Abstract
Human papillomavirus (HPV) vaccination can prevent numerous cancers, yet uptake remains low for adolescents. Given disproportionate burden of cancers among African Americans, it is important to identify factors that influence HPV vaccination decisions among African American parents, specifically the role and preferences of vaccine campaign messages. The objectives of this study were to (1) identify the predictors of parents’ decisions to get their children vaccinated against HPV, (2) assess parents’ evaluation of current HPV vaccination campaign messages, and (3) uncover message strategies or themes parents consider to be effective and motivating to vaccinate their children against HPV. Focus groups were conducted with African American mothers and fathers (n = 18) in person. Several themes emerged regarding HPV vaccine acceptability including the desire to be informed, the unfamiliarity of vaccination, and mistrust toward government, pharmaceutical companies, and healthcare providers. Parental review of existing campaign messages highlighted the importance of clarifying risks and benefits of vaccination, including cancer prevention, and the preference for straightforward language. When brainstorming strategies to craft effective messages, parents highlighted need for the inclusion of diverse groups across race, gender, and age. Additionally, parents recommended clear language on side effects, eligibility, and additional resources for further information. Our findings highlight concerns and potential strategies to promote HPV vaccination tailored to African American parents and their children. Targeted interventions to increase vaccination need to consider the importance of building trust and representation in health promotional materials. Considerations for how messages were shared were also discussed such as physical locations, word of mouth, and social media.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the Centers for Disease Control and Prevention (CDC), human papillomavirus (HPV) is the most common type of sexually transmitted infection (STI). HPV spreads through sexual contact and is linked with cervical, anal, vaginal, vulvar, penile, and oropharyngeal (head and neck) cancers, many of which can be prevented through vaccination [1]. The CDC has recommended HPV vaccination as a safe and effective method of preventing HPV infections for girls since June 2006 and for males since October 2011. Routine vaccination is recommended for preteen girls and boys starting at ages 11 and 12, as a preventive measure before sexual activity and potential HPV exposure [1]. National rates of HPV vaccination remain suboptimal, with only 56.8% for females and 51.8% for males aged 13–17 completing the recommended series [1]. HPV vaccination completion rates among African American adolescents (54.3%), are well below the Healthy People 2030 objective to increase HPV vaccination series completion for adolescents aged from 13 to 15 years to 80%. Suboptimal vaccination rates may perpetuate HPV-related cancer disparities, particularly for African American women, who are at greater risk for cervical cancer compared to non-Hispanic White women [2]. Compounding the issue, African American women are more likely to receive diagnoses at later stages, diminishing survival rates compared to diagnosis at earlier stages [2]. Given disproportionate burden of cancers among African Americans, it is important to identify and understand factors that influence HPV vaccination decisions.
As HPV vaccination is targeted toward young adolescents, it is important to consider parental attitudes that influence vaccine decision-making for their children. Vaccine decision-making is complex, with numerous factors that contribute to vaccine acceptance such as concerns of safety and side effects, linkage with sexual activity, and a general limited knowledge of HPV and HPV vaccines [3]. Prior literature has demonstrated that many parents do not believe their children to be vulnerable to HPV infection, citing that their children are too young/not sexually active and do not need vaccination [4]. Furthermore, HPV vaccination is often erroneously associated with cervical cancer exclusively. Thus, males are perceived to be less at risk [5], perpetuating misconceptions that HPV-related infection is not a serious concern resulting in suboptimal uptake. African American mothers expressed lack of information about the vaccine to make informed decisions and a mistrust of healthcare system [6]. Particularly for African Americans, mistrust of healthcare providers and pharmaceutical companies and a history of medical mistreatment of African Americans were also drivers of HPV vaccine uptake [7]. Additionally, literature suggests that provider communication is critical in HPV vaccine series uptake and completion, yet physicians are more likely to recommend other vaccines (e.g., tetanus and diphtheria) compared to HPV vaccine [8]. Less frequent and less emphasized recommendations may influence parents to perceive HPV vaccination as less important [8].
Health promotion materials such as educational brochures distributed by healthcare providers or national campaign messages broadcast across various mediums may be influential for parental HPV vaccine acceptability for their children. Kennedy et al. (2011) found that parents who received educational materials had improved attitudes toward and knowledge about the vaccine [9]. Formative findings from Shafer et al. (2011) found that mothers preferred visuals representing racially diverse groups on HPV vaccine campaign messages [10]. Similarly, in Dela Cruz et al.’s study (2017), parents reported that HPV vaccine educational brochures were more effective when culturally tailored to the Asian American and Pacific Islander population in Hawaii [11]. In particular, parents preferred promotional materials that included Hawai’ian faces and culture as well as testimonials from locals. In a qualitative study based on social marketing principles, Hull et al.’s (2014) showed that African American mothers and adolescents preferred campaign messages tailored toward younger adolescents and their parents [6]. Engaging community members to understand preferences on vaccine campaign materials is especially relevant during the coronavirus (COVID-19) pandemic. The pandemic has demonstrated the widening health disparities among African Americans and other people of color in addition to highlighting the public’s skepticism of the COVID-19 vaccine [12, 13]. Through a series of focus groups with African American custodial parents of children ages 9–17 years old, the current study aimed to identify the predictors of parents’ decisions to get their children vaccinated against HPV, assess parents’ evaluation of current HPV vaccination campaign messages, and uncover message strategies or themes parents consider to be effective and motivating. Findings can highlight opportunities to tailor educational materials to promote HPV vaccination among African American parents and their children.
Methods
Focus groups were conducted with parents or legal guardians of children ages 9–17 years old to expand current understanding of factors influencing HPV vaccine acceptability, the effectiveness of current mass media health campaigns, and the development of messages that would appeal to parents to increase HPV vaccine uptake. The focus group format allowed us to explore dynamic range of viewpoints among participants enriching the discussion, which may not have been adequately captured with individual interviews.
Settings and Participants
Parents or legal guardians were recruited via newspaper ads in the DC metropolitan area. Participants were screened by research assistants over the phone and were eligible if they were 21 years or older, in custody of a child (male or female) between the ages of 9 and 17, and self-identified as African American. We sought to represent both male and female parents and legal guardians to explore HPV vaccine decision-making in greater detail among caretakers. In-depth focus groups lasting 60 min were conducted at a university research center during fall 2018 with a total of 18 African American parents across four focus groups. Each session was attended by four or five participants on average. Each participant received a $50 gift card upon completion of the focus group.
Procedure
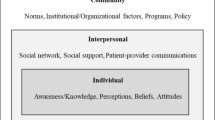
Prior to the focus group discussion, participants were asked to complete a consent form and a survey to collect demographic information and measure knowledge about and intentions to receive the HPV vaccine. Participants completed a baseline questionnaire and participated in one of four focus groups. At the beginning of the focus group, we surveyed participants about their HPV vaccine behavior and their knowledge related to HPV (n = 18). Each session was attended by four or five participants on average. Participants were read a short, educational explanation of HPV and the HPV vaccine at the start of the focus group to establish basic information to allow full participation. Participants were then asked about HPV vaccine acceptability and their decision-making-related process such as “In your own words, why did you decide to vaccinate or not vaccinate your child? Did you talk with anyone before deciding?” The focus group protocol development was guided by the health belief model and prospect theory to gauge how parents assess risk and benefits of deciding to vaccinate their children. Participants were subsequently provided with existing HPV campaign messages from the CDC and state public health departments for their feedback on the effectiveness of these materials. Finally, participants were prompted to develop message content and format that would appeal to parents. Groups were facilitated by trained research assistants. Interviews were audio-recorded and transcribed verbatim for analysis. This study was approved by the institutional review board at the University of Maryland.
Data Analysis
Following a qualitative content analysis approach, we analyzed transcripts to identify patterns and themes across the following domains: (1) HPV vaccine acceptability; (2) commentary on existing HPV vaccine campaign materials; and (3) commentary on developing effective HPV vaccine messages. Using an inductive content analysis approach, codes, categories, and themes were directly drawn from the data. Two independent reviewers read each focus group transcript for accuracy and flagged comments to be categorized into codes to be developed into broader themes. After the initial open coding, codes and themes were revised and compared for consistency and relevancy. Transcripts were analyzed in an iterative manner until no new themes emerged from the data and agreement was reached across codes and themes between reviewers [14]. To reach consensus, an additional review process was held which also consisted of the consolidation of similar themes. Data were coded and organized for thematic analysis using NVivo 12.
Results
Participants were predominantly female (66.7%). Age of participants ranged from 30 to 64 years old. A majority of participants had more than one child (66.7%) and were never married (61.1%). Among the parents, 16.7% had less than high school education, 22.2% were high school graduates, 33.4% had some college or an associate degree, and 27.8% had a bachelor’s degree or higher. Over 70% were on Medicaid and 22.2% were on private insurance. We first organized our results based on the three parts of the focus group protocol: (1) HPV vaccine acceptability and parents’ decision-making, (2) effective components of existing HPV vaccine campaign messages, and (3) strategies for effective HPV vaccine messages. Within each part, we categorized the results based on different themes that emerged from participants’ discussion. Most of the participants had not vaccinated their children (n = 12, 72.2%). Among the reasons for not vaccinating their children against HPV, “needing more information about the HPV vaccine” and “not receiving a healthcare professional’s recommendation” were most frequently cited (n = 5, 27.8%). “Healthcare provider discussions or recommendations” was the most salient reason for vaccinating children against HPV, together with “cervical cancer/disease prevention” (n = 5, 27.8%). Participants were mostly aware of HPV (n = 16, 88.9%) and that it is a sexually transmitted infection (n = 13, 72.2%) but were not aware of its link to a variety of cancers: 44.4% (n = 8) of the participants knew that HPV causes cervical cancer; 66.7% (n = 12) were aware of its link to anal/rectal cancer, whereas 33.3% (n = 6) were aware that it can cause cancer in the throat.
Themes
HPV Vaccine Acceptability and Parents’ Decision-making
Several themes emerged related to HPV vaccine acceptability and parental decision-making related to their children’s health (Table 1). First, parents felt that being informed was critical in deciding to vaccinate. This encompassed having specific information on HPV, HPV vaccination, and how it is spread. One parent commented that communication could be clearer in stating the risks and benefits of vaccination: The commercials were, to me, so vague, and I wasn’t really clear on understanding like, well what is HPV exactly? Why do we need to do it? Additionally, logistical concerns related to cost and insurance coverage were also discussed as a potential barrier to vaccination.
Given the unfamiliarity of HPV and the vaccine among participants, some parents expressed skepticism in vaccinating their children. Further deepening concerns, some participants felt they received conflicting information from credible sources. One participant mentioned that their physician cautioned against receiving the vaccine due to lack of trust, highlighting the underlying theme of mistrust among African American parents. Parents cited hesitancy to vaccinate, recalling past atrocities committed to African Americans medically: And then the Tuskegee experiments they had. All of those things make me more cautious. I want to be more informed. Lack of trust was emphasized at the government, pharmaceutical companies, and healthcare providers, citing questionable motives related to financial incentives in vaccination. Concerns of side effects, including the debunked potential link with autism, and the stigma of HPV being an STI further undermined parental vaccine acceptance.
Effective Components of Existing HPV Vaccine Campaign Messages
In this qualitative study, we focused heavily on parental perceptions of existing HPV campaign messages and potential future improvement to make messages more effective. During the focus groups, we distributed existing HPV vaccine campaign messages in the format of posters and asked participants to comment on these messages for both text and visual information (Table 2). Within the text of the existing HPV vaccine promotional material, parents stated it was necessary to include details on side effects, and emphasis on the vaccine as a cancer prevention measure, the efficacy of the vaccine, and who is eligible to receive vaccination: I didn’t understand it. Who is this for? Is this for me? Something like that. Even with the parents. Some of us may look at it and be like what is that? Parents felt that highlighting the risks and benefits of vaccination was key, while underscoring the benefit of cancer prevention which may prompt conversations with healthcare providers: It provokes a discussion, for one, with the provider, and then it specifically says it can reduce your son or daughter’s risk of certain HPV related cancers.
Regarding visual representation on existing promotional material, parents pointed to the inclusion of healthcare providers, which could help facilitate patient-provider dialogue. The conversations of who is represented on health communication materials were complex as related to race. A participant stated that they had not seen African Americans reflected in HPV commercials and had not heard of HPV affecting an African American child: Like the commercials and everything and stuff right. It’s more of Caucasians and I’m being honest. And so really honest I have not heard of a black child catching this okay? Another participant highlighted the complex power and race dynamics of including a healthcare provider on images: This one with the white doctor and the black patients, it says to me, come in and save us. I don’t know, maybe, and then … I guess my tainted thing just miss being tainted, because if it was a black doctor, and I’m saying, okay. We got to sell out. This you can’t win. With both textual and visual elements, participants preferred a material that used straightforward language for increased effectiveness of promotional communication. Inclusion of additional resources was also found to be beneficial, such as a website link or phone number, to receive further information.
Strategies to Develop Effective HPV Vaccine Messages
In addition to having participants comment on existing campaign messages about the HPV vaccine, we also arranged an activity in which participants brainstormed ideas about developing new campaign messages as if parents were charged with creating effective health campaigns (Table 3). Dovetailing their comments on existing campaign messages, participants emphasized the importance of including diverse audience members in the messages. Parents stated their preference for the inclusion of diverse groups across race, gender, and age: Put the boy and girl, because it’s for both, so they’ll know it’s for both. Doing so can showcase who is at risk of HPV infection and who can benefit from vaccination, without singling out a specific group: Have a diverse poster so nobody feels like they’re picked on or they’re being targeted. In addition to who is represented, participants had suggestions on the textual messages such as highlighting the benefits and risks of vaccination: HPV ads should have messages concerning the principal benefits of the vaccine and the person should be aware of the side effects, also. Specifically, parents found that focusing on cancer prevention was a compelling message to increase effectiveness of promotional material.
In a similar response to existing health promotional material, parents stated their preference for inclusion of links to other resources where they could get further information. The resources should include phone numbers in addition to links to the CDC website: I need something more than go online to CDC.gov. No, I need a 1–800 number or I need directions as to where to go. Regarding other elements, parents suggested featuring endorsements by celebrities or other public figures to garner attention for intended audiences. Doing so can raise awareness and potentially encourage parents and children to start a conversation about HPV vaccination. One parent recommended including a physician in the message to encourage patient-provider conversations: And a picture of the doctor. Because then it make the people say, oh I got to talk to the doctor about that. Because sometimes the doctor really don’t ask you that. In addition to the visual and textual features of an effective message, parents stressed the importance of how the message was shared. This included placement in physical locations such as public transportation hubs, buildings with foot traffic, and medical centers. Some ways to share messages included word of mouth, public service announcements on radio or television, and social media. One parent suggested using YouTube, leveraging its popularity and ability to generate user-created content: Everybody goes on YouTube, do a little skit.
Discussion
The purpose of this study was to investigate HPV vaccine acceptability, reactions to existing HPV vaccine campaigns, and considerations for developing effective HPV vaccine messages among a community sample of African American parents. Mothers and fathers who participated in focus groups indicated that parental vaccine acceptability is influenced by multiple factors such as the role of healthcare providers, vaccine safety, and mistrust, consistent with prior literature [3]. While we asked parents to assess elements of existing material that are effective, we also asked parents to suggest effective health campaign messages, a unique contribution to the literature. Our findings extend existing research on effective elements of existing campaign messages such as inclusion of specific HPV vaccine information (e.g., dosage, eligibility criteria) and the representation of intended audiences (e.g., boys and girls, parents, and African American families). Parents reported inclusion of these visual and narrative elements in the message content (e.g., representation of diverse families, transparent information on side effects) as well as message platform and delivery considerations when asked to develop their own messages promoting HPV vaccination. Our findings suggest potential messages strategies to promote HPV vaccination for African American parents and their children.
Vaccine Acceptability
While vaccination benefits, namely cancer prevention, resonated with parents, lack of information or recommendation about the vaccine led to feelings of hesitancy surrounding the vaccine. Specifically, parents felt that information on HPV (e.g., eligibility guidelines) vaccination was lacking or conflicting and impeded their ability to make informed decisions. Lack of information or awareness of HPV is also problematic as parents with lower knowledge are less likely to vaccinate [15]. Given the unfamiliarity of the vaccine and the lack of clarity on HPV vaccine guidelines, some parents preferred to delay vaccination until they received more information, which has implications for children’s health as vaccination is recommended at 11–12 years of age. HPV vaccination is more effective when administered to younger adolescents and may be especially beneficial for populations who experience a disproportionate disease burden. Delayed vaccination may also be due to parents associating HPV vaccination with adolescent sexual activity, even though they acknowledge the importance of protecting children from HPV-related infection [4]. Delayed vaccination may lead to missed opportunities for cancer prevention.
Compounding the issue of missed opportunities, some parents cited lack of healthcare provider (HCP) recommendation, which is disconcerting given that receipt of HCP recommendation is a strong predictor of HPV vaccination uptake. Provider communication is critical in HPV vaccine series uptake and completion: over 70% of adolescents who receive provider recommendation initiate HPV vaccination, highlighting opportunities for HCPs to increase vaccination [16]. African American adolescents and parents were less likely to receive a recommendation from a healthcare professional compared to white adolescents. These findings are troubling given that provider recommendations are influential among parents; 64% of African American parents reported they would have their child vaccinated if a doctor recommended it [17]. Given parental concerns, HCPs can engage with hesitant parents by addressing knowledge gaps of HPV vaccinations as well as benefits and risks which has shown to be associated with same-day vaccination [18].
Campaign Messages
We found that parents preferred health communication messages that conveyed pertinent details on HPV and HPV vaccination in a clear and straightforward manner. Moreover, parents preferred messages that reflect those who are susceptible to HPV-associated cancers. Parents overwhelmingly supported the inclusion of both girls and boys in campaign messages. Prior research suggests that parents who perceive the HPV vaccine to be associated with cervical cancer are less likely to consider males to be at risk, and thus, do not believe the vaccine is necessary [5]. Parents also called for the representation of African American families while including other diverse families to reflect susceptible communities. Therefore, messages need to be culturally sensitive to represent those at risk to increase effectiveness while avoiding stigma that may be associated with being specifically targeted.
In addition to the inclusion of those at risk, parents sought messages with specific details of vaccination such as the dosage and eligibility. Other important message elements highlighted the crucial role of healthcare providers, particularly as a cue to action to receive the vaccination. Parents expressed interest in including providers in visual messages promoting HPV vaccination, highlighting the importance of HCPs as a credible source of information for parents. Furthermore, parents reported the importance of racial diversity and representation with HCPs. Nazione, Perrault, and Keating (2019) found that Black adults paired with a Black physician had higher levels of similarity which may facilitate trust [20]. Similarly, displaying African American providers on communication materials intended for an African American audience may be beneficial to increase representation, credibility, and foster trust of vaccination.
Implications
We found that parents are strongly concerned with cancer prevention and vaccine safety. Research has shown that when framed as cancer prevention, HPV vaccination has been perceived as beneficial by parents, encouraging uptake [23]. Thus, disseminating accurate information highlighting benefits of vaccination from credible sources such as community organizations may mitigate mistrust. Given the importance of religion among African American persons, partnering with faith-based institutions may be effective in promoting vaccination [24]. While parents noted concerns of lack of information about vaccination, they also provided potential strategies for communication to reach other parents effectively. Given the importance of HCP recommendation for vaccine uptake, HCPs need to be encouraged to share information and provide the vaccination within the same visit. As HCPs are trusted sources of health information and decision-making, they are ideally positioned to assuage parental concerns of vaccine safety and address misconceptions such as the unsupported link between adolescent sexual behaviors due to vaccination. A framing approach to messaging may accentuate the perceived benefits of vaccination as cancer prevention and reduce the stigma associated with STIs, in line with the prospect theory [19]. Given the emphasis on cancer prevention desired by parents on health promotion messages, our findings suggest that gain-framed messaging accentuating the cancer prevention benefits of HPV vaccination may be useful in developing messages to encourage vaccine uptake. Additionally, the HPV vaccine can be bundled with other childhood vaccines or offered at school-based health centers to increase acceptance and convenience for families [25]. Doing so may reduce logistical barriers such as transportation that may discourage parents from vaccination.
Investigating factors related to HPV vaccine acceptability and message preferences is particularly relevant during the COVID-19 pandemic. Culturally competent health communication is especially central given the impact of COVID-19 on communities of color. Specifically, African Americans, who have higher rates on underlying chronic conditions, are more likely to be hospitalized and die from COVID-19 compared to non-Hispanic Whites [12, 21]. A consequence of structural racism and the burdens of social, economic, and environmental injustices have further contributed to widening disparities [4]. For example, African Americans represent a higher percentage of front-line workers that increase virus exposure risk while having lower access to quality healthcare [21]. Additionally, due to issues of trust and maltreatment, African Americans have lower rates of willingness to receive the COVID-19 vaccine (42% AA vs 61% Whites) [13]. This is consistent with findings from previous studies that found lower willingness among African Americans to receive vaccines in development [22].
To foster trust of COVID-19 and HPV vaccination among communities of color, the government, pharmaceutical organizations, public health institutions, and other related groups need to demonstrate being trustworthy by increasing transparency and community agency [21]. Consistent with our findings, communication needs to be clear with pertinent information such as vaccine effectiveness, side effects, dosage, and cost with consideration to literacy levels. Communication needs to be culturally and linguistically appropriate featuring members of the community (e.g., local leaders, clergy) and circulated where community members meet regularly (e.g., barbershops, places of worship). Existing communication networks can be leveraged to include trusted messengers to share promotional materials and increase credibility and trust of HPV and COVID-19 vaccination.
While our study provides novel formative findings, it is not without limitations. First, the study recruited a modest convenience sample of parents from the greater Washington DC area. Furthermore, participants were recruited from newspaper ads in the DC metropolitan area, which affects the generalizability of our findings to other populations. Over 70% of parents were of lower income, which also affects the external validity of findings. Finally, vaccination status was self-reported, and thus subject to recall bias. Nonetheless, we were able to cull rich formative findings regarding health promotion message considerations on HPV vaccination among African American male and female parents of both sons and daughters, whereas previous research has broadly focused on mothers and daughters. Future research can further examine differences in parental responses by gender. Furthermore, we are able to extend existing research on HPV vaccine acceptability by examining preferences of campaign messages in order to promote vaccination and with the goal of reducing cancer disparities. Findings demonstrate the importance of culturally tailored health campaign materials reflecting the faces and voices of the intended audience, the central role of trust within the African American community, and the importance of provider recommendation in facilitating HPV vaccine uptake. Integrating the sentiments of participants can contribute to the development of culturally relevant health promotion messages that align with beliefs and values of African American parents to achieve health equity.
Abbreviations
- CDC:
-
Centers for Disease Control and Prevention
- HCP:
-
Healthcare provider
- HPV:
-
Human papillomavirus
- STI:
-
Sexually transmitted infection
References
Elam-Evans LD, Yankey D, Singleton JA, Sterrett N, Markowitz LE, Williams CL, Fredua B, McNamara L, Stokley S (2020) National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years - United States, 2019. MMWR. Morbidity and mortality weekly report 69(33):1109–1116. https://doi.org/10.15585/mmwr.mm6933a1
American Cancer Society. (2019). Cancer facts and figures 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf. Accessed 11-5-2020
Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S (2014) Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 168(1):76–82. https://doi.org/10.1001/jamapediatrics.2013.2752
Bednarczyk, R. A. (2019). Addressing HPV vaccine myths: practical information for healthcare providers. Human Vaccines & Immunotherapeutics, 15(7–8), 1628–1638.
Lacombe-Duncan A, Newman PA, Baiden P (2018) Human papillomavirus vaccine acceptability and decision-making among adolescent boys and parents: a meta-ethnography of qualitative studies. Vaccine 36(19):2545–2558. https://doi.org/10.1016/j.vaccine.2018.02.079
Hull PC, Williams EA, Khabele D, Dean C, Bond B, Sanderson M (2014) HPV vaccine use among African American girls: qualitative formative research using a participatory social marketing approach. Gynecol Oncol 132:S13–S20. https://doi.org/10.1016/j.ygyno.2014.01.046
Fu LY, Zimet GD, Latkin CA, Joseph JG (2017) Associations of trust and healthcare provider advice with HPV vaccine acceptance among African American parents. Vaccine 35(5):802–807. https://doi.org/10.1016/j.vaccine.2016.12.045
Cooper DL, Hernandez ND, Rollins L, Akintobi TH, McAllister C (2017) HPV vaccine awareness and the association of trust in cancer information from physicians among males. Vaccine 35(20):2661–2667. https://doi.org/10.1016/j.vaccine.2017.03.083
Kennedy A, Sapsis KF, Stokley S, Curtis CR, Gust D (2011) Parental attitudes toward human papillomavirus vaccination: evaluation of an educational intervention, 2008. J Health Commun 16(3):300–313. https://doi.org/10.1080/10810730.2010.532296
Shafer A, Cates JR, Diehl SJ, Hartmann M (2011) Asking mom: formative research for an HPV vaccine campaign targeting mothers of adolescent girls. J Health Commun 16(9):988–1005. https://doi.org/10.1080/10810730.2011.571343
Dela Cruz MRI, Tsark JAU, Chen JJ, Albright CL, Braun KL (2017) Human papillomavirus (HPV) vaccination motivators, barriers, and brochure preferences among parents in multicultural Hawai’i: a qualitative study. J Cancer Educ 32(3):613–621. https://doi.org/10.1007/s13187-016-1009-2
Centers for Disease Control and Prevention (2020) COVID-19 hospitalization and death by race/ethnicity. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed 18 Jan 2021
Pew Research Center (2020) Intent to get a COVID-19 vaccine rises to 60% as confidence in research and development process increases. https://www.pewresearch.org/science/2020/12/03/intent-to-get-a-covid-19-vaccine-rises-to-60-as-confidence-in-research-and-development-process-increases. Accessed 15 Jan 2021
Strauss A, Corbin JM (1997) Grounded theory in practice. Sage
Dorell CG, Yankey D, Santibanez TA, Markowitz LE (2011) Human papillomavirus vaccination series initiation and completion, 2008–2009. Pediatrics 128(5):830–839. https://doi.org/10.1542/peds.2011-0950
Savas LS, Fernández ME, Jobe D, Carmack CC (2012) Human papillomavirus vaccine: 2–1–1 helplines and minority parent decision-making. Am J Prevent Med 43(6, Supplement 5), S490–S496. https://doi.org/10.1016/j.amepre.2012.09.003
Shay LA, Baldwin AS, Betts AC, Marks EG, Higashi RT, Street RL, Persaud D, Tiro JA (2018) Parent-provider communication of HPV vaccine hesitancy. Pediatrics e20172312. https://doi.org/10.1542/peds.2017-2312
Lindley MC, Jeyarajah J, Yankey D, Curtis CR, Markowitz LE, Stokley S (2016) Comparing human papillomavirus vaccine knowledge and intentions among parents of boys and girls. Hum Vaccin Immunother 12(6):1519–1527. https://doi.org/10.1080/21645515.2016.1157673
Tversky A, Kahneman D (1992) Advances in prospect theory: cumulative representation of uncertainty. J Risk Uncertain 5(4):297–323
Nazione S, Perrault EK, Keating DM (2019) Finding common ground: can provider-patient race concordance and self-disclosure bolster patient trust, perceptions, and intentions? J Racial Ethn Health Disparities 6(5):962–972. https://doi.org/10.1007/s40615-019-00597-6
Trust for America’s Health (2020) Building trust in and access to a covid-19 vaccine among people of color and tribal nations: a framework for action convening. https://www.tfah.org/article/vaccine-trust-witing-communities-of-color/. Accessed January 15, 2021.
Quinn SC, Lama Y, Jamison A, Freimuth V, Shah V (2020) Willingness of black and white adults to accept vaccines in development: an exploratory study using national survey data. Am J Health Prom, 0890117120979918. https://doi.org/10.1177/0890117120979918
Shah PD, Calo WA, Gilkey MB, Boynton MH, Dailey SA, Todd KG, ..., Brewer NT (2019) Questions and concerns about HPV vaccine: a communication experiment. Pediatrics 143(2) e20181872
Galbraith KV, Lechuga J, Jenerette CM, Moore LAD, Palmer MH, Hamilton JB (2016) Parental acceptance and uptake of the HPV vaccine among African-Americans and Latinos in the United States: a literature review. Soc Sci Med 159(Supplement C), 116–126. https://doi.org/10.1016/j.socscimed.2016.04.028
Kaul S, Do TQN, Hsu E, Schmeler KM, Montealegre JR, Rodriguez AM (2019) School-based human papillomavirus vaccination program for increasing vaccine uptake in an underserved area in Texas. Papillomavirus Research 8:100189. https://doi.org/10.1016/j.pvr.2019.100189
Funding
The research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number 1R01CA219060-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Other funding sources include the Maryland Department of Health's Cigarette Restitution Fund Program (Grant number: CH-649-CRF) and the National Cancer Institute - Cancer Center Support Grant (CCSG) - P30CA134274.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lama, Y., Qin, Y., Nan, X. et al. Human Papillomavirus Vaccine Acceptability and Campaign Message Preferences Among African American Parents: a Qualitative Study. J Canc Educ 37, 1691–1701 (2022). https://doi.org/10.1007/s13187-021-02014-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-021-02014-1