Abstract
The aim of this study was to determine the antimicrobial resistance characteristics of Listeria species isolated from foods and food processing environments, animal and human specimens in Iran. A systematic review of the papers published in Persian and English languages up to 20th May 2019 and indexed in the Scientific Information Database, PubMed, Scopus and Google Scholar databases using related keywords was conducted. Eligible articles were selected based on the predefined inclusion and exclusion criteria, followed by data extraction and meta-analysis using random-effects or fixed-effects models. A total of 27 articles were found reporting antibiotic resistance patterns of different Listeria species using disk diffusion method. Among Listeria species, Listeria monocytogenes resistance to commonly used antibiotics i.e. penicillin, ampicillin and gentamicin was as follows: 34.5%, 26.4%, 8.9% in isolates from foods and food processing environments, 47.1%, 29.5%, 9.2% in isolates from animal specimens and 56.8%, 29.5%, 32.4% in human strains, respectively. A high prevalence of L. monocytogenes strains resistant to penicillin, ampicillin and gentamicin was observed in Iran. Our findings suggested that trimethoprim/sulfamethoxazole, vancomycin and ciprofloxacin can be used as alternatives in the treatment of human listeriosis in Iran due to their low resistance rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The genus Listeria consists of β-hemolytic, non-spore-forming, motile (at 22–28 °C; tumbling motility), Gram-positive, facultative anaerobic rods which can be arranged as pairs or short chains (Carroll et al. 2016; Murray et al. 2015). Among 19 identified Listeria species, two species are considered as pathogens i.e. Listeria monocytogenes (L. monocytogenes) that regularly infects humans and Listeria ivanovii (L. ivanovii) that infects animals and rarely humans (Murray et al. 2015; Orsi and Wiedmann 2016). L. monocytogenes is a facultative intracellular food-borne pathogen that is widely found in nature and isolated from humans, wild and domestic animals, birds, insects, vegetation, water, food products and soil (Schuppler and Loessner 2010; Ramaswamy et al. 2007). Usually, the newborn (3.4 per 100,000), the elderly people (10 per 100,000), pregnant women (12 per 100,000) and patients with defects in cellular immunity are susceptible to Listeria infections which can be acquired via consumption of contaminated food products and mother to child transfer in utero or at birth (Murray et al. 2015; Olaimat et al. 2018). L. monocytogenes can cause neonatal diseases including early-onset listeriosis characterized by abortion, stillbirth, premature birth and high mortality rate which is acquired in utero. The pathogen can also cause late-onset listeriosis characterized by meningitis or meningoencephalitis with septicemia which is acquired 2–3 weeks after birth. The bacterium is also associated with a mild influenza-like illness and acute self-limited gastroenteritis in healthy adults, infections in pregnant women and meningitis in adults (Murray et al. 2015). In addition, the presence of Listeria species in food products is an important issue due to the consequent economic costs for the community in terms of consumer safety, and for the food industry (Ivanek et al. 2005). Hence, identification, control and treatment of Listeria infections are necessary. Combination regimens including a β-lactam alone or in combination with an aminoglycoside, i.e. either gentamicin with penicillin or gentamicin with ampicillin, are drugs of choice in the treatment of severe Listeria infections (Murray et al. 2015). Other antibiotics, such as trimethoprim-sulfamethoxazole, are successfully used to treat listeriosis but Listeria resistance to some of them has been reported, especially to fluoroquinolones, macrolides and tetracyclines (Murray et al. 2015; Olaimat et al. 2018). The prevalence of food-borne listeriosis varies between 0.1 and 11.3 cases per million persons in different countries with a mortality rate of ≤ 30% (Olaimat et al. 2018). In Iran, a systematic review and meta-analysis estimated the prevalence of L. monocytogenes to be 10%, 7% and 4% in humans, animals and food products, respectively (Ranjbar and Halaji 2018). However, no comprehensive information regarding antibiotic resistance of Listeria species in Iran has yet been presented. Therefore, the aim of this study was to determine the prevalence of antibiotic-resistant Listeria species, particularly L. monocytogenes, isolated from foods and food processing environments, animal and human specimens in Iran.
Methods
Search strategy
According to the PRISMA guidelines (Liberati et al. 2009), the current meta-analysis was conducted on the prevalence of Listeria species antibiotic resistance isolated from foods and food processing environments, animal and human specimens in Iran. For this purpose, a systematic literature search was done to find published articles until May 20, 2019 through international databases such as PubMed, Scopus and Google Scholar, as well as an Iranian national database i.e. the Scientific Information Database (SID) (https://www.sid.ir/En/Journal). We used three search terms including “antibiotic resistance”, “Listeria” and “Iran” in both Persian and English languages. Finally, reference lists of the included eligible articles were checked for additional studies which might have been missed during databases searching.
Selection criteria
Identification of articles evaluating Listeria species antibiotic resistance was performed using the related keywords by two investigators independently. Retrieved articles were transferred to the EndNote reference management software. At first, the titles and abstracts and then the full texts were assessed based on inclusion and exclusion criteria. Studies with the following criteria were included in the meta-analysis: cross-sectional studies published in English or Persian languages, which were limited to Iran, Listeria species samples collected from foods and food processing environments, animal and human origins, and studies presenting data on the prevalence of antibiotic resistance. Non-original articles, duplicate reports, research evaluating drug resistance profiles only at the genus Listeria level or with insufficient data or small sample size and also articles measuring antibiotic resistance Listeria species isolated from mixed and non-specified samples were excluded.
Quality assessment and data extraction
The Joanna Briggs Institute (JBI) critical appraisal checklist was used to assess the quality of eligible studies (Munn et al. 2015). As shown, the main data were extracted and organized into Table 1 including the name of the first author, study publication date, Listeria species type, samples origins, the frequency of Listeria species, methods used for assessing susceptibility to different antibiotics and number of resistance to each antibiotic of Listeria species.
Meta-analysis
The prevalence of Listeria species resistant to different antibiotics was estimated as percentage and 95% confidence intervals (CIs) through pooling the data using either random-effects model (when the heterogeneity was high among included studies) or fixed-effects model (when the heterogeneity was low). In this regard, heterogeneity was estimated using the I2 statistic and the Chi-square test with the Cochrane Q statistic (significant at I2 > 25% and p < 0.1). Asymmetry of funnel plots was explored as an indicator of potential publication bias. Meta-analysis was performed using the Comprehensive Meta-Analysis (CMA) software version 2.2 (Biostat, Englewood, NJ).
Results
Literature search and study characteristics
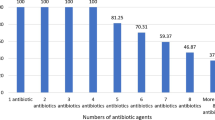
Of 1069 collected reports after searching in national and international databases, a total of 27 articles met predefined inclusion and exclusion criteria and were found to be eligible for the analysis of Listeria species antibiotic resistance (Fig. 1). Included studies were reported from Ahvaz, Bandar Torkaman, Chahar Mahal & Bakhtiyari, Isfahan, Karaj, Kurdistan, Lorestan, Marvdasht, Mashhad, Mazandaran, Shiraz, Tehran, Urmia and Yazd. As shown in Table 1, 20, 4 and 3 the research papers assessed antibiotic resistance profiles of Listeria species isolated from foods and food processing environments, human and animal origins, respectively. Food products as raw, ready-to-cook and ready-to-eat included seafood products, milk and traditional dairy products, processed meat, poultry products as well as market and processing environments which have been used for food products. Clinical specimens were collected from pregnant women with vaginitis (vaginal swab) and woman with spontaneous abortion (blood, urine, placental tissue, fecal and vaginal swabs). Also, animal specimens were obtained from ducks, geese, bovine, ovine, caprine, buffalo and camel species. L. monocytogenes was the most common Listeria species isolated from foods and food processing environments (57.9% samples), human (100% samples) and animal (86.2% samples) specimens.
Characteristics of Listeria species antibiotic resistance in Iran
All eligible studies used disk diffusion technique to determine antimicrobial susceptibility of Listeria species isolated in Iran. The results of antibiotic resistance according to the type of sample are shown in Table 2 for L. monocytogenes, L. ivanovii, L. innocua, L. seeligeri, L. grayi and L. welshimeri. As shown in Table 2, there is a heterogeneity among some studies in determining the prevalence of antibiotic resistance in Listeria species. In this case, random-effects model was used for pooling the data. Also, funnel plots were asymmetric suggesting potential publication bias in estimating the percentage of resistance for some antibiotics (Fig. 2).
Discussion
Listeria together with other pathogens including Campylobacter, Vibrio, Salmonella, Shigella, Escherichia, Yersinia, Staphylococcus, Clostridium and Bacillus are causative agent for more than 90% of food poisonings (Jalalpour 2012). It has been suggested that antibiotic therapy is necessary in severe cases of infection but drug resistance has increased among food-borne pathogens during the past few decades. Drug-resistant microbial species are a significant threat to public health, food security and treatment of diseases, and account for long-term hospitalization, increased mortality rates and enormous medical costs in the world (Olaimat et al. 2018; Jamali et al. 2014). One of the main food-borne microbes associated with major public health concern, especially in the food industry, is L. monocytogenes (Olaimat et al. 2018). In the present study, resistance rates of L. monocytogenes as well as other Listeria species in food products were high against some antibiotics (Table 1). Antibiotic resistance of food-borne L. monocytogenes pathogen may be either intrinsic or acquired due to genetic alterations or adaptation to environmental stresses including physical (e.g., heat and high pressure), chemical (e.g., acids and salts) and biological (e.g., microbial antagonism) stressors during food production and in the food processing environments (Olaimat et al. 2018; Lungu et al. 2011). Studies have also shown that factors such as the use of antimicrobial compounds in food preservation (via inducing efflux pumps), as well as sublethal exposure to disinfectants in food processing environments may contribute to the emergence of antibiotic-resistant food isolates of L. monocytogenes (Olaimat et al. 2018). Since L. monocytogenes is isolated from ubiquitous sources, the food chain can play an important role in transferring antibiotic resistant strains between animals and humans (Olaimat et al. 2018). In this study, antimicrobial resistance of L. monocytogenes isolated from human specimens against antibiotics used in primary therapy of Listeria infections i.e. penicillin, ampicillin and gentamicin was found to be 56.8%, 29.5% and 32.4% (Fig. 3), respectively. These prevalence rates are higher than the results of L. monocytogenes isolated from food (34.5%, 26.4% and 8.9%) and animal (47.1%, 29.5% and 9.2%) origin specimens. Frequent use of these antibiotics as the first-line drugs in listeriosis treatment as well as acquisition of resistance genes from the commensal unrelated bacterial species in foods and food processing environments through mobile genetic elements and efflux pumps can justify the high levels of L. monocytogenes resistance in human samples (Olaimat et al. 2018; Abdollahzadeh et al. 2016). Additionally, in penicillin-allergic individuals, vancomycin or trimethoprim/sulfamethoxazole are recommended for the treatment of invasive listeriosis (Abdollahzadeh et al. 2016). The prevalence of vancomycin- and trimethoprim/sulfamethoxazole-resistant L. monocytogenes isolated from different origins was as follow: 5.9% to trimethoprim/sulfamethoxazole and 5.8% to vancomycin in food specimens, 6.3% to trimethoprim/sulfamethoxazole in human specimens and 2.6% to vancomycin in animal specimens (Table 2). The antibiotic resistance of L. monocytogenes isolated from food products in different countries was as follows: 100% to penicillin, 4.8% to gentamicin, 57.1% to vancomycin and 4.8% to trimethoprim/sulfamethoxazole in India, 93.8% to penicillin, 3.1% to gentamicin, 46.8% to vancomycin and 6.3% to trimethoprim/sulfamethoxazole in Egypt, and 100% to penicillin, 7.8% to gentamicin, 45.1% to vancomycin and 11.7% to trimethoprim/sulfamethoxazole in Yemen (Obaidat et al. 2015). Another study from Turkey showed 66.7% resistance to penicillin, 75% to ampicillin, 8.3% to gentamicin, 0% to vancomycin and 50% to trimethoprim/sulfamethoxazole (Aras and Ardiç 2015). Also, Ha et al. in a study in South Korea indicated that ampicillin, gentamicin, vancomycin and trimethoprim/sulfamethoxazole resistance rates of L. monocytogenes isolated from food products were 97%, 0%, 0% and 0%, respectively, (Ha et al. 2017). On the other hand, it is necessary to monitor the extensive use of antibiotics as supplements to enhance the growth or prevent, control and treat diseases in animals or as pesticide on fruits, and also use of sub-inhibitory concentrations of antibiotics in human diseases treatment which can lead to the emergence of the antibiotic resistance and effect on human infection therapy (Olaimat et al. 2018). It is worth noting that tetracycline is frequently used for treating animal infections in Iran (Akrami-Mohajeri et al. 2018). This drug is also used in treating human infections (Olaimat et al. 2018). Our results indicated that L. monocytogenes strains isolated from food products (40.5%), animal (69.5%) and human (18.3%) samples exhibited a high resistance rate to tetracycline. Similar results were observed for other Listeria species (Table 2). However, 3% and 6% of L. monocytogenes isolates from food products in Italy and Canada were resistant to tetracycline, respectively (Abdollahzadeh et al. 2016). In pregnant women, erythromycin is an antibiotic of choice to treat listeriosis (Olaimat et al. 2018). However, the current study showed that 26.8% of human isolates of L. monocytogenes were resistant to erythromycin. Other antibiotics used to treat listeriosis are rifampicin, chloramphenicol and fluoroquinolones (Olaimat et al. 2018). Among them, chloramphenicol-resistant L. monocytogenes strains isolated from food (17.7%), animal (27.8%) and human (23.3%) origins and ciprofloxacin-resistant L. monocytogenes strains isolated from food origin (25.4%) showed high resistance rates. However, rifampin-resistant L. monocytogenes strains isolated from food (5.4%) and animal (2.6%) origins had low resistance rates. In addition to the pathogen source, other species of the genus Listeria can affect the emergence of L. monocytogenes antibiotic resistance in through genetic material exchange (Allen et al. 2016). Therefore, investigation of the antibiotic resistance of other Listeria species is also important. Our study showed that resistance of Listeria species isolated from foods and food processing environments and animal sources in Iran was high to some antibiotics (Table 2).
Conclusion
The present systematic review and meta-analysis warns about the emergence of Listeria species resistant to different antibiotics in different pathogen sources in Iran. For example, a high prevalence of L. monocytogenes strains resistant to commonly used antibiotics in treating human listeriosis i.e. penicillin, ampicillin and gentamicin was observed in Iran. In addition, other species of the genus Listeria indicated high resistance rates to some antibiotics. Therefore, to reduce the spread of Listeria drug resistance in Iran, excessive use of antibiotics either in the treatment of human infections or in animal feeding as growth supplements and prophylaxis should be controlled and limited. Nonetheless, our findings suggest that trimethoprim/sulfamethoxazole, vancomycin and ciprofloxacin can be alterative antibiotics, due to their low resistance rates, in the treatment of human listeriosis in Iran. Finally, we recommend evaluating mechanisms of antibiotic resistance in Listeria species, especially L. monocytogenes in Iran.
References
Abbasinejad B, Neyriz-Nagadehi M, Taher Talatappeh N (2015) Prevalence and antimicrobial susceptibility of Listeria monocytogenes in Koozeh cheeses of Urmia retails. J Food Hyg 5:27–34 (in Persian)
Abdollahzadeh E, Ojagh SM, Hosseini H, Ghaemi EA, Irajian G, Heidarlo MN (2016) Antimicrobial resistance of Listeria monocytogenes isolated from seafood and humans in Iran. Microb Pathog 100:70–74
Akrami-Mohajeri F, Derakhshan Z, Ferrante M, Hamidiyan N, Soleymani M, Conti GO, Tafti RD (2018) The prevalence and antimicrobial resistance of Listeria spp in raw milk and traditional dairy products delivered in Yazd, central Iran (2016). Food Chem Toxicol 114:141–144
Allen KJ, Wałecka-Zacharska E, Chen JC, Katarzyna KP, Devlieghere F, Van Meervenne E, Osek J, Wieczorek K, Bania J (2016) Listeria monocytogenes—an examination of food chain factors potentially contributing to antimicrobial resistance. Food Microbiol 54:178–189
Aras Z, Ardıç M (2015) Occurrence and antibiotic susceptibility of Listeria species in turkey meats. Korean J Food Sci Anim Resour 35:669–673
Babazadeh Naseri A, Soltan Dallal MM (2019) Frequency, antimicrobial susceptibility and serotyping of Listeria monocytogenes isolated from food samples in Tehran, Iran. J Gorgan Univ Med Sci 21:101–107 (in Persian)
Bahador A, Sadeghi Kalani B, Valian F, Irajian G, Lotfollahi L (2015) Phenotypic and genotypic characteristics of Listeria monocytogenes isolated from dairy and meat products. Avicenna J Clin Microb Infect 2:e26905
Carroll KC, Butel JS, Morse SA (2016) Jawetz Melnick & Adelbergs medical microbiology, 27th edn. McGraw Hill Professional, Philadelphia, pp 196–198
Dehkordi FS, Barati S, Momtaz H, Ahari SN, Dehkordi SN (2013) Comparison of shedding, and antibiotic resistance properties of Listeria monocytogenes isolated from milk, feces, urine, and vaginal secretion of bovine, ovine, caprine, buffalo, and camel species in Iran. Jundishapur J Microbiol 6:284–294
Fallah AA, Saei-Dehkordi SS, Rahnama M, Tahmasby H, Mahzounieh M (2012) Prevalence and antimicrobial resistance patterns of Listeria species isolated from poultry products marketed in Iran. Food Control 28:327–332
Fallah AA, Saei-Dehkordi SS, Mahzounieh M (2013) Occurrence and antibiotic resistance profiles of Listeria monocytogenes isolated from seafood products and market and processing environments in Iran. Food Control 34:630–636
Ha JH, Lee MK, Cho YS (2017) Antimicrobial susceptibility and serotyping of Listeria monocytogenes isolated from ready-to-eat seafood and food processing environments in Korea. Food Sci Biotechnol 26:287–291
Heidarzadeh S, Dallal MM, Pourmand MR, Pirjani R, Foroushani AR, Noori M, Naseri AB (2018) Prevalence, antimicrobial susceptibility, serotyping and virulence genes screening of Listeria monocytogenes strains at a tertiary care hospital in Tehran, Iran. Iran J Microbiol 10:307–313
Ivanek R, Gröhn YT, Tauer LW, Wiedmann M (2005) The cost and benefit of Listeria monocytogenes food safety measures. Crit Rev Food Sci Nutr 44:513–523
Jalalpour S (2012) Food borne diseases bacteria; frequency antibiotic resistance bacteria in Iranian foods. Afr J Microbiol Res 6:719–723
Jamali H, Radmehr B (2013) Frequency, virulence genes and antimicrobial resistance of Listeria spp. isolated from bovine clinical mastitis. Vet J 198:541–542
Jamali H, Radmehr B, Thong KL (2013) Prevalence, characterisation, and antimicrobial resistance of Listeria species and Listeria monocytogenes isolates from raw milk in farm bulk tanks. Food Control 34:121–125
Jamali H, Radmehr B, Ismail S (2014) Prevalence and antimicrobial resistance of Listeria, Salmonella, and Yersinia species isolates in ducks and geese. Poult Sci 93:1023–1030
Jamali H, Paydar M, Ismail S, Looi CY, Wong WF, Radmehr B, Abedini A (2015) Prevalence, antimicrobial susceptibility and virulotyping of Listeria species and Listeria monocytogenes isolated from open-air fish markets. BMC Microbiol 15:144
Kalani BS, Pournajaf A, Sedighi M, Bahador A, Irajian G, Valian F (2015) Genotypic characterization, invasion index and antimicrobial resistance pattern in Listeria monocytogenes strains isolated from clinical samples. J Acute Dis 4:141–146
Kargar M, Ghasemi A (2011) A survey on prevalence rate and antibiotic resistance of Listeria monocytogenes in fresh cheese of marvdasht, (2007). J Food Technol Nutr 8:72–77 (in Persian)
Khalili Borujeni F, Moshtaghi H, Bonyadian M (2013) Study on contamination of sheep meat in Shahrekord area with Listeria ivanovii and determination its antibiotic resistance pattern. Iran J Med Microbiol 7:15–21 (in Persian)
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Lotfollahi L, Nowrouzi J, Irajian G, Masjedian F, Kazemi B, Falahat LE, Ramez M (2011) Prevalence and antimicrobial resistance profiles of Listeria monocytogenes in spontaneous abortions in humans. Afr J Microbiol Res 5:1990–1993
Lungu B, O’Bryan CA, Muthaiyan A, Milillo SR, Johnson MG, Crandall PG, Ricke SC (2011) Listeria monocytogenes: antibiotic resistance in food production. Foodborne Pathog Dis 8:569–578
Maktabi S, Pourmehdi M, Zarei M, Fooladgar AA (2016) Detection of antibiotic resistant Listeria spp. in beef burgers distributed in Ahvaz city, Iran. Jundishapur J Health Sci 8:e34780
Mojtahedi A, Tarrahi MJ, Sepahvand A, Khakpour AD, Radsari E, Ttavasoli M et al (2004) Frequency determination of Listeria contamination in dairy products and their antibiotic resistance pattern, department for controlling food stuffs, Lorestan. Yafte 6:27–32 (in Persian)
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C (2015) Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int J Evid Based Healthc 13:147–153
Murray PR, Rosenthal KS, Pfaller MA (2015) Medical microbiology, 8th edn. Elsevier Health Sciences, London, pp 210–213
Obaidat MM, Bani Salman AE, Lafi SQ, Al-Abboodi AR (2015) Characterization of Listeria monocytogenes from three countries and antibiotic resistance differences among countries and Listeria monocytogenes serogroups. Lett Appl Microbiol 60:609–614
Olaimat AN, Al-Holy MA, Shahbaz HM, Al-Nabulsi AA, Abu Ghoush MH, Osaili TM, Ayyash MM, Holley RA (2018) Emergence of antibiotic resistance in Listeria monocytogenes isolated from food products: a comprehensive review. Compr Rev Food Sci Food Saf 17:1277–1292
Orsi RH, Wiedmann M (2016) Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol 100:5273–5287
Rahimi E, Ameri M, Momtaz H (2010) Prevalence and antimicrobial resistance of Listeria species isolated from milk and dairy products in Iran. Food Control 21:1448–1452
Rahimi E, Yazdi F, Farzinezhadizadeh H (2012a) Prevalence and antimicrobial resistance of Listeria species isolated from different types of raw meat in Iran. J Food Prot 75:2223–2227
Rahimi E, Momtaz H, Sharifzadeh A, Behzadnia A, Ashtari MS, Esfahani SZ, Riahi M, Momeni M (2012b) Prevalence and antimicrobial resistance of Listeria species isolated from traditional dairy products in Chahar Mahal & Bakhtiyari, Iran. Bulg J Vet Med 15:115–122
Rahimi E, Jahanmard MJ, Sohrab Safari S, Ansari M, Torki Baghbadorani Z (2017) Prevalence and antimicrobial resistance of Listeria species isolated from filleted Argyrosomus hololepidotus, Scomberomorus commerson and Alburnus spp. J Food Microbiol 3:1–9 (in Persian)
Ramaswamy V, Cresence VM, Rejitha JS, Lekshmi MU, Dharsana KS, Prasad SP, Vijila HM (2007) Listeria-review of epidemiology and pathogenesis. J Microbiol Immunol Infect 40:4–13
Ranjbar R, Halaji M (2018) Epidemiology of Listeria monocytogenes prevalence in foods, animals and human origin from Iran: a systematic review and meta-analysis. BMC Public Health 18:1057
Rezai R, Ahmadi E, Salimi B (2018) Prevalence and antimicrobial resistance profile of Listeria species isolated from farmed and on-sale rainbow trout (Oncorhynchus mykiss) in Western Iran. J Food Prot 81:886–891
Rostami F, Shaygannia Sh, Madahi H, Rahimi E, Jalali M, Safarpoor Dehkordi F (2015) Prevalence and antimicrobial resistance of isolated Listeria spp. from nugget chicken in Isfahan province, Iran. JFST 7:97–103 (in Persian)
Schuppler M, Loessner MJ (2010) The opportunistic pathogen Listeria monocytogenes: pathogenicity and interaction with the mucosal immune system. Int J Inflam 2010:1–12
Soleymani Najaf Ababdi M, Hamidian N, Heydari A, Ehrampoush M, Fallahzade H, Safari F et al (2017) Prevalence and antimicrobial resistance of Listeria monocytogenes poultry meat and poultry slaughterhouse environment, Yazd, Iran (1394). J Toloo e Behdasht 16:61–72 (in Persian)
Zeinali T, Jamshidi A, Rad M, Bassami M (2017) Analysis of antibiotic susceptibility profile and RAPD typing of Listeria monocytogenes isolates. J Health Sci Technol 1:11–16
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khademi, F., Sahebkar, A. A systematic review and meta-analysis on the prevalence of antibiotic-resistant Listeria species in food, animal and human specimens in Iran. J Food Sci Technol 56, 5167–5183 (2019). https://doi.org/10.1007/s13197-019-04040-w
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13197-019-04040-w