Abstract
Oncoplastic breast surgery involves immediate reshaping of the breast after tumor excision. It enables wider excision of the tumor while maintaining a satisfactory cosmetic outcome. One hundred and thirty seven patients underwent oncoplastic breast surgery at our institute between June 2019 and December 2021. The procedure performed was decided based on the location of tumor and volume of excision. All patient and tumor characteristics were entered into an online database. The median age was 51 years. The mean tumor size was 3.666 cm (± 0.2512). Twenty-seven patients underwent a type I oncoplasty, 89 patients type 2 oncoplasty, and 21 patients a replacement procedure. Only 5 patients had margin positivity out of which 4 patients underwent a re-wide excision with negative margins. Oncoplastic breast surgery is a safe and effective method to manage patients who need conservative surgery of breast tumors. It allows us to provide good esthetic outcome to the patients ultimately aiding in better emotional and sexual well-being.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
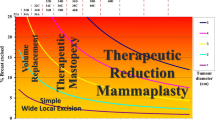
Breast conservation surgery (BCS) involves excision of the tumor with adequate margins. It provides equivalent survival as modified radical mastectomy [1,2,3]. Though the goal of such treatment is to preserve a near normal breast, almost 40% of patients end up having poor cosmetic results [4]. It has been shown that the upper limit of volume excision for a standard BCS to give an esthetically pleasing outcome is 10% [5]. Mastectomies are reserved for those patients with extensive microcalcifications and multifocal tumors or those with recurrent tumors [6]. There still remain a large proportion of patients who do not fit into either category and for whom a conservative surgery would definitely mean a severely deformed breast.
Oncoplastic breast surgery (OBS) helps us in bridging such lacunae. First introduced in 1984, by W. Audretsch, it integrates the principles of plastic surgery techniques allowing immediate reshaping of the breast without compromising oncological principles [7, 8]. It enables us to allow for wider excisions of tumors without the need to worry about the final esthetic result [9, 10]. The factors that need to be taken into consideration when performing an oncoplastic procedure are (1) the location of the tumor, (2) the volume of the tumor excised, and (3) the density of the breast. Accordingly, if lesser than 50% of the breast volume is excised, a displacement oncoplastic procedure is performed. More than 50% of excision volume would require replacement of the lost tissue [11].
At Homi Bhabha Cancer Hospital and Research Centre, Visakhapatnam, we strive to perform oncoplastic breast surgery in all patients undergoing breast conservation. In this paper, we would like to present our experience with oncoplastic breast surgery at our institute and the challenges faced by us.
Materials and Methods
A retrospective analysis was conducted on one hundred and thirty-seven patients who underwent conservative surgery of the breast at our institute between June 2019 and December 2021, after obtaining institutional ethical clearance. Oncoplastic procedures were performed on all of these 137 patients. All patients were preoperatively assessed by the surgical oncologist. Standard mammogram images were taken. The oncoplastic procedure to be performed was decided based on tumor location, expected excision volume, and breast density. In patients whose tumor size was more than 5 cm or who had unfavorable tumor breast ratio or large tumors located in unfavorable areas of the breast, neoadjuvant chemotherapy was given to downstage the tumor. All patients were explained about symmetrization of the opposite breast.
A 2-team approach (surgical oncologist and plastic surgeon) was used for all patients. Preoperative markings were done in the standing position. Excision of the tumor with adequate margins and axillary clearance was done by the surgical oncologist. If the tumor was located far away from the axilla, a second incision was placed along the axillary hairline to address the axilla. If the operating surgeon felt that the primary tumor excision and axillary clearance could be performed through a single incision, the radial extension of the racquet mammoplasty incision was used to address both. The base of the defect was marked with titanium clips. The oncoplastic procedure was carried out by the plastic surgeon. As frozen section facility was not available at our institution, all specimens were subjected to routine histopathological examination. If final histopathological report showed that margins were involved by the tumor, then re-excision of the involved margins or mastectomy was performed at a second sitting. Adjuvant systemic therapy (chemotherapy/targeted therapy and hormonal therapy) was given based on the pathologic grade and ER/PR/HER2 status. All the patients received adjuvant radiotherapy, 40 Gy in 15 fractions followed by 12.5 Gy boost to the tumor bed, after completion of chemotherapy. Patient and tumor characteristics, procedure performed, postoperative complications, margin positivity status, and details of adjuvant therapy were entered into a clinical database. All clinical photographs were taken after obtaining informed written consent from the patient.
Results
The median age of the patients operated was 51 years (range 27–76, 50.63 ± 1.902). Most patients (n = 76) had tumors located in the upper outer quadrant. The average tumor size was 3.666 cm (± 0.2512). The majority of patients (n = 77) had a heterogeneously dense breast on mammogram. Sixty-three patients received neoadjuvant chemotherapy to downsize the tumor. Following neoadjuvant chemotherapy, the mean tumor size was 1.9523 cm (± 0.2838). Twenty-seven patients (19.708%) underwent a type I oncoplasty, 89 patients (64.963%) type 2 oncoplasty, and 21 patients (15.328%) underwent a replacement procedure. The details of individual procedures are described in Table 1. None of our patients opted for an opposite side symmetrization procedure. Early postoperative complications mostly included seroma formation below the skin flaps which was managed conservatively with compression dressings. Five out of 137 (3.64%) patients had positive margins on histopathological examination. Four of these patients underwent re-wide excision during a second surgery with negative margins. One patient underwent mastectomy.
Discussion
Breast cancer remains the most common cancer among women in the Indian population [12]. More patients present to the oncologist at an advanced stage due to lack of awareness of the disease and lack of screening [13]. The administration of neoadjuvant chemotherapy in such patients enables us to downstage most tumors [14]. Patients who would have been previously subjected to upfront mastectomy end up being eligible candidates for breast conservation surgery. In addition, advances in systemic therapy have led to improved survival of all breast cancer patients [15]. Hence, it becomes the responsibility of the operating surgeon to focus not only on providing a disease-free life to the patient but also to improve the esthetic outcome, ultimately enhancing the emotional, sexual, and psychological well-being of the patient.
The limitations of BCS become more obvious when more than 20% of breast volume resection is expected, those with large tumors and small breasts or those with unfavorable tumor–breast ratio [11]. Similarly when tumors are located in unfavorable areas of the breast such as the inner quadrant, resection leads to significant deformity [16]. The seroma that collects in the cavity left behind consolidates over time leading to tissue retraction, adhesion formation, nipple deviation, nipple malposition, and asymmetry between both the breasts [17]. The added effects of radiation further worsens these deformities. Oncoplastic breast surgery mitigates such deficiencies. When OBS was first started, the reduction mammoplasty procedure was used to reshape the breast following tumor resections [6]. However, it became difficult to manage tumors located at various parts of the breast with reduction procedure alone. At our institute, we performed surgeries according to the per quadrant atlas first described by Clough et al [11]. They recommend using a donut mastopexy or inferior pedicle reduction mastopexy for superior quadrant tumors, racquet mastopexy for upper outer quadrant tumors, J mammoplasty for lower outer quadrant tumors, superior pedicle reductions for lower pole tumors, V mammoplasty for lower inner quadrant tumors, and batwing/hemibatwing procedure for upper inner quadrant tumors. The most commonly performed procedures in our series were the racquet mastopexy (Fig. 1a and b) and donut mastopexy (Fig. 2a and b). Though these procedures were typically described for upper outer quadrant tumors and superior pole tumors, respectively, we found them to be very versatile. Using these incisions, tumors from almost all quadrants of the breast could be excised with satisfactory cosmetic outcome. For all central quadrant defects, we performed a Grisotti procedure [18] (Fig. 3). When tissue replacement was required (more than 50% breast tissue excised), we performed a transposition flap [19] (upper outer quadrant defects/lateral defects) or a latissimus dorsi myocutaneous (LD) flap (Fig. 4a and b). In most patients, a LD flap with transverse skin paddle was harvested so that the final scar line remained hidden underneath the bra strap.
Opposite breast symmetrization forms an integral component of oncoplastic breast surgery. Excision of the tumor combined with rearrangement of the remaining breast tissue can lead to significant asymmetry between the breasts. Adjuvant radiation therapy worsens the fibrosis which could possibly lead to an increase in the discrepancy between both the breasts. Symmetrization can be done at the same sitting or as a secondary procedure [20]. The major challenge that we face with patients at our institute is acceptance of conservative surgery. Most patients think that chances of recurrence are higher with breast conservation surgery and opt for modified radical mastectomy. Persuading patients to undergo oncoplastic breast surgery is a task in itself. In such situations, getting patients to agree to be operated on the opposite normal breast in order to achieve symmetry is even more difficult. As reduction procedures would result in a significantly smaller breast and make the asymmetry between the breasts more conspicuous, we avoided performing it on any of our patients and chose procedures that would not lead to significant difference between the appearance of both breasts.
One of the major advantages of oncoplastic breast surgery is the ability to remove the tumor with wider margins than possible in a conventional BCS. Bali et al. [21] reported a margin positivity of 5.7% in their OBS group compared to 20.8% in the wide local excision group. Clough et al. [22], in their study, had a margin positivity rate of 11.9%. They noted that there were significantly more positive margins in patients with T3 and T2 cancers than T1 cancers. Similarly, patients with invasive lobular carcinoma had a higher risk than invasive ductal carcinoma for positive margins. It is not necessary for all patients with positive margins to undergo a mastectomy, unless there is repeated positivity after multiple attempts at BCS. In our series, the margin positivity rate was 3.64%. Eighty percent of the patients with positive margins underwent re-wide excision with negative margins. One patient did not consent to a conservative surgery and hence underwent a mastectomy.
Oncoplastic breast surgery provides better cosmetic outcome compared to breast conservation surgery. There are many methods by which this can be evaluated, either subjectively or objectively. The limitation of our study is that we have been unable to assess our cosmetic outcomes due to (1) logistical problems of patients being seen by different specialists postoperatively and (2) lack of documentation of the cosmetic outcome. However, we have undertaken an ambispective trial with systematic documentation to objectively assess the delayed cosmetic result in our patients using the BCCT.core [23] software and compare it with subjective patient satisfaction scores. The next step in our endeavor would be to assess the long-term cosmetic outcome, local recurrence rates, and survival rates of all patients who have undergone OBS at our institute.
Oncoplastic breast surgery can be easily implemented across all breast cancer units in the country. Though most centers function with a dual team concept(surgical oncologist and plastic surgeon), a one-surgeon dual-role model can also be utilized if specialized training in the field can be obtained by breast surgeons [13]. This can ensure surgical cost reduction and better delivery of the procedure across all strata of society.
Conclusion
Oncoplastic breast surgery forms a safe third pathway for treating those tumors that cannot be satisfactorily managed by conventional breast conservation surgery or those that do not warrant a modified radical mastectomy. It enables us to remove tumors with better margins without the need to worry about the final esthetic outcome. It can be easily performed across all breast cancer units with adequate training. It is not only important to assess the oncological safety of OBS but imperative to assess and document the short- and long-term cosmetic outcomes of the procedure.
References
Veronesi U, Cascinelli N, Mariani L et al (2002) Twenty-year follow-up of a randomised study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 347:1227e32. https://doi.org/10.1056/NEJMoa020989
Fisher B, Anderson S, Bryant J et al (2002) Twenty-year follow-up of a randomised trial comparing total mastectomy, lumpectomy and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347:1233e41. https://doi.org/10.1056/NEJMoa022152
Van Dongen JA, Voogd AC, Fentiman IS et al (2000) Long-term results of a randomised trial comparing breast-conserving therapy with mastectomy: European Organisation for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst 92:1143e50. https://doi.org/10.1093/jnci/92.14.1143
Haloua MH, Krekel NM, Winters HA et al (2013) A systematic review of oncoplastic breast-conserving surgery: current weaknesses and future prospects. Ann Surg 257(4):609–620. https://doi.org/10.1097/SLA.0b013e3182888782
Cochrane RA, Valasiadou P, Wilson ARM et al (2003) Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. Br J Surg 90:1505e9. https://doi.org/10.1002/bjs.4344
Berry MG, Fitoussi AD, Curnier A, Couturaud B, Salmon RJ (2010) Oncoplastic breast surgery: a review and systematic approach. J Plast Reconstr Aesthet Surg 63(8):1233–1243. https://doi.org/10.1016/j.bjps.2009.05.006
Audretsch W (1987) Space-holding technic and immediate reconstruction of the female breast following subcutaneous and modified radical mastectomy. Arch Gynecol Obstet 241(Suppl):S11–S19. https://doi.org/10.1007/BF00930983
Audretsch W (1998) Tumor-specific immediate reconstruction in breast cancer patients. Perspect Plast Surg 11:71–100. https://doi.org/10.1055/s-2008-1080243
Clough KB, Lewis JS, Couturaud B et al (2003) Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 237:26–34. https://doi.org/10.1097/00000658-200301000-00005
von Smitten K (2008) Margin status after breast-conserving treatment of breast cancer: how much free margin is enough? J Surg Oncol 98:585–587. https://doi.org/10.1002/jso.21038
Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM (2010) Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol 17(5):1375–1391. https://doi.org/10.1245/s10434-009-0792-y
Asthana S, Chauhan S, Labani S (2014) Breast and cervical cancer risk in India: an update. Indian J Public Health 58:5–10. https://doi.org/10.4103/0019-557X.128150
Koppiker CB, Chintamani, Dixit S (2019) Oncoplastic breast surgery in India: thinking globally, acting locally. Indian J Surg 81:103–110. https://doi.org/10.1007/s12262-019-01890-8
Mieog JS, van der Hage JA, van de Velde CJ (2007) Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev 2007(2):CD005002. https://doi.org/10.1002/14651858.CD005002.pub2
Anon. Breast cancer: incidence rises while deaths continue to fall. http://www.statistics.gov.uk. Accessed January 2009
Clough KB, Baruch J (1992) Plastic surgery and conservative treatment of breast cancer. Indications and results. Ann Chir Plast Esthet 37:682–92
Choi JY, Alderman AK, Newman LA (2006) Aesthetic and reconstruction considerations in oncologic breast surgery. J Am Coll Surg 202:943–52. https://doi.org/10.1016/j.jamcollsurg.2006.02.026
Grisotti A, Casella D, Calabrese C (2010) Immediate reconstruction of central quadrantectomy defects with a rotation flap—the Grisotti technique. In: Fitzal F, Schrenk P (eds) Oncoplastic breast surgery; a guide to clinical practice. Springer-Verlag Wien, New York, p 97
Joshi S, Jaiswal D, Chougle Q, Wadasadawala T, Badwe RA (2021) Transposition flap for the oncoplastic reconstruction of outer quadrant breast defects. J Plast Reconstr Aesthet Surg 74(9):2176–2183. https://doi.org/10.1016/j.bjps.2020.12.037
Kaviani A, Safavi A, Mirsharifi R (2015) Immediate and delayed contralateral symmetrization in oncoplastic breast reduction: patients’ choices and technique formulation. Plast Reconstr Surg Glob Open 3(1). https://doi.org/10.1097/GOX.0000000000000246
Bali R, Kankam HK, Borkar N, Provenzano E, Agrawal A (2018) Wide local excision versus oncoplastic breast surgery: differences in surgical outcome for an assumed margin (0, 1, or 2 mm) distance. Clin Breast Cancer 18(5):e1053-7
Clough KB, Gouveia PF, Benyahi D, Massey EJ, Russ E, Sarfati I, Nos C (2015) Positive margins after oncoplastic surgery for breast cancer. Ann Surg Oncol 22(13):4247–4253. https://doi.org/10.1245/s10434-015-4514-3
Cardoso MJ, Cardoso J, Amaral N, Azevedo I, Barreau L, Bernardo M, Christie D, Costa S, Fitzal F, Fougo JL, Johansen J (2007) Turning subjective into objective: the BCCT. Core software for evaluation of cosmetic results in breast cancer conservative treatment. Breast 16(5):456–61. https://doi.org/10.1016/j.breast.2007.05.002
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Disclosures
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Babu, P., Chidananda Murthy, G. Oncoplastic Breast Surgery: a Single-Institution Experience. Indian J Surg Oncol 14, 199–203 (2023). https://doi.org/10.1007/s13193-022-01660-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-022-01660-1