Abstract
Fine-needle aspiration biopsy (FNAB) is the first-line modality in the evaluation of thyroid nodules. However, the results of indeterminate pathology place the thyroid surgeon in difficult management situations. This study evaluates McGill Thyroid Nodule Score (MTNS) to identify thyroid nodules that harbor malignancy in cases of indeterminate FNABs and to guide surgeon about the need and extent of surgery. We conducted a retrospective chart review of 344 patients who underwent total thyroidectomy between January 2013 and January 2018. Patients with FNAB of indeterminate nodules (Bethesda types III, IV, and V) and calculated MTNS were included in the study. Postoperative histopathology was divided into benign and malignant groups. The median and the mean MTNS, the malignancy rate, and the standard deviations were calculated for each subgroup. Of the 344 patient charts reviewed, 106 (30.8%) had an indeterminate FNA biopsy. Eighty-one (76.4%) patients were females and 25 (23.6%) were males. Final pathology revealed malignancy in 69 patients (65.1%). The mean MTNS of patients with malignant pathology (12.81 ± 3.55) was higher than the mean in the benign group (8.32 ± 2.32). 82.4% of thyroid nodules with median MTNS of less than 8 had a benign pathology, and 91.4% of thyroid nodules with median MTNS equal or more than 11 had a malignant pathology (p = 0.002). The rate of malignancy in our series of indeterminate FNABs was 65.1%. The MTNS can be of value to thyroid surgeons in preoperative decision-making when dealing with an indeterminate thyroid nodule.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
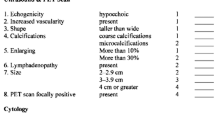
Thyroid cancer is the most common endocrine malignancy. Its incidence is steadily been rising over the last four decades [1, 2]. Data from the National Cancer Registry have shown a significant increase in the rate of thyroid malignancy [3]. Thyroid malignancy is the second most common cancer in females after breast cancer and its incidence has also been increasing in males [3]. The rise of thyroid malignancy appears to be a worldwide phenomenon. Ultrasound-guided fine-needle aspiration biopsy (USFNA) is the gold standard in the assessment and management of thyroid nodules [4]. Biopsy results are categorized into three main groups: benign, malignant, or indeterminate. According to the Bethesda system for reporting thyroid cytopathology, the indeterminate group of FNAB results consists of Bethesda type III, atypia of undetermined significance (AUS); type IV, follicular lesion of undetermined significance (FLUS); follicular neoplasm or suspicious for follicular neoplasm (FN); Hurthle cell neoplasm (HN), and type V, suspicious for malignancy. The management decision and counseling in cases of benign or malignant FNAB results is almost clear for the surgeon and the patients. The indeterminate results that accounted for average 25% of thyroid nodule biopsies are challenging concerning diagnosis and management [5]. The risk of malignancy with these types ranges from 10 to 70% [6]. Improvement in the assessment of indeterminate FNA results with molecular testing allows for better risk stratification, reduces the need for diagnostic thyroid surgery, and guides the surgeon about the extent of surgery [6, 7]. With such dilemma in the diagnosis and management of indeterminate thyroid nodules, it is crucial to find a complementary clinical tool to evaluate the risk of malignancy and select patients who require surgery and help to decide the type of surgery. The McGill Thyroid Nodule Score (MTNS) was developed by a multidisciplinary committee at the McGill University to estimate the malignancy risk of a thyroid nodule. This non-validated scoring system uses evidence-based risk factors according to the American Thyroid Association guidelines as well as the literature review. It combines patient history, demographics, imaging, and FNA results [8]. Each of the 22 variables in the MTNS is assigned a weighted, relative point score based on the current supporting evidence for that risk factor as demonstrated in Fig. 1. The MTNS has been shown to correlate with the malignancy risk in a large series of patients [8]. McGill Thyroid Nodule Score can be used as a tool to guide the management of indeterminate risk thyroid nodules. This study aims to assess the utility of the MTNS in predicting the rate of thyroid malignancy preoperatively in cases of indeterminate FNAB and thus will help to differentiate benign from malignant thyroid nodules. This will guide the surgeon in doing the appropriate surgery and avoiding unwarranted surgical procedures in those that contain benign pathology. Besides, the utility of MTNS preoperatively will clarify the communication between surgeons and patients.
Materials and Methods
We performed a retrospective review of 344 patients who underwent total thyroidectomy at the Section of Otolaryngology-Head and Neck Surgery, King Abdulaziz Medical City, Jeddah, Kingdom of Saudi Arabia, between January 2013 and January 2018. The study received approval from the institutional review board (IRB) of King Abdullah International Medical Research Center (Reference No. IRBC/2169/18). One hundred six patients (30.8%) met the inclusion criteria that consisted of having Bethesda types (III, IV, and V), FNA biopsy results, and preoperative calculated MTNS. In our center, the pathologist performed most of FNA biopsies in the pathology department. In selected cases, the interventional radiologist performed FNA biopsies under ultrasound (US) guide as the nodule was not clinically palpable or the suspicious nodule is difficult to be done without US guide, or the previous result was not satisfactory. The study excluded all cases of benign (Bethesda type II) and malignant (Bethesda type VI) FNAB. Patients who had missing, irretrievable, or incomplete data were excluded from the study. Collected information on the MTNS was based on a scoring sheet that has been filled out retrospectively from the database charts (see Fig. 1). Positron emission tomography (PET) scan and BRAF mutation are the two MTNS variables that are not routinely measured. We divided the postoperative results into benign and malignant based on the permanent pathology. Documentation of the site of FNA allowed us to ensure malignancy and was assigned to the same site nodule that was biopsied, thus avoiding falsely assigning malignancy to benign nodules in patients with multinodular thyroid glands. The malignancy rate, the median and the mean MTNS, and the standard deviations were calculated for each subgroup. Data were collected and analyzed using the Statistical Package for Social Sciences Version 21.0 (SPSS Inc., Chicago, IL, USA). For comparative analysis, we used the Pearson chi-square and independent sample student t test. All tests were two-tailed and the p value of < 0.05 was considered significant.
Results
Of the 344 charts reviewed, 106 patients (30.8%) met the inclusion criteria. There were 81 (76.4%) female patients and 25 (23.6%) male patients, with a mean age of 43.6 years (range, 10 to 87 years) ± 15.4 standard deviation (SD). Distribution of Bethesda types (III, IV, and V) FNA biopsy results were demonstrated in Table 1. MTNS ranged from 5 to 24, with a mean value and standard deviation (SD) of 11.20 ± 2.63. Final pathology revealed malignancy in 69 patients (65.1%), while 37 (34.9%) were benign. Benign and malignant rates and densities for each MTNS are presented in Table 2. The mean of the cumulative MTNS of patients with malignant pathology (12.81 ± 3.55) was higher than the mean of patients in the benign group (8.32 ± 2.32) (see Table 3). 82.4% of thyroid nodules with median MTNS of less than 8 had a benign pathology post-surgery, and 91.4% of thyroid nodules with median MTNS equal or more than 11 had a malignant pathology. Benign nodules with median MTNS less than 8 were significantly more than malignant nodules (p = 0.002) (see Tables 4 and 5). 31/106 (29.2%) patients had median MTNS values between 8 and 10. Eighteen (58.1%) out of those had benign pathology and 13 (41.9%) had malignancy. All thyroid nodules have MTNS more than 14.
Discussion
Fine-needle aspiration biopsy (FNAB) is the gold standard in the evaluation of thyroid nodules [9]. Up to 30% of fine-needle aspiration biopsies were diagnosed as indeterminate thyroid lesions [10]. Based on the Bethesda System for Reporting Thyroid Cytopathology, indeterminate thyroid nodules encompass atypia of undetermined significance/follicular lesion of undetermined significance (AUS/FLUS; Bethesda category III); follicular neoplasm or suspicious for a follicular neoplasm (FN/SFN; Bethesda category IV); and suspicious for malignancy (SM; Bethesda category V). When an FNA biopsy indicates an indeterminate result, the risk of malignancy is often uncertain [5]. Zarif et al. in a national study documented a 50%, 52%, and 95.7% incidence of malignancy in Bethesda III–V, respectively [11]. This high rate of malignancy in Bethesda III and IV could be related to a high threshold in some cytopathologists to make a diagnosis of malignancy and a low threshold of the treating physicians in deciding to refer patients directly to surgery without repeating the FNA [11]. The higher rate observed in Bethesda V could relate to sampling issues and variable experience with techniques of aspiration between pathologists along with differences in interpretation of findings [11]. In the literature, the reported malignancy rates for Bethesda III category vary widely, from a similar rate of 50% [12] to higher rates of 79% [13] as well as much lower rates of 5–15% in the Bethesda System for Reporting Thyroid Cytopathology (BSRTC) definition and 15.9% in a meta-analysis [14, 15]. The reported malignancy rates associated with Bethesda IV category vary from 50 [16] to 79% [13] with lower rates of 15–30% given in the BSRTC definition and 26.1% reported in a meta-analysis [15]. Besides, the reported malignancy rates associated with Bethesda V category vary from 60 to 75% given in the BSRTC definition or the 75.2% reported in a meta-analysis [14, 15]. Traditionally, most patients with indeterminate nodules have been referred for diagnostic surgery, even though most of these nodules ultimately prove to be benign by surgical histopathology [16]. So, the risk of malignancy needs to be weighed against the risk of serious surgical complications such as recurrent laryngeal nerve injury, hypocalcemia, and the lifelong need for thyroid hormone replacement [17]. Our study shows that 30.8% of patients with preoperative FNA results are indeterminate (Bethesda III, IV, and V) which is within the average rate that reported in the literature [18]. In our series, 82.4% of thyroid nodules with median MTNS of less than 8 had a benign pathology post-surgery, and 91.4% of thyroid nodules with median MTNS equal or more than 11 had a malignant permanent pathology. Although many would argue that there is a malignancy risk in all, the difference lies in the mode of intervention to be decided. In cases of a median MTNS of less than 8 with 32% risk of malignancy risk, a diagnostic hemithyroidectomy would most likely be the therapeutic option chosen [5]. While in cases of a median MTNS more or equal to 11 with 88% risk of malignancy, a discussion with patients about the utility of a total thyroidectomy may be advocated, precluding the need for completion thyroidectomies in cases of malignancy [5]. Despite this, the challenge in the decision in our study was in the thyroid nodules with median MTNS values between 8 and 10 that accounted for 29.2% as the malignancy risk that was statistically not significant. The overall malignancy rate in our series of indeterminate nodules was 65.1% which was similar to the national study done by Zarif et al. [11] and higher than most of the reported malignancy rate in the literature [19,20,21,22]. This wide range of reported malignancy may be explained by variations in technique, expertise, and subjective interpreting differences between pathologists reading the slides and physicians performing ultrasounds and FNABs with or without US guide in different institutions [23]. The high rate (30.8%) of indeterminate nodules in our series along with a significant incidence of malignancy (65.1%) within this population reinforces the need for ancillary objective tools to help guide management. There has been a rise in diagnostic tests available to thyroid specialists in the past few years. Genetic markers and molecular analysis were tools that can help in cases of indeterminate nodules. One such tool is the 4-gene classifier (BRAF, RET/PTC, PAX8/PPARϒ, and RAS) [24]. Genetic markers have high specificity and positive predictive value and can improve diagnostic accuracy [19]. However, they have low sensitivity and negative predictive value [25, 26]. A more recent advancement is the Afirma gene expression classifier (Veracyte, Inc., San Francisco, USA) which measures mRNA transcript expression levels of 142 genes [5, 19]. It has shown to have high sensitivity with moderate specificity [19]. Nonetheless, a major obstacle to their widespread use is the high costs associated with such tests [19]. Another tool available to guide clinical management of thyroid nodules is MTNS [8]. The MTNS is based on risk factors according to the American Thyroid Association guidelines as well as the literature review on thyroid malignancy risk factors. There are factors that limit the generalization of this study including heterogeneity of the specimens and subjectivity in calculating MTNS which may affect the statistics of the results. In addition, MTNS is non-validated scoring system, and not all patients that were seen at our institution have a calculated MTNS, resulting in patients being excluded from the analysis. For those challenges and the importance of dealing with such group of thyroid nodules that harbor a significant risk of malignancy, modern diagnostic tests to help direct the need for and extent of surgery are crucial.
Conclusion
Our study showed that indeterminate thyroid lesions accounted in about one third of fine-needle aspirations with a variable rate of malignancy were challenging in their management. The MTNS was able to demonstrate an increased preoperative risk of malignancy for nodules that found to be malignant. Based on these results, we suggest that the MTNS be considered as a tool to guide the management of indeterminate thyroid nodules, as it not only refines the preoperative estimated risk of malignancy but also clarifies communication between physicians and patients.
References
Mao Y, Xing M (2016) Recent incidences and differential trends of thyroid cancer in the USA. Endocr Relat Cancer 23:313–322. https://doi.org/10.1530/ERC-15-0445
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30. https://doi.org/10.3322/caac.21332
Hussain F, Iqbal S, Mehmood A, Bazarbashi S, ElHassan T, Chaudhri N (2013) Incidence of thyroid cancer in the Kingdom of Saudi Arabia, 2000-2010. Hematol Oncol Stem Cell Ther 6:58–64. https://doi.org/10.1016/j.hemonc.2013.05.004
Kloos RT, Reynolds JD, Walsh PS, Wilde JI, Tom EY, Pagan M, Barbacioru C, Chudova DI, Wong M, Friedman L, LiVolsi V, Rosai J, Lanman RB, Kennedy GC (2013) Does addition of BRAF V600E mutation testing modify sensitivity or specificity of the Afirma gene expression classifier in cytologically indeterminate thyroid nodules? J Clin Endocrinol Metab 98:E761–E768. https://doi.org/10.1210/jc.2012-3762
Varshney R, Forest VI, Mascarella MA, Zawawi F, Rochon L, Hier MP, et al. The Mcgill thyroid nodule score - does it help with indeterminate thyroid nodules? J Otolaryngol Head Neck Surg 2015; 3;44:2. doi: https://doi.org/10.1186/s40463-015-0058-6
Cibas ES, Ali SZ (2017) The 2017 Bethesda system for reporting thyroid cytopathology. Thyroid 27:1341–1346. https://doi.org/10.1089/thy.2017.0500
Valderrabano P, Mclver B (2017) Evaluation and management of indeterminate thyroid nodules: the revolution of risk stratification beyond cytological diagnosis. Cancer Control 24:1073274817729231. https://doi.org/10.1177/1073274817729231
Sands NB, Karls S, Amir A, Tamilia M, Gologan O, Rochon L, et al. McGill Thyroid Nodule Score (MTNS): “rating the risk,” a novel predictive scheme for cancer risk determination. J Otolaryngol Head Neck Surg 2011; 40 (Suppl 1):S1–13
Pezolla A, Lattarulo S, Madaro A, Docimo G, Lacalendola E, Prete F et al (2017) What really is an indeterminate FNA thyroid nodule? Ann Ital Chir 88:275–281
Hegedus L (2004) Clinical practice. The thyroid nodule. N Engl J Med 351:1764–1771
Zarif HA, Ghandurah SE, Al-Garni MA, Binmahfooz SK, Alsaywid BS, Satti MB (2018) Thyroid nodules cytopathology applying the Bethesda system with histopathological correlation. Saudi J Med Sci 6:143–148
Mufti ST, Molah R (2012) The Bethesda system for reporting thyroid cytopathology: a five-year retrospective review of one center experience. Int J Health Sci (Qassim) 6:159–173
Lee K, Jung CK, Lee KY, Bae JS, Lim DJ, Jung SL (2010) Application of Bethesda system for reporting thyroid aspiration cytology. Korean J Pathol 44:521–527
Cibas ES, Ali SZ; NCI Thyroid FNA State of the Science Conference. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol 2009;132:658–665
Bongiovanni M, Spitale A, Faquin WC, Mazzucchelli L, Baloch ZW (2012) The Bethesda system for reporting thyroid cytopathology: a meta-analysis. Acta Cytol 56:333–339
Park JH, Yoon SO, Son EJ, Kim HM, Nahm JH, Hong S et al (2014) Incidence and malignancy rates of diagnoses in the Bethesda system for reporting thyroid aspiration cytology: an institutional experience. Korean J Pathol 48:133–139
Baloch ZW, LiVolsi VA, Asa SL, Rosai J, Merino MJ, Randolph G, Vielh P, DeMay R, Sidawy MK, Frable WJ (2008) Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: a synopsis of National Cancer Institute Thyroid Fine-Needle Aspiration State of the Science Conference. Diagn Cytopathol 36:425–437. https://doi.org/10.1002/dc.20830
Alexander EK, Kennedy GC, Baloch ZW, Cibas ES, Chudova D, Diggans J et al (2012) Preoperative diagnosis of benign thyroid nodules with indeterminate cytology. N Engl J Med 3(67):705–715. https://doi.org/10.1056/NEJMoa1203208
Li H, Robinson KA, Anton B, Saldanha IJ, Ladenson PW (2011) Cost-effectiveness of a novel molecular test for cytologically indeterminate thyroid nodules. J Clin Endocrinol Metab 96:E1719–E1726. https://doi.org/10.1210/jc.2011-0459
Rossi M, Buratto M, Bruni S, Filieri C, Tagliati F, Trasforini G, Rossi R, Beccati MD, Degli Uberti EC, Zatelli MC (2012) Role of ultrasonographic/clinical profile, cytology, and BRAF V600E mutation evaluation in thyroid nodule screening for malignancy: a prospective study. J Clin Endocrinol Metab 97:2354–2361. https://doi.org/10.1210/jc.2011-3494
Granados-Garcia M, Cortes-Flores AO, del Carmen G-RI, Cano-Valdez AM, Flores-Hernandez L, Aguilar-Ponce JL (2010) Follicular neoplasms of the thyroid: importance of clinical and cytological correlation. Cir Cir 78:473–478
Lee EK, Chung KW, Min HS, Kim TH, Ryu JS, Jung YS et al (2012) Preoperative serum thyroglobulin as a useful predictive marker to differentiate follicular thyroid cancer from benign nodules in indeterminate nodules. J Korean Med Sci 27:1014–1018. https://doi.org/10.3346/jkms.2012.27.9.1014
Sugino K, Ito K, Nagahama M, Kitagawa W, Shibuya H, Ohkuwa K, Yano Y, Uruno T, Akaishi J, Suzuki A, Masaki C, Ito K (2013) Diagnostic accuracy of fine needle aspiration biopsy cytology and ultrasonography in patients with thyroid nodules diagnosed as benign or indeterminate before thyroidectomy. Endocr J 60:375–382
Khalifa S, Bouhabel S, Forest VI, Hier MP, Rochon L, Tamilia M et al (2016) The McGill thyroid nodule Score's (MTNS+) role in the investigation of thyroid nodules with benign ultrasound guided fine needle aspiration biopsies: a retrospective review. J Otolaryngol Head Neck Surg 45:29. https://doi.org/10.1186/s40463-016-0141-7
Nikiforov YE, Ohori NP, Hodak SP, Carty SE, LeBeau SO, Ferris RL, Yip L, Seethala RR, Tublin ME, Stang MT, Coyne C, Johnson JT, Stewart AF, Nikiforova MN (2011) Impact of mutational testing on the diagnosis and management of patients with cytologically indeterminate thyroid nodules: a prospective analysis of 1056 FNA samples. J Clin Endocrinol Metab 96:3390–3397. https://doi.org/10.1210/jc.2011-1469
Daniels GH (2013) What is the role of molecular markers in the management of “indeterminate” thyroid nodules? Cancer Cytopathol 121:223–224. https://doi.org/10.1002/cncy.21289
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al-Hakami, H.A., Al-Mohammadi, R., Al-Mutairi, R. et al. McGill Thyroid Nodule Score in Differentiating Thyroid Nodules in Total Thyroidectomy Cases of Indeterminate Nodules. Indian J Surg Oncol 11, 268–273 (2020). https://doi.org/10.1007/s13193-020-01053-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-020-01053-2