Abstract
Malignant mesotheliomas most often affect the pleura and tend to spread locally within the originating cavity. Mesotheliomas are already rare diseases, and cases with synchronous pleural and peritoneal involvement are scarce in the literature. Mesothelioma in children is a rare disease representing only 0.9% of all mesotheliomas. They exhibit similar distribution and characteristics as mesotheliomas in adults and generally, a poor prognosis. Due to the rarity, there is no standardized treatment recommendation for children with mesothelioma. Though the malignant mesothelioma tends to spread locally within the originating cavity, pleuM have been reported to metastasize into the peritoneal cavity and vice versa. As there are only few studies concerning the metastatic spread of mesothelioma, it is difficult to define a precise incidence and risk factors for patients to develop metastases of the other mesothelium. There is no standardized therapeutic recommendation for patients with synchronous pleuM and perM. Our patient proved to profit from a radical two-stage surgical approach in combination with locoregional chemotherapy; she showed no sign of tumor recurrences 9 years after tumor resection. In conclusion, clinical studies are needed to confirm the benefit of this treatment and to determine its limitations and selection criteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The malignant mesothelioma is a tumor affecting the pleura, which is most commonly affected, the peritoneum [1], and other mesothelia, like the pericardium. Pleural mesotheliomas (pleuM) constitute 68.0–92.4% of all mesotheliomas. The peritoneum is the second leading location for mesotheliomas. Peritoneal mesotheliomas (perM) represent 6.9–24.1% of all cases. Malignant mesotheliomas of the pericardium (6.1%) and the tunica vaginalis testis (0.3%) are rare [2, 3].
The majority (74%) of malignant mesotheliomas occur in patients aged 50 to 79 years, while the mean age at the time of diagnosis is about 64–69 years (2, 3). Patients with perM are usually approximately 10 years younger at time of diagnosis (54–59 years) compared to patients with pleuM (69 years) [4,5,6].
Malignant mesothelioma predominantly affects men over women. Approximately 70% of all patients are men. However, there are some differences in gender distribution concerning different locations of the mesothelioma. Especially for pleuM, a tendency to affect men is reported. Approximately 74.8–79.3% of patients with pleuM are male and 20.7–25.2% are female, resulting in a ratio (male/female) of three. For perM, this tendency is less distinct. About 55.9% of patients are male and 44.1% are female, showing a ratio of 1.3 [2, 6,7,8]. Women presenting with perM are significantly younger than men with 17.2% under 60 years compared to 9.9% and show better overall survival with a 5-year-survival rate of 9.4% versus 4.2% [7].
We report the case of a 14-year-old female who presented initially with an epithelioid mesothelioma of the peritoneum and developed a recurrence in both the peritoneum and the right thorax after multiple chemotherapeutic regimens.
Case Report
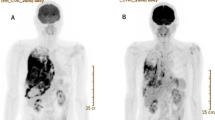
A 14-year-old female presented herself in April 2008 a periphery health center with sore throat, sub-febrile temperature, weight loss of about 3 kg, and a 4-week long deterioration of the general condition. The medical history of the patient was uneventful; no chronical diseases or long-term medication were reported. The patient’s father originated from Iran, and the mother was Caucasian. There was no family history of thrombophilia or vasculitis. Being pneumonia the suspected diagnosis, antibiotic treatment was administered, and a computer tomography (CT) scan of the thorax was carried out. A right-sided thrombosis of the internal jugular vein, of the axillary vein, and of the superior vena cava as well as a pleural effusion was confirmed. The pleural effusion was drained and cytologically evaluated, showing no sign of malignant cells, but an accumulation of chyle. The chylothorax was suspected as a result of the extended thrombosis. Diagnoses of malignant lymphoma, Behçet’s disease, and thrombophilia among others were ruled out. There was no evidence of a malignant disease, with normal levels of uric acid and lactate dehydrogenase and no sign of tumors in a diagnostic whole-body fluorodeoxyglucose (FDG)-positron emission tomography (PET).
In September 2008, the patient was referred to our hospital due to a 3-month-long secondary amenorrhea. Sonography of the abdomen showed a suspicious, right-sided, paracolic tumor. The CA-125 tumor marker was 692 U/ml (normal value up to 35 U/ml). A diagnostic laparoscopy for sample collection combined with a laparoscopic appendectomy was performed, and the diagnosis of an epithelioid mesothelioma was histologically confirmed. The mesothelioma showed both solid and papillary formation of epithelioid tumor cells with expression of HBME1, calretinin, podoplanin, and CK5/6; with no expression of CD45, CD68, galectin-3, S-100, or BerP4; and a MIB-1-proliferation index of 5%.
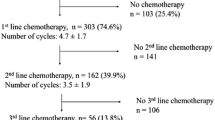
After the diagnosis was reached, the pediatric oncologists decided to commence with systemic therapy. A surgical option was not considered due to the precarious data available at the time and the young age of the patient. Therefore, the patient was treated with different chemotherapeutic regimens. The first regime consisted of cisplatin and pemetrexed. Due to tumor progression, chemotherapy was changed to carboplatin and gemcitabine and finally to the combination of vincristine, actinomycin, and cyclophosphamide (VAC). Treatment with VAC revealed a complete remission with no macroscopic tumor found in a diagnostic laparoscopy carried out 5 months later. To preserve the complete remission, a 6-month long maintenance treatment with vinblastine and cyclophosphamide followed.
In 2013, conspicuous iliac lymph nodes were noticed via FDG-PET in the course of regular follow-up examination. Together with an increased level of the tumor marker CA 125 (237 U/ml), the suspected diagnosis was a recurrence of the previously diagnosed mesothelioma. A CT scan of the thorax showed an apical pneumothorax and a suspicious nodular tumor in the middle lobe. Subsequently, both a diagnostic laparoscopy and a thoracoscopy with the collection of specimens were performed. Histopathological examination confirmed the diagnosis of recurrences of the mesothelioma within both the abdomen and the right thorax.
After discussing this case in the interdisciplinary tumor board, a two-stage surgical approach was recommended. In agreement with the patient, then 18 years old, we performed a right-sided thoracotomy with extended pleurectomy combined with an atypical segmental resection of the right lower lobe. All macroscopic tumor nodules could be removed with a completeness of cytoreduction (CCR) score of zero. After closure of the wound, a hyperthermic intrathoracic chemotherapy (HITOC) followed via two drains with cisplatin at a 75 mg/m2 and mitomycin at a 15 mg/m2 dose for a duration of 60 min. The postoperative course was uneventful, and the patient was discharged on postoperative day (POD) 5.
One month later, the second step of the radical surgical approach was performed with the aim of clearing the abdominal cavity. During explorative laparotomy, peritoneal manifestations were found at the parietal peritoneum, omentum, small bowel mesentery, gall bladder, liver capsule, uterus, both ovaries, both fallopian tubes, and the rectum, resulting in a Peritoneal Cancer Index (PCI) of 15. A total parietal peritonectomy, including multiple organ resection (omentectomy, extraperitoneal rectum resection, bilateral salpingo-oophorectomy, and cholecystectomy), was performed. A CCR-0 was achieved. Hyperthermic intraperitoneal chemotherapy (HIPEC) was performed immediately after wound closure with 132 mg cisplatin and 26.5 mg doxorubicin at 42 °C and a duration of 60 min. Histopathological slides are presented in Figs. 1 and 2.
The tumors (2008 and 2013) are characterized by an infiltratively growing epithelioid cell proliferation with a solid and papillary pattern. Corresponding tumor architecture can be appreciated in the pleural and peritoneal tumor manifestation. The mesothelial origin is demonstrated by the immunohistochemical expression of calretin as well as WT1 and the lacking expression of BerP4
After the abdominal surgery, the patient developed several minor to moderate postoperative complications, including an extended nausea treated with antiemetic medication; a left-sided pleural effusion, which was treated with a chest drain; and a catheter-associated thrombosis of the left subclavian vein resolved with therapeutic anticoagulation. The patient was discharged on POD 10.
In 2017, the patient presented with a persisting left-sided pneumothorax. A possible contralateral pleural mesothelioma was suspected. For further clarification, a thoracoscopy with collection of specimens was performed in June 2017. There were both macroscopically and histologically no indications for tumor recurrence. In January 2018, the patient developed an obstructive ileus, which was surgically addressed and solved in our department via laparotomy with adhesiolysis. The abdomen was free of recurrence as well.
To this date, the patient is alive and disease free. A visual overview of the case is represented in Fig. 3.
Method
A search strategy was defined following a consensus of the authors. The search strategy used variations in the MeSH Terms — “pleura mesothelioma” AND “malignant pleura mesothelioma” with “peritoneal mesothelioma” AND “malignant peritoneal mesothelioma” — found in title, abstract, or keywords to retrieve articles in the Medline (PubMed) Database referring to combined pleural and peritoneal mesothelioma. The search input was: (((“pleural mesothelioma”[All Fields]) AND (malignant pleural mesothelioma)) AND (“peritoneal mesothelioma”[All Fields])) AND (malignant peritoneal mesothelioma). The filters “Case Reports”, “Classical Article”, “Clinical Study”, “Introductory Journal Article”,”Meta-Analysis”, “Multicenter Study”, “Observational Study”, “Review”, “Guideline” and “Practice Guideline” were selected. A total of 38 results were queried.
Pleural and Peritoneal Mesothelioma
Risk Factors
The most important risk factor for developing a malignant mesothelioma is the exposure to asbestos, as about 80% of all patients with pleuM report an exposition to asbestos in the past. For perM, the association to asbestos is less distinct, with 33–50% of all cases associated to exposure [4, 9]. There is also a gender difference, whereas 78–87% of men with mesothelioma show an association to asbestos, and only 10–65% of mesotheliomas in woman are attributable to exposure [10]. Though asbestos causes the majority of mesotheliomas, other factors, such as mineral fibers like erionite and fluoro-edenite, balangeroite, carbon nanotubes, radiotherapy, chronic inflammation, simian virus 40 (SV40), and germline mutations of BRCA1-associated protein-1 (BAP1), have also shown to increase the risk to develop a mesothelioma [10]. Nevertheless, mesotheliomas with somatic BAP1 mutations are associated with longer survival. Therefore, the loss of BAP-1 may result in a better prognosis [10,11,12].
Histopathology
Histologically, the mesothelioma is divided into three subtypes: epithelioid, sarcomatoid, and biphasic or mixed. The most common histological subtype is the epithelioid subtype, constituting 41.0–46.3% of all mesotheliomas, followed by the sarcomatoid (14.5–30.9%) and the biphasic subtype (28.1–31.5%) [2, 3]. For pleuM, diverse data regarding the distribution of the histological growth pattern are reported: Epithelioid subtype is found in 21–73%, biphasic subtype in 14–71%, and sarcomatoid subtype in 5–34.8% of all pleuM [2, 8, 13, 14]. The majority of perM present with an epithelial histological growth pattern (52.4–81%). A biphasic subtype is found in 8–29.4%, a sarcomatoid subtype in about 18.3% of cases [2, 4]. The classification of the mesothelioma in different histological subtypes is relevant as the subtypes have an influence on the patient’s survival and may affect the choice of treatment [15].
Diagnosis
Both perM and pleuM usually present with vague and unspecific symptoms, and therefore, patients with mesothelioma are often diagnosed at an advanced stage of disease. For perM, abdominal pain constitutes the predominant symptom, found in about 33–69% of patients [4, 16]. Other common symptoms reported for patients with perM are abdominal distension, new-onset hernia, weight loss, fatigue, fever, diarrhea, and vomiting. About 8% of perM are detected incidentally [16, 17]. Patients with pleuM commonly present with chest pain (31,7%) and dyspnea (30%) [18, 19].
Mesotheliomas exhibit a tendency to spread locally within the originating pleural or peritoneal cavity. Nevertheless, distant metastases can also be found, especially at a late stage of disease. At the initial staging, only 3.5–5% of patients with pleuM present a metastatic disease. The most commonly affected sites of metastases are distant lymph nodes (27.4%) and the abdominal cavity (26.2%), followed by the contralateral lung (15.5%), the peritoneum (10.7%), bones (9.5%), the liver (8.3%), the contralateral pleura (7.1%), and the brain (2.4%) [8, 20]. At the time of initial staging, about 4% of perM present with an extra-abdominal metastatic disease, in the form of tumor penetrating the diaphragm or old scars [21].
Prognosis
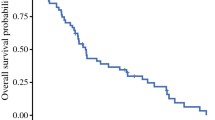
Overall, malignant mesotheliomas are associated with a poor prognosis. Depending on the initial tumor staging, an overall median survival of 10.1–22.9 months is reported for patients with pleuM. Especially patients with distant metastases show a poor prognosis. A median survival of 17.3 months is described for patients with single metastatic lesions and 5.8 months for multiple lesions [6, 8]. For perM, a median survival time of 13–16 months is reported [5, 17]. There are many different variables affecting the prognosis of these patients, such as the patients’ age, the extent of disease, the histological subtype, and the treatment [9].
Therapy
For both pleuM and perM, different treatment strategies exist. Common treatment options for patients with perM include surgical resection of the tumor and chemotherapy. For both pleuM and perM, best outcomes are reported for the combination of different treatment modalities.
Pleural Mesothelioma
For pleuM, different approaches for surgical treatment with curative intent exist: (extended) pleurectomy/decortication and extrapleural pneumonectomy. These approaches differ regarding the extent of resection. Whereas the extrapleural pneumonectomy includes the complete resection of the lung, the visceral and parietal pleura, diaphragm and pericardium, the extended pleurectomy/decortication is performed without the resection of the lung and the pleurectomy/decortication without the resection of the diaphragm and the pericardium [22]. The rationale of local chemotherapy following radical surgery is to address remaining tumor cells after macroscopic tumor removal. Hyperthermic intrathoracic chemotherapy (HITOC) contains the intrapleural injection of cytotoxic agents combined with hyperthermic perfusion. It has shown to enhance the cytotoxic effect on tumor cells with limited systemic side effect. Zhao et al. [23] demonstrated the positive effect of HITOC in patients with pleuM, showing significantly longer median survival compared to patients without HITOC in a meta-analysis. An important modality in the treatment of pleuM is systemic chemotherapy. For over 15 years, the standard first-line treatment is cisplatin and pemetrexed. The combination of both drugs has been reported to improve survival with a median overall survival of 12.1–12.8 months compared to 9.0–9.3 months for cisplatin alone [22, 24]. Possible indications for radiotherapy in the treatment of pleuM include adjuvant radiotherapy after extrapleural pneumonectomy or neoadjuvant radiotherapy. Additionally, palliative radiotherapy can be used in patients with pleuM to treat pain, dysphagia, and airway obstruction and to relief compression of the superior vena cava [22, 25].
Peritoneal Mesothelioma
The majority of patients with perM is treated with systemic chemotherapy. Commonly used chemotherapeutic agents for the treatment of perM are pemetrexed, cisplatin, and carboplatin. A median survival of 8.7–13.1 months is reported for patients with perM treated with one agent or with pemetrexed combined with cisplatin or carboplatin. In combination, these drugs proved to achieve increased survival [9]. A potentially curative treatment approach is the combination of cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). A median survival of 29.5–67 months has been demonstrated in different studies after CRS and HIPEC. Especially the completeness of cytoreduction is a main prognostic factor reported for this treatment. After complete tumor resection, a median survival up to 80.7–94 months can be reached [26]. Regarding chemotherapeutic drugs used for HIPEC, an improved survival is reported for cisplatin and carboplatin compared to mitomycin [9].
Discussion
In light of the case herein report, we would like to emphasize the following highlights: firstly, the young age of the patient at the time of diagnosis; secondly, the synchronous aspect of the pleural and peritoneal involvement; and lastly, the radical two-stage surgical approach, which has resulted in a disease-free survival (DFS) up to May 2020.
Mesothelioma in Children
Mesothelioma in children is a very rare disease. Approximately 0.9% of all mesotheliomas are diagnosed in the first two decades of life [2]. Therefore, for this age cohort, there is a lack of information about the incidence, typical characteristics, and treatment recommendations. Nevertheless, some cases of mesothelioma in children are reported in the literature, most often in the form of a case report. For children, a similar distribution regarding the origin of the tumor is reported as for adults. About 67.5–85% of mesotheliomas in childhood are pleuM and 15–25% perM. In about 7.5%, mesotheliomas originate from the pericardium [27, 28]. The majority of mesotheliomas in childhood occur during the teenager years [27]. Nonetheless, Silberstein et al. reported a case of a congenital peritoneal mesothelioma in 1983. The patient was diagnosed at an age of 6 weeks with a papillary peritoneal mesothelioma of low-grade malignancy [29].
Brenner et al. described seven cases of mesothelioma in childhood: six with pleuM and one with perM. For none of the patients, an exposure to asbestos was reported. Of the 7 children, 5 died within the first 2 years after diagnosis [27]. Another study concerning mesothelioma in childhood analyzed four neoplasms of the pleura and four neoplasms of the peritoneum. The patients’ age was 4 to 17 years at diagnosis. Histologically, the majority of mesotheliomas (75%) exhibited an epithelial subtype. Coffin et al. analyzed the immunohistochemical profile of the eight mesotheliomas. All tumors were immunopositive for vimentin, seven for cytokeratin, six for epithelial membrane antigen (EMA, MUC1), and each one positive for CA-125, B27,3, and the S100 protein. All mesotheliomas were negative for carcinoembryonic antigen, Leu-M1, and placental alkaline phosphatase. They concluded that the immunohistochemical profile for mesothelioma in adults and in younger patients is comparable [30]. Faire et al. evaluated a group of 80 cases. The cases were identified via different sources, like review of the literature and correspondence with different institutions and hospitals. In summary, 58.7% of the patients were boys and 41.3% were girls. In four children, risk factors for developing a malignant mesothelioma were found: Two presented with a possible exposure to asbestos, one had previous radiotherapy for a Wilms’ tumor and one had in utero exposure to isoniazid [28]. Reported symptoms of children presenting with pleuM are chest pain, difficulty in breathing, hemoptysis, cough, and hoarseness. Children with perM were reported to present with abdominal pain [27].
Synchronicity of Pleural and Peritoneal Involvement
Our patient was initially diagnosed with and treated for a perM. After the successful systemic chemotherapeutic treatment of the tumor, the patient developed a simultaneous recurrence of the mesothelioma both in the peritoneal and the pleural cavity. This coincidence of perM and pleuM seems to be very rare, but other cases can be found in literature.
Del Gobbo et al. reported a case of a 58-year-old woman presenting with a pleural mesothelioma and a synchronous peritoneal mesothelioma. Growth pattern and histological morphology seemed to be comparable in both manifestations of mesothelioma. In trying to demonstrate whether both mesotheliomas developed synchronously, or one manifestation is the result of the metastasis of the other, they failed to achieve conclusive results. The patient was treated with chemotherapy and was still alive after a follow-up of 6 months. The authors performed a review of literature for synchronous pleuM and perM. They found only one case of simultaneous mesotheliomas, bilaterally located in both tunica vaginalis of the testis [31]. Del Gobbo et al. concluded to be the first to report a case with synchronous pleuM and perM [32].
Nonetheless, there are several examples reported in the literature of mesotheliomas with tumor spreading from the thoracic cavity into the peritoneum and vice versa. Murai et al. evaluated 1.846 (0.17%) malignant mesothelioma cases among 1,056,259 autopsy cases. They found 0.5% of all patients with malignant mesothelioma showed an involvement of both the pleura and the peritoneum [2].
PleuM constitute the majority of mesotheliomas. The tumors tend to spread locally within the pleural cavity. However, distant metastases can occur, especially at a late stage of disease. Roberts examined 32 cases of pleuM via complete autopsy. He found distant visceral metastases in 47% of the cases. In 15.6% of all cases, metastases were found in the peritoneal cavity. In all cases of peritoneal metastases, the diaphragm and the surface of the liver were infiltrated. Other common sites of distant metastases were the opposite lung (21.9%), the kidneys (15.6%), and the adrenals (9.4%). Metastases were also found in the heart, the brain, the thyroid, the liver, and the pancreas [33]. Another retrospective study analyzing postmortem examinations of pleuM found distant metastases in 30% of 48 cases. Peritoneal involvement was detected in 25% of all evaluated cases. They found the metastases pattern to be independent of growth pattern and histological morphology [13]. In a two-center study, Finn et al. analyzed postmortem records of 334 patients with proven pleuM. They reported a tumor involvement beyond the ipsilateral pleural layer in 8.7% of cases. Extrathoracic mesothelioma was found in 55.4% and in 24.4% of cases, and the tumor showed spreading into the peritoneal cavity [14]. Rice et al. performed an extended surgical staging for 118 patients with pleuM clinically and radiologically considered to be resectable. They executed a mediastinoscopy in 111 patients, laparoscopy in 109 patients, and peritoneal lavage in 78 patients. Diagnostic laparoscopy exhibited transdiaphragmatic extension of the pleuM in 8.3% of patients and diffuse peritoneal metastases in one patient (0.9%). In two patients (2.6%), peritoneal lavage was cytologically positive for malignant cells. No evidence of transdiaphragmatic invasion was found in both cases [34]. Rusch et al. found distant metastases in 3.5% of patients with newly diagnosed, cytologically, or histologically confirmed malignant pleuM. Initial staging revealed peritoneal metastases in 0.4% of all cases.
PerM is less common than pleuM, and therefore, only little is reported about the occurrence of metastases. A multi-institutional study collected data on 294 patients with perM who underwent CRS and HIPEC to formulate a clinicopathological staging system. Overall, 4% of patients presented with extra-abdominal metastatic disease in the form of the tumor penetrating the diaphragm or old abdominal wall scars. Though extra-abdominal tumor manifestations were resected during CRS, the prognosis for these patients was poorer (median survival of 20 months) than for patients without extra-abdominal metastasis (median survival of 76 months) [21]. Magge et al. prospectively evaluated 65 patients with perM treated with CRS and HIPEC. The tumor was confined to the peritoneum in 86% of patients, while nine patients (14%) showed combined peritoneal and pleural disease at presentation: Two patients presented on follow-up imaging with localized, non-progressive, and asymptomatic pleural plaques without any sign of abdominal disease recurrence. Another patient developed a persistent postoperative pleural effusion with positive cytology, successfully treated with pleurodesis. Rapid peritoneal and pleural disease progression was detected in two patients, who died within 1 year of CRS and HIPEC. A combined surgical approach with resection of the pleural and peritoneal tumor involvement was performed in four patients with pleural metastases: One patient underwent palliative resection of a mediastinal mesothelioma 20 months after CRS and HIPEC. Two patients previously had bilateral pleurectomy and HITOC before developing peritoneal tumor recurrence. Treated with CRS and HIPEC, one patient was reported to remain disease-free. The other patient underwent palliative CRS and HIPEC for severe ascites and pain and died in the early postoperative period. The last patient was treated with CRS and HITOC for pleural tumor involvement 6 months following CRS and HIPEC. This patient died due to recurrence in the chest cavity. Magge et al. concluded that this subgroup of patients with combined mesothelioma exhibits no survival difference from those with exclusive perM [4].
The pattern of treatment failure after CRS and HIPEC of diffuse malignant peritoneal mesothelioma was addressed by a study of Baratti et al. They observed a disease progression in 38 of 70 patients (54.3%) undergoing CRS and HIPEC after a median follow-up of 43 months. Involvement of the pleura was noticed in four patients (5.7%): two patients presented with localized recurrence of the basal pleura, and the remaining two patients developed a tumor involvement of both abdominal and pleural cavity. Tumor progression in the pleural cavity showed no correlation with the opening of the particular hemidiaphragms during surgery. For all patients with tumor recurrences, the median time to progression was 9 months. and the median survival from progression was 8 months [35].
There are only limited numbers of studies concerning the survival of patients with combined thoracic and peritoneal involvement. Table 1 lists cases described in the literature with perM and pleuM and their respective treatment and survival. There was no information available on BAP1 mutation status and Ki-67 expression.
Two-Stage Surgical Approach for Bicavitary Disease
Due to the small number of cases, no standardized therapeutic approach for patients with synchronous pleuM and perM exists. Table 1 lists cases found in the literature treated for combined pleuM and perM. For pleuM with peritoneal metastases, Sugarbaker claims that cytoreductive surgery of the peritoneal involvement and HIPEC should be considered in patients where combined surgical and regional chemotherapy treatments have achieved local control of the pleural tumor manifestation [36].
For these patients, he coins different clinical features suggesting a favorable outcome for the use of CRS and HIPEC:
-
General medical condition compatible with survival and recovery from the procedure
-
Peritoneal metastases compatible with a complete or near complete cytoreduction illustrated via contrast-enhanced CT
-
Relative sparing of the small bowel and colon
-
No disease outside the abdomen/pelvis
-
No or limited resectable hepatic metastases
-
No disease within the porta hepatis
-
Low or moderate PCI for tumors with a high-grade malignancy
-
Symptomatic patients
For patients without local control within the pleural space, treatment options are limited to systemic chemotherapy or best supportive care [36].
Our patient showed a long-term survival after combined and radical treatment of the pleural and the peritoneal cavity. Magge et al. also reported cases treated with the combination of CRS plus HIPEC and CRS plus HITOC. One of three patients showed a long-term survival [4]. As only isolated cases of combined perM and pleuM treated with a radical two-stage surgical approach and locoregional chemotherapy exist, it is difficult to determine the outcome, selection criteria, and the limitation of this treatment. As in some cases, a long-term survival can be achieved; patients with good performance status and tumor involvement of both the peritoneum and the pleura compatible with a complete or near complete cytoreduction could benefit from a radical two-stage surgical approach with locoregional chemotherapy.
Conclusion
In summary, our case presents several rare medical characteristics. Firstly, the mesotheliomas are rare in children, and due to its rarity, there is no standardized treatment recommendation for children with mesothelioma. Secondly, the synchronous aspect of the pleural and peritoneal involvement. Though the malignant mesothelioma tends to spread locally within the originating cavity and pleuM has been reported to metastasize into the peritoneal cavity and perM into the pleural cavity, it is difficult to define a precise incidence and risk factors for patients to develop metastases of the other mesothelium. Lastly, our radical two-stage surgical approach has resulted in a long-term DFS, meaning that selected patients could benefit from a two-stage surgical approach combined with a locoregional chemotherapy. Clinical studies are needed to confirm the benefit of this treatment and to determine its limitations and selection criteria.
References
National Cancer Institute NCI Dictionary of Cancer Terms. Bethesda, USA 2019 https://www.cancer.gov/publications/dictionaries/cancer-terms/def/mesothelioma. Accessed June 9 2019
Murai Y (2001) Malignant mesothelioma in Japan: analysis of registered autopsy cases. Arch Environ Health 56(1):84–88
Dragani TA, Colombo F, Pavlisko EN, Roggli VL (2018) Malignant mesothelioma diagnosed at a younger age is associated with heavier asbestos exposure. Carcinogenesis 39(9):1151–1156
Magge D, Zenati MS, Austin F, Mavanur A, Sathaiah M, Ramalingam L et al (2014) Malignant peritoneal mesothelioma: prognostic factors and oncologic outcome analysis. Ann Surg Oncol 21(4):1159–1165
Kaya H, Sezgi C, Tanrikulu AC, Taylan M, Abakay O, Sen HS et al (2014) Prognostic factors influencing survival in 35 patients with malignant peritoneal mesothelioma. Neoplasma 61(4):433–438
Laaksonen S, Ilonen I, Kuosma E, Sutinen E, Wolff H, Vehmas T et al (2019) Malignant pleural mesothelioma in Finland: regional and gender variation. Acta oncologica (Stockholm, Sweden) 58(1):38–44
Van Gerwen M, Alpert N, Wolf A, Ohri N, Lewis E, Rosenzweig KE, Flores R, Taioli E (2019) Prognostic factors of survival in patients with malignant pleural mesothelioma: an analysis of the National Cancer Database. Carcinogenesis. 40(4):529–536. https://doi.org/10.1093/carcin/bgz004
Rusch VW, Chansky K, Kindler HL, Nowak AK, Pass HI, Rice DC et al (2016) The IASLC mesothelioma staging project: proposals for the M descriptors and for revision of the TNM stage groupings in the forthcoming (Eighth) edition of the TNM classification for mesothelioma. J Thorac Oncol 11(12):2112–2119 (official publication of the International Association for the Study of Lung Cancer)
Kim J, Bhagwandin S, Labow DM (2017) Malignant peritoneal mesothelioma: a review. Ann Transl Med 5(11):236
Attanoos RL, Churg A, Galateau-Salle F, Gibbs AR, Roggli VL (2018) Malignant mesothelioma and its non-asbestos causes. Arch Pathol Lab Med 142(6):753–760
Cigognetti M, Lonardi S, Fisogni S, Balzarini P, Pellegrini V, Tironi A, Bercich L, Bugatti M, Rossi G, Murer B, Barbareschi M, Giuliani S, Cavazza A, Marchetti G, Vermi W, Facchetti F (2015) BAP1 (BRCA1-associated protein 1) is a highly specific marker for differentiating mesothelioma from reactive mesothelial proliferations. Mod Pathol 28(8):1043–1057
Carbone M, Ferris LK, Baumann F, Napolitano A, Lum CA, Flores EG et al (2012) BAP1 cancer syndrome: malignant mesothelioma, uveal and cutaneous melanoma, and MBAITs. J Transl Med 10:179
Scharmach M, Neumann V, Muller KM, Fischer M (2006) Comparison of patterns of metastasis between malignant pleural mesotheliomas and pulmonary carcinomas. Pneumologie (Stuttgart, Germany) 60(5):277–283
Finn RS, Brims FJH, Gandhi A, Olsen N, Musk AW, Maskell NA et al (2012) Postmortem findings of malignant pleural mesothelioma: a two-center study of 318 patients. Chest 142(5):1267–1273
Sugarbaker PH, Turaga KK, Alexander HR Jr, Deraco M, Hesdorffer M (2016) Management of malignant peritoneal mesothelioma using cytoreductive surgery and perioperative chemotherapy. J Oncol Pract 12(10):928–935
Acherman YI, Welch LS, Bromley CM, Sugarbaker PH (2003) Clinical presentation of peritoneal mesothelioma. Tumori 89(3):269–273
Manzini Vde P, Recchia L, Cafferata M, Porta C, Siena S, Giannetta L et al (2010) Malignant peritoneal mesothelioma: a multicenter study on 81 cases. Ann Oncol 21(2):348–353 (official journal of the European Society for Medical Oncology / ESMO)
Najmi K, Khosravi A, Seifi S, Emami H, Chaibakhsh S, Radmand G et al (2014) Clinicopathologic and survival characteristics of malignant pleural mesothelioma registered in hospital cancer registry. Tanaffos 13(2):6–12
Bibby AC, Tsim S, Kanellakis N, Ball H, Talbot DC, Blyth KG et al (2016) Malignant pleural mesothelioma: an update on investigation, diagnosis and treatment. Euro Respir Rev 25(142):472–486 (an official journal of the European Respiratory Society)
Rice D, Chansky K, Nowak A, Pass H, Kindler H, Shemanski L et al (2016) The IASLC Mesothelioma staging project: proposals for revisions of the N descriptors in the forthcoming eighth edition of the TNM classification for pleural mesothelioma. J Thorac Oncol 11(12):2100–11 (official publication of the International Association for the Study of Lung Cancer)
Yan TD, Deraco M, Elias D, Glehen O, Levine EA, Moran BJ et al (2011) A novel tumor-node-metastasis (TNM) staging system of diffuse malignant peritoneal mesothelioma using outcome analysis of a multi-institutional database*. Cancer 117(9):1855–1863
Berzenji L, Van Schil P. Multimodality treatment of malignant pleural mesothelioma. F1000Res. 2018;7:F1000 Faculty Rev-1681. https://doi.org/10.12688/f1000research.15796.1.
Zhao ZY, Zhao SS, Ren M, Liu ZL, Li Z, Yang L (2017) Effect of hyperthermic intrathoracic chemotherapy on the malignant pleural mesothelioma: a systematic review and meta-analysis. Oncotarget 8(59):100640–100647
de Gooijer CJ, Baas P, Burgers JA (2018) Current chemotherapy strategies in malignant pleural mesothelioma. Transl Lung Cancer Res 7(5):574–583
Perrot M, Wu L, Wu M, Cho BCJ (2017) Radiotherapy for the treatment of malignant pleural mesothelioma. Lancet Oncol 18(9):e532–e542
Garcia-Fadrique A, Mehta A, Mohamed F, Dayal S, Cecil T, Moran BJ (2017) Clinical presentation, diagnosis, classification and management of peritoneal mesothelioma: a review. J Gastrointest Oncol 8(5):915–924
Brenner J, Sordillo PP, Magill GB (1981) Malignant mesothelioma in children: report of seven cases and review of the literature. Med Pediatr Oncol 9(4):367–373
Fraire AE, Cooper S, Greenberg SD, Buffler P, Langston C (1988) Mesothelioma of childhood. Cancer 62(4):838–847
Silberstein MJ, Lewis JE, Blair JD, Graviss ER, Brodeur AE (1983) Congenital peritoneal mesothelioma. J Pediatr Surg 18(3):243–245
Coffin CM, Dehner LP (1992) Mesothelial and related neoplasms in children and adolescents: a clinicopathologic and immunohistochemical analysis of eight cases. Pediatr Pathol 12(3):333–347
Menut P, Herve JM, Barbagelata M, Botto H (1996) Bilateral malignant mesothelioma of the tunica vaginalis testis Apropos of a case. Prog Urol 6(4):587–9 (journal de l'Association francaise d'urologie et de la Societe francaise d'urologie)
Del Gobbo A, Fiori S, Gaudioso G, Bonaparte E, Tabano S, Palleschi A et al (2014) Synchronous pleural and peritoneal malignant mesothelioma: a case report and review of literature. Int J Clin Exp Pathol 7(5):2484–2489
Roberts GH (1976) Distant visceral metastases in pleural mesothelioma. Br J Dis Chest 70(4):246–250
Rice DC, Erasmus JJ, Stevens CW, Vaporciyan AA, Wu JS, Tsao AS et al (2005) Extended surgical staging for potentially resectable malignant pleural mesothelioma. Ann Thorac Surg 80(6):1988–92 (discussion 92-3)
Baratti D, Kusamura S, Cabras AD, Dileo P, Laterza B, Deraco M (2009) Diffuse malignant peritoneal mesothelioma: Failure analysis following cytoreduction and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol 16(2):463–472
Sugarbaker PH (2017) Intra-abdominal manifestations of pleural mesothelioma. Ann Transl Med 5(11):231
Author information
Authors and Affiliations
Contributions
Conceptualization: E.P., A.B., B.R. Methodology: E.P, M.E.A.V., A.B. Formal analysis and investigation: E.P., M.E.A.V., A.B., A.A. Writing — original draft preparation: E.P., M.E.A.V, A.B. Writing — review and editing: All authors: resources and supervision: A.B., B.R.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alberto Vilchez, M.E., Pachmayr, E., Arnold, A. et al. Synchronous Pleural and Peritoneal Mesothelioma: a Case Report and Narrative Review. Indian J Surg Oncol 14 (Suppl 1), 97–105 (2023). https://doi.org/10.1007/s13193-022-01637-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-022-01637-0