Abstract
Head and neck squamous cell carcinomas (HNSCC) have proven to be inherently resistant to systemic treatments as a result of histological, molecular, and etiological heterogeneity, with limited responses seen after second-line therapy and beyond. With limited treatment options after progression on systemic chemotherapy in HNSCCs, immunotherapy has a role to play with improved results. In this prospective, observational, non-randomized, open-label study, a total of 12 patients with advanced, relapsed, or metastatic HNSCC received Inj. Nivolumab weight-based dose of 3 mg per kg, intravenously every 2 weeks along with low-dose capecitabine 500 mg twice a day, was prospectively assessed. The patient’s clinical, hematological, and staging characteristics were described and the clinical benefit rate (CBR) was calculated. A total of 12 patients received the combined metronomic chemo-immunotherapy (CMCI). The majority of patients were belonging to ECOG-PS 1(66%), with all patients being in stage IV disease. Six, four, and two patients received immunotherapy as the 5th, 3rd, and 4th line of therapy, respectively. Nivolumab and low-dose capecitabine were used in all 12 patients. CBR was seen in 66% (8/12) of patients, one patient died due to hepatitis and hepatic encephalopathy, another patient died due to pneumonia and respiratory complications, two patients had progressive disease, and two patients with stable disease discontinued treatment because of financial constraints and kept on capecitabine alone. The majority tolerated therapy well with no grade 3/4 immune-related adverse events (IRAEs). Two patients required supportive therapy with packed red cell transfusion and albumin infusions. Six-month overall survival (OS) and progression-free survival (PFS) in the study population were 83.3% and 66.6%, respectively. In conclusion, nivolumab along with metronomic chemotherapy with low-dose capecitabine was very well tolerated and exhibited anti-tumor activity with a CBR of 66%, 6-month OS of 83.3%, and 6-month PFS of 66.6%, in extensively pretreated patients with HNSCCs. Additional studies of nivolumab and metronomic chemotherapy and immuno-immuno combination therapy in these diseases are ongoing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck squamous cell carcinoma (HNSCC) is one of the most common malignancies worldwide, accounting for more than 550,000 new cases and 380,000 deaths per year [1]. Besides established risk factors like smoking and alcohol consumption, human papillomavirus (HPV) infection has become an important factor in the epidemiology and prognosis of patients [2]. Most of the patients have locally advanced disease at the time of presentation and require a multimodal approach for treatment with surgery, radiotherapy, and systemic therapy. Despite this, more than half of the patient’s relapse. Expected median survival for a patient with incurable, locally advanced, recurrent, or metastatic remains under a year, or marginally longer for patients who develop metastases from an HPV-related HNSCC [3]. The addition of an EGFR-targeting monoclonal antibody has been shown to improve overall survival compared with platinum-based chemotherapy alone by 2.7 months [4].
There has been great momentum in the field of immuno-oncology after the Nobel Laureates, James P Allison, and Dr. Tasuku Honjo published pioneering work proving that, besides antigen presentation, a second co-stimulatory signal is essential to activate cytotoxic T cells to provide anti-tumor immunity [5]. With this improved understanding, the spectrum of immunotherapeutic options has increased beyond melanoma/renal cell carcinoma to include head and neck, lung, bladder, hepatocellular, and gastrointestinal malignancies. Drugs that block the immune regulatory checkpoints namely the PD-1/PDL1 (nivolumab, pembrolizumab, and atezolizumab) have shown tremendous responses [6,7,8]. Western data have a response rate of 15–40% and some cases with durable responses [9]. Although early clinical immunotherapy trials have yielded mixed results with ambiguous clinical benefits, cancer immunotherapy is nowadays regarded as an important pillar of anticancer treatment [10].
Metronomic chemotherapy, defined as the frequent administration of chemotherapeutic agents at a non-toxic dose without extended rest periods, was originally designed to overcome drug resistance by shifting the therapeutic target from tumor cells to tumor endothelial cells. Metronomic chemotherapy also exerts anti-tumor effects on the immune system (immunomodulation) and tumor cells. The goal of immunotherapy is to enhance host anti-tumor immunities. Metronomic chemotherapy decreases angiogenesis, decreases therapeutic resistance, and targets cancer stem cells and anti-tumor immunity. In this era of immunotherapy, combining immune checkpoint inhibition with metronomic administration of chemotherapeutic drugs may create a synergistic effect that augments anti-tumor immune responses and clears metabolic competition. This would allow immune-mediated elimination of therapy-resistant cancer cells, an effect that may be unattainable by using either therapeutic modality alone [11, 12]. In this research study, we evaluated the role of combined metronomic low-dose oral capecitabine along with the immunotherapeutic agent nivolumab.
Material and Methods
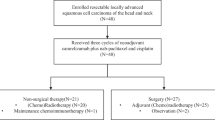
This study was conducted in a prospective observational manner in a tertiary care center at the Department of Medical and Pediatric Oncology over 4 years from June 2018 to May 2022. The study was approved by the Institutional Ethics Committee of our institute. Written informed consent was obtained from the patients or the parent/ guardian for publication of the clinical details in this report. In this prospective, observational, non-randomized, open-label study, all consecutive patients with relapse, recurrent, locally advanced, and metastatic HNSCC who received weight-based Inj. Nivolumab along with low-dose oral capecitabine, after the failure of a minimum of two lines of chemotherapy at our center, were enrolled prospectively. A total of 12 cases met the inclusion criteria for enrolment in the study group. Diagnosis of HNSCC was made by histopathology, fine needle aspiration cytology, and imaging studies.
Aims and Objectives of the Study
Aims
The primary aim of this study is to know the response rate of combined metronomic low-dose capecitabine along with Inj. Nivolumab in advanced HNSCC patients who have received a minimum of two lines of chemotherapy.
Objectives
The objectives of this study are to calculate the clinical benefit rate and study the side effect profile, need for component support, and other supportive measures required in this study.
Endpoints
Primary endpoints are progression-free survival (PFS) and event-free survival (EFS).
Secondary endpoints of this study are to calculate the clinical benefit rate and overall survival.
Patient Selection and Treatment
Patients, with relapse, recurrent, locally advanced, and metastatic HNSCC who received ICIs along with low-dose oral capecitabine, after the failure of a minimum of two lines of chemotherapy at our center were prospectively assessed. Patient data was collected and entered in the Microsoft Excel sheet and analyzed for efficacy, side effects, and need for supportive care for the patients who were taking ICI nivolumab along with low-dose oral capecitabine. Patients receiving < 4 weeks of treatment were excluded from the study.
Inclusion Criteria
All the patients who are willing to give informed consent, with relapse, recurrent, locally advanced, and metastatic HNSCC who present, after the failure of a minimum of two lines of chemotherapy and or not willing for further injectable chemotherapy at our center were prospectively assessed.
Exclusion Criteria
-
1.
Patients who are not willing to give consent for enrolment in the study
-
2.
Patients with altered RFT and/or LFT
-
3.
ECOG performance status (PS) 4
-
4.
Newly diagnosed HNSCC patients or those who have not received at least two lines of chemotherapy
-
5.
Patients receiving < 4 weeks of treatment
Intervention
All the enrolled patients received weight-based Inj. Nivolumab infusion at a dose of 3 mg/kg every 2 weeks along with continuous oral low-dose metronomic capecitabine at 500 mg twice a day schedule [13, 14] after discussing with the patients and their family members regarding the benefits and pitfalls of the therapy.
Follow-up and Monitoring
All the patients were monitored with history and physical examination, complete blood counts, renal function tests, and liver function tests on the first day of every cycle. All the patients were monitored for the common toxicities associated with nivolumab and capecitabine according to the Common Toxicity Criteria for Adverse Events (CTCAE) criteria.
Response Assessment
All the patients were monitored with a computed tomography (CT) scan for response assessment for their disease status at an interval of every 3 months of therapy using imRECIST (Immune-modified Response Criteria in Solid Tumours) based on the NCCN and ESMO Guidelines. According to the imaging reports, patients were stratified as partial responders (PR), complete response (CR), stable disease (SD), or progressive disease (PD) as per the RECIST 1.1 criteria.
Therapy was continued until progression or unacceptable toxicity.
Statistical Analysis
Clinical benefit (CBR) was defined as the proportion of patients without clinical or radiological progression at 3 months. Progression-free survival (PFS)/event-free survival (EFS) was defined as the period from the start of combined metronomic chemo-immunotherapy to the date of clinical or radiological progression of disease or death due to any cause. Data analysis and data entry were done using MS Office 2010. Disease evaluation was done with computed tomography (CT). According to the imaging reports, patients were stratified as partial responders (PR), complete response (CR), stable disease (SD), or progressive disease (PD) as per the RECIST 1.1 criteria.
Results (Table 1)
This prospective observational study was conducted in a tertiary care center, situated in the northern part of Karnataka, India. From June 2018 to May 2022, a total of 12 patients who are willing to give informed consent, with relapse, recurrent, locally advanced, and metastatic HNSCC who present, after the failure of a minimum of two lines of chemotherapy and or not willing for further injectable chemotherapy at our center were enrolled. Diagnosis was done with clinical signs, symptoms, imaging, histopathological, and FNAC studies. These 12 patients constituted the study cohort. All 12 patients had a history of prior treatment like surgery, chemotherapy, and radiotherapy as per the local and national standard treatment guidelines, followed by first-line chemotherapy at a recurrence of the disease. All the patients initially have some response followed by progression. At progression on first-line chemotherapy, those with good performance status were given second-line chemotherapy. Those who progressed on second-line chemotherapy were counseled thoroughly regarding disease status, prognosis, treatment options available, the option of best supportive care, and clinical trial enrolment. Those who were not willing to best supportive care or further injectable chemotherapy were given the option of low-dose metronomic continuous oral capecitabine along with injection nivolumab at 3 mg per Kg, as per our study protocol.
After explaining the side effects, benefits, and cost of low-dose metronomic continuous oral capecitabine and Inj, nivolumab along with supportive management and high-risk consent was taken for the study enrolment from the patient and their relatives. Baseline investigations like complete blood counts, renal function tests, electrolytes, and liver function tests were within the normal range for their respective ages and sex.
A total of 12 HNSCC cancer patients met the inclusion criteria and received combined metronomic chemo-immunotherapy at the prescribed schedule. Out of 12 patients, 4 were carcinoma tongue, two cases each of Carcinoma of Buccal Mucosa, Carcinoma of the Oropharynx, Carcinoma of the Hypopharynx, and Carcinoma of Cricopharynx. HPV testing by P16 immunochemistry has been done in both the oropharyngeal cancer patients and both were negative; due to lower positivity rates in other subsites, we did not subject other patients to the P16 immunohistochemistry. None of the patients was subjected to PD-L1 testing as it is not a required criterion for the nivolumab therapy. Sixty-six percent of patients were in ECOG-PS = 1, 33% were in ECOG-PS = 2, 66% patients had metastatic disease, and 33% were having recurrent, locally advanced disease at the time of starting of CMCI. All the patients had cervical lymphadenopathy and all had squamous cell histology.
All patients had to have a history of pre-treatment with surgery, concurrent chemoradiotherapy, and combination chemotherapy. Most of the patients received prior drugs in the form of combination chemotherapy, like paclitaxel-carboplatin, paclitaxel-cisplatin, docetaxel-carboplatin, docetaxel-cisplatin, gemcitabine-carboplatin, nab-paclitaxel-carboplatin; single agents, like cisplatin, gemcitabine, and irinotecan; and pemetrexed and metronomic chemotherapy drugs, like cyclophosphamide, celecoxib, and methotrexate in the study group (Table 2). We have not used infusional 5-FU-based combination regimens like PF, TPF, and DCF, given higher toxicity like mucositis and neutropenia. Out of 12 patients, 6 (50%) were receiving as 5th line, 4 (33%) were receiving as 3rd line, and 2 (16.5%) as 4th line of CMCI therapy. The mean number of cycles of weight-based nivolumab therapy received by the study population was 6.33 (6 ± 1). At the end of 6 months of regular treatment, six patients (50%) had partial response (PR), 2 (16.5%) patients had stable disease (SD), and 2 (16.5%) patients had progressive disease (PD) (Fig. 1). CBR that is a combination of PR and SD was seen in 66% (8/12) patients. None of the patients had a complete response (CR). Two patients with stable disease discontinued treatment because of financial constraints and kept on capecitabine alone. At the end of the 6 months, 83.3% were surviving (Fig. 2) and 66.6% were free from the progression of the disease. Fatigue was seen in 66% of patients, 33% of patients had anemia, 2 patients required blood and albumin transfusion, 1 patient had hepatitis, and 1 patient had pneumonia. Two patients developed IRAEs out of these 2, one patient died due to hepatitis and hepatic encephalopathy, and another patient died due to pneumonia and respiratory complications. None of the patients developed capecitabine-related side effects, because we used low-dose oral metronomic capecitabine of 500 mg twice a day as compared to the standard dose of 1.25 mg per m2. At the end of the 6 months, 66% of the patients were surviving.
Discussion
The 5-year prognosis in HNSCC remains around 50% at 5 years and median overall survival (OS) in RM-HNSCC is less than 11 months [15]. The realization of long-term durable responses in a subset of patients represents a transformative event. Since the 2011 FDA approval of ipilimumab (anti-CTLA4) for the treatment of metastatic melanoma, 5 additional checkpoint blockade therapies, all targeting the PD-1/PD-L1 axis, have been approved for the treatment of a broad range of tumor types. Immune checkpoint blockade removes inhibitory signals of T cell activation, which enables tumor-reactive T cells to overcome regulatory mechanisms and mount an effective anti-tumor response [16, 17]. Nivolumab (anti PD-1), an FDA-approved immunotherapeutic agent used in our study, has shown promising responses according to Western data [6,7,8, 18, 19]. This distinct mechanism of action has translated into clinical efficacy; impressive results have been seen in large international trials of metastatic solid tumors, initially in the relapsed setting and now, increasingly, in the frontline [20,21,22,23,24,25]. Although these drugs have durable responses, their utilization in the Indian setting is a challenge as they are very expensive and there is limited data in the Indian scenario. The cost and financial limitations of cancer care in the Indian population cannot be overstated [26].
Metronomic chemotherapy (MCT) also known as “multi-targeted therapy” involves repeated administration of conventional anti-neoplastic agents at very low doses (1/10th–1/3rd of the maximum tolerated dose [MTD]) without a long drug-free period with minimal or no adverse effects and a rare chance of developing acquired drug resistance. The scientific basis for MCT is that in conventional chemotherapy, the vascular endothelial cell death effect cannot be sustained because endothelial cells get a chance to recover during treatment breaks and this may be overcome by frequent administration of chemotherapy drugs at doses below the MTD and with no prolonged drug-free break, thus achieving a sustained low blood level of the drug without significant toxic side-effects [27, 28]. Metronomic chemotherapy also exerts anti-tumor effects on the immune system (immunomodulation) and tumor cells. The goal of immunotherapy is to enhance host anti-tumor immunities.
Inhibitory immune checkpoint receptors (CTLA-4, PD-1, and PD-L1) were increased in TILs. PD-L1 expression in HNSCC was described in 66 to 87% of HNSCC primary tumors [19]. So far, the only fully published randomized phase III trial (Checkmate 141) compared nivolumab with standard-of-care therapy in patients with recurrent/metastatic HNSCC refractory to platinum therapy. Survival rates after 1 year were more than doubled with nivolumab (16.6 vs 36%) [18, 29].
Various chemotherapeutic agents are utilized to achieve adequate locoregional control. Cisplatin, fluorouracil (FU), and taxanes are often used to treat HNC but these regimens have shown high toxicity and poor patient compliance. Capecitabine is an orally administered prodrug that is preferentially converted to FU in tumor cells in comparison to normal cells, by exploiting the higher thymidine phosphorylase activity in tumoral tissue. Various phase II trials conducted on capecitabine in the management of recurrent HNC have shown comparable results and tolerable toxic effects, especially in pre-treated fragile patients. Capecitabine, used in induction or concurrent settings in the radical management of locoregionally advanced HNC, has also shown promising results. Oral capecitabine administration offers an alternative to the more inconvenient, i.v., administration of 5FU and seems to be an active, feasible, and well-tolerated mode of palliative treatment for advanced HNSCC patients who have previously received platinum-based treatment schedules. Given all these characteristics, this treatment may be considered a suitable therapeutic alternative in a palliative setting [30, 31].
Paradoxically, many of the chemotherapeutic compounds tend to become essential to promote the activity of immunotherapy and to offer a sustained therapeutic effect. The major cytotoxic drugs—carboplatin, cisplatin, cytarabine, dacarbazine, docetaxel, doxorubicin, ecteinascidin, etoposide, fluorouracil, capecitabine, gemcitabine, irinotecan, oxaliplatin, paclitaxel, and pemetrexed—all can up-regulate PD-L1 expression on cancer cells (via the generation of danger signals) and promote anti-tumor immunogenicity, via activation of cytotoxic T lymphocytes, maturation of antigen-presenting cells, depletion of immunosuppressive regulatory T cells, and/or expansion of myeloid-derived suppressor cells. The use of “immunocompatible” cytotoxic drugs combined with anti-PD-(L)1 antibody is a modern approach, not only for increasing the direct killing of cancer cells but also as a strategy to minimize the activation of immunosuppressive and cancer cell pro-survival program responses [11].
Repeated cycle treatment with 5-FU or capecitabine tends to repress the anti-tumor immune functions and elevate the expression of PD-L1 on tumor cells. The drug initially promotes proliferation and cytotoxicity of tumor-infiltrating CD8+ T cells after one cycle of treatment, but after repeated cycles, the anti-tumor immune functions get impaired, with the release of immune-suppressive factors such as transforming growth factor beta and interleukin 10 (IL-10). This trend could diminish the anti-tumor efficacy of the chemotherapy. 5-FU up regulates PD-L1 and this early induction of PD-L1 expression is beneficial when combining the drug with an anti-PD-L1 antibody. The combined treatment of 5-FU + an anti-PD-L1 mAb displays a greater efficacy compared to 5-FU or immunotherapy alone [32, 33].
Rationale
Most of the cancer patients in developing countries present to us with stage IV disease. Metronomic chemotherapy decreases angiogenesis, decreases therapeutic resistance, and targets cancer stem cells and anti-tumor immunity. In this era of immunotherapy, combining immune checkpoint inhibition with metronomic administration of chemotherapeutic drugs may create a synergistic effect that augments anti-tumor immune responses and clears metabolic competition. This would allow immune-mediated elimination of therapy-resistant cancer cells, an effect that may be unattainable by using either therapeutic modality alone [34].
Background
Therapeutic resistance remains a major obstacle in treating many cancers, particularly in advanced stages. Cytotoxic lymphocytes (CTLs) likely have the potential to eliminate therapy-resistant cancer cells. However, their effectiveness may be limited either by the immunosuppressive tumor microenvironment or by immune cell death induced by cytotoxic treatments. High-frequency low-dose (also known as metronomic) chemotherapy can help improve the activity of CTLs by providing sufficient stimulation for cytotoxic immune cells without excessive depletion. Additionally, therapy-induced removal of tumor cells that compete for shared nutrients may also facilitate tumor infiltration by CTLs, further improving prognosis. Metronomic chemotherapy can also decrease the number of immunosuppressive cells in the tumor microenvironment, including regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs). When beneficial, metronomic therapy seems to be associated with the normalization of the tumor microenvironment including improvements in tumor perfusion, tissue oxygenation, and drug delivery as well as activation of the immune system. Immune checkpoint inhibition can further augment anti-tumor immune responses by maintaining T cells in an activated state [35,36,37,38].
The significance of this study is based on the mechanisms of action of both metronomic chemotherapy and immune checkpoint inhibitors; one can surmise that a combination of the two therapeutic approaches would have a synergistic effect for the following reasons [33,34,35].
-
1.
Both immune checkpoint inhibitors and metronomic chemotherapy increase immune cell activation. While metronomic chemotherapy can promote tumor-specific immune activation, concurrent administration of immune checkpoint inhibitors would maintain the activated state of T cells.
-
2.
Administration of metronomic chemotherapy would allow competition for nutrients between tumor and immune cells to be reduced via gradual removal of tumor cells. This would facilitate tumor infiltration by cytotoxic immune cells, which has been associated with improved clinical outcomes.
-
3.
Experimental evidence has shown that blocking PD-L1 directly on tumors dampens glycolysis, giving cytotoxic lymphocytes an additional competitive advantage.
Drawbacks of the Study
-
1.
As data on this type of study is very scarce, we did not get many of the studies based on our study protocol and most of the study cohort patients were in the end stage of their life and had received multiple lines of chemotherapy before the enrolment in the study, so we have stressed more on the basic information about the tumor microenvironment (TME) and mechanisms involved in inhibition of angiogenesis, tumor resistance, and the effect of immunotherapeutic drugs and metronomic chemotherapy drug combinations at immune cells and TME level.
-
2.
Ideally, PDL1 testing should be done, even though the FDA approval of nivolumab is irrespective of PDL1 status, but we have not done PDL1 because it is not mandatory for nivolumab therapy and most of the patients were at the end stage of best supportive care life and we just started the therapy of less toxic regimen like CMCI after proper counseling and consent, as we were not aware of the exact results and benefits as we do not have any data on this type of therapy.
-
3.
Two deaths in a study population of 12 is a significant percentage, but in this study, the majority of patients were having stage IV and very advanced disease. Six, four, and two patients received CMCI as the 5th, 3rd, and 4th line of therapy. We cannot recommend based on this small study and will wait for more studies and data to come up with a good number of patients, and at this point of time, what we could think of is a less toxic regimen like CMCI as most of the patients were at the end stage of their life due to advanced stage of the disease and most of them had received multiple lines of chemotherapy.
-
4.
As it is a small prospective observational study, more studies like phase III-RCTs with a higher number of patients with adequately matched patients are required to conclude.
Conclusions
A combination of immune checkpoint inhibitors and metronomic chemotherapy may provide an avenue for targeting therapy-resistant cells, including CSCs and TICs, without inflicting unacceptable toxicity, resulting in high treatment compliance, improved long-term outcomes for difficult-to-treat cancers, and improved patient quality of life. So, to conclude, nivolumab along with metronomic chemotherapy with low-dose capecitabine was very well tolerated and exhibited anti-tumor activity with a CBR of 66%, 6-month OS of 83.3%, and PFS of 66.6%, in an extensively pretreated patient population with HNSCCs with lesser side effects and better quality of life as compared to conventional chemotherapy. Additional studies of nivolumab and metronomic chemotherapy and immuno-immuno combination therapy in these diseases are ongoing.
Data Availability
All required data is available in the article itself, so if any updates are available we will provide as and when required.
Abbreviations
- ECOG:
-
Eastern Cooperative Oncology Group
- Ca BM:
-
Carcinoma Buccal Mucosa
- Ca BOT:
-
Carcinoma of Base of Tongue
- SqCC:
-
Squamous cell carcinoma
- PCV:
-
Packed cell volume
- Alb:
-
Albumin
- PD:
-
Progressive disease
- PR:
-
Partial response
- LFU:
-
Lost to follow-up
- SD:
-
Stable disease
References
Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F et al (2017) GBD 2016 Disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390(10100):1211–59
Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C (2015) Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma. J Clin Oncol 33(29):3235–3242
Argiris A, Li S, Ghebremichael M, Egloff AM, Wang L, Forastiere AA et al (2014) Prognostic significance of human papillomavirus in recurrent or metastatic head and neck cancer: an analysis of Eastern Cooperative Oncology Group trials. Ann Oncol 25(7):1410–1416
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S et al (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 359(11):1116–1127
Zang X (2018) 2018 Nobel Prize in medicine awarded to cancer immunotherapy: Immune checkpoint blockade – a personal account. Genes Dis 5(4):302–303
Sundar R, Cho B, Brahmer JR, Soo AR (2015) Nivolumab in NSCLC: latest evidence and clinical potential. Ther Adv Med Oncol 7(2):85–96
Bellone S, Buza N, Choi J, Zammataro L, Gay L, Elvin J et al (2018) Exceptional response to pembrolizumab in a metastatic, chemotherapy/radiation-resistant ovarian cancer patient harboring a PD-L1-genetic rearrangement. Clin Cancer Res 24(14):3282–3291
Facchinetti F, Bordi P, Leonetti A, Buti S, Tiseo M (2018) Profile of atezolizumab in the treatment of metastatic non-small-cell lung cancer: patient selection and perspectives. Drug Des Devel Ther 12:2857–2873
Onyshchenko M (2018) The puzzle of predicting response to immune checkpoint blockade. EBioMedicine 33:18–19
Rosenberg SA, Yang JC, Restifo NP (2004) Cancer immunotherapy: moving beyond current vaccines. Nat Med 10(9):909–915
Bailly C, Thuru X, Quesnel B (2020) Combined cytotoxic chemotherapy and immunotherapy of cancer: modern times. NAR Cancer 2(1):zcaa002. https://doi.org/10.1093/narcan/zcaa002
Revannasiddaiah S, Madabhavi I, Bodh A, Thakur P, Sharma M (2015) Metronomic chemotherapy in anaplastic thyroid carcinoma: a potentially feasible alternative to therapeutic nihilism. Indian J Palliat Care 21(2):245–249
Revannasiddaiah S, Pandey KC, Madabhavi IV et al (2019) Evaluation of continuous low dose versus standard dose capecitabine monotherapy as second/third-line chemotherapy for metastatic malignancies. Ann Oncol 30(suppl_9):ix118–ix121. https://doi.org/10.1093/annonc/mdz430
Madabhavi IV, Sarkar M, Sagar R (2021) Metronomic low-dose capecitabine in metastatic, recurrent, or persistent carcinoma of the cervix as 3rd line and beyond. Ann Oncol 32(suppl_5):S725–S772. https://doi.org/10.1016/annonc/annonc703
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S et al (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 359(11):1116–27
Sharma P, Allison JP (2015) The future of immune checkpoint therapy. Science 348:56–61
Topalian SL, Drake CG, Pardoll DM (2015) Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell 27:450–461
Ferris RL, Blumenschein G Jr, Fayette J, Guigay J, Colevas AD, Licitra L et al (2016) Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med 375(19):1856–1867
Zandberg DP, Strome SE (2014) The role of the PD-L1: PD-1 pathway in squamous cell carcinoma of the head and neck. Oral Oncol 50(7):627–632
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP et al (2015) Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 372:2018–2028
Horn L, Spigel DR, Vokes EE, Holgado E, Ready N, Steins M et al (2017) Nivolumab versus docetaxel in previously treated patients with advanced non-small-cell lung cancer: two-year outcomes from two randomized, open-label, phase III trials (CheckMate 017 and checkMate 057). J Clin Oncol 35:3924–3933
Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WE, Poddubskaya E et al (2015) Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 373:123–135
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375:1823–1833
Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F et al (2018) Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 378:2078–2092
Cramer JD, Burtness B, Ferris RL (2019) Immunotherapy for head and neck cancer: recent advances and future directions. Oral Oncol 99:104460
Gupta VG, Bakhshi S (2017) Pediatric hematopoietic stem cell transplantation in India: status, challenges and the way forward: Based on Dr. K. C. Chaudhuri oration 2016. Indian J Pediatr 84:36–41
Maiti R (2014) Metronomic chemotherapy. J Pharmacol Pharmacother 5(3):186–192
Nai-Wen Su, Chen Y-J (2021) Metronomic therapy in oral squamous cell carcinoma. J Clin Med 10(13):2818
Patil Vijay Maruti, Noronha Vanita, Menon Nandini, Rai Rahul, Bhattacharjee Atanu, Singh Ajay et al (2023) Low-dose immunotherapy in head and neck cancer: a randomized study. J Clin Oncol 41(2):222–23
Iqbal H (2016) Quintin Pan; Capecitabine for treating head and neck cancer. Expert Opin Investig Drugs 25(7):851–859
Van Der Kraak L, Goel G, Ramanan K, Kaltenmeier C, Zhang L, Normolle DP et al (2016) 5-Fluorouracil up-regulates cell surface B7–H1 (PD-L1) expression in gastrointestinal cancer. J Immunother Cancer 4:65
Chen YL, Chang MC, Cheng WF (2017) Metronomic chemotherapy and immunotherapy in cancer treatment. Cancer Lett 400:282–292
Kareva I (2017) A combination of immune checkpoint inhibition with metronomic chemotherapy as a way of targeting therapy-resistant cancer cells. Int J Mol Sci 18:2134
Chang CH, Qiu J, O’Sullivan D, Buck MD, Noguchi T, Curtis JD et al (2015) Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell 162:1229–1241
Mpekris F, Voutouri C, Panagi M, Baish JW, Jain RK, Stylianopoulos T (2022) Normalizing tumor microenvironment with nanomedicine and metronomic therapy to improve immunotherapy. J Control Release 345:190–199
Aravind S, Jose J, Shenoy PK, Avaronnan M, Thavarool SB, Nayanar SK (2022) The spectrum of histomorphological changes and pathological tumor response following preoperative oral metronomic chemotherapy in oral squamous cell carcinoma South Asian J. Cancer 11(2):146–151
Martinez-Trufero J, Isla D, Adansa J, Irigoyen A, Hitt R, Gil-Arnaiz I et al (2010) Phase II study of capecitabine as palliative treatment for patients with recurrent and metastatic squamous head and neck cancer after previous platinum-based treatment. Br J Cancer 102:1687–1691
Wu Y, Deng Z, Wang H, Ma W, Zhou C, Zhang S (2016) Repeated cycles of 5-fluorouracil chemotherapy impaired anti-tumor functions of cytotoxic T cells in a CT26 tumor-bearing mouse model. BMC Immunol 17:29
Author information
Authors and Affiliations
Contributions
IM conceived and designed the experiment, made critical revisions, and approved the final version. IM, MS, VK, and RS analyzed the data and wrote the first draft of the manuscript. IM, MS, VK, and RS contributed to the writing of the manuscript. IM, MS, VK, and RS agree with the manuscript results and conclusions. IM, MS, VK, and RS jointly developed the structure and arguments for the paper. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
None declared. Initial 2-year data has been accepted in an abstract form in the Proceedings of the AACR-NCI-EORTC Virtual International Conference on Molecular Targets and Cancer Therapeutics; 2021 Oct 7–10. Philadelphia (PA): AACR; Mol Cancer Ther 2021;20(12 Suppl): Abstract nr P101.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Madabhavi, I., Sarkar, M., Kumar, V. et al. Combined Metronomic Chemo-immunotherapy (CMCI) in Head and Neck Cancers–An Experience from a Developing Country. Indian J Surg Oncol 15, 321–331 (2024). https://doi.org/10.1007/s13193-024-01900-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-024-01900-6