Abstract
Preoperative prediction of morbidity in colorectal cancer (CRC) surgery helps to optimize the surgical outcome. In this study, we aim to develop a dedicated equation for predicting operative morbidity using colorectal possum scoring system and also to validate the predictive accuracy of CR-POSSUM scoring system in prognosticating actual complications. We did a retrospective analysis of 322 patients undergoing colorectal cancer surgery from a single centre in South India from 2004 to 2016. Mortality and morbidity risk factors as defined by CR POSSUM were collected from 322 patients who underwent CRC surgery and were used to derive equations to predict morbidity, and the results were compared with the observed morbidity. Logistic regression analysis was used to derive the equation. The model fit and model discrimination were analysed using the Hosmer-Lemeshow statistical test for goodness of fit, the Nagelkerke R2 and area under the receiver operating characteristic (ROC) curve respectively. Out of 322 patients, 103 (32%) patients developed complications and 10 (3%) died due to complications. The regression equation we derived has an overall correct classification of about 70% (P < 0.01) with positive and negative predictive value of 60% and 73% respectively. The Hosmer-Lemeshow goodness of fit was 3.147 (P = 0.829), and the Nagelkerke R2 was 17% and area under ROC as model discrimination was 71.6%. Hence, CR-POSSUM scoring which was originally used for predicting mortality risk can also be extrapolated to predict morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal malignancy is the third most common malignancy among men and the second most common among women around the world [1]. Fortunately, in India, the incidence is not too high. However, the incidence has been found to be rising, with the AAR (adjusted annual incidence rate) for colon cancer in men and women being 4.4 and 3.9 per 100,000, respectively [2]. Being in a country, where people living with poor access to quality healthcare, extreme presentation like advanced stage and perforation are common in tertiary care centres [3, 4]. In such scenarios, the mortality and morbidity for the patients undergoing surgery are relatively high [5]. Complications following major surgeries will proportionately increase the hospital cost and duration of hospital stay [6]. Apart from such hardships, complications also had an adverse impact on long-term survival [7]. So in a country like India, where the spending on health by the government is low and health insurance is under-penetrated, morbidity following a major surgical procedure will further drain the already constrained resources [8]. The complication rates are not uniform and cannot be generalised, as there are certain factors, such as age, patients’ co-morbidity and operative severity, influencing the outcome of surgery [9]. So, putting together these factors and assessing the postoperative outcome preoperatively will help in optimizing the available resources. In such cases, the predictive scoring has to be more accurate, and its predictive ability should be proven in multiple centres. In our study, we devised a morbidity scoring system with already established parameters in CR-Possum which influence the outcome of colorectal surgery in terms of mortality and assessed the model calibration and discrimination with statistical analysis tools.
Patient and Methods
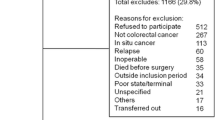
Data of 506 patients undergoing colorectal surgery for colorectal malignancy from January 2004 to December 2017 was collected from the medical records department of a single tertiary care centre. The in-patient files were analysed and the required variables as per CR-POSSUM scoring [physiologic severity score (PSS) (age, cardiac failure if any, systolic blood pressure, pulse, urea, haemoglobin) and operative severity score (OSS) (operative severity, peritoneal soiling, operative urgency, cancer staging in Dukes)] were collected and entered in an excel data sheet. Patient files, with single missing variable, were excluded from the study. Therefore, only 322 patients with complete details were included. The dichotomous outcome of each patient, either dead/alive, with/without complication, was entered. Presence or absence of complications, such as haemorrhage, wound infection, wound dehiscence, anastomotic leak, deep vein thrombosis, pulmonary embolus, cerebrovascular accident, myocardial infarction, cardiac failure, impaired renal function and respiratory failure were also entered. Complications were also graded based on Clavien-Dindo scale of surgical morbidity, and all grades were considered. Duration of hospital stay in terms of number of days for each patient was also recorded. The study was approved by institutional ethics committee.
Statistical Analysis
The data was analysed using SPSS version 24. Mean and standard deviation were calculated for continuous variables. Chi-square test was done to check association between categorical variables. The equation to predict morbidity was derived using multiple logistic regression analysis, and the model discrimination was measured by calculating the area under ROC (receiver operating characteristic) curve. The Nagelkerke R2 and the Hosmer-Lemeshow statistics were used for model calibration (goodness of fit). Positive and negative predictive values were also calculated. P < 0.05 was considered as statistically significant.
Results
Out of a total of 506 patients undergoing colorectal surgery for malignancy, 322 (63.2%) satisfied the criteria to be included in the study. Among the 322 patients, 103 (31.9%) developed complications and 10 (3%) patients died of complications. The average duration of hospital stay for all patients who underwent surgery was 15.5 days. The mean duration of in-hospital stay for patients with and without complications was 18 and 14.5 days respectively (P = 0.01) which was statistically significant. The proportion of patients with and without complications and in-hospital stay days are shown in Fig. 1. The summary of procedures and their associated complications were shown in Table 1. The complications rates were more in tumours located in sigmoid and rectum compared to other sites (P < 0.05). The complications were graded as per Clavin-Dindo classification. Wound-related complication tops the list (37%) followed by respiratory complications (18%). These are shown in Table 2. The patient’s demographic characteristics and the in-hospital morbidity rates for the factors taken into consideration for CR-POSSUM scoring are shown in Table 3. Majority of the patients are in the age group less than 60 years (51%) and there is a male preponderance (61%). Table 4 summarizes the CR-POSSUM scoring system which we used for the analysis. The equation we derived using above data was In (R/(1 − R)) = −4.83 + 0.09(PSS) + 0.35(OSS)(P < 0.001). The positive and negative predictive value of the equation was 60.87% and 73.09% respectively. The overall percentage of correct classification was 70%. The goodness of fit was looked at to check whether the predicted probability was assigned accordingly to individual patient’s outcome. The Hosmer-Lemeshow test statistics was 3.147 (P = 0.829) which was reasonably a good fit for higher the P value, more fit the model is. The Nagelkerke R2 which was another test to check goodness of fit was fairly good (17%). Model discrimination calculated by area under ROC curve was 71.6% (Fig. 2), which was reasonably a fair discrimination. The observed and expected ratio was almost close to 1 among the different range of predictions.
Discussion
POSSUM AND P-POSSUM were original scoring systems which enumerated the mortality and morbidity in a patient undergoing major surgeries [10, 11]. These have been validated in numerous studies outside the UK, and their value in surgical audit has been proven beyond doubt [12,13,14]. A study conducted by the American College of Surgeons (ACS-NSQIP) in 2005 to 2006 showed that ten procedure groups among various general surgical operations accounted for 62% of complications, and colectomy was topping in the list [15]. It accounts for 24% of adverse events. CR-POSSUM, developed by Tekkis et al., a modification in the original scoring system, was designed for enumeration of mortality in patients undergoing colorectal procedures [16]. Since the mortality following colorectal surgery was brought down with improvement in postoperative critical care but the morbidity following such procedures especially in patients undergoing emergency surgery for perforation and obstruction was considerably high [17]. Complication rates in surgery for colorectal malignancy elective and emergency were 26 and 38% respectively. In our study, the overall complication rate was 31.9%. The original CR-POSSUM was devised by identifying odds of risk factor causing mortality. However, it was a well-known fact that mortality was the end point of severe morbidity [18, 19]. Therefore, we used the same scoring system to analyse the outcome in terms of complications in our study. The equation, though, using the same odds as for mortality did not overpredict morbidity in our study. But in the physiological severity scoring, except for preoperative cardiac status and urea level, other variables have no significant correlation with outcome. Since wound infection and its sequelae occupy a considerable share (37%) of complications in our study, the role of physiological factors influencing the result may be less significant compared to operative severity score where later affects the outcome in terms of surgical site soft tissue infection [20]. Next common complications were respiratory (16.5%) and anastamotic leak (14.5%). Regarding mortality, CR-POSSUM observed and expected mortality ratio was 1 and area under ROC curve was 80% showing good model discrimination. But with low mortality rate [n = 10 (9.7%)] in our study, the validity of it may not be reliable.
Among the various risk factors, age and cancer staging are considered non-modifiable risk factors. The rest are modifiable risk factors and give the extent of scope to which the complications can be prevented by addressing such factors. But once patients present to tertiary centres in emergency or semi-emergency conditions, most of the risk factors will be present. Tackling such elements will be time-consuming and lead to a further chance of increasing complication [21]. Surgical site-related complications top in our study (37%) and elsewhere, as well [22]. They have an adverse impact in terms of long-term survival [23]. Since operative factors play a significant role in outcome in terms of wound infection as per our study, measures that reduce the chance of acquiring surgical site infections with high level of evidence are appropriate and timely administration of antibiotic, discontinuation of prophylactic antibiotic within 24 h of surgery, optimization of blood glucose levels and avoiding spillage of bowel contents [21]. Similar to SSIs, respiratory complication and anastomotic leak leading to deep-seated infection also affect the long-term survival [24]. PSS and OSS both play a significant role in predicting the latter two complications here. Hence tackling both physiological and operative variable assumes an important role prevention of these two problems.
CR-POSSUM, which was originally developed to predict mortality, can also be used to predict morbidity. But, there are some limitations to our study. Both CR-POSSUM and POSSUM models for mortality and POSSUM model for predicting morbidity left many variables like preoperative nutrition level, operative duration, BMI and length of preoperative stay, all of which influence the eventual outcome. These were not considered while developing the equation [21]. But these scoring systems were developed 10 and 25 years ago respectively, and many new influencing variables were found in subsequent research.
Our results may be biased since there is a high proportion of SSI-related complication. We, therefore, validated the equation after excluding this group of patients. We excluded surgical site infection (SSI) in further analysis, to check whether physiological factors had a role in predicting non-SSI-related complications. We found that there was, indeed, a significant association (P = 0.005) between PSS and other non-SSI complications. The results were similar with few minor variations in predictive values. So, if a new model is developed considering the various new variables, then the predictive accuracy of such an equation can be close to reality.
To conclude, these predictive models once validated, across various centres in India, can be used as a measure of quality control in different institutions. Secondly, they can also be used to allocate resources and adequately trained professionals to deal with those patients whose expected morbidity and mortality are high.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008. Int J Cancer 127:2893–2917
Comparison of cancer incidence and patterns of all population-based cancer registries. Available from: http://www.ncrpindia.org/all_ncrp_reports/pbcr_report_2012_2014/all_content/pdf_Printed_Version/Chapter7_Printed.pdf. Assessed 26th Jan 2018
Sudarshan V, Hussain N, Gahine R, Mourya J (2013) Colorectal cancer in young adults in a tertiary care hospital in Chhattisgarh, Raipur. Indian J Cancer 50:337–340
Patil PS, Saklani A, Gambhire P, Mehta S, Engineer R, De'Souza A et al (2017) Colorectal cancer in India: an audit from a tertiary center in a low prevalence area. Indian J SurgOncol 8:484
MohdSuan MA, Tan WL, Soelar SA, Ismail I, Abu Hassan MR (2015) Intestinal obstruction: predictor of poor prognosis in colorectal carcinoma? Epidemiol Health 37:e2015017
Itani KM, Hawn MT (2013) Prevention of surgical site infection in colorectal surgery. Colorectal Cancer 2:467–475
Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ (2005) Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 242:326–341
World Health Organisation global health expenditure database. Available from: https://data.worldbank.org/indicator/SH.XPD.TOTL.ZS. Accessed 7th Jan 2018
Longo WE, Virgo KS, Johnson FE, Oprian CA, Vernava AM, Wade TP, Phelan MA, Henderson WG, Daley J, Khuri SF (2000) Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum 43:83–91
Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ (1998) POSSUM and portsmouth POSSUM for predicting mortality. Physiological and operative severity score for the enumeration of mortality and morbidity. Br J Surg 85:1217–1220
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360
Teeuwen PHE, Bremers AJA, Groenewoud JMM (2011) Predictive value of POSSUM and ACPGBI scoring in mortality and morbidity of colorectal resection: a case-control study. J Gastrointest Surg 15:294–303
Cengiz F, Kamer E, Zengel B, Uyar B, Tavusbay C, Unalp HR (2014) Comparison of different scoring systems in patients undergoing colorectal cancer surgery for predicting mortality and morbidity. Indian J Cancer 51:543–548
Baré M, Alcantara M, Gil M, Collera P, Pont M, Escobar A et al (2018) Validity of the CR-POSSUM model in surgery for colorectal cancer in Spain (CCR-CARESS study) and comparison with other models to predict operative mortality. BMC Health Serv Res 18:49
Schilling PL, Dimick JB, Birkmeyer JD (2008) Prioritizing quality improvement in general surgery. J Am CollSurg 207:698–704
Tekkis PP, Prytherch DR, Kocher HM, Senapati A, Poloniecki JD, Stamatakis JD, Windsor ACJ (2004) Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg 91:1174–1182
Gallardo-Valverde JM, Calanas-Continente A, Baena-Delgado E, Zurera-Tendero L, Vazquez-Martinez C, Membrives-Obrero A, Muntane J, Arevalo-Jimenez E (2005) Obstruction in patients with colorectal cancer increases morbidity and mortality in association with altered nutritional status. Nutr Cancer 53:169–176
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Petros AJ, Marshall JC, van Saene HK (1995) Should morbidity replace mortality as an endpoint for clinical trials in intensive care. Lancet 345:369–371
Mahajna A, Krausz M, Rosin D, Shabtai M, Hershko D, Ayalon A, Zmora O (2005) Bowel preparation is associated with spillage of bowel contents in colorectal surgery. Dis Colon Rectum 48:1626–1631
Pedroso-Fernandez Y, Aguirre-Jaime A, Ramos MJ, Hernández M, Cuervo M, Bravo A, Carrillo A (2016) Prediction of surgical site infection after colorectal surgery. Am J Infect Control 44:450–454
Young PY, Khadaroo RG (2014) Surgical site infections. Surg Clin North Am 94:1245–1264
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH (2015) Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg 261:497–505
Tu R-H, Lin J-X, Li P, Xie J-W, Wang J-B, Lu J, Chen QY, Cao LL, Lin M, Zheng CH, Huang CM (2017) Prognostic significance of postoperative pneumonia after curative resection for patients with gastric cancer. Cancer Med 6:2757–2765
Acknowledgements
We thank our institute, its medical records and IT department for providing immense support in collecting data of the patients. We also offer special thanks to Prof. Dr. Karthikeyan of respiratory medicine department for his valuable input in design of the study. We thank Prof. Malmarugan Devanathan for his guidance in statistical analysis and make us to understand the statistical results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicting Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key message: CR-Possum can be used to predict morbidity in patient undergoing colorectal cancer surgery.
Rights and permissions
About this article
Cite this article
Prabakaran, V., Thangaraju, T., Mathew, A.C. et al. CR-Possum—Can It Be Used to Predict Morbidity? A Single-Centre Retrospective Study. Indian J Surg Oncol 10, 174–179 (2019). https://doi.org/10.1007/s13193-018-0841-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-018-0841-8