Abstract
Mucocele of the appendix (AM) is a descriptive term for mucinous distension of the appendiceal lumen. It refers to the progressive retrograde dilatation of the vermiform appendix. Because of a lack of specific signs or due to its sometime quiet presentation, this condition is frequently diagnosed only at an advanced stage. We present three isolated cases of AM complicated by the development of acute inflammation of the appendix. Currently, the assessment of appendiceal lesions relies heavily on Ultra Sonography (US) as the primary diagnostic tool. This however may not always identify the origin of such a tumour. Therefore, additional investigative modalities are implemented. Despite recent research on the therapeutic strategies against appendiceal neoplastic disorders, surgical resection appears the only potentially curative approach. Accepted management includes appendectomy, right hemicolectomy, partial colectomy with debulking or palliative resection combined with additional chemotherapy. Even if laparoscopy has been successfully used to perform appendectomy, some concerns exist regarding its use in dealing with mucinous secreting lesions because of possible spillage of mucin intra-operatively. The aim of this investigation was to analyze all cases of AM complicated by the development of acute inflammation of the appendix presented in our institution. The relevant literature is briefly reviewed. Clinical features, diagnostic approach and management algorithm for appendiceal lesions are also discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucocele of the appendix (AM) is a descriptive term for mucinous distension of the appendiceal lumen regardless of the underlying pathology [1]. It refers to the progressive retrograde dilatation of the vermiform appendix with concomitant intraluminal accumulation of the mucoid substance. The incidence is estimated between 0.2 % and 0.4 % of the appendectomied specimens [2]. Recent investigations suggest four causal pathologic conditions with regard to retention cyst, mucosal hyperplasia, cystadenoma (or mucinous tumour of unknown malignant potential) and cystadenocarcinoma [3]. Because of a lack of specific signs or due to its sometime quiet presentation, this condition is frequently diagnosed only at an advanced stage. Alternatively the lesion represents an unexpected finding during surgical procedures performed for acute appendicitis or various not appendiceal pathologies [4]. Otherwise, AM comes to clinical attention because of symptoms such as right lower quadrant pain and palpable pelvic mass. Natural history is strongly influenced by anatomic peculiarities of the vermiform appendix that predispose to perforation and subsequent mucinous spillage into the peritoneal cavity leading to pseudomyxoma peritonei (PP) [5]. Histological subtype as well as the extent of dissemination consist significant prognostic factors.
Currently, the assessment of appendiceal lesions relies heavily on Ultra Sonography (US) as the primary diagnostic tool. This however may not always identify the origin of such a tumour [6]. In this case additional investigative modalities are implemented. Despite recent research on the therapeutic strategies against appendiceal neoplastic disorders, surgical resection appears the only potentially curative approach [7]. Accepted management includes appendectomy or right hemicolectomy either as a primary intervention or as secondary procedure in case of incidentally discovery of AM following the microscopic examination of the surgical specimen. Partial colectomy with debulking or palliative resection combined with additional chemotherapy has also been proposed. Additional intra-operative search for synchronous lesions and a life-long surveillance program for the detection of early stage metachronous carcinomas are recommended [8]. Even if laparoscopy has been successfully initiated to perform appendectomy, some concerns exist regarding its use in dealing with mucinous secreting lesions because of possible spillage of mucin intra-operatively [9]. The aim of this investigation was to analyze all cases of AM complicated by the development of acute inflammation of the appendix presented in our institution. The relevant literature is briefly reviewed. Clinical features, diagnostic approach and management algorithm for appendiceal lesions are also discussed.
Methods and Results
The records of the patients registered in the 4th Department of Surgery of Attikon University Hospital from 01/01/2013–31/12/2014 were subjected to meticulous examination. Into this retrospective survey were consecutively enrolled three cases of AM. The first patient was a 31-year old female admitted due to a 2-day history of intermittent pain in the right lower quadrant of the abdomen. Clinical examination revealed intense pain at palpation at the right iliac fossa. Pre-operative laboratory as well as imaging (US) investigation was within normal limits. The patient was operated with the presumed diagnosis of acute appendicitis. During surgical intervention, the appendix was found moderately dilated, without macroscopic findings indicating acute inflammation. Pathological examination revealed the diagnosis of AM. As the appendix was removed intact, without signs of perforation, further treatment was not provided to the patient. Post-operative course was uneventful and she remains without symptoms 21 months after surgery.
The second case referred to a 24-year old female patient admitted at the department of gynaecology, with the presumed diagnosis of a cyst of the right ovary. The patient described recurrent similar episodes of pain in the right iliac fossa. Subsequent US depicted a well demarcated cystic mass in the area of the right ovary. The patient underwent laparoscopy by the gynaecologists. Intra-operatively, the right ovary appeared normal, and the surgical team was called into the operating theatre for consultation. The mass was found to be originated from the appendix. Through a McBurney incision the caecum and the grossly dilated appendix were mobilized and a caecectomy with concomitant removal of the vermiform appendix was performed using a GIA stapler, which was placed just below the ileocaecal junction. Meticulous histological examination was indicative of AM. Evidence of malignancy was not documented. Because of the absence of perforation (spontaneous or intra-operatively) of the appendix additional treatment was not implemented. Post-operative recovery was unremarkable. The patient was discharged on the third post-operative day and she remains without signs of recurrence 9 months after surgery.
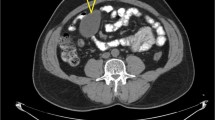
Finally, we describe a 23-year old woman presented with an intermittent right lower quadrant abdominal pain, persisting for the last two years. Vital signs as well as standard laboratory tests were within normal ranges. Bimanual palpation revealed a mildly mobile tender mass at the right iliac fossa. US demonstrated a hypoechoic cystic formation measuring 9 × 3 × 2 cm in contact with the caecum, anterior-exteriorly of the iliac vessels. Evidence of inflammation or other pathology on peri-appendiceal, abdominal or pelvic tissues was not apparent. Contrast enhanced Computed Tomography (CT) revealed a well encapsulated cystic structure (10 × 3 × 3 cm) with peripheral enhancement in the region of the caecum and curvilinear mural calcification (Fig. 1). Surgical exploration confirmed a distended appendix with intact wall, without inflammatory signs. In order to avoid a rupture and spillage of potentially malignant cystic contents a midline sub-umbilical incision was performed (Fig. 2). The histological diagnosis identified a mucinous cystadenoma of the appendix with focal low degree dysplasia of epithelium and profound production of mucous. Evidence of malignancy was not elucidated. The patient’s post-operative course was unremarkable, and she was discharged on the fourth post-operative day.
Discussion
AM was first described as a pathological entity by Rokitansky in 1842 and definitely named by Feren in 1876 [10]. It represents a gross descriptive term referring to the dilatation of the lumen of the vermiform appendix accompanied by an abnormal accumulation of mucous. Higa considered AM according to one of the four causative histopathological processes: a) simple or retention mucocele; b) mucinous cystadenoma defined as a dilated mucin-filled appendix containing adenomatous mucosa lined by atypical mucinous epithelium with minimal dysplastic features; c) mucinous cystadenocarcinoma characterized by the presence of high-grade cell dysplasia and usually stromal invasion beyond the muscularis mucosae; and d) myxoglobulosis defined as cystic dilatation of the appendix associated with mucinous globoid bodies. Given the poor histological criteria concerning invasiveness of mucinous tumours of the appendix some researchers proposed a third category of lesions (mucinous tumours of uncertain malignant potential), which reflects the occasional difficulty defining these lesions as either benign or malignant according to other variables apart from clinical behaviour [11]. The 5-year survival rate is 100 % in case of benign lesion and only 45 % in malignant tumours.
Historically, the majority of the patients are asymptomatic and AM appears as an incidental finding during surgical intervention, imaging study or endoscopic procedures. In a review of 135 patients with AM, 51 % were asymptomatic, while the most frequent clinical manifestations included abdominal pain (27 %), a palpable pelvic mass (16 %), weight loss (13 %), nausea or vomiting (9 %) or gastrointestinal (GI) bleeding (5 %) [12]. Urinary dysfunction has also been described. Among the three cases reported above, pain in the right lower quadrant of the abdomen was apparent, while one patient appeared with concomitant palpable lesion at the right iliac fossa. Therefore, pre-operative clinical diagnosis of AM is uncertain due to the absence of specific associated signs. The initial detection of the lesion may be facilitated by radiological, sonographic or endoscopic means.
In a plain abdominal radiography the most common finding is a mass in the lower right quadrant of the abdomen with a curvilinear parietal calcification. On barium enema the lesion may be depicted as a sharply outlined sub-mucosal or extrinsic mass indenting and laterally displacing the caecum [13]. US examination demonstrates a cystic mass with posterior enhancement, poorly defined wall and variable internal echogenicity depending on the composition of the mucous. Giant AM appears with the typical, pathognomonic “onion-skin sign”. Appendiceal diameter over 15 mm has been determined as the threshold for AM diagnosis with a sensitivity of 83 % and a specificity of 92 % [14]. Outer diameter limit for acute appendicitis detection has been established as 6 mm [15]. In our patients US examination was not indicative of an AM in the first case while in the second one depicted a well demarcated cystic mass in the area of the right ovary. In the third case a hypoechoic cystic formation in contact with the caecum, anterior-exteriorly of the iliac vessels was apparent. Therefore US findings are not specific for AM and differential diagnosis from other pathological entities including carcinoid, lymphoma, mesenteric cysts, ovarian neoplasms and GI carcinomas is implemented [16]. US-guided Fine needle aspiration (FNA) has not been proposed in order to avoid dissemination of the mucous leading to PP.
The CT appearance of AM has been adequately described. In general, a mucocele presents as a well circumscribed, low-attenuation, spheric or tubular mass contiguous with the base of the cecum. The finding of curvilinear mural calcification suggests the diagnosis although it is encountered in less than 50 % of affected cases. Intraluminal gas bubbles or an air-fluid level within a mucocele indicates the presence of infection, which can occur in either benign or malignant processes. Moreover, CT findings of acute appendicitis with associated mucocele can overlap those of the pathological condition without additional appendiceal lesion. The most discriminating CT features proved the maximal luminal diameter of the appendix and the identification of cystic dilatation along with mural calcification [17]. Recent survey reports that an overall appendiceal diameter of 15 mm or greater is suggestive of a neoplastic disorder. In addition mural enhancement was apparent in the majority of patients with acute appendicitis without mucocele, while in the presence of an appendicolith, a co-existing mucocele can be considered less likely. This observation may be related to the fact that mucoceles result from chronic appendiceal obstruction, whereas acute appendicitis without mucocele is associated with acute occlusion of the lumen of the vermiform appendix [18]. Finally, CT features including appendiceal wall thickening, focal appendiceal mass, intra-peritoneal fluid, peri-appendiceal fat stranding, lymphadenopathy, small-bowel mural thickening, extraluminal gas, the arrow-head sign, irregular contour and the presence of abscess proved insufficient in differential diagnosis of AM from other appendiceal lesions correlated with acute appendicitis.
Colonoscopic findings in patients with AM include the “volcano sign”, the appendiceal orifice observed in the centre of a firm mound covered by normal mucosa or a yellowish, lipoma-like submucosal mass. Colonoscopy in patients with abdominal pain is also useful for the detection of synchronous GI tumours [19]. In the above mentioned case reports endoscopic surveillance was avoided and the decision of excision of AM was made on the base of diagnostic uncertainty and the necessity to exclude malignancy. CT was performed pre-operatively in the last case and the suspicion of AM was significant.
Surgical approach of AM can be accomplished either by laparotomy or laparoscopy. Post-operative complications include intestinal obstruction, GI bleeding, fistula formation, volvulus and PP related to iatrogenic rupture of the mucocele [20]. Thus, the vast majority of investigators support conventional surgical intervention as the treatment of choice for AM, as the tissues should be handled carefully intra-operatively. Furthermore, a simple and thorough evaluation of these patients with a new algorithm has been suggested. Simple appendectomy is preferred in each case of benign AM with negative margins of resection without perforation. In patients with signs of perforation or positive margins of excision, cytology or appendiceal lymph nodes, right hemicolectomy and cytoreductive surgery (CRS) combined with heated intra-peritoneal chemotherapy (HIC) or early post-operative intra-peritoneal chemotherapy (EPIC) should be considered [21]. Long-term follow-up of these patients is also implemented. Perforated AM with positive margins of resection, positive cytology and negative lymph nodes necessitate caecectomy, CRS and HIC or EPIC. Finally, perforated AM with positive cytology and negative margins of excision and appendiceal lymph nodes should be treated with appendectomy, CRS and HIC or EPIC.
Laparoscopic surgery provides the advantage of adequate exposure and evaluation of the abdominal cavity as well as rapid recovery. Nevertheless, thorough handling of the specimen is recommended as spillage of the content can lead to PP. Atraumatic removal of the appendix and use of impermeable bag is also highly suggested. Conversion to laparotomy should be considered if the lesion is traumatically grasped, the tumour clearly extends beyond the appendix or signs of malignancy such as peritoneal deposits are present [22]. Involvement of the caecum or adjacent organs remains an indication for right hemicolectomy and meticulous exploration of GI tract and ovaries [23]. Nevertheless, few authors support a minimally invasive approach in selected patients for this rare entity. Recent publication elucidates a series of 8 patients with AM who successfully underwent laparoscopic resection indicating that whether the excision is accomplished by laparoscopy or the open approach long-term results are similar [24]. As the technique of laparoscopic appendectomy evolves, the feasibility of resecting appendiceal neoplasms should be further assessed, provided certain precautions are taken.
In conclusion AM is a descriptive term for mucinous distension of the appendiceal lumen. Currently, the assessment of appendiceal lesions relies heavily on US as the primary diagnostic tool. In case of diagnostic insufficiency additional investigative modalities are implemented. Accepted management includes appendectomy, right hemicolectomy, partial colectomy with debulking or palliative resection combined with additional chemotherapy. Even if laparoscopy has been successfully used to perform appendectomy, some concerns exist regarding its use in dealing with mucinous secreting lesions.
References
El Ajmi M, Rebai W, Ben SZ (2009) Mucocele of the appendiceal stump—an atypical presentation and a diagnostic dilemma. Acta Chir Belg 109:414–415
da Fonseca LM, Lacerda-Filho A, da Silva RG (2010) Pseudomyxoma peritonei syndrome 12 months after an intact resection of malignant mucocele of the appendix: A case report. Clinics 65:817–818
Malya FU, Hasbahceci M, Serter A, Cipe G, Karatepe O, Kocakoc E, Muslumanoglu M (2014) Appendiceal mucocele: clinical and imaging features of 14 Cases. Chirurgia (Bucur) 109:788–793
Spyropoulos C, Rentis A, Alexaki E, Triantafillidis JK, Vagianos C (2014) Appendiceal mucocele and pseudomyxoma peritonei; the clinical boundaries of a subtle disease. Am J Case Rep 15:355–360
Gillion JF, Franco D, Chapuis O, Serpeau D, Convard JP, Jullès MC, Balaton A, Karkouche B, Capelle P, Parmentier T, Chollet JM, Thillois JM, Berthelot G (2009) Appendiceal mucoceles, pseudomyxoma peritonei and appendiceal mucinous neoplasms: update on the contribution of imaging to choice of surgical approach. J Chir 146:150–166
García Lozano A, Vázquez Tarrago A, Castro García C, Richart Aznar J, Gómez Abril S, Martínez Abad M (2010) Mucocele of the appendix: Presentation of 31 cases. Cir Esp 87:108–112
Wei-Ming L, Chih-Hui L, Kuo LM, Yang BY (2010) Intussusception secondary to a giant appendiceal mucocele: preoperative diagnosis by multi-slice computed tomography. Abdom Imaging 35:428–430
Gonzalez-Moreno S, Sugarbaker PH (2004) Right colectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br J Surg 9:304–311
Gonzalez SM, Shmookler BM, Sugarbaker PH (1998) Appendiceal mucocele: contraindication to laparoscopic appendectomy. Surg Endosc 12:1177–1179
Ruiz-Tovar J, Teruel DG, Castiñeiras VM, Dehesa AS, Quindós PL, Molina EM (2007) Mucocele of the appendix. World J Surg 31:542–548
Misdraji J, Yantiss RK, Graeme-Cook FM, Balis UJ, Young RH (2003) Appendiceal mucinous neoplasm: a clinicopathological analysis of 107 cases. Am J Surg Pathol 27:1089–1103
Stocchi L, Wolff BG, Larson DR, Harrington JR (2003) Surgical treatment of appendiceal mucocele. Arch Surg 138:585–590
Dachman AH, Lichtenstein JE, Friedman AC (1985) Mucocele of the appendix and pseudomyxoma peritonei. AJR Am J Roentgenol 144:923–929
Lien WC, Huang SP, Chi CL, Liu KL, Lin MT, Lai TI, Liu YP, Wang HP (2006) Appendiceal outer diameter as an indicator differentiating appendiceal mucocele from appendicitis. Am J Emerg Med 24:801–805
Karakaya K, Barut F, Emre AU, Ucan HB, Cakmak GK, Irkorucu O, Tascilar O, Ustundag Y, Comert M (2008) Appendiceal mucocele: Case reports and review of current literature. World J Gastroenterol 14:2280–2283
Ruiz-Tovar J, Teruel DG, Castiñeiras VM, Dehesa AS, Quindós PL, Molina EM (2007) Mucocele of the appendix. World J Surg 31:542–548
Bennett GL, Tanpitukpongse TP, Macari M, Cho KC, Babb JS (2009) CT Diagnosis of mucocele of the appendix in patients with acute appendicitis. AJR Am J Roentgenol 192:103–110
Rabie ME, Al Shraim M, Al Skaini MS, Alqahtani S, El Hakeem I, Al Qahtani AS, Malatani T, Hummadi A (2015) mucus containing cystic lesions “mucocele” of the appendix: the unresolved issues. Int J Surg Oncol 2015:139461
Zanati SA, Martin JA, Baker JP, Streutker CJ, Marcon NE (2005) Colonoscopic diagnosis of mucocele of the appendix. Gastrointest Endosc 62:452–456
Faure M, Salgado R, Op de Beeck B, Bellinck P, Termote JL, Parizel PM (2014) mucocele of the appendix: case report and review of the literature. JBR-BTR 97:217–221
Palanivelu C, Rangarajan M, John SJ, Senthilkumar K, Annapoorni S (2008) Laparoscopic Right Hemicolectomy for Mucocele Due to a Low-Grade Appendiceal Mucinous Neoplasm. JSLS 12:194–197
Navarra G, Asopa V, Basaglia E, Jones M, Jiao LR, Habib NA (2003) Mucous cystadenoma of the appendix: is it safe to remove it by a laparoscopic approch? Surg Endosc 17:833–834
Bucher P, Mathe Z, Demirag A, Morel P (2004) Appendix tumors in the era of laparoscopic appendectomy. Surg Endosc 18:1063–1066
Rangarajan M, Palanivelu C, Kavalakat AJ, Parthasarathi R (2006) Laparoscopic appendectomy for mucocele of the appendix. Indian J Gastroenterol 25:256–257
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mastoraki, A., Sakorafas, G., Vassiliu, P. et al. Mucocele of the Appendix: Dilemmas in Differential Diagnosis and Therapeutic Management. Indian J Surg Oncol 7, 86–90 (2016). https://doi.org/10.1007/s13193-015-0463-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-015-0463-3