Abstract
Internal jugular vein duplication (IJVD) is a rare phenomenon. Twenty-one such instances in 18 individuals have been reported to date. We report an intra-operative case of unilateral IJVD in a 32-year-old male, who was operated for cancer of gingivobuccal sulcus. We have reviewed the published literature and have proposed a classification scheme in order to make future reporting systematic. The condition has been classified into type A, B and C based on their morphology. About 75 % of the reported cases are of Type A. Type C is the most complex of all the duplications. Though IJVD is physiologically inconsequential, it has clinical implications. Percutaneous catheterisation of the vein could be hazardous in all cases, but more so in type B and C duplications. As with any anomaly, the risk of accidental injury increases during surgical procedures. It is important to document findings of this anomaly in order to understand its anatomy and implications in a better way.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Internal jugular v. (IJV) is the principle deep vein of the neck that collects blood from the cranium, face and neck. The IJV is the primary route of drainage of deoxygenated intracranial blood. It starts from the jugular foramen in base of skull as a continuation of sigmoid sinus and joins the subclavian v. behind the clavicle. It has been demonstrated to have a predictable anatomical course, with only 5.5 % patients having variations [1]. Jugular foramen also transmits vagus n., accessory n., glossopharyngeal n. and posterior meningeal a. Normal IJV traverses the carotid sheath in antero-lateral position, accompanied by common carotid a. and vagus n., finally joining the subclavian v. to form brachiocephalic v.
IJV anomalies can create difficulties during surgical or other interventional procedures, and thus increase the rate of complications. In the literature, there are 21 reported internal jugular v. duplications (IJVD) in 18 individual cases. Out of these ten were identified operatively [2–9], four radiologically [10–12] and four by cadaveric dissections [13–16] (Table 1). The condition is unilateral in most of the cases, with only three of the 18 reported cases being bilateral [2, 10, 13]. The cases with angiographic studies have shown normal sigmoid sinus anatomy [5, 10, 12]. We report an operative case of unilateral IJVD in a patient who was operated for cancer of gingivo-buccal sulcus. .
Case Report
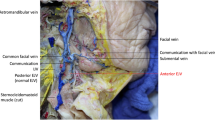
We report the case of a 32-year-old male with squamous cell carcinoma of left lower gingivo-buccal sulcus in T4 N2b M0 stage, who presented to our institute in January 2008. He was placed on the institutional tumour board and was advised radical surgery followed by chemo-radiation. He underwent wide excision of the lesion along with hemimandibulectomy and ipsilateral modified radical neck dissection (MRND) preserving IJV, accessory n. and sternocleidomastoid muscle. On splitting the carotid sheath during MRND, duplication of IJV into anterior and posterior components was noted (Fig. 1). Duplication started from 1 cm bellow the jugular foramen. The two components joined at the level of central tendon of omohyoid. The accessory n. traversed between the anterior and the posterior components of IJV. Vagus n. maintained its normal anatomical course, traversing posterior to IJV. Multiple external jugular vein phlebectasias were also noted. The anterior component of the IJV was sacrificed in order to achieve adequate lymph nodal clearance preserving accessory n. and vagus n. Postoperative recovery was uneventful. A review of the preoperative contrast enhanced computed tomography (CECT) showed high duplication of IJV on left side (Fig. 2). Right IJV showed normal anatomy on CECT.
Discussion
Duplication of IJV is a rare phenomenon. Due to the rarity of the condition, the exact prevalence of it is unknown. A case report by Prades JM, et al. has estimated the prevalence of IJVD to be 4 per 1000 unilateral neck dissections, based on 3 cases of duplication among 750 neck dissections over 5 years [5]. Our record for 2008 shows only one case of IJVD in 127 unilateral neck dissections. The morphology of IJVD varies significantly among cases and has not yet been fully classified. Downie et al. characterized two distinct morphologies of IJV variation, fenestrated and duplicated, both of which are referred to in the literature as duplicated. A complete classification is essential in order to report the cases in a scientific manner.
Classification of IJVD
Review of the published literature yielded 21 instances of IJVD; the present case makes 22. We found that IJVD conformed to three morphological patterns, each with different potential clinical implications (Fig. 3).
-
Type A: In this type of duplication the IJV starts from above the level of inferior border of posterior belly of digastric muscle [4–6, 10–12]. The duplicate veins join each other cranial to or at the level of the central tendon of omohyoid muscle [4–6, 10–12]. They are enclosed within the carotid sheath throughout their course. The accessory n. consistently traverses the gap between the two veins in all the described operative cases of type A IJVD [5, 6, 10–12]. There are 15 such instances reported to date, including our case. This accounts for nearly 75 % of the reported IJVDs. This type of IJVD has been previously described using various terminologies like fenestrated IJV [8, 12, 13], partial duplication [10, 16] and incomplete duplication [11]. This is the least complex of the three types of duplications.
-
Type B: This type differs from type A only in the caudal extent of the IJV duplication, which continues inferior to the omohyoid tendon [9, 10]. Previously these duplications have been describes as either complete [10] or total IJVDs [9]. These duplications have clinical significance because the segment of the IJV below the omohyoid tendon is often used for catheterization [17, 18]. The routine use of ultrasound guidance for catheterisation could prevent an injury to IJV in the presence of type B IJVD. Also during neck dissections, the presence of duplication in the distal IJV could pose difficulty both in preserving the vein as well as ligation. Two instances of type B IJVD have been reported in two individuals [9, 10]. One of these has been reported to have a bilateral anomaly with type B on one side and type A IJVD on the other [10]. It is interesting to note that both the reported cases had phlebectasia of the lower part of the vein.
-
Type C: There are five reported instances of type C IJVD [2, 4, 13], of which two are bilateral [2, 13]. These anomalies are more complex in nature. The duplication starts around the level of hyoid bone. The lateral component takes a course outside the carotid sheath and lateral to the omohyoid muscle, traversing the posterior triangle of neck, before curving and entering the carotid sheath at the root of the neck [2, 13]. Downie SA, et al. have described a bilateral Type C IJVD case with formation of a large bulbous jugulo-vertebro-subclavian venous sinus on one side [13]. This type anomaly would be difficult to handle surgically or for cauterization even under image guidance.
Embryology
Embryologically IJV develops from the ventral pharyngeal vein (VPV) in the region of mandibular and hyoid arch [19]. VPV drains into the precardinal v., which contributes to the formation of the lower part of the IJV, as the neck elongates [19]. Three hypotheses have been proposed to explain IJV duplication. They implicate the neuronal, skeletal and venous systems [5].
-
Venous Hypothesis: The development of neurocranium, cranial nerves and neck veins takes place during 3rd to 8th week of gestation [20]. The veins of neck are formed by the condensation of embryonic venous capillary plexuses [20]. Persistence of two venous channels during condensation could lead to the duplication of IJV [5]. This hypotheses could explain all three types of duplication.
-
Neuronal Hypothesis: This hypothesis states that the developing accessory n. may be trapped within the developing embryonic venous capillary plexuses [5]. Entrapment could lead to the formation of anterior and posterior VPV in relation to the nerve. As the embryonic neck elongates, the accessory n. migrates downwards along with its myotome [19] and the length of the duplication increases. This hypothesis may explain the development of type A and B IJVDs. However, it would not explain type C. It is known that accessory n. generally traverses the gap between the duplicate veins in type A IJVD.
-
Bony Hypothesis: Bony hypothesis states that the duplication of IJV is related to the duplication of jugular foramen during ossification [5]. The neurocranium starts developing in the 4th week of gestation and most of it is ossified by birth [20]. A study of foetal skulls looking at variations of jugular foramen, has described the presence of duplication as well as triplication of the foramen [21]. However, in all these variations of jugular foramen, the IJV exits through the posterior most foramen and is always single [21]. Thus, the bony hypotheses does not explain the development of IJVD.
Clinical Importance
The anomalies of major veins of the body are rare when compared to the variations of peripheral veins. Though IJVD is unlikely to have any physiological implications, it can lead to difficulties during clinical interventions. The understanding of this anomaly is important while performing procedures such as central venous catheterisation and neck dissections for cancers of head and neck region.
As IJV has a consistent anatomical course [1], it is an important reference point during surgical neck dissections. Depending on the type of dissection performed, the nodal tissue surrounding IJV is removed with or without the vein itself, accessory n. and/or sternocleidomastoid muscle. It is advisable to preserve IJV, accessory n. and sternocleidomastoid muscle in order to reduce the postoperative morbidity [22]. It is important to preserve the vagus n., which is in posteromedial relationship to IJV. Injury to vagus n. in the neck causes vocal cord palsy, loss of gag reflex and other autonomic dysfunctions. A CECT or magnetic resonance imaging of neck performed for pre-operative staging can diagnose the presence of IJVD. An angiogram would further be indicated to type the IJVD and plan an approach. In the presence of type A or B IJVD, the access to posteromedial structures in the upper neck is difficult without the ligation of the anterior component of the vein. Typically the anterior component of IJVD may be sacrificed with no added morbidity, as in our case. During those neck dissections where IJV ligation becomes essential due to advanced nature of the disease, it is important to identify and isolate both components of the duplicate IJV’s and ligate each separately in order to avoid haemorrhage. In case of type B and C IJVD, the drainage pattern of thoracic duct would be different from normal, posing a risk of injury during neck dissection.
Internal jugular v. is often used for percutaneous central venous catheterization. There are many techniques described for this procedure. Usually the vein is approached at the level of cricoid cartilage [23] or between the two heads of sternocleidomastoid [17, 18]. Though second approach could be safe in the presence of type A IJVD, an image guided procedure would be ideal in all patients needing IJV catheterisation.
Phlebectasia (a fusiform dilatation) of IJV or external jugular v. has been described in six of the reported cases of IJVD [4, 7, 9–11] and it is absent in 7 of them [2, 5, 12, 13]. Six of the cases have not mentioned either way [3, 6, 8, 14–16]. From the reported cases, 46 % of the IJVD cases have associated phlebectasias. The reason for the association is unclear. While no pathophysiological significance has been associated with phlebectasias, their presence could pose difficulty in choosing an appropriate recipient vein for anastomosis when performing a microvascular free-flap reconstruction. When a microvascular free flap has to be fashioned, presence of phlebectasias could pose difficulty in choosing appropriate recipient vein for anastomosis. It is unknown whether these veins heal normally following anastomosis.
Conclusion
Internal jugular vein duplication is a rare congenital anomaly, which is yet to be fully understood. We have proposed a classification scheme based on the morphology of IJV duplications reported to date. Each type, A, B and C, carries a unique potential for clinical problems during common procedures. Type A is the simplest and the most common form. Type B and C need to be handled with caution during interventional procedures.
References
Denys BG, Uretsky BF (1991) Anatomical variations of internal jugular vein location: impact on central venous access. Crit Care Med 19:1516–1519
Coca PA, Rodrigo Tapia JP (2008) Bilateral duplication of the internal jugular vein. Acta Otorrinolaringol Esp 59:314
Gardiner KJ, Irvine BW, Murray A (2002) Anomalous relationship of the spinal accessory nerve to the internal jugular vein. Clin Anat 15:62–63
Munoz Guerra MF, Campo FR, Gias LN et al (2000) Double internal jugular vein. Plast Reconstr Surg 106:1434–1435
Prades JM, Timoshenko A, Dumollard JM et al (2002) High duplication of the internal jugular vein: clinical incidence in the adult and surgical consequences, a report of three clinical cases. Surg Radiol Anat 24:129–132
Sylaidis P, Bardsley A, Montgomery P (1997) Duplication of internal jugular vein. Arch Otolaryngol Head Neck Surg 123:1358
Turan-Ozdemir S, Coskun H, Balban M (2004) Phlebectasia of the external jugular vein associated with duplication of the internal jugular vein. Clin Anat 17:522–525
Uecker FC, Wustenberg E, Zahnert T (2007) High duplication of an internal jugular vein. Laryngorhinootologie 86:592–594
Zukschwerdt L (1929) Seltene Lokalisation einer Venektasie. Dtsch Z Chir 216:283–285
Rossi A, Tortori-Donati P (2001) Internal jugular vein phlebectasia and duplication: case report with magnetic resonance angiography features. Pediatr Radiol 31:134
Som PM, Shugar JM, Sacher M et al (1985) Internal jugular vein phlebectasia and duplication: CT features. J Comput Assist Tomogr 9:390–392
Towbin AJ, Kanal E (2004) A review of two cases of fenestrated internal jugular veins as seen by CT angiography. AJNR Am J Neuroradiol 25:1433–1434
Downie SA, Schalop L, Mazurek JN et al (2007) Bilateral duplicated internal jugular veins: case study and literature review. Clin Anat 20:260–266
Kessel F (1928) Verlauf des Nervus accessorius durch eine Insel der Vena jugularis interna. Anat Anz 65:162–164
Nayak BS (2006) Surgically important variations of the jugular veins. Clin Anat 19:544–546
Setty LR (1960) A partially double internal jugular vein and its relation to the spinal accessory nerve. J Natl Med Assoc 52:174–175
Bannon MP, Heller SF, Rivera M (2011). Anatomic considerations for central venous cannulation. Risk Management and Healthcare Policy 4:27–39. doi:10.2147/RMHP.S10383
Sunavala JD (1999) Procedures in the intensive care unit. In: Udwadia FE (ed) Principles of critical care. Oxford University Press, New Delhi, pp 47–58
Standring S, Berkovitz B, Hackney C et al (2005) Neck and upper aerodigestive tract: development of the face and neck. In: Standring S (ed) Gray’s anatomy. Elsevier Churchill Lvingstone, London, pp 609–618
Sadler TW (2006) Langman’s medical embryology. Lippincott Williams & Wilkins, Philadelphia
Dodo Y (1986) Observations on the bony bridging of the jugular foramen in man. J Anat 144:153–165
Myers EN, Suen JY, Myers JN et al (2003) Cancer of the head and neck. Saunders, Philadelphia
Mark JB, Slaughter TF (2005) Cardiovascular monitoring. In: Miller RD (ed) Miller’s anesthesia. Elsevier Churchill Livingstone, California, pp 1265–1362
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nayak, S.P., Ashraf, M., Dam, A. et al. Internal Jugular Vein Duplication: Review and Classification. Indian J Surg Oncol 8, 222–226 (2017). https://doi.org/10.1007/s13193-015-0452-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-015-0452-6