa. The findings suggest that, similar to FOS, M. crassa fruit bodies can be utilized by gut microorganisms to create SCFAs and modulate the composition of gut microbiota. The results validate the biological potential of this mushroom for use as a functional food source to improve health and prevent diseases by promoting intestinal health in the future. As a result, future research should investigate the effect of M. crassa powder on human gut microbiota in relation to diseases such as diabetes, inflammation, colonic cancer, and autism spectrum disorders (ASDs).
References
Aguilar T, Nava GM, Olvera-Ramírez AM, Ronquillo D, Camacho M, Zavala GA, Caamaño MC, Acevedo-Whitehouse K, Rosado JL, García OP (2020) Gut bacterial families are associated with body composition and metabolic risk markers in school-aged children in rural Mexico. Childhood Obes 16(5):358–366
AOAC (1995) Official methods of analysis of the Association of Official Analytical Chemists. Retrieved from
Ayimbila F, Keawsompong S (2021) Functional composition and antioxidant property of crude polysaccharides from the fruiting bodies of Lentinus squarrosulus. 3 Biotech 11(1):1–13
Ayimbila F, Siriwong S, Nakphaichit M, Keawsompong S (2022) In vitro gastrointestinal digestion of Lentinus squarrosulus powder and impact on human fecal microbiota. Sci Rep 12(1):1–17
Cantu-Jungles TM, Ruthes AC, El-Hindawy M, Moreno RB, Zhang X, Cordeiro LM, Hamaker BR, Iacomini M (2018) In vitro fermentation of Cookeina speciosa glucans stimulates the growth of the butyrogenic Clostridium cluster XIVa in a targeted way. Carbohydr Polym 183:219–229
Cardoneanu A, Mihai C, Rezus E, Burlui A, Popa I, Prelipcean CC (2021) Gut microbiota changes in inflammatory bowel diseases and ankylosing spondylitis. J Gastrointestin Liver Dis. https://doi.org/10.15403/jgld-2823
Carlson JL, Erickson JM, Lloyd BB, Slavin JL (2018) Health effects and sources of prebiotic dietary fiber. CDN 2(3):nzy005
Carrasco-González JA, Serna-Saldívar SO, Gutiérrez-Uribe JA (2017) Nutritional composition and nutraceutical properties of the Pleurotus fruiting bodies: potential use as food ingredient. J Food Compost Anal 58:69–81
Cateni F, Gargano ML, Procida G, Venturella G, Cirlincione F, Ferraro V (2021) Mycochemicals in wild and cultivated mushrooms: nutrition and health. Phytochem Rev 21:339–383. https://doi.org/10.1007/s11101-021-09748-2
Chen G, Xie M, Wan P, Chen D, Ye H, Chen L, Zeng X, Liu Z (2018) Digestion under saliva, simulated gastric and small intestinal conditions and fermentation in vitro by human intestinal microbiota of polysaccharides from Fuzhuan brick tea. Food Chem 244:331–339
Chen Y, Liu D, Wang D, Lai S, Zhong R, Liu Y, Yang C, Liu B, Sarker MR, Zhao C (2019) Hypoglycemic activity and gut microbiota regulation of a novel polysaccharide from Grifola frondosa in type 2 diabetic mice. Food Chem Toxicol 126:295–302
Clemente JC, Ursell LK, Parfrey LW, Knight R (2012) The impact of the gut microbiota on human health: an integrative view. Cell 148(6):1258–1270
Cox LM, Blaser MJ (2013) Pathways in microbe-induced obesity. Cell Metab 17(6):883–894
Cui S, Guo W, Chen C, Tang X, Zhao J, Mao B, Zhang H (2022) Metagenomic analysis of the effects of Lactiplantibacillus plantarum and fructooligosaccharides (FOS) on the fecal microbiota structure in mice. Foods 11(9):1187
Das AK, Nanda PK, Dandapat P, Bandyopadhyay S, Gullón P, Sivaraman GK, McClements DJ, Gullón B, Lorenzo JM (2021) Edible mushrooms as functional ingredients for development of healthier and more sustainable muscle foods: a flexitarian approach. Molecules 26(9):2463
De Vuyst L, Moens F, Selak M, Rivière A, Leroy F (2014) Summer meeting 2013: growth and physiology of bifidobacteria. J Appl Microbiol 116(3):477–491
Di T, Chen G, Sun Y, Ou S, Zeng X, Ye H (2018) In vitro digestion by saliva, simulated gastric and small intestinal juices and fermentation by human fecal microbiota of sulfated polysaccharides from Gracilaria rubra. J Funct Foods 40:18–27
FDA U (2013) Guidance for industry: a food labeling guide. In: US Department of Health and Human services, Food and Drug Administration
Feng C, Tian L, Hong H, Wang Q, Zhan X, Luo Y, Tan Y (2022) In vitro gut fermentation of whey protein hydrolysate: an evaluation of its potential modulation on infant gut microbiome. Nutr 14(7):1374
Ferreira-Halder CV, de Sousa Faria AV, Andrade SS (2017) Action and function of Faecalibacterium prausnitzii in health and disease. Best Pract Res Clin Gastroenterol 31(6):643–648
Franks AH, Harmsen HJ, Raangs GC, Jansen GJ, Schut F, Welling GW (1998) Variations of bacterial populations in human feces measured by fluorescent in situ hybridization with group-specific 16S rRNA-targeted oligonucleotide probes. Appl Environ Microbiol 64(9):3336–3345
Ghosh S, Acharya K (2022) Milky mushroom: a healthy nutritious diet. Food Res Int 156:111113. https://doi.org/10.1016/j.foodres.2022.111113
Gibson GR (2022) Commentary on: prebiotic effects: metabolic and health benefits. Br J Nutr 127(4):554–555
Gibson GR, Scott KP, Rastall RA, Tuohy KM, Hotchkiss A, Dubert-Ferrandon A, Gareau M, Murphy EF, Saulnier D, Loh G, Macfarlane S, Delzenne N, Ringel Y, Kozianowski G, Dickmann R, Lenoir-Wijnkoop I, Walker C, Buddington R (2010) Dietary prebiotics: Current status and new definition. IFIS Functional Foods Bulletin 7(1):1–19
Gibson, G., Hutkins, R., Sanders, M. et al. (2017) Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol 14:491–502. https://doi.org/10.1038/nrgastro.2017.75
González A, Nobre C, Simões LS, Cruz M, Loredo A, Rodríguez-Jasso RM, Contreras J, Texeira J, Belmares R (2021) Evaluation of functional and nutritional potential of a protein concentrate from Pleurotus ostreatus mushroom. Food Chem 346:128884
Harmsen HJ, Elfferich P, Schut F, Welling GW (1999) A 16S rRNA-targeted probe for detection of lactobacilli and enterococci in faecal samples by fluorescent in situ hybridization. Microb Ecol 11(1):3–12
Harmsen HJ, Wildeboer-Veloo AC, Grijpstra J, Knol J, Degener JE, Welling GW (2000) Development of 16S rRNA-based probes for the Coriobacterium group and the Atopobium cluster and their application for enumeration of Coriobacteriaceae in human feces from volunteers of different age groups. Appl Environ Microbiol 66(10):4523–4527
He X-Q, Liu D, Liu H-Y, Wu D-T, Li H-B, Zhang X-S, Gan R-Y (2022) Prevention of ulcerative colitis in mice by sweet tea (lithocarpus litseifolius) via the regulation of gut microbiota and butyric-acid-mediated anti-inflammatory signaling. Nutr 14(11):2208
Hold GL, Schwiertz A, Aminov RI, Blaut M, Flint HJ (2003) Oligonucleotide probes that detect quantitatively significant groups of butyrate-producing bacteria in human feces. Appl Environ Microbiol 69(7):4320–4324
Hussain N, Baqar Z, Mumtaz M, El-Sappah AH, Show PL, Iqbal HM, Varjani S, Bilal M (2022) Bioprospecting fungal-derived value-added bioproducts for sustainable pharmaceutical applications. Sustain Chem Pharm 29:100755
Inyod T, Sassanarakit S, Payapanon A, Keawsompong S (2016) Selection of Macrocybe crassa mushroom for commercial production. ANRES 50:186–191
Inyod I, Sassanarakit S, Payapanon A, Keawsompong S (2017) Morphological characteristics and molecular identification of a wild Thai isolate of the tropical mushroom Hed Taen Rad (Macrocybe crassa). Biodiversitas 18:221–228
Inyod T, Ayimbila F, Payapanon A, Keawsompong S (2022) Antioxidant activities and prebiotic properties of the tropical mushroom Macrocybe crassa. Bioact Carbohydr Diet Fibre 27:100298
Kang J, Yin S, Liu J, Li C, Wang N, Sun J, Li W, He J, Guo Q, Cui SW (2022) Fermentation models of dietary fibre in vitro and in vivo—a review. Food Hydrocoll. https://doi.org/10.1016/j.foodhyd.2022.107685
Kimura I, Ichimura A, Ohue-Kitano R, Igarashi M (2019) Free fatty acid receptors in health and disease. Physiol Rev. https://doi.org/10.1152/physrev.00041.2018
Konopelski P, Mogilnicka I (2022) Biological effects of indole-3-propionic acid, a gut microbiota-derived metabolite, and its precursor tryptophan in mammals’ health and disease. Int J Mol Sci 23(3):1222
Koutrotsios G, Patsou M, Mitsou EK, Bekiaris G, Kotsou M, Tarantilis PA, Pletsa V, Kyriacou A, Zervakis GI (2019) Valorization of olive by-products as substrates for the cultivation of Ganoderma lucidum and Pleurotus ostreatus mushrooms with enhanced functional and prebiotic properties. Catalysts 9(6):537
Kumar Singh A, Cabral C, Kumar R, Ganguly R, Kumar Rana H, Gupta A, Rosaria Lauro M, Carbone C, Reis F, Pandey AK (2019) Beneficial effects of dietary polyphenols on gut microbiota and strategies to improve delivery efficiency. Nutrients 11(9):2216
Kumari K (2020) Mushrooms as source of dietary fiber and its medicinal value: a review article. J Pharmacogn Phytochem 9:2075–2078
Kwan S-Y, Sabotta CM, Joon A, Wei P, Petty LE, Below JE, Wu X, Zhang J, Jenq RR, Hawk ET (2022) Gut microbiome alterations associated with diabetes in Mexican Americans in South Texas. Msystems. https://doi.org/10.1128/msystems.00033-22
Langendijk PS, Schut F, Jansen GJ, Raangs GC, Kamphuis GR, Wilkinson M, Welling GW (1995) Quantitative fluorescence in situ hybridization of Bifidobacterium spp. with genus-specific 16S rRNA-targeted probes and its application in fecal samples. Appl Environ Microbiol 61(8):3069–3075
Laparra JM, Sanz Y (2010) Interactions of gut microbiota with functional food components and nutraceuticals. Pharmacol Res 61(3):219–225
Li N, Wang Q, Wang Y, Sun A, Lin Y, Jin Y, Li X (2019) Fecal microbiota transplantation from chronic unpredictable mild stress mice donors affects anxiety-like and depression-like behavior in recipient mice via the gut microbiota-inflammation-brain axis. Stress 22(5):592–602
Li P-H, Chan Y-J, Lu W-C, Huang D-W, Chang T-C, Chang W-H, Nie X-B, Jiang C-X, Zhang X-L (2020) Bioresource utilization of djulis (Chenopodium formosanum) biomass as natural antioxidants. Sustain 12(15):5926
Liu J, Liu J, Shen F, Qin Z, Jiang M, Zhu J, Wang Z, Zhou J, Fu Y, Chen X (2018) Systems pharmacology analysis of synergy of TCM: an example using saffron formula. Sci Rep 8(1):1–11
Liu Y, Duan X, Duan S, Li C, Hu B, Liu A, Wu Y, Wu H, Chen H, Wu W (2020) Effects of in vitro digestion and fecal fermentation on the stability and metabolic behavior of polysaccharides from Craterellus cornucopioides. Food Funct 11(8):6899–6910
Loo YT, Howell K, Chan M, Zhang P, Ng K (2020) Modulation of the human gut microbiota by phenolics and phenolic fiber-rich foods. Compr Rev Food Sci Food Saf 19(4):1268–1298
Louis P, Flint HJ (2017) Formation of propionate and butyrate by the human colonic microbiota. Environ Microbiol 19(1):29–41
Ma G, Kimatu BM, Zhao L, Yang W, Pei F, Hu Q (2017) In vivo fermentation of a Pleurotus eryngii polysaccharide and its effects on fecal microbiota composition and immune response. Food Funct 8(5):1810–1821
Ma G, Xu Q, Du H, Kimatu BM, Su A, Yang W, Hu Q, Xiao H (2022) Characterization of polysaccharide from Pleurotus eryngii during simulated gastrointestinal digestion and fermentation. Food Chem 370:131303
Maccaferri S, Vitali B, Klinder A, Kolida S, Ndagijimana M, Laghi L, Calanni F, Brigidi P, Gibson GR, Costabile A (2010) Rifaximin modulates the colonic microbiota of patients with Crohn’s disease: an in vitro approach using a continuous culture colonic model system. J Antimicrob Chemother 65(12):2556–2565
Madsen L, Myrmel LS, Fjære E, Liaset B, Kristiansen K (2017) Links between dietary protein sources, the gut microbiota, and obesity. Front Physiol 8:1047
Mahdavi M, Laforest-Lapointe I, Massé E (2021) Preventing colorectal cancer through prebiotics. Microorganisms 9(6):1325
Manz W, Amann R, Ludwig W, Vancanneyt M, Schleifer K-H (1996) Application of a suite of 16S rRNA-specific oligonucleotide probes designed to investigate bacteria of the phylum cytophaga-flavobacter-bacteroides in the natural environment. Microbiology 142(5):1097–1106
Manzi P, Aguzzi A, Pizzoferrato L (2001) Nutritional value of mushrooms widely consumed in Italy. Food Chem 73(3):321–325
Mo X, Sun Y, Liang X, Li L, Hu S, Xu Z, Liu S, Zhang Y, Li X, Liu L (2022) Insoluble yeast β-glucan attenuates high-fat diet-induced obesity by regulating gut microbiota and its metabolites. Carbohydr Polym 281:119046
Munson RD, Nelson WL (1990) Principles and practices in plant analysis. Soil Testing and Plant Analysis 3:359–387
Nie Y, Yu M, Zhou H, Zhang P, Yang W, Li B (2020) Effect of boiling time on nutritional characteristics and antioxidant activities of Lentinus edodes and its broth. CyTA-J Food 18(1):543–550
Nunes S, Madureira AR, Campos D, Sarmento B, Gomes AM, Pintado M, Reis F (2017) Solid lipid nanoparticles as oral delivery systems of phenolic compounds: overcoming pharmacokinetic limitations for nutraceutical applications. Crit Rev Food Sci Nutr 57(9):1863–1873
Obodai M, Narh Mensah DL, Fernandes Â, Kortei NK, Dzomeku M, Teegarden M, Schwartz SJ, Barros L, Prempeh J, Takli RK (2017) Chemical characterization and antioxidant potential of wild Ganoderma species from Ghana. Molecules 22(2):196
Parracho HM, Bingham MO, Gibson GR, McCartney AL (2005) Differences between the gut microflora of children with autistic spectrum disorders and that of healthy children. J Med Microbiol 54(10):987–991
Payapanon A, Srijumpa N (2008) Collection and selection on strains of Macrocybe crassum from various sources for commercial production. Paper presented at the Proceedings of the 46th Kasetsart University Annual Conference, Kasetsart, 29 January-1 February, 2008. Subject: Plants
Portincasa P, Bonfrate L, Vacca M, De Angelis M, Farella I, Lanza E, Khalil M, Wang DQ-H, Sperandio M, Di Ciaula A (2022) Gut microbiota and short chain fatty acids: implications in glucose homeostasis. Int J Mol Sci 23(3):1105
Prayoonthien P, Rastall RA, Kolida S, Nitisinprasert S, Keawsompong S (2019) In vitro fermentation of copra meal hydrolysate by human fecal microbiota. 3 Biotech 9(3):1–11
Raman J, Jang K-Y, Oh Y-L, Oh M, Im J-H, Lakshmanan H, Sabaratnam V (2021) Cultivation and nutritional value of prominent Pleurotus spp.: an overview. Mycobiology 49(1):1–14
Riva A, Borgo F, Lassandro C, Verduci E, Morace G, Borghi E, Berry D (2017) Pediatric obesity is associated with an altered gut microbiota and discordant shifts in F. irmicutes populations. Environ Microbiol 19(1):95–105
Ruthes AC, Cantu-Jungles TM, Cordeiro LM, Iacomini M (2021) Prebiotic potential of mushroom D-glucans: implications of physicochemical properties and structural features. Carbohydr Polym 262:117940
Saa P, Urrutia A, Silva-Andrade C, Martín AJ, Garrido D (2021) Modeling approaches for probing cross-feeding interactions in the human gut microbiome. Comput Struct Biotechnol J 20:79–89
Sagbasan B (2022) Investigation of the impact of prebiotics and blueberry (source of flavonoids) on the production of metabolites by gut microbiota and related impacts on cognitive function. Univ Read. https://doi.org/10.48683/1926.00106778
Sánchez B, Delgado S, Blanco-Míguez A, Lourenço A, Gueimonde M, Margolles A (2017) Probiotics, gut microbiota, and their influence on host health and disease. Mol Nutr Food Res 61(1):1600240
Saranya T, Ramya S, Kavithaa K, Paulpandi M, Cheon Y-P, HaryshWinster S, Balachandar V, Narayanasamy A (2022) Green synthesis of selenium nanoparticles using solanum nigrum fruit extract and its anti-cancer efficacy against triple negative breast cancer. J Clust Sci. https://doi.org/10.1007/s10876-022-02334-2
Sato J, Kanazawa A, Ikeda F, Yoshihara T, Goto H, Abe H, Komiya K, Kawaguchi M, Shimizu T, Ogihara T (2014) Gut dysbiosis and detection of “live gut bacteria” in blood of Japanese patients with type 2 diabetes. Diabetes Care 37(8):2343–2350
Shen W-D, Lin X, Liu H-M, Li B-Y, Qiu X, Lv W-Q, Zhu X-Z, Greenbaum J, Liu R-K, Shen J (2022) Gut microbiota accelerates obesity in peri-/post-menopausal women via Bacteroides fragilis and acetic acid. Int J Obes. https://doi.org/10.1038/s41366-022-01137-9
Singdevsachan SK, Auroshree P, Mishra J, Baliyarsingh B, Tayung K, Thatoi H (2016) Mushroom polysaccharides as potential prebiotics with their antitumor and immunomodulating properties: a review. Bioact Carbohydr Diet 7(1):1–14
Sun Y, Zhang S, Nie Q, He H, Tan H, Geng F, Ji H, Hu J, Nie S, Nutrition, (2022) Gut firmicutes: relationship with dietary fiber and role in host homeostasis. Crit Rev Food Sci Nutr. https://doi.org/10.1080/10408398.2022.2098249
Swanson KS, Gibson GR, Hutkins R, Reimer RA, Reid G, Verbeke K, Scott KP, Holscher HD, Azad MB, Delzenne NM (2020) The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat Rev Gastroenterol Hepatol 17(11):687–701
Tian Y, Nichols RG, Roy P, Gui W, Smith PB, Zhang J, Lin Y, Weaver V, Cai J, Patterson AD (2018) Prebiotic effects of white button mushroom (Agaricus bisporus) feeding on succinate and intestinal gluconeogenesis in C57BL/6 mice. J Funct Foods 45:223–232
Tsukuda N, Yahagi K, Hara T, Watanabe Y, Matsumoto H, Mori H, Higashi K, Tsuji H, Matsumoto S, Kurokawa K (2021) Key bacterial taxa and metabolic pathways affecting gut short-chain fatty acid profiles in early life. ISME J 15(9):2574–2590
Verma R, Thakur A, Pandro V (2017) Diversity of Macro-fungi in central India-X: edible mushrooms Macrocybe crassa and Macrocybe lobayensis. Van Sangyan 4(12):39–49
Vijay A, Valdes AM (2022) Role of the gut microbiome in chronic diseases: a narrative review. Eur J Clin Nutr 76(4):489–501
Walker AW, Duncan SH, McWilliam Leitch EC, Child MW, Flint HJ (2005) pH and peptide supply can radically alter bacterial populations and short-chain fatty acid ratios within microbial communities from the human colon. Appl Environ Microbiol 71(7):3692–3700
Wang B, Mao YK, Diorio C, Pasyk M, Wu RY, Bienenstock J, Kunze WA (2010) Luminal administration ex vivo of a live Lactobacillus species moderates mouse jejunal motility within minutes. FASEB J 24(10):4078–4088
Willard HH, Merritt Jr LL, Dean JA, Settle Jr FA (1988) Instrumental methods of analysis, 7th edition. United States: Wadsworth Publishing Company
You SW, Hoskin RT, Komarnytsky S, Moncada M (2022) Mushrooms as functional and nutritious food ingredients for multiple applications. ACS Food Sci Technol 2(8):1184–1195
Zhang X, Shen D, Fang Z, Jie Z, Qiu X, Zhang C, Chen Y, Ji L (2013) Human gut microbiota changes reveal the progression of glucose intolerance. PLoS One 8(8):e71108
Zhang X, Aweya JJ, Huang Z-X, Kang Z-Y, Bai Z-H, Li K-H, He X-T, Liu Y, Chen X-Q, Cheong K-L (2020) In vitro fermentation of Gracilaria lemaneiformis sulfated polysaccharides and its agaro-oligosaccharides by human fecal inocula and its impact on microbiota. Carbohydr Polym 234:115894
Acknowledgements
This work was financially supported by the Office of the Ministry of Higher Education, Science, Research and Innovation; and Thailand Science Research and Innovation through the Kasetsart University Reinventing University Program 2021. The National Research Council of Thailand (NRCT) also provided financial support for this research project.
Author information
Authors and Affiliations
Contributions
FA, PP and TI performed an experiment. FA analysed the data and wrote the manuscript. DH and SK supervised the experiment and finally edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ayimbila, F., Prayoonthien, P., Inyod, T. et al. Bioactive composition and modulatory effects of Hed-Tean-Rad Mushroom, Macrocybe crassa on gut microbiota. 3 Biotech 12, 314 (2022). https://doi.org/10.1007/s13205-022-03388-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13205-022-03388-9