Abstract
Laparoscopic procedures to treat endometrial cancer are currently emerging. At present, we have evidence to do laparoscopic oncologic resections for endometrial cancer as proven by many prospective studies from abroad such as LAP2 by GOG. So, we have decided to assess the safety and feasibility of such a study in our population with the following as our primary objectives: (1) to study whether laparoscopy is better compared to open approach in terms of duration of hospital stay, perioperative morbidity and early recovery from surgical trauma and (2) to study whether the laparoscopic approach is noninferior to the open approach in terms of number of lymph nodes harvested in lymphadenectomy and rate of conversion to open surgery. We did a prospective nonrandomized comparative study of open versus laparoscopy approach for surgical staging of endometrial cancer from 16th May 2013 to 15th May 2015. To prove a significant difference in the hospital stay, we needed 29 patients in each arm. Thirty patients in each arm were enrolled for the study. The median duration of stay in the open arm was 7 days and in the laparoscopy arm it was 5 days. The advantage of 2 days in the laparoscopic arm was statistically significant (P value 0.006). Forty percent of patients in the open arm had to stay in the hospital for more than 7 days whereas only 3% of patients in the laparoscopy arm required to stay for more than 7 days (P value 0.001). This difference was statistically significant. There was no significant difference between the early complication rates between the two arms (20% in open vs. 13% in laparoscopy; P value 0.730). There was a conversion rate of 10% in laparoscopy. The median number of nodes harvested in open arm was 16.50 and in the laparoscopy arm, it was 13.50. The difference was not statistically significant (P value 0.086). Laparoscopy approach for endometrial cancer staging is feasible in Indian patients and the short-term advantages are replicable with same oncologic safety as proved by randomized controlled trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endometrial cancer is the second most common gynaecological malignancy around the world after carcinoma cervix and most common gynaecological malignancy in developed countries. In India, it is the third most common malignancy among females only after cervix and ovary [1]. The incidence of endometrial cancer cases is very low in India. Age standardized rates (ASR) of incidence in Bangalore, Delhi and Mumbai are 4.2, 4.3 and 2.8 per 100,000 populations [2]. In Chennai, the ASR is 4.23 per 100,000 populations and it is 3.25% of the total cancer burden [3].
Endometrial cancer is now a surgically staged malignancy. The pilot study by Creasman et al. [4] and subsequent reports of the GOG studies have been instrumental in this change. The surgical treatment for early stage endometrial cancer is highly variable and is currently under investigation; the classic standard treatment is total abdominal hysterectomy and bilateral salpingo-oophorectomy, with pelvic and para-aortic lymph node dissection if risk factors are present [5, 6]. Childers et al. [7] reported on a series of 59 patients considered candidates for laparoscopically assisted surgical staging (LASS) for management of their clinical stage I adeno-carcinoma of the endometrium. These authors successfully carried out pelvic and para-aortic lymphadenectomy on 23 patients. The first laparoscopic pelvic and aortic lymph node dissection for endometrial cancer was performed in 1992 by Childers and Surwit [7]. In LAP2 study [8] byWalker JL et al. conducted from 1996 to 2005 by GOG in which 1630 laparoscopy and 886 laparotomy patients were randomized, they inferred that comprehensive surgical staging of endometrial cancer can be performed using laparoscopy without increased intraoperative injuries, with fewer postoperative complications, and with shorter hospital stay. The median number of pelvic node harvested was 17 in the laparoscopy arm and 18 in the laparotomy arm. Median number of para-aortic nodes harvested was 7 in both the arms. There was no significant difference in the number of lymph nodes harvested.
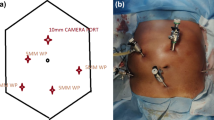
A prospective nonrandomized comparative study was conducted during the period from 16th May 2013 to 15th May 2015 to compare laparoscopy with laparotomy for complete comprehensive surgical staging of endometrial cancer. All the consecutive patients undergoing surgical staging for endometrial cancer during the study period who met the criteria and who were willing to participate in the study were enrolled after obtaining an informed written consent. The primary outcome of the study was number of days of hospital stay. Other end points included intraoperative complications, blood loss, and fall in haemoglobin level and duration of surgery. Postoperative analgesic usage, therapeutic antibiotic usage, number of days to return of normal bowel function and bladder function and number of days to resume normal routine activities, conversion to laparotomy, number of nodes harvested, and number of cases upstaged were studied. After getting the approval of the scientific and ethical committee, we prospectively collected and evaluated the data of all patients included in the study. Sample size calculation was done based on the LAP2 study [8] in which hospital stay of more than 2 days were observed in 94% of open cases and 52% of laparoscopy cases. With the level of significance at 5%, power of study at 95%, allocation ratio of 1 and with two-tailed distribution to detect a 42% difference (from reference) in proportion of patients requiring hospital stay of more than 2 days, a sample size of 29 was needed in both arms. Sample size calculation was done based on the software G*Power 3.1.9.2. A total of 77 patients were enrolled during the study period. Out of which, 45 underwent open surgical staging and 32 underwent laparoscopic staging. Out of the 45 who underwent open surgical staging, only 15 underwent para-aortic lymphadenectomy and the remaining, only pelvic lymphadenectomy alone was done. Only two patients in the laparoscopic group underwent para-aortic lymphadenectomy. So, in our study, a cohort of 30 patients in each arm underwent pelvic lymphadenectomy alone and we decided to compare this cohort.
In surgical staging, total abdominal hysterectomy (type 1) (TAH) and bilateral salpingo-oophorectomy (BSO) was done followed by pelvic lymphadenectomy. Para-aortic area was inspected in all cases. Para-aortic lymphadenectomy was done for those patients with preoperative diagnosis of nonendometrioid histology, high grade disease, fundal tumour with outer third myometrial invasion and intraoperative evidence of enlarged pelvic nodes or para-aortic nodes. Peritoneal washing was taken only when there was fluid in the cul-de sac. Demographic data including age, weight, height and BMI were recorded. The performance status was assessed by the ECOG score. Intraoperative blood loss was assessed by mop count and measuring the blood in the suction apparatus. Postoperative analgesic requirement was assessed by counting the number of doses and days of analgesic usage to have a zero pain score in a visual analogue scale. Postoperative use of therapeutic antibiotic was assessed by calculating the number of courses of antibiotic used other than the prophylactic antibiotics. Return of normal bowel function was assessed by return of normal bowel sounds and tolerance of oral diet. Return of normal voiding was assessed by the ability to void normally after removal of Foley’s catheter. Return of normal routine activity was assessed by the ability of the patient to be self-ambulant and go to the rest room without assistance. Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 published on May 28, 2009 (v4.02: Sept. 15, 2009) was used for grading complications. Febrile morbidity after surgery is defined as the documentation of body temperature >38 °C on two occasions at least 4 h apart during the postoperative period, excluding the first 24 h after surgery. Duration of surgery was from time of incision to the time of recovery. Duration of stay was calculated from the day of surgery to the day of discharge or from the day of surgery to the day of transfer to other departments for adjuvant therapy planning. Postoperative mortality was defined as death from any cause within 30 days after surgery. Pathological parameters such as FIGO grade and stage, histologic type, number of lymph nodes harvested and positivity rate, lymphovascular space invasion and outer third myometrial invasion were recorded and patients were categorized according to the risk category into low risk, low intermediate risk, high intermediate risk and high risk categories.
Data entry was done on MS Excel spread sheet. Data validation and analysis were carried out by SPSS version 11.0. Comparison of all nonnormally distributed continuous variables was done by Mann-Whitney U test. Comparisons of categorical variables were done by either chi-square test or Fisher’s exact test based on the number of observations. All P values <0.05 are considered as statistically significant.
There was no significant difference of distributions of age, height, weight, BMI, performance status, previous abdominal surgery and co-morbidities between the two arms. There was no significant difference in pathologic type, grade, FIGO stage, myometrial invasion, LVSI or risk category wise distributions between the open and laparoscopy arms. There was no significant difference in the number of lymph nodes harvested between the two arms. The median number of nodes harvested in open arm was 16.50 and in the laparoscopy arm, it was 13.50. The difference was not statistically significant (P value 0.086). There was a conversion rate of 10% in laparoscopy. Out of the three converted patients, one (33%) was due to bleeding and poor visibility. In the remaining two cases (66%), it was due to unusual adhesions in the ureterovesical junction involving the bladder, ureter and the parametrium. Two cases were converted to midline vertical incision and one to transverse muscle cutting incision. In 6 out of 27 patients (22%), specimen could not be delivered per vaginum and had to undergo a Pfannenstiel incision for the specimen delivery. Nulliparous women have a low probability of vaginal specimen delivery compared to parous women. The difference was statistically significant (P value 0.0432).
The duration of surgery was significantly more in the laparoscopic approach but the blood loss was significantly less. There was no significant difference in transfusion rate, fall in haemoglobin level or intraoperative complication rate. Number of days and doses of intravenous analgesic usage, number of days of return of bladder function, number of days of return of normal routine activities and duration of hospital stay were significantly less in the laparoscopic arm. There was a trend for early return of bowel sounds and less number of antibiotic usages in the laparoscopic arm but it was not statistically significant. The median duration of stay in the open arm was 7 days and in the laparoscopy arm, it was 5 days. The advantage of 2 days in the laparoscopic arm was statistically significant (P value 0.006). Comparison of pathologic characteristics (Table 1), patient characteristics ( Table 2), clinical characteristics (Table 3) between the study arms is given in table form.
Conversion to Open Surgery
There was a conversion rate of 10% in laparoscopy in our study. The conversion rate in the LAP2 study [8] was 25.8%. Poor exposure was the reason for conversion in 56.7% of the cases and cancer requiring laparotomy (15.9%) and excessive bleeding (11.3%) were the other main reasons reported for conversion. In the LACE trial [9], overall 29 conversions (3.8%) were recorded, five from TAH to TLH due to patient decision after randomisation and 24 from TLH to TAH. Fifteen for anatomical reasons of which six needed an abdominal incision to remove the uterus, two for technical reasons, and seven due to intraoperative complications. The conversion rate was directly related to BMI and higher conversion for each unit increase in BMI.
Intraoperative Parameters
Duration of Surgery
In the current study, the average duration of surgery in open arm was 127 min whereas in laparoscopy arm, it was 185 min. There was mean extra time of 57 min to complete the surgery by laparoscopy. This difference was statistically significant (P value 0.000). In the LAP2 study, the median operative time for the open laparotomy arm was 130 min, and for the laparoscopy arm, it was 204 min (P value 0.001). Similarly, the duration of surgery was 25 min longer in the TLH compared to the TAH arm (P < 0.001) in the LACE trial [9].
Blood Loss
The average blood loss in open arm was 328 ml whereas in laparoscopy arm, it was 124 ml. There was mean extra loss of 204 ml in the open arm which was statistically significant (P value 0.000). The average fall in haemoglobin in the open arm was 1.057 g/dl and in the laparoscopy arm, it was 0.813 g/dl. There was a difference of 0.243 g/dl between open and laparoscopic arm. The trend is towards less fall in haemoglobin in the laparoscopic arm but it was not statistically significant (P value 0.194). In the LACE trial [9], the drop in haemoglobin from baseline to day 1 postoperatively was 2.3 g/L lower in the TLH compared to the TAH arm (P value 0.006). Zullo F et al. [10] in a systematic review and meta-analysis noticed similar results but the benefits for these end points such as less blood loss and fall in haemoglobin are not known. In the present study, even though the blood transfusion rate was more in the open group, it was not statistically significant (16 vs. 6%; P value 0.423). In the LAP2 study, the blood transfusion requirement was more in laparoscopy compared to open (9 vs. 7%; P value 0.280) but it was not statistically significant.
Intraoperative Injuries
No intraoperative injuries were reported in the open arm. Three minor injuries were reported in the laparoscopic arm. A bladder injury, serosal burn of the caecum and right obturator artery injury were reported. None of those injuries had any consequences intraoperatively or postoperatively and were managed laparoscopically (P value 0.237). In the LAP2 study, intraoperative complications were not significantly different between the two treatment groups (8% for laparotomy vs. 10% for laparoscopy, P value 0.106). The incidence of intraoperative adverse events was similar between the treatment allocation arms (total abdominal hysterectomy 4.6%; total laparotomy hysterectomy 7.4%; P value 0.105) in the LACE trial.
Postoperative Parameters
Analgesic Requirement
The median number of days of IV analgesia usage was 3 days in the open arm and 2 days in the laparoscopy arm. Median extra 1 day of analgesic usage was observed in the open arm. This difference was statistically significant (P value 0.000). The median number of doses of IV analgesia usage was nine doses in the open arm and six doses in the laparoscopy arm. The difference was statistically significant (P value 0.0018). In the LACE trial [11], in the first 2 days after surgery, significantly more patients in the open arm required epidural analgesia (33% in TAH vs. 0.5% in TLH 푃 < 0.0001) and paracetamol (98% versus 95%, 푃 = 0.03) compared to the laparoscopy arm. At 3–5 days after surgery, significantly higher proportions of patients allocated to open surgery required more analgesia and this effect persisted at 6–14 days after surgery but not after that.
Antibiotic Requirement
In the current study, 8 out of 30 patients (26%) in the open arm received one or two therapeutic doses of antibiotic compared to 2 out of 30 (6%) in the laparoscopic arm, but the difference was not statistically significant (P value 0.080). But in the LAP2 study, the difference was statistically significant (23% in the open arm vs. 16% in the laparoscopy arm P value 0.001).
Bowel and Bladder Function
The median number of days to return the normal bowel function was 2 days in the open arm and 1 day in the laparoscopy arm. The trend was towards an advantage of 1 day in the laparoscopic arm but was not statistically significant (P value 0.360). The median number of days of return of normal bladder function in the open arm was 4 days and in the laparoscopy arm, it was 2 days. The advantage of 2 days in the laparoscopic arm was statistically significant (P value 0.000).
Normal Routine Activities
The median number of days to return of normal routine activities in the open arm was 2 days and in the laparoscopy arm, it was 1.5 days. The advantage of 0.50 days in the laparoscopic arm was statistically significant (P value 0.007).
Duration of Stay
The median duration of stay in the open arm was 7 days and in the laparoscopy arm, it was 5 days (Graph 1). The advantage of 2 days in the laparoscopic arm was statistically significant (P value 0.006). Forty percent of patients in the open arm had to stay in the hospital for more than 7 days whereas only 3% of patients in the laparoscopy arm required to stay for more than 7 days (P value 0.001). This difference was statistically significant in the present study. In LAP2 study, the proportion of patients requiring more than 2 days of hospitalization after surgery was significantly smaller in laparoscopy compared with laparotomy (52 vs. 94%, respectively; P value 0.0001), even after controlling for age, race/ethnicity, BMI and performance status. The median length of stay for laparotomy patients was 4 days, and the median length of stay for the intent-to-treat laparoscopy arm patients was 3 days. Similarly, in the LACE trial [9], the median length of hospital stay was 2 days in the TLH arm and 5 days in the TAH arm (p < 0.001) with a significant difference in favour of laparoscopy.
Even though there was a difference between the median numbers of days of hospital stay among three studies the advantage in the laparoscopy arm is significant. In our study the advantage was 2 days and in LAP2 study it was 1 day and in LACE trial it was 3 days.
Postoperative Complications
There was no significant difference between the early complication rates between the two arms (20% in open vs. 13% in laparoscopy; P value 0.730). In contrast to our study, in LAP2 study, eight complications ≥ grade 2 were more common in laparotomy patients than laparoscopy patients (21 vs. 14%, respectively; P value 0.001), even after controlling for patient age, race/ethnicity, BMI, and performance status. In our study, 3 (10%) patients in the open arm reported postoperative ileus but none in the laparoscopy arm had ileus. Similarly, in LAP2 study, ileus occurred significantly more often in laparotomy patients than laparoscopy patients (7 vs. 4%, respectively; P value 0.004). Other complications were not significantly different in LAP2 study at the adjusted significance level of P value of 0.005. In LACE trial [9], also, patients randomized to TAH had a 44% higher incidence of postoperative AE CTC grade ≥3 (18.6% in TAH, 12.9% in TLH; P value 0.03) when compared to those randomized to TLH. The incidence of serious AE was 74% higher in the TAH group compared with that in the TLH group (14.3% in TAH, 8.2% in TLH; P = 0.007). Wound infection or dehiscence contributed to the statistically significant differences between the treatment arms for postoperative AE and serious AE.
Body Mass Index
A BMI cut-off of 28 was considered for obesity and parameters were compared in the laparoscopy arm. Seventy percent (n = 21) patients were obese. On subset analysis, there observed a mean extra duration of surgery of 31.81 min in the high BMI arm (BMI >27.9). This difference was not statistically significant (P value 0.204). There was mean extra blood loss of 50.63 in the high BMI arm. This difference was not statistically significant (P value 0.209). There was no statistically significant difference in the complication rates between the low BMI (1 out of 10) and high BMI (4 out of 20) arms (P value 0.553).
Co-morbidities
Forty-eight patients out of 60 (80%) had some form of co-morbidities. Diabetes mellitus (n = 30, 50%), hypertension (n = 33, 55%), hypothyroidism (n = 13, 21%), bronchial asthma (n = 5, 8%) and ischaemic heart disease (n = 2, 3%) were the common co-morbidities observed in the order of frequency. There was no significant difference between the co-morbidity distributions between the groups (P value 0.203) except for diabetes mellitus which was significantly more in laparoscopic arm (70 vs. 30%; P value 0.004). There was no significant difference between the early complication rates between the two arms (20% in open vs. 13% in laparoscopy; P value 0.730). No patients with ischaemic heart disease underwent laparoscopic surgery.
Comparison to Meta-analysis
Meta-analysis by Juhasz-Böss I et al. [12] studied 1458 open and 1023 laparoscopic surgeries and they found no significant difference in the number of nodes removed and average hospital stay was significantly less in the laparoscopy arm. The data of our study has been compared with the meta-analysis in Table 4. In the De la Orden S G et al. [13] meta-analysis as illustrated in Table 5, there was no significant difference in the mean number of nodes harvested in different studies. Except in one study, all other studies recorded a significantly more operative time for the laparoscopic approach. Blood loss was significantly less in all the studies but fall in haemoglobin level varied in different studies. Intraoperative complication rates were similar in the study by Zullo et al. and our study. Postoperative complications were significantly less in the meta-analysis but in our study, there was only a trend towards fewer complications in the laparoscopy arm. All the studies consistently showed less number of days of hospital stay in the laparoscopy arm even though there observed a wide variation (2 to 8 days) in the number of days of hospital stay. Conversion rate varied from 6.9 to 12.5% in this meta-analysis.
Recommendations
-
1.
We recommend laparoscopic approach for staging all grades and histological types of endometrial cancer for FIGO stages IA, IB and II whenever the facility and expertise are available.
-
2.
Co-morbidities such as diabetes mellitus, hypertension, hypothyroidism and obesity are not contraindications for laparoscopic approach.
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2013) GLOBOCAN 2012 v1.0, Cancer incidence and mortality worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer. Available from: http://globocan.iarc.fr. Accessed 01 June 2015
Balasubramaniam G, Sushama S, Rasika B, Mahantshetty U (2013) Hospital-based study of endometrial cancer survival in Mumbai, India. Asian Pacific J Cancer Prev 14(2):977–980
National centre for disease informatics and research. National cancer registry programme ICMR: 3 year report of population based cancer registries 2009–2011. population based cancer registry chennai. [Internet] http://ncrpindia.org/ALL_NCRP_REPORTS/PBCR_REPORT_2009_2011/index.htm. Accessed 01 June 2015
Creasman WT, Morrow CP, Bundy BM, Homesley HD, Graham JE, Heller TB (1987) Surgical pathological study of endometrial cancer: a gynecology oncology group. Cancer 60:2035–2041
Creutzberg CL, Van Putten WLJ, Koper PC, Lybeert MLM, Jobsen JJ, Warlam-Rodenhuis CC, De Winter KAJ, Lutgens LCHW, Van den Bergh ACM, Van der Steen-Banasik E, Beerman H, Van Lent M (2003) Survival after relapse in patients with endometrial cancer: results from a randomized trial. Gynecol Oncol 89:201–209
Mariani A, Webb MJ, Keeney GL, Lesnick TG, Podratz KC (2002) Surgical stage I endometrial cancer: predictors of distant failure and death. Gynecol Oncol 87:274–280
Childers JM, Brzechffa P, Hatch KD, Surwit EA (1993) Laparoscopically assisted surgical staging (LASS) of endometrial cancer. Gynecol Oncol 47:669–685
Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, Spiegel G, Barakat R, Pearl ML, Sharma SK (2009) Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: gynecologic oncology group study LAP2. J Clin Oncol 27:5331–5336
Obermair A, Janda M, Baker J et al (2012) Improved surgical safety after laparoscopic compared to open surgery for apparent early stage endometrial cancer: results from a randomised-controlled clinical trial. Eur J Cancer 48(8):1147–1153
Zullo F, Falbo A, Palomba S (2012) Safety of laparoscopy vs laparotomy in the surgical staging of endometrial cancer: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol 207(2):94–100
Baker J, Janda M, Belavy D, Obermair A (2013) Differences in epidural and analgesic use in patients with apparent stage I endometrial cancer treated by open versus laparoscopic surgery: results from the randomised LACE trial. Minimally Invasive Surgery 2013:764329
Juhasz-Böss I, Haggag H, Baum S, Kerl S, Rody A, Solomayer E (2012) Laparoscopic and laparotomic approaches for endometrial cancer treatment: a comprehensive review. Arch Gynecol Obstet 286:167–172
De la Orden SG, Reza M, Blasco JA, Andradas E, Callejo D, Pérez T (2008) Laparoscopic hysterectomy in the treatment of endometrial cancer: a systematic review. J Minim Invasive Gynecol 15(4)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ansar P P, Ayyappan S & Mahajan, V. Prospective Nonrandomized Comparative Study of Laparoscopic Versus Open Surgical Staging for Endometrial Cancer in India. Indian J Surg Oncol 9, 133–140 (2018). https://doi.org/10.1007/s13193-017-0633-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-017-0633-6