Abstract
Hospital cockroaches are probable sources of pathogenic bacteria. The present investigation was performed to assess the antibiotic resistance properties and distribution of virulence factors in the Streptococcus spp. isolated from hospital cockroaches. Six hundred and sixty cockroach samples were collected. Cockroaches were washed with normal saline, and the achieved saline was used for bacterial culture. Isolated Streptococcus spp. were subjected to disk diffusion. The distribution of virulence factors and antibiotic resistance genes were assessed using a polymerase chain reaction. The prevalence of S. pyogenes, S. agalactiae, and S. pneumonia amongst examined samples was 4.82%, 1.66%, and 6.96%, respectively. Cfb (53.93%), cyl (52.8%), scaa (51.68%) and glna (50.56%) were the most commonly detected virulence factors. Pbp2b (71.91%), pbp2x (58.42%), mefA (46.06%), ermB (46.06%) and tetM (46.06%) were the most commonly detected antibiotic resistance genes. Streptococcal spp. harbored the highest prevalence of resistance against tetracycline (80.89%), trimethoprim (65.16%), and penicillin (56.17%). To the best of our knowledge, this is the first prevalence report of virulence factors and antibiotic resistance genes in the Streptococcal spp. isolated from American, German, and oriental hospital cockroaches in Iran. Our findings indicated a certain role for cockroaches in nosocomial pathogens transmission in the hospital environment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cockroaches are considered among the most common pests in numerous homes and public places such as hospitals, hotels, bughouses, boarding schools, barracks, kindergartens, and dorms (Abdolmaleki et al. 2019b). Pest cockroaches are in close contact with humans (Doosti et al. 2015; Abdolmaleki et al. 2019a). Initially, they are tropical; however, most species live in parts of houses and other places where moisture, warmth, and food are adequate in the temperate zones (Feizhaddad et al. 2012; Abdolmaleki et al. 2019b). Among over 3500 recognized species, only a few ones are important to human, including Blattella germanica (German cockroach), Periplaneta americana (American cockroach), and Blatta orientalis (Oriental cockroach) (Pai et al. 2004; Lemos et al. 2006; Fakoorziba et al. 2010; Tetteh-Quarcoo et al. 2013; Pomés and Arruda 2014).
Cockroaches quickly move from buildings, gardens, drains, sewers, and latrines to human habitations. Since they feed on human food and feces, they can spread several types of pathogenic microorganisms. Likewise, several epidemiological investigations indicated that cockroaches were one of the main sources of different types of dangerous bacteria such as Shigella dysenteriae, Salmonella typhi, Streptococcus species (spp.), Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa (Pai et al. 2004; Lemos et al. 2006; Fakoorziba et al. 2010; Tetteh-Quarcoo et al. 2013; Pomés and Arruda 2014).
Streptococci are anaerobic gram-positive cocci forming a heterogeneous group with more than 30 different species. Some species such as S. pneumoniae, S. pyogenes (Lancefield Group A) and S. agalactiae (Lancefield Group B) are important human pathogens (Musher 1992; Tunkel and Sepkowitz 2002; Edwards and Baker 2005; Krzyaściak et al. 2013; Stevens and Bryant 2016; Ruppen et al. 2018). S. pneumoniae is recognized as one of the main causes of pneumonia, septic arthritis, acute sinusitis, endocarditis, pericarditis, peritonitis, meningitis, and septicaemia (Musher 1992; Edwards and Baker 2005; Krzyaściak et al. 2013). S. pyogenes causes serious infections including sepsis, necrotizing fasciitis, tonsillitis, and superficial skin infections (Edwards and Baker 2005; Krzyaściak et al. 2013; Stevens and Bryant 2016). Lastly, S. agalactiae is the most common cause of neonatal sepsis and animal mastitis (Krzyaściak et al. 2013; Ruppen et al. 2018).
Streptococcus spp. are mainly resistant to several antibiotics. In this regard, documented data indicated that Streptococcus spp. isolated from various clinical infections harbored a high prevalence of resistance against different antibiotics such as aminoglycosides, ampicillin, cephalothin, fluoroquinolone, sulfonamides, tetracyclines, trimethoprim, gentamicin, and chloramphenicol (Lin et al. 2004; Cattoir 2016). Studies into molecular epidemiological demonstrated that presence of specific antibiotic resistance genes, including those encoding resistance against penicillins (pbp (penicillin-binding protein)), tetracyclines (tetK, tetM, tetO, and tetL), macrolides (erm ((erythromycin ribosome methylase) and mef (macrolide efflux)), streptogramins A and B (rplV) (L22 and L4 ribosomal protein gene) and lytA (autolysin-encoding gene) are the most important reason for the occurrence of antibiotic resistance in these bacteria (Sapkota et al. 2006; Cattoir 2016).
Bac (encode for β-antigen), cyl (encode for β-hemolysin), glnA (encode for glutamine synthetase), cfb (encode for the Christie–Atkins–Munch–Peterson (CAMP) factor), hylB (encode for hyaluronidase), scaA (encode for aggregation factor), bca (encode for α-antigen), scpB (C5a peptidase) and lmb (laminin-binding protein) are another important virulence factors amongst the Streptococcus spp. isolated from clinical specimens (Kayansamruaj et al. 2014; Blumental et al. 2015). The presence of these virulence factors contributes to the high pathogenicity of Streptococcus spp. (Kayansamruaj et al. 2014; Blumental et al. 2015).
According to the high presence of cockroaches in the hospital environment as well as their significant importance as risk factors for maintenance and transmission of pathogenic bacteria, the present investigation was conducted to study the prevalence rate, distribution of virulence factors, and antimicrobial resistance properties of S. pneumoniae, S. pyogenes and S. agalactiae strains in German, American and Oriental cockroaches of Iranian hospitals.
Results
The present survey was conducted to assess the prevalence and distribution of the Streptococcus species' virulence factors and antibiotic resistance properties isolated from German, American, and Oriental cockroaches. Table 1 presents the total distribution of Streptococcus spp. isolated from different types of hospital cockroaches. The prevalence of S. pyogenes, S. agalactiae and S. pneumonia strains among all the studied samples was 4.82%, 1.66%, and 6.96%, respectively. Among other cockroach species, S. pneumonia had a higher prevalence (9.45%). A statistically significant difference was found between types of cockroaches and the prevalence of Streptococcus spp. (P < 0.05).
Table 2 shows the distribution of streptococcal putative virulence factors in different types of studied cockroaches. We found that cfb (53.93%), cyl (52.8%), scaa (51.68%), and glna (50.56%) were the most commonly detected streptococcal virulence factors. The highest prevalence of virulence factors was found in American cockroaches. The most commonly detected virulence factors amongst the German, American, and oriental cockroaches were cfb (85%), ScaA (63.15%), and cfb (50.00%), respectively. Among other cockroach species, Cyl (46.15%) was the most prevalent virulence factor. A statistically significant difference was found between types of cockroaches and the prevalence of virulence factors (P < 0.05).
Table 3 depicts the distribution of penicillin, macrolides, tetracyclines, and streptogramins antibiotic resistance genes in the Streptococcus spp. isolated from different types of hospital cockroaches. We found that pbp2b (71.91%), pbp2x (58.42%), mefA (46.06%), ermB (46.06%) and tetM (46.06%) were the most commonly detected antibiotic resistance genes in the Streptococcal spp. isolated from different types of hospital cockroaches. TetO (6.74%), DF-L22 (21.34%), and DF-L4 (24.71%) had the lowest prevalence in the studied antibiotic resistance genes. The most commonly detected antibiotic resistance genes amongst the German, American, and oriental cockroaches were pbp2b (80%), pbp2b and pbp2x (68.42%), and tetM (77.77%), respectively. Among other cockroach species, pbp2b (76.92%) was the most prevalent antibiotic resistance gene. A statistically significant difference was found between cockroaches and the prevalence of antibiotic resistance genes (P < 0.05).
Table 4 presents the antibiotic resistance pattern of the Streptococcus spp. isolated from different types of hospital cockroaches. Streptococcal spp. harbored the highest prevalence of resistance against tetracycline (80.89%), trimethoprim (65.16%), and penicillin (56.17%), while harbored the lowest against chloramphenicol (3.37%), ciprofloxacin (19.10%), and nitrofurantoin (29.21%). S. pyogenes strains harbored the highest prevalence of resistance against tetracycline (84.37%), penicillin (81.25%), enrofloxacin (56.25%), and erythromycin (53.12%). S. agalactiae strains harbored the highest prevalence of resistance against trimethoprim (72.72%), tetracycline (72.72%), penicillin (63.63%) and erythromycin (63.63%). S. pneumoniae strains harbored the highest prevalence of resistance against tetracycline (80.43%), trimethoprim (73.91%), and lincomycin (50.00%).
Discussion
Medically, cockroaches are much more important than generally realized as they have been demonstrated to harbor some pathogenic and non-pathogenic microorganisms. Since various workers have reported the isolation of various human pathogens from these insects, cockroaches are known vectors of human enteropathogens. Their filthy and nocturnal habits cause them to be ideal carriers for transmitting numerous pathogenic microorganisms. Klebsiella spp., E. coli, P. aeruginosa, Streptococcus spp. and some other potential pathogens have been isolated from cockroaches gathered from hospitals (Pai et al. 2004; Lemos et al. 2006; Fakoorziba et al. 2010; Tetteh-Quarcoo et al. 2013).
The present investigation was conducted to assess the prevalence rate, antibiotic resistance pattern, and genotyping evaluation of antibiotic resistance and virulence factor of the Streptococcus spp. isolated from American, German, oriental, and other species of hospital cockroaches. We found that S. pneumoniae had the highest prevalence among the studied cockroaches (6.96%). Oriental cockroaches had the highest prevalence of S. pyogenes (5.71%) and S. agalactiae (2.85%), while German cockroaches had the highest prevalence of S. pneumoniae (6.83%). Easily transmission of Hospital cockroaches in different parts of hospitals and sewage systems caused a high prevalence of Streptococcus spp. According to the research, American cockroaches are the most dangerous cockroach in nosocomial infections as they carry both of the highest virulence factors and antibiotic-resistant genes. Various studies have been carried out in this field. For example, Fotedar et al. (1991) indicated that one hundred and fifty-eight out of 159 (99–4%) cockroaches gathered from the hospital (test) and 113 out of 120 (94–2%) cockroaches gathered from residential areas (control) carried medically significant microorganisms. They indicated that 10–20% of cockroaches harbored Streptococcus spp. Kassiri et al. (2014) disclosed that culturing outer surface wash of cockroaches resulted in the isolation of Klebsiella, Pseudomonas, E. coli, Staphylococcus, Proteus, and Streptococcus. The main common bacteria were Klebsiella (35%) and Pseudomonas (30%). Elgderi et al. (2006) indicated that 27 and 25 species of the potential pathogen were isolated from the hospital and household cockroaches, respectively, with Klebsiella, Enterobacter, Serratia, and Streptococcus being predominant. Salehzadeh et al. (2007) demonstrated that 130 out of 133 (98%) German cockroaches had contamination with a high bacterial load (more than 1 × 103). Enterobacter (22.60%), Klebsiella (21%), Enterococcus (17.30%), Staphylococcus (16.50%), E. coli and Streptococcus (8.3%), Pseudomonas (3%), as well as Shigella, Haemophilus and group A ß-hemolytic Streptococcus (less than 1%) were the most commonly detected bacteria. Pai et al. (2004) revealed that the prevalence of Streptococcus spp. in the intestinal content and surface of American and German cockroaches were 38.10% and 38.80% and 32.80% and 17.20%, respectively. Similar findings were achieved in the studies conducted in Iran (Ahmad Vahhabi et al. 2011; Kassiri and Shahnaz 2012), Thailand (Chaichanawongsaroj et al. 2004), and Brazil (Prado et al. 2006). As S. agalactiae derived from animal species, particularly in the cases of bovine mastitis, its presence in the cockroaches may be explained by the permanent presence of cockroaches in the environment. They can transfer easily anywhere. As a result, they may transfer from the area near to mastitic cows.
Results of our investigation indicated that the Streptococcus spp. strains isolated from cockroaches harbored a high prevalence of resistance against the commonly used antibiotics, particularly tetracycline, trimethoprim, enrofloxacin, erythromycin, lincomycin, and penicillin. The findings demonstrate the antibiotic resistance seriousness of the common pathogenic bacteria in Iran. A boost prevalence of antibiotic resistance was also reported in the pathogenic bacteria in the hospitals of Taiwan (Chang et al. 2000). More than 30% of S. pneumoniae, S. aureus, Enterobacteriaceae, P. aeruginosa, Acinetobacter baumannii, Haemophilus influenza, coagulase-negative Staphylococci, beta-hemolytic Streptococci, viridans Streptococci, and Enterococcal isolates of Taiwanese hospitals were resistant to different antibiotics (Chang et al. 2000). Pai et al. (2004) reported that all common pathogenic bacteria (Streptococcus spp. S. aureus and P. aeruginosa) isolated from cockroaches harbored resistance against ampicillin, chloramphenicol, tetracycline, trimethoprim and sulfamethoxazole. Bouamama et al. (2010) reported that pathogenic bacterial strains isolated from American cockroaches in Spain harbored the high prevalence of resistance against ampicillin, amoxicillin-clavulanate, cefoxitin; gentamicin, cotrimoxazole, and ciprofloxacin antibiotics. Hammad and Mahdy (2012) reported the high prevalence of antibiotic resistance of Streptococcus spp. isolated from cockroaches against ampicillin, cephalothin, chloramphenicol, ciprofloxacin, gentamycin, nalidixic acid, tetracycline, trimethoprim and sulfamethoxazole. Different patterns of antibiotic resistance of pathogenic bacterial strains isolated from cockroaches have been reported from Bangladesh (Islam et al. 2016), Nigeria (Chakraborty et al. 2015), and India (Leshan Wannigama et al. 2013). Such differences in the prevalence of antibiotic resistance reported in different studies may be due to the differences in the idea of medical practitioners in antibiotic prescription, availability and expense of antibiotics, and the laws of various countries for an antibiotic prescription. Furthermore, the high prevalence of antibiotic resistance reported in the present study may be due to the irregular and unauthorized prescription of antibiotics. The phenotypic pattern of antibiotic resistance was supported by the genotypic profile of antibiotic resistance genes. We found that the genes encoding resistance against penicillins (pbp), tetracyclines (tetK, tetM, tetO, and tetL), macrolides (erm and mef), streptogramins A and B (rplV), and the lytA gene had considerable prevalence in the Streptococcus spp. strains isolated from hospital cockroaches. To the best of our knowledge, there existed no previously published data in this field in Iran. High prevalence of pbp, tetK, tetM, tetO, tetL, erm, mef, rplV, and lytA antibiotic resistance genes was reported in the Streptococcus spp. strains isolated from different hospital infections (Malhotra-Kumar et al. 2005; Zeng et al. 2006; Xu et al. 2010). Kargar et al. (2012) reported the high prevalence of ermB, mefA, pbp1a, pbp2b and pbp2x genes in the S. pneumonia strains isolated from different types of the hospital infections of hospitalized patients in the Intensive Care Unit (ICU) centers. Presence of these genes in the Streptococcus spp. caused their severe resistance against some specific antibiotics. Our findings also disclosed a higher incidence of the phenotypic profile of resistance to some antibiotic agents than genotypic profiles. This finding is maybe because the presence of antibiotic resistance genes is one of the known procedures for antibiotic resistance in bacteria. On the other hand, higher incidence of phenotypic resistance toward antibiotics may be supported by procedures other than the presence of antibiotic resistance genes.
The final part of the present research was focused on detecting putative virulence genes in the Streptococcus spp. strains isolated from different types of hospital cockroaches. We found that bac, cyl, glnA, cfb, hylB, scaA, bca, scpB, and lmb had considerable prevalence in Streptococcus. Spp. strains isolated from hospital cockroaches. To the best of our knowledge, there existed no previously published data in this field worldwide. The α-protein of protein C was encoded by bac and bca genes. This gene group helps bacteria to enter the host cells. Genes bac and bca were detected in 1.12% and 6.74% of bacteria, respectively. Eskandarian et al. (2015) reported that the bca and bac genes were found in 14.6% and 9.7% of Streptococcus isolates of hospital infections. A lower prevalence of the bac gene was reported from the United States, New Zealand, and Europe (Manning et al. 2006; Persson et al. 2008; Sadowy et al. 2010). We found that the prevalence of cyl, lmb, and scpB genes was 52.80%, 22.47% and 7.86%, respectively. Duarte et al. (2005) reported that the prevalence of lmb and scpB genes in the Streptococcus spp. strains isolated from clinical samples was 97.30% and 96.70%, respectively, which was higher than our findings. Franken et al. (2001) and Dmitriev et al. (1999) also reported a higher prevalence of these genes. Cfb gene is encoded by complement factor B facilitating the essential component of the alternative course of complement activation. Factor B circulates in the blood as one chain polypeptide. This gene was also predominant in the Streptococcus spp. strains isolated from different hospital infections (Udo et al. 2013; Ding et al. 2016).
The current survey revealed that hospital cockroaches, mainly German and American types, may be sources and reservoirs of pathogenic and antibiotic-resistant Streptococcus spp. Thus, monitoring hospital cockroaches may be helpful to decrease the dissemination of virulent and resistant bacteria in the hospital environment.
Conclusions
In summary, the present study results disclosed the high prevalence of different cockroaches in the hospital environment with high content of S. pyogenes, S. agalactiae, and S. pneumoniae strains. High prevalence of resistance against the commonly used antibiotics with the considerable distribution of virulence and antibiotic resistance genes in the Streptococcus spp. strains isolated from hospital cockroaches pose a significant public health issue. The presence of multi-drug resistant strains increases the importance of the research. The present study shows the high importance of hospital cockroaches as dangerous reservoirs for harboring virulent and resistant Streptococcus strains in the hospital environment and their transmission to the human population. Moreover, with a considerable rate of medically significant virulent and resistant bacteria, cockroaches may cause bacterial epidemic disease in hospitals. The findings indicate a possible role for cockroaches in the epidemiology of nosocomial infections, particularly those caused by Streptococcus spp. However, further studies are required to find additional knowledge about the microbiological and epidemiological roles of the hospital cockroaches in the survival and transmission of virulent and antibiotic-resistant bacteria.
Materials and methods
Sample's collection
From July 2016 to July 2020, 660 hospital cockroach samples were randomly collected from different educational hospitals. The cockroaches were gathered using hand catch, sticky traps, and vacuum cleaner methods. For sampling, sterile hand-gloves were used. Separate clean and sterile plastic bags were utilized to transfer the collected cockroaches (Paul et al. 1992). Only whole and alive cockroaches were investigated in the study. The samples were immediately transferred to Biotechnology Research Center, Shahrekord Branch, Sharekord, Iran. The cockroaches were identified using reliable taxonomic keys by an expert in the Department of Entomology, Shahrekord University, Shahrekord, Iran (Burgess 1993).
Isolation and identification of Streptococcus spp.
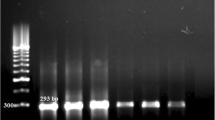
Sterile normal saline (0.9%) (5 mL) (Merck, Germany) was added to each test tube, and the cockroaches were vigorously washed and transferred to the secondary sterile test tubes using sterile forceps. A loop full of each suspension was cultured on streptococcal selection broth (BD Biosciences, USA) and incubated at 37 °C for 6 h with 5% CO2. After enrichment, the samples were streaked onto 5% sheep blood agar and incubated at 37 °C for 24–48 h with 5% CO2. The suspected streptococcal colonies were purified on BHI agar (Merck, Germany). The cultures purified were tentatively identified based on Gram's staining and biochemical tests, including bile esculin hydrolysis, catalase, and oxidase. Species identification was carried out using specific biochemical tests, including hemolysis activity (S. pneumonia (alpha), S. pyogenes (beta) and S. agalactiae (beta)), resistance to bacitracin (S. pneumonia (resistant/sensitive), S. pyogenes (sensitive) and S. agalactiae (resistant)), resistance to sulfamethoxazole (S. pneumonia (-), S. pyogenes (resistant) and S. agalactiae (resistant)), resistance to optochin (S. pneumonia (sensitive), S. pyogenes (resistant) and S. agalactiae (resistant)), bile:asculin activity (S. pneumonia (−/−), S. pyogenes (−/−) and S. agalactiae (−/+ and −/+)) and growth on 6.5% NaCl (S. pneumonia (−), S. pyogenes (−) and S. agalactiae (−)). Confirmation of the species was carried out using the specific Polymerase Chain Reaction (PCR). According to the manufacturer's instruction, genetic DNA was extracted from bacterial colonies using the DNA extraction kit (Fermentas, Germany). Purity (A260/A280) and concentration of extracted DNA were then checked (NanoDrop, Thermo Scientific, Waltham, MA, USA). The truth of the DNA was assessed on a 2% agarose gel stained with ethidium bromide (0.5 μg/mL) (Thermo Fisher Scientific, St. Leon-Rot, Germany). Table 5 shows the list of primers and the PCR conditions used to detect S. pyogenes, S. agalactiae, and S. pneumonia in DNA samples. Primers specific for S. pyogenes, S. agalactiae, and S. pneumonia were designed based on its conservative 16S ribosomal RNA (16S rRNA) gene. Each PCR reaction contained 4 μL of the extracted template DNA, 1.25 U of Taq DNA polymerase, 1 μM of each primer, 2 mM MgCl2, 5 μL of 10X PCR buffer, 200 μM dNTPs, and double-distilled water was added to a final volume of 25 μL.
Antibiotic susceptibility test
Antibiotic resistance patterns of Streptococcus spp. were specified by the simple disk diffusion method. The Mueller–Hinton agar (Merck, Germany) media were used for the antibiotic susceptibility test. For this purpose, the principles proposed by the Clinical and Laboratory Standards Institute (CLSI) were used (Wayne 2015). A 0.5 McFarland concentration of bacteria was prepared and used in the disk diffusion. Susceptibility of Streptococcus spp. was tested against tetracycline (30 u/disk), penicillin (10 u/disk), cephalothin (30 µg/disk), gentamicin (10 µg/disk), ciprofloxacin (5 µg/disk), lincomycin (15 µg/disk), nitrofurantoin (300 µg/disk), enrofloxacin (5 µg/disk), sulfamethoxazole (25 µg/disk), trimethoprim (5 µg/disk), erythromycin (15 µg/disk) and chloramphenicol (30 µg/disk) antibiotic agents (Oxoid, UK). The inoculated plates were aerobically incubated at 37 °C for 18–24 h in an anaerobic atmosphere. Results were interpreted based on the instruction provided by CLSI (2015). S. pyogenes ATCC 12,384, S. pneumonia ATCC 6305, and S. agalactiae ATCC 27,956 were used as quality controls.
PCR-based detection of virulence factors
Table 5 represents the primer sequence and PCR conditions used to detect putative virulence factors in the Streptococcus spp. isolated from different types of hospital cockroaches. Each PCR reaction contained 5 μL of 10X PCR amplification buffer, 2 μL of extracted DNA, 1 U of Taq DNA polymerase, 1 μM of each primer, 2 mM MgCl2, 200 μM dNTPs, and double-distilled water was added to a final volume of 25 μL.
PCR-based detection of antibiotic resistance genes
Table 5 represents the primer sequence and PCR conditions used to detect penicillin, macrolide, streptogramin, and tetracycline antibiotic resistance genes in the Streptococcus spp. isolated from different types of hospital cockroaches. Each PCR reaction contained 3 μL of extracted template DNA, 1 U of Taq DNA polymerase, 1 μM of each primer, 2 mM MgCl2, 5 μL of 10X PCR buffer, 200 μM dNTPs, and double-distilled water was added to a final volume of 25 μL. Positive DNA of each targeted gene was used as positive, while sterile PCR grade water (Thermo Fisher Scientific, Germany) was used as negative controls.
Agarose gel electrophoresis
The PCR amplified products (10 μL) were subjected to electrophoresis on a 1.5% agarose gel in 1X TBE buffer at 80 V for 30–40 min stained with a solution of ethidium bromide (Fermentas, Germany) and examined under Ultra Violet illumination (Uvitec, UK) (Ranjbar and Chehelgerdi 2018; Sadeghifard et al. 2010; Ranjbar et al. 2018).
Statistical analysis
The data obtained from all the tests were entered into the Microsoft Excel spreadsheet (Microsoft Corp., Redmond, WA) to be analyzed. All the data were first presented to the Kolmogorov–Smirnov to study their distribution. In this respect, the statistical analysis was then conducted using SPSS/20.0 software (SPSS Inc., Chicago, IL). P-values were calculated using Chi-square and Fisher's exact tests to find any significant relationship between Streptococcus spp. and their virulence factors and antibiotic resistance properties among different types of hospital cockroaches. The P-value less than 0.05 was considered statistically significant.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- S. pneumoniae :
-
Streptococcus pneumonia
- S. pyogenes :
-
Streptococcus pyogenes
- S. agalactiae :
-
Streptococcus agalactiae
- bac :
-
Encode for β-antigen
- cyl :
-
Encode for β-hemolysin
- glnA :
-
Encode for glutamine synthetase
- cfb :
-
Encode for the Christie–Atkins–Munch–Peterson (CAMP) factor
- hylB :
-
Encode for hyaluronidase
- scaA :
-
Encode for aggregation factor
- bca :
-
Encode for α-antigen
- scpB :
-
C5a peptidase
- lmb :
-
Laminin-binding protein
- CLSI:
-
Clinical Laboratory Standards Institute
- PCR:
-
Polymerase chain reaction
References
Abdolmaleki Z, Mashak Z, Dehkordi FS (2019a) Molecular and virulence characteristics of methicillin-resistant staphylococcus aureus bacteria recovered from hospital cockroaches. Jundishapur J Microbiol. https://doi.org/10.5812/jjm.98564
Abdolmaleki Z, Mashak Z, SafarpoorDehkordi F (2019b) Phenotypic and genotypic characterization of antibiotic resistance in the methicillin-resistant Staphylococcus aureus strains isolated from hospital cockroaches. Antimicrob Resist Infect Control. https://doi.org/10.1186/s13756-019-0505-7
Ahmad Vahhabi A, Shemshad K, Mohammadi P et al (2011) Microbiological study of domestic cockroaches in human dwelling localities. Afr J Microbiol Res 5:5790–5792. https://doi.org/10.5897/AJMR11.1075
Billal DS, Hotomi M, Suzumoto M et al (2008) Determination of pneumococcal serotypes/genotypes in nasopharyngeal secretions of otitis media children by multiplex PCR. Eur J Pediatr 167:401–407. https://doi.org/10.1007/s00431-007-0510-3
Blumental S, Granger-Farbos A, Moïsi JC et al (2015) Virulence factors of Streptococcus pneumoniae comparison between African and French invasive isolates and implication for future vaccines. PLoS ONE 10:1. https://doi.org/10.1371/journal.pone.0133885
Bouamama L, Sorlozano A, Laglaoui A et al (2010) Antibiotic resistance patterns of bacterial strains isolated from Periplaneta americana and Musca domestica in Tangier, Morocco. J Infect Dev Ctries 4:194–201
Burgess NRH (1993) Cockroaches (Blattaria). Medical insects and arachnids. Springer, Netherlands, Dordrecht, pp 473–482
Cattoir V (2016) Mechanisms of antibiotic resistance. In: Ferretti JJ, Stevens DL, Fischetti VA (eds) Streptococcus pyogenes: Basic biology to clinical manifestations [Internet]. University of Oklahoma Health Sciences Center, Oklahoma City (OK), PMID: 26866217
Chaichanawongsaroj N, Vanichayatanarak K, Pipatkullachat T et al (2004) Isolation of gram-negative bacteria from cockroaches trapped from urban environment. Southeast Asian J Trop Med Public Health 35:681–684
Chakraborty A, Pal NK, Sarkar S, Gupta MS (2015) Antibiotic resistance pattern of Enterococci isolates from nosocomial infections in a tertiary care hospital in Eastern India. J Nat Sci Biol Med 6(2):394–397. https://doi.org/10.4103/0976-9668.160018
Chang SC, Hsieh WC, Liu CY (2000) High prevalence of antibiotic resistance of common pathogenic bacteria in Taiwan. The antibiotic resistance study group of the infectious disease society of the Republic of China. Diagn Microbiol Infect Dis 36:107–112
Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Testing (2015) Wayne, PA, USA: CLSI
Ding Y, Zhao J, He X et al (2016) Antimicrobial resistance and virulence-related genes of Streptococcus obtained from dairy cows with mastitis in Inner Mongolia, China. Pharm Biol 54:162–167. https://doi.org/10.3109/13880209.2015.1025290
Dmitriev A, Tkáciková L, Suvorov A et al (1999) Comparative genetic study of group B streptococcal strains of human and bovine origin. Folia Microbiol (praha) 44:449–453
Dmitriev A, Hu YY, Shen AD et al (2002) Chromosomal analysis of group B streptococcal clinical strains; bac gene-positive strains are genetically homogenous. FEMS Microbiol Lett 208:93–98. https://doi.org/10.1016/S0378-1097(02)00446-9
Doosti A, Pourabbas M, Arshi A et al (2015) TEM and SHV genes in klebsiella pneumoniae isolated from cockroaches and their antimicrobial resistance pattern. Osong Public Heal Res Perspect 6:3–8. https://doi.org/10.1016/j.phrp.2014.10.011
Duarte RS, Bellei BC, Miranda OP et al (2005) Distribution of antimicrobial resistance and virulence-related genes among Brazilian group B streptococci recovered from bovine and human sources. Antimicrob Agents Chemother 49:97–103. https://doi.org/10.1128/AAC.49.1.97-103.2005
Edwards MS, Baker CJ (2005) Group B streptococcal infections in elderly adults. Clin Infect Dis an off Publ Infect Dis Soc Am 41:839–847. https://doi.org/10.1086/432804
Elgderi RM, Ghenghesh KS, Berbash N (2006) Carriage by the German cockroach (Blattella germanica) of multiple-antibiotic-resistant bacteria that are potentially pathogenic to humans, in hospitals and households in Tripoli, Libya. Ann Trop Med Parasitol 100:55–62. https://doi.org/10.1179/136485906X78463
Eskandarian N, Ismail Z, Neela V et al (2015) Antimicrobial susceptibility profiles, serotype distribution and virulence determinants among invasive, non-invasive and colonizing Streptococcus agalactiae (group B streptococcus) from Malaysian patients. Eur J Clin Microbiol Infect Dis 34:579–584. https://doi.org/10.1007/s10096-014-2265-x
Fakoorziba MR, Eghbal F, Hassanzadeh J, Moemenbellah-Fard MD (2010) Cockroaches (Periplaneta americana and Blattella germanica) as potential vectors of the pathogenic bacteria found in nosocomial infections. Ann Trop Med Parasitol 104:521–528. https://doi.org/10.1179/136485910X12786389891326
Farrell DJ, Douthwaite S, Morrissey I et al (2003) Macrolide resistance by ribosomal mutation in clinical isolates of Streptococcus pneumoniae from the PROTEKT 1999–2000 study. Antimicrob Agents Chemother 47:1777–1783. https://doi.org/10.1128/AAC.47.6.1777-1783.2003
Feizhaddad MH, Kassiri H, Sepand MR, Ghasemi F (2012) Bacteriological survey of American cockroaches in hospitals. Middle East J Sci Res 12:985–989. https://doi.org/10.5829/idosi.mejsr.2012.12.7.7153
Fotedar R, Shriniwas UB, Verma A (1991) Cockroaches (Blattella germanica) as carriers of microorganisms of medical importance in hospitals. Epidemiol Infect 107:181–187. https://doi.org/10.1017/S0950268800048809
Franken C, Haase G, Brandt C et al (2001) Horizontal gene transfer and host specificity of beta-haemolytic streptococci: the role of a putative composite transposon containing scpB and lmb. Mol Microbiol 41:925–935. https://doi.org/10.1046/j.1365-2958.2001.02563.x
Hammad KM, Mahdy HM (2012) Antibiotic resistant-bacteria associated with the cockroach, Periplaneta americana collected from different habitat in Egypt. NY Sci J NY Sci J 55:198–206
Islam A, Aurjun ND, Islam K et al (2016) Isolation, identification and antimicrobial resistance profile of Staphylococcus aureus in Cockroaches (Periplaneta a mericana). J Adv Vet Anim Res Islam Al J Adv Vet Anim Res 3:221–228. https://doi.org/10.5455/javar.2016.c153
Kargar M, Baghernejad M, Ghorbani-Dalini S (2012) Multi-drug resistance and molecular pattern of erythromycin and penicillin resistance genes in Streptococcus pneumoniae. Afr J Biotechnol 11:968–973. https://doi.org/10.5897/AJB11.2783
Kasahara K, Maeda K, Mikasa K et al (2005) Clonal dissemination of macrolide-resistant and penicillin-susceptible serotype 3 and penicillin-resistant Taiwan 19F–14 and 23F–15 Streptococcus pneumoniae isolates in Japan: a pilot surveillance study. J Clin Microbiol 43:1640–1645. https://doi.org/10.1128/JCM.43.4.1640-1645.2005
Kassiri H, Shahnaz K (2012) Cockroaches [periplaneta americana (L.), dictyoptera; blattidae] as carriers of bacterial pathogens, khorramshahr County Iran. Jundishapur J Microbiol 5:320–322
Kassiri H, Kassiri A, Kazemi S (2014) Investigation on American cockroaches medically important bacteria in Khorramshahr hospital, Iran. Asian Pac J Trop Dis 4:201–203. https://doi.org/10.1016/S2222-1808(14)60505-3
Kayansamruaj P, Pirarat N, Katagiri T et al (2014) Molecular characterization and virulence gene profiling of pathogenic Streptococcus agalactiae populations from tilapia (Oreochromis sp.) farms in Thailand. J Vet Diagn Investig 26:488–495. https://doi.org/10.1177/1040638714534237
Krzyaściak W, Pluskwa KK, Jurczak A, Koaścielniak D (2013) The pathogenicity of the Streptococcus genus. Eur J Clin Microbiol Infect Dis 32:1361–1376
Lemos AA, Lemos JA, Prado MA et al (2006) Cockroaches as carriers of fungi of medical importance. Mycoses 49:23–25. https://doi.org/10.1111/j.1439-0507.2005.01179.x
LeshanWannigama D, Dwivedi R, Zahraei-Ramazani A (2013) Prevalence and antibiotic resistance of gram-negative pathogenic bacteria species isolated from periplaneta americana and blattella germanica in Varanasi, India. J Arthropod Borne Dis 8:10–20
Li XX, Xiao SZ, Gu FF et al (2019) Serotype distribution, antimicrobial susceptibility, and multilocus sequencing type (MLST) of Streptococcus pneumoniae from adults of three hospitals in Shanghai. China Front Cell Infect Microbiol. https://doi.org/10.3389/fcimb.2019.00407
Lin K, Tierno PM Jr, Komisar A (2004) Increasing antibiotic resistance of streptococcus species in New York City. Laryngoscope 114:1147–1150. https://doi.org/10.1097/00005537-200407000-00003
Lopardo HA, Vidal P, Jeric P et al (2003) Six-month multicenter study on invasive infections due to group B streptococci in Argentina. J Clin Microbiol 41:4688–4694
Malhotra-Kumar S, Lammens C, Piessens J, Goossens H (2005) Multiplex PCR for simultaneous detection of macrolide and tetracycline resistance determinants in streptococci. Antimicrob Agents Chemother 49:4798–4800. https://doi.org/10.1128/AAC.49.11.4798-4800.2005
Manning SD, Ki M, Marrs CF et al (2006) The frequency of genes encoding three putative group B streptococcal virulence factors among invasive and colonizing isolates. BMC Infect Dis. https://doi.org/10.1186/1471-2334-6-116
Musher DM (1992) Infections caused by streptococcus pneumoniae: clinical spectrum, pathogenesis, immunity, and treatment. Clin Infect Dis 14:801–809. https://doi.org/10.1093/clinids/14.4.801
Naccache SN, Lustestica M, Fahit M et al (2018) One year in the life of a rapid syndromic panel for meningitis/encephalitis: a pediatric tertiary care facility’s experience. J Clin Microbiol. https://doi.org/10.1128/JCM.01940-17
NajafiMosleh M, Gharibi M, Alikhani MY et al (2014) Antimicrobial susceptibility and analysis of macrolide resistance genes in Streptococcus pneumoniae isolated in Hamadan. Iran J Basic Med Sci 17:595–599. https://doi.org/10.22038/ijbms.2014.3193
Pai H-H, Chen W-C, Peng C-F (2004) Cockroaches as potential vectors of nosocomial infections. Infect Control Hosp Epidemiol 25:979–984. https://doi.org/10.1086/502330
Paul S, Khan AM, Baqui MA, Muhibullah M (1992) Evaluation of the common cockroach Periplaneta americana (L.) as carrier of medically important bacteria. J Commun Dis 24:206–210
Persson E, Berg S, Bevanger L et al (2008) Characterization of invasive group B streptococci based on investigation of surface proteins and genes encoding surface proteins. Clin Microbiol Infect 14:66–73. https://doi.org/10.1111/j.1469-0691.2007.01877.x
Pomés A, Arruda LK (2014) Investigating cockroach allergens: aiming to improve diagnosis and treatment of cockroach allergic patients. Methods 66:75–85. https://doi.org/10.1016/j.ymeth.2013.07.036
Prado MA, Gir E, Pereira MS et al (2006) Profile of antimicrobial resistance of bacteria isolated from cockroaches (Periplaneta americana) in a Brazilian Health Care Institution. Braz J Infect Dis 10:26–32
Ranjbar R, Chehelgerdi M (2018) Genotyping and antibiotic resistance properties of helicobacter pylori strains isolated from human and animal gastric biopsies. Infect Drug Resist. https://doi.org/10.2147/IDR.S187885
Ranjbar R, Farsani FY, Dehkordi FS (2018) Phenotypic analysis of antibiotic resistance and genotypic study of the vacA, cagA, iceA, oipA and babA genotypes of the Helicobacter pylori strains isolated from raw milk. Antimicrob Res Infect Control 7:1–4
Ruppen C, Notter J, Strahm C et al (2018) Osteoarticular and skin and soft-tissue infections caused by Streptococcus agalactiae in elderly patients are frequently associated with bacteremia. Diagn Microbiol Infect Dis 90:55–57. https://doi.org/10.1016/j.diagmicrobio.2017.09.008
Sadeghifard N, Ranjbar R, Zaeimi J et al (2010) Antimicrobial susceptibility, plasmid profiles, and RAPD-PCR typing of Acinetobacter bacteria. Asian Biomed 4(6):901–911
Sadowy E, Matynia B, Hryniewicz W (2010) Population structure, virulence factors and resistance determinants of invasive, non-invasive and colonizing Streptococcus agalactiae in Poland. J Antimicrob Chemother 65:1907–1914. https://doi.org/10.1093/jac/dkq230
Salehzadeh A, Tavacol P, Mahjub H (2007) Bacterial, fungal and parasitic contamination of cockroaches in public hospitals of Hamadan. Iran J Vector Borne Dis 44:105–110
Sapkota AR, Ojo KK, Roberts MC, Schwab KJ (2006) Antibiotic resistance genes in multidrug-resistant Enterococcus spp. and Streptococcus spp. recovered from the indoor air of a large-scale swine-feeding operation. Lett Appl Microbiol 43:534–540. https://doi.org/10.1111/j.1472-765X.2006.01996.x
Stevens DL, Bryant AE (2016) Severe group a streptococcal infections. In: Ferretti JJ, Stevens DL, Fischetti VA (eds) Streptococcus pyogenes: Basic biology to clinical manifestations [Internet]. University of Oklahoma Health Sciences Center, Oklahoma City (OK), PMID: 26866227
Tetteh-Quarcoo PB, Donkor ES, Attah SK et al (2013) Microbial carriage of cockroaches at a tertiary care hospital in ghana. Environ Health Insights 7:59–66
Tunkel AR, Sepkowitz KA (2002) Infections caused by Viridans Streptococci in patients with neutropenia. Clin Infect Dis 34:1524–1529. https://doi.org/10.1086/340402
Udo EE, Boswihi SS, Al-Sweih N (2013) Genotypes and virulence genes in group B streptococcus isolated in the maternity hospital, Kuwait. Med Princ Pract 22:453–457. https://doi.org/10.1159/000349932
Xu X, Cai L, Xiao M et al (2010) Distribution of serotypes, genotypes, and resistance determinants among macrolide-resistant Streptococcus pneumoniae isolates. Antimicrob Agents Chemother 54:1152–1159. https://doi.org/10.1128/AAC.01268-09
Zeng X, Kong F, Wang H et al (2006) Simultaneous detection of nine antibiotic resistance-related genes in Streptococcus agalactiae using multiplex PCR and reverse line blot hybridization assay. Antimicrob Agents Chemother 50:204–209. https://doi.org/10.1128/AAC.50.1.204-209.2006
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Baqiyatallah Hospital, Tehran, Iran, for guidance and advice. The authors also gratefully acknowledge the Biotechnology Research Center, Shahrekord Branch, Islamic Azad University, Shahrekord in southwest Iran for their sincere support.
Funding
The authors declare that no funding was received for the research.
Author information
Authors and Affiliations
Contributions
RR and MC conceived and designed the study; MC conducted the research; MC performed the experiments. RR and MC analyzed the data. MC carried out the writing and drafting of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
This Research was approved in the Baqiyatallah University of Medical Sciences, Tehran, Iran (Project Ref Number 96-91002480). Verification of this research project and the licenses related to the sampling process were approved by Prof. Reza Ranjbar (Approval Ref Number Med-96-91002480).
Rights and permissions
About this article
Cite this article
Chehelgerdi, M., Ranjbar, R. Virulence factors and antibiotic resistance properties of Streptococcus species isolated from hospital cockroaches. 3 Biotech 11, 321 (2021). https://doi.org/10.1007/s13205-021-02874-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13205-021-02874-w