Abstract
Thyroidectomy conventionally accompanies total laryngectomy. This study intends to analyze the incidence and factors leading to thyroid gland involvement in carcinoma larynx and hypopharynx. Retrospective chart review from March 2011 to December 2016 of all patients who had undergone total laryngectomy at our institute. A total of 125 patients entered into the analysis. Subsites involved were glottis (n = 32), supraglottis (n = 28), transglottis (n = 52), pyriform sinus (n = 12), and subglottis (n = 1). TNM distribution according to AJCC 7th edition is as follows: T2 (n = 1), T3 (n = 34), T4 (n = 90); N0 (n = 97), N1 (n = 13), N2a (n = 5), N2b (n = 5), N2c (n = 4), and N3 (n = 1). Total thyroidectomy was performed in 16 patients, near total thyroidectomy in 5, and hemithyroidectomy in 104. Histopathologically thyroid gland involvement was seen in 11/125 (8.8%). The overall incidence of hypothyroidism was 48% (hemithyroidectomy, 43/104; total thyroidectomy, 16/16; near total thyroidectomy, 1/5). The incidence of permanent hypoparathyroidism was 12.8% (total thyroidectomy, 11; hemithyroidectomy, 5). On multivariate analysis (Cox proportional hazards model), extralaryngeal spread into level 6 (HR = 5.5, p = .006, C.I = 1–18.8) and extracapsular extension (HR = 9.3, p = 0.02, C.I = 1.29–67.5) were statistically significant predictors for thyroid gland involvement. Survival analysis of patients with thyroid gland involvement (n = 11) revealed 5-year overall survival (OS) of 100% and 5-year disease-free survival (DFS) of 59.3% compared with patients without thyroid gland involvement, 71% and 51.7%, respectively (median follow-up, 30 months). Thyroid gland involvement did not show a statistically significant effect on OS/DFS on multivariate analysis. In view of the endocrine abnormalities and lack of survival benefit seen, thyroidectomy should be performed judiciously during total laryngectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
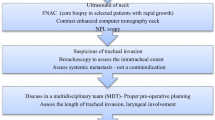
Total laryngectomy (TL) with neck dissection guided by the nodal status of individual patients is the standard of care for locally advanced laryngeal or hypopharyngeal cancers not suitable for organ-preservation modalities [1, 2]. A hemithyroidectomy invariably accompanies total laryngectomy, with total thyroidectomy being reserved for cases with involvement of anterior commissure, post-cricoid area, subglottis, and direct extension to thyroid gland and level VI nodal involvement [3]. Arguments put forth to justify thyroid gland sacrifice include better access to the central compartment and the possibility of tumor spread to the thyroid gland either by direct spread or extension via lymphatics [4]. It has been observed by many investigators that the incidence of thyroid gland involvement (TGI) ranges between 8 and 12.6% [5]. These figures definitely challenge the age-old practice of thyroid gland sacrifice for all cases requiring TL. Thyroidectomy whether hemi or total has been shown to be associated with hypothyroidism and hypoparathyroidism [6, 7]. The incidence of thyroid and parathyroid insufficiency is higher in the setting of adjuvant radiation or chemoradiation [8]. This calls for proper guidelines to tailor thyroid gland resection in patients at risk for TGI. This study endeavors to identify the factors predicting TGI and analyze the impact of thyroid and parathyroid insufficiency following sacrifice of thyroid gland routinely during TL.
Methods
This study was performed on a retrospective cohort of patients who had undergone TL for laryngeal or hypopharyngeal cancers at a tertiary care referral center from March 2011 to December 2016. Pre-operative factors which could contribute to TGI and were considered for the analysis were T and N classification (as per AJCC 7th edition) and pre-operative tracheostomy. Tumor extent was retrieved from the records of direct laryngoscopy, cross-sectional imaging, and intraoperative assessment to look for subglottic extension, hypopharyngeal involvement, and extralaryngeal spread (ELS) to the central compartment. Histopathological parameters taken into account were margin status, extracapsular spread (ECE), perineural invasion (PNI), and lymphovascular emboli (LVI). TGI status was identified from histopathology.
Serum thyroid stimulating hormone (TSH) levels were obtained on the last follow-up. Hypoparathyroidism was determined by corrected calcium levels and requirement of calcium and vitamin D3 requirements 1 year after surgery.
Survival analysis was performed using the Kaplan-Meier method. Comparison between survival curves of two different cohorts was done using the log-rank test. Factors predictive of TGI were determined using the Cox proportional hazards model. All statistical analysis was performed using MedCalc statistical software ver 18.10.2.
Results
A total of 178 patients with carcinoma larynx and hypopharynx had undergone TL during the study period. Complete data with regard to tumor extent, histopathology, and follow-up status was available for 125 patients. This series included 13 patients where TL was performed as a salvage procedure. Patient and tumor characteristics have been enumerated in Table 1.
Factors Associated with Thyroid Gland Involvement
Thyroid gland abnormality was noted in 12/125 (9.6%) patients. Of these squamous cell carcinomas, secondary to carcinoma larynx was seen in 11 (8.8%) and papillary thyroid microcarcinoma in 1 patient. Subsites implicated in these 11 cases were transglottis (TGL), 7 (odds ratio = 2.68, p = 0.19), pyriform sinus (PFS), 1 (odds ratio = 0.93, p = 1); glottis, 2 (odds ratio = 0.622, p = 0.72); and supraglottis (SGL), 1 (odds ratio = 0.32, p = 0.45). Multivariate analysis was performed for possible predictive factors indicating TGI using Cox proportional hazards model. The variables considered were as follows: ECE, PNI, LVI, ELS into the central compartment, pathologically positive neck nodes (pN+), subglottic extension, hypopharyngeal involvement, and pre-operative tracheostomy (Fig. 1). Statistically significant association with TGI was seen in ECE (HR = 9.3, 95% C.I = 1.29–67.5, p = 0.02) and ELS into the central compartment (HR = 5.5, 95% C.I = 1.1–18.88, p = 0.006).
Forest plot depicting the results of a multivariate analysis of factors predicting thyroid gland involvement in carcinoma larynx and hypopharynx. The center of the square depicts the odds ratio. Horizontal line for each variable represents the 95% confidence interval. Horizontal line crossing the number “1” on X-axis represents a statistically insignificant result. ECE extracapsular spread, ELS extralaryngeal spread to the central compartment, pN+ pathologically positive neck nodes
Oncological Outcomes
With a median follow-up time of 30 months, 5-year overall survival (OS) and disease-free survival (DFS) for the entire cohort were 81.9% and 58.5%, respectively (Fig. 2). The corresponding 5-year survival for the 13 cases of salvage laryngectomies were 59.3% and 47.3%, respectively. For the entire cohort, failure at the local site was seen in 10 patients, nodal recurrence in 9 patients, distant metastasis in 7, and second primary in 6 cases. A separate subset analysis was performed for patients with and without TGI (TG+/TG−). No statistically significant difference was seen between the two groups with respect to the pattern of failure (p > 0.05) (Table 2). Survival analysis of TG+ revealed 5-year OS of 100% and 5-year DFS of 59.3% compared with the cohort of TG− which showed corresponding outcomes of 71% and 51.7%, respectively (p > 0.05) (Fig. 2). Another multivariate analysis was performed to look for prognostic variables associated with oncological outcomes. Of the various factors considered, pre-operative tracheostomy (HR = 0.15, p = 0.006, 95% C.I = 0.03–0.59) and PNI (HR = 5.1, p = 0.04, 95% C.I = 1.07–24.48) had statistically significant correlation with OS and DFS, respectively (Table 3). TGI was not associated with negative survival outcomes as evident in the multivariate analysis.
Kaplan-Meier survival analysis. a, b Overall survival (red) and disease-free survival (blue) for the entire cohort and following salvage laryngectomy. Dotted lines represent 95% confidence interval. c, d Overall survival (OS) and disease-free survival (DFS) for patients with thyroid gland involvement (blue) and without thyroid gland involvement (red)
Endocrinological Aspects
Hypothyroidism as assessed by serum TSH at last follow-up was seen in 60/125 (48%) patients, and the mean TSH was 50.69 mIU/L (SD = 43.3, range 7.8–177mIU/L). The incidence of permanent hypothyroidism based on the type of thyroidectomy performed was as follows: hemithyroidectomy (43/104), total thyroidectomy (16/16), and near total thyroidectomy (1/5). Permanent hypoparathyroidism was seen in 16/125 (12.8%) patients (total thyroidectomy, 11; near total thyroidectomy, 5). Amongst patients with TGI (11/125), hypothyroidism was seen in all patients and hypoparathyroidism in 2 patients.
Discussion
We have identified an 8.8% incidence of TGI in a consecutive series of 125 patients of carcinoma larynx and hypopharynx following TL with some form of thyroid gland sacrifice. Such a routine sacrifice of the thyroid gland was associated with a 48% incidence of hypothyroidism and 12.8% incidence of hypoparathyroidism. From an oncological point of view, TGI did not emerge to be an independent prognostic factor. In addition, no statistically significant difference was seen between TG+ and TG− patients in terms of the pattern of failure and overall survival outcomes. Our multivariate analysis model identified ECE and ELS to central compartment as predictors of TGI. In other words, thyroidectomy and its associated endocrinological derangements can be avoided if thyroidectomy is tailored to patients with risk factors for TGI while planning TL.
Studies analyzing the whole organ section of laryngectomy specimens have established that direct spread of carcinoma to the thyroid gland is the most common route of spread [9]. This spread occurs through anatomically weak, preformed pathways in the laryngeal framework like the thyrohyoid membrane, cricothyroid membrane, and the anterior commissure [9,10,11]. To involve the thyroid gland, malignant cells need to traverse the central compartment. Based on these studies and supplemented by the results of our multivariate analysis, thyroid gland sacrifice can be avoided if ELS to the central compartment is effectively ruled out by radiology and intraoperative assessment. Similarly, in the presence of ECE which signifies loco-regional burden of the disease, it is wise to sacrifice the thyroid gland not only due to the possibility of harboring metastasis but also to enable a meticulous central compartment clearance. The ability to identify anterior ELS on computed tomography with a high positive and negative predictive value was identified by Harris et al. [12]. Anterior ELS has emerged as a very reliable predictor of TGI in numerous studies [3, 10, 13], unlike the mere presence of cartilage erosion and hypopharyngeal involvement. Subglottic extension was also evaluated for its association with TGI by multivariate analysis in our study. Though numerous studies including two meta-analyses have found a significant association with TGI [5, 14], this present study failed to corroborate this particular result. Majority of the patients undergoing TL will have thyroid cartilage erosion by virtue of being T4. Also in the era of organ preservation, concurrent chemoradiation is the norm for the majority of the patients with T3 disease. Therefore, though the absence of cartilage erosion has a 100% negative predictive value towards TGI, its presence does not provide enough information about thyroid gland metastasis owing to a positive predictive value of 52.9% [12]. Therefore, based on the available literature and results of this study, we would like to recommend total thyroidectomy in the presence of extralaryngeal spread to the central compartment (intraoperative/radiology), extracapsular extension, and subglottic involvement. Due to extensive lymphatic communication between the two lobes of the thyroid gland, hemithyroidectomy in the presence of any of the above-mentioned risk factors may jeopardize oncological outcomes. In case of hypopharyngeal extension, we would like to suggest incorporating a hemithyroidectomy on the ipsilateral side to facilitate the clearance of paratracheal lymph nodes [15, 16].
Of all the studies reviewed [3, 10, 11, 13], the incidence of TGI ranged from 8 to 18% and pooled results from a meta-analysis by Kumar et al. [14], quoted an incidence of 10.7%. Therefore, owing to the relative rarity of TGI, very few studies have performed long-term survival analysis on cohorts with TGI. The present study as well as the series by Nayak et al. [10] did not reveal any significant difference in terms of survival depending on TGI. In contrast, Gorphe et al. [3] revealed survival outcomes to be poorer if TGI is present. To study the effect TGI has on oncological outcomes, we have adjusted for confounders and performed a multivariate analysis with other possible poor prognostic factors, but did not find a statistically significant impact of TGI on OS or DFS.
The consequences hypothyroidism and hypoparathyroidism have on the quality of life and wound healing are profound [17, 18]. Surgery even in the absence of adjuvant radiotherapy can be associated with a 63% incidence of hypoparathyroidism and hypothyroidism [8]. Even in the setting of hemithyroidectomy accompanying TL, an incidence of hypothyroidism to the tune of 23–63% has been reported [19]. We did not encounter metastases to the parathyroid gland in our study. Therefore, in case of inadvertent parathyroid gland devascularization, one can attempt autotransplantation after frozen section confirmation. One needs to bear in mind that the management of hypoparathyroidism is much more troublesome than hypothyroidism [20]. In the face of such morbidity and questionable oncological benefits gained, it is necessary to restrict thyroidectomy to high-risk cases like ECE, ELS to the central compartment, and subglottic extension. Though the latter, did not emerge to be an independent risk factor in our analysis, such a conclusion has been drawn from the results of the systematic review on this subject [14].
Our study and other existing literature in this field are limited by the retrospective nature of the study design. Future studies should aim at prospective analysis with step serial sectioning of the thyroid gland to determine the true incidence of TGI.
Conclusion
The practice of indiscriminate sacrifice of the thyroid gland during TL needs to be reviewed due to the documented incidence of TGI ranging between 8 and 18%. We would like to suggest ECE, ELS to the central compartment, and subglottic extension as risk factors for TGI. Restricting thyroidectomy to these patients may strike a balance between oncological outcomes and endocrinological morbidity.
References
Spector GJ, Sessions DG, Lenox J, Newland D, Simpson J, Haughey BH (2004) Management of stage IV glottic carcinoma: therapeutic outcomes. Laryngoscope 114(8):1438–1446
Sessions DG, Lenox J, Spector GJ, Newland D, Simpson J, Haughey BH et al (2002) Management of T3N0M0 glottic carcinoma: therapeutic outcomes. Laryngoscope 112(7 Pt 1):1281–1288
Gorphe P, Ben Lakhdar A, Tao Y, Breuskin I, Janot F, Temam S (2015) Evidence-based management of the thyroid gland during a total laryngectomy. Laryngoscope 125(10):2317–2322
Fagan JJ, Kaye PV (1997) Management of the thyroid gland with laryngectomy for cT3 glottic carcinomas. Clin Otolaryngol Allied Sci 22(1):7–12
Mendelson AA, Al-Khatib TA, Julien M, Payne RJ, Black MJ, Hier MP (2009) Thyroid gland management in total laryngectomy: meta-analysis and surgical recommendations. Otolaryngol Head Neck Surg 140(3):298–305
Kim JW, Han GS, Byun SS, Lee DY, Cho BH, Kim YM (2008) Management of thyroid gland invasion in laryngopharyngeal cancer. Auris Nasus Larynx 35(2):209–212
Biel MA, Maisel RH (1985) Indications for performing hemithyroidectomy for tumors requiring total laryngectomy. Am J Surg 150(4):435–439
Thorp MA, Levitt NS, Mortimore S, Isaacs S (1999 Apr) Parathyroid and thyroid function five years after treatment of laryngeal and hypopharyngeal carcinoma. Clin Otolaryngol 24(2):104–108
Lam KH (1983) Extralaryngeal spread of cancer of the larynx: a study with whole-organ sections. Head Neck Surg 5(5):410–424
Nayak SP, Singh V, Dam A, Bhowmik A, Jadhav TS, Ashraf M et al (2013) Mechanism of thyroid gland invasion in laryngeal cancer and indications for thyroidectomy. Indian J Otolaryngol 65(Suppl 1):69–73
Li SX, Polacco MA, Gosselin BJ, Harrington LX, Titus AJ, Paydarfar JA (2017) Management of the thyroid gland during laryngectomy. J Laryngol Otol 131(8):740–744
Harris AS, Passant CD, Ingrams DR (2018) How reliably can computed tomography predict thyroid invasion prior to laryngectomy? Laryngoscope 128(5):1099–1102
Mangussi-Gomes J, Danelon-Leonhardt F, Moussalem GF, Ahumada NG, Oliveira CL, Hojaij FC (2017) Thyroid gland invasion in advanced squamous cell carcinoma of the larynx and hypopharynx. Braz J Otorhinolaryngol 83(3):269–275
Kumar R, Drinnan M, Robinson M, Meikle D, Stafford F, Welch A et al (2013) Thyroid gland invasion in total laryngectomy and total laryngopharyngectomy: a systematic review and meta-analysis of the English literature. Clin Otolaryngol 38(5):372–378
Joo YH, Sun DI, Cho KJ, Cho JH, Kim MS (2010) The impact of paratracheal lymph node metastasis in squamous cell carcinoma of the hypopharynx. Eur Arch Otorhinolaryngol 267(6):945–950
de Bree R, Leemans CR, Silver CE, Robbins KT, Rodrigo JP, Rinaldo A et al (2011) Paratracheal lymph node dissection in cancer of the larynx, hypopharynx, and cervical esophagus: the need for guidelines. Head Neck 33(6):912–916
Simcock R, Simo R (2016) Follow-up and survivorship in head and neck cancer. Clin Oncol 28(7):451–458
de Bree R, Lips P, Leemans CR (2008) The need for patients’ endocrine function vigilance following treatment of head and neck cancer. Curr Opin Otolaryngol 16(2):154–157
Cinar U, Yiğit O, Alkan S, Uslu B, Topuz E, Unsal O et al (2003) [The effect of laryngectomy and postoperative radiotheraphy on thyroid gland functions]. Ear Nose Throat 10(6):226–230
Abd Elmaksoud AE, Farahat IG, Kamel MM (2015) Parathyroid gland autotransplantation after total thyroidectomy in surgical management of hypopharyngeal and laryngeal carcinomas: a case series. Ann Med Surg (Lond) 4(2):85–88
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Panda, S., Kumar, R., Konkimalla, A. et al. Rationale behind thyroidectomy in total laryngectomy: analysis of endocrine insufficiency and oncological outcomes. Indian J Surg Oncol 10, 608–613 (2019). https://doi.org/10.1007/s13193-019-00935-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-019-00935-4