Abstract
Background
Definitive concurrent chemoradiation (cCRT) is offered to only 3% of Russian patients with stage III NSCLC. To determine the patterns of care and barriers to cCRT utilization in Russia, we conducted a survey of practicing radiation oncologists (ROs).
Methods
Electronic IRB-approved survey containing 15 questions was distributed to Russian ROs. Fisher’s exact test or Cochran-Armitage test of trend was used to assess the associations between clinical experience, practice type, and patterns of care.
Results
We analyzed 58 questionnaires completed by ROs—16 respondents from tertiary referral hospitals, and 42 from community or private centers. A total of 88% of respondents formulate treatment recommendations in multi-disciplinary tumor boards. For unresectable stage III NSCLC, the most common recommendation is sequential CRT (50%), followed by concurrent CRT (40%), with an observed higher utilization of cCRT in tertiary centers (9/16, 56% vs 14/42, 33%). Of the respondents, 31% do not offer cCRT to their pts. Among reasons for avoiding cCRT are (1) poor performance of pts (76%); (2) high toxicity of therapy (55%); (3) lack of consensus among tumor board members (33%); and (4) preference for sequential CRT (31%). Only 3% do not irradiate elective LNs. Eighty-six percent of respondents counsel their NSCLC pts regarding smoking cessation.
Conclusions
Despite level 1 evidence, cCRT is rarely used in Russia for pts with locally advanced NSCLC, and preference for sequential therapy and concerns over high toxicity are the most common barriers. Education of Russian ROs may increase cCRT utilization, leading to improved survival, notably in the era of maintenance immunotherapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lung cancer is a leading cause of cancer deaths in the world [1]. More than 60,000 new lung cancer cases are diagnosed annually in Russia, and over 50,000 of patients die every year, with half of these patients succumbing to their disease within 1 year of diagnosis, and less than one-fifth of lung cancer patients remaining alive past 5 years after initial diagnosis [2]. Non-small cell lung cancer makes up 85% of all lung cancer diagnoses and stage III is diagnosed in 40% of these patients—a clinical condition when a single treatment modality is simply not sufficient.
Patients with stage III NSCLC who are deemed non-resectable either because of extent of mediastinal adenopathy or due to comorbid medical conditions derive the best outcomes from concurrent chemoradiation therapy [3], especially when this definitive treatment is followed by maintenance immunotherapy [4]. Concurrent administration of both modalities—radiation therapy and chemotherapy—has been shown in randomized clinical trials and meta-analyses to offer a survival advantage over sequential administration, although at the cost of increased treatment-related toxicity [5,6,7,8,9,10].
Despite level 1 evidence, the utilization of concurrent chemoradiation therapy for management of stage III NSCLC is incredibly limited in Russia. In 2017, only one-third of lung cancer patients in Russia were diagnosed with early stage disease, yet among lung cancer patients who received radical therapy only 2.9% were treated with chemoradiation therapy [11]. This number decreased to 2.5% in 2018 [12]. For comparison, in the USA in 2016, over 35% of patients with locally advanced NSCLC were treated with cCRT [13].
One explanation for this dramatic difference is that thoracic surgery continues to play the dominant role in management of locally advanced NSCLC in Russia, either as a monotherapy or in combination with (neo)adjuvant therapies. In order to determine the barriers to CRT utilization in Russia, we have developed and conducted a survey of practicing radiation oncologists.
Material and Methods
An online survey was approved by the Oregon Health and Sciences University Institutional Review Board and distributed in February 2019 to 128 Russian oncologists, who registered to participate in the Russian Society of Clinical Oncology (RUSSCO) annual thoracic malignancy conferences in 2018 and 2019. All participants were contacted by email and invited to complete the survey, which was hosted by SurveyMonkey. The survey was closed on April 15, 2019; results were translated from Russian to English for descriptive analysis. Fisher’s exact test (categorical variables) or Cochran-Armitage test for trend (for ordinal variables) was used to evaluate association between respondents’ characteristics and their answers regarding preferred treatment approaches to patients with stage III NSCLC.
Results
Respondent Characteristics
Seventy-six respondents completed the survey, yielding a 59% response rate. We excluded from analysis 18 responses from non-radiation oncologists (10 medical oncologists, 3 surgeons, and 5 physicists), leaving 58 analyzable surveys. Among these respondents, 29% practiced independently less than 5 years, 29% between 5 and 10 years, and 41% over 10 years after completing their specialty training. Sixteen respondents (28%) identified a tertiary referral hospital whereas 42 (72%) identified a community-based secondary care center or a private clinic as the site of their clinical practice.
Stage III NSCLC Management Recommendations
Among 58 RO respondents, 88% acknowledged that treatment strategy for patients with newly diagnosed stage III NSCLC in their centers is formulated by a multi-disciplinary tumor board. Among the 42 RO respondents from regional or private clinics, 10% indicated that treatment decisions were formulated by thoracic surgeons in comparison to 0% of respondents from tertiary cancer centers. At the same time, for the 16 RO respondents from tertiary cancer centers, medical or radiation oncologists-driven treatment formulations were more common (19%) in comparison to regional/private clinics (0%) (Table 1).
Routine brain MRI in staging workup for a newly diagnosed stage III NSCLC was recommended by 24% of respondents, with 70% of respondents reserving brain MRI only for patients with neurological symptoms.
For patients with resectable stage IIIA NSCLC, 57% of RO respondents selected upfront surgery with adjuvant therapy as the preferred treatment strategy in their centers, whereas 29% of respondents selected neoadjuvant chemotherapy followed by surgery. Out of the 42 RO respondents from regional/private clinics, 17% selected trimodality therapy with neoadjuvant chemoradiation therapy followed by surgery as a preferred treatment strategy.
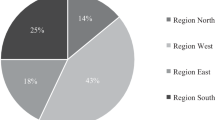
For patients with unresectable stage IIIB NSCLC, concurrent chemoRT was selected by 40% of respondents, whereas sequential chemotherapy followed by radiation therapy was selected by 50% of RO respondents as preferred treatment strategies at their centers. The remaining 10% selected surgery after completion of neoadjuvant therapy (Fig. 1).
Standard fractionation was preferred by 97% of RO respondents. For the purposes of simulation and treatment planning, computer tomography without intravenous contrast is chosen by 81%, PET/CT simulation by 24%, CT with IV contrast by 22%, 4-dimensional CT simulation by 7%, and 2-dimensional simulation by 7% of RO respondents (Table 2). Increased use of IV contrast with CT simulation was associated with more years of clinical practice (6% among RO respondents with less than 5 years of experience, 24% with 5–10 years of experience, and 33% with over 11 years of clinical experience, test of trend p value 0.04).
Among chemotherapy agents used with thoracic radiation therapy (concurrently or sequentially), the most commonly reported by RO respondents was cis-etoposide (76%) and carboplatin-paclitaxel (45%). Cis-etoposide was preferred by clinicians practicing in regional or private clinics vs tertiary referral hospitals (91% vs 38%, p< 0.001), whereas carboplatin-paclitaxel was preferred by respondents from tertiary hospitals (75% vs 33%, p=0.007) (Table 2).
Elective coverage of regional lymph nodes during radiation therapy planning was supported by 86% of respondents: 30 of these 50 respondents include ipsilateral hilar lymph nodes and the other 20 include all ipsilateral mediastinal lymph nodes. There was a greater tendency to treat thoracic lymph nodes electively among respondents from regional and private clinics in comparison to tertiary hospitals.
Eighty-six percent of RO respondents routinely counsel their lung cancer patients regarding smoking cessation.
Barriers to Utilization of Concurrent Chemoradiation Therapy in Unresectable Stage III NSCLC
Thirty-one percent of respondents do not administer thoracic radiation therapy with chemotherapy concurrently in their centers (Table 1). This rate was similar among respondents from tertiary hospitals and regional/private clinics. We observed a significant trend in concurrent chemoRT utilization and respondent’s clinical experience: 53%, 65%, and 83% with less than 5, between 5 and 10, and over 11 years of experience, respectively (test of trend, p =0.04). Fourteen percent of respondents stated that more than 50% of their patients with stage III NSCLC receive concurrent chemoradiation therapy (Table 1).
Among the most cited reasons for avoiding cCRT were (1) poor performance of patients (76%); (2) high toxicity of concurrent therapy (55%); (3) lack of consensus among tumor board members regarding cCRT (33%); and (4) preference for sequential CRT (31%) (Fig. 2).
Forty-seven percent of respondents from centers that rarely treat patients with concurrent chemoRT (less than 25%) sited “preference for sequential chemotherapy and radiation therapy” as a barrier for treatment, compared with no respondents from centers standardly treating such patients (more than 25%) (p value < 0.0001) (Table 3). Similarly, respondents who do not administer concurrent chemoRT were more likely to report “preference for sequential chemotherapy and radiation therapy” as a barrier for treatment (p value = 0.002).
Thirty-five percent of respondents from centers that treat more than 25% patients with concurrent chemoRT site “reimbursement of only one treatment modality” as a barrier to treatment, compared with 8% of respondents from centers that treat less than 25% of patients with concurrent chemoRT (p value = 0.023) (Table 3).
Discussion
Concurrent chemoradiation therapy remains the standard treatment modality for a vast majority of patients with stage III NSCLC. This level 1 evidence is supported by several prospective randomized clinical trials, as well as two large meta-analyses. The first meta-analysis of 2728 patients with NSCLC treated on 19 randomized clinical trials revealed a 14% reduction of cancer mortality with addition of chemotherapy to radiation therapy, and concurrent administration led to a 10% increase in 3-year overall survival in comparison to sequential administration [5]. This improvement in outcomes was accompanied by increased toxicity, especially esophagitis, anemia, and leukopenia. Grade 5 toxicity increased from 2% with sequential to 4% with concurrent chemoradiation therapy. A second meta-analysis was based on 1295 patients from 6 randomized clinical trials and demonstrated similar outcomes—a 5.7% improvement in 3-year overall survival at the price of increased acute grade 3–4 esophagitis [6]. Therefore, concurrent platinum-based chemoradiation therapy is a standard of care for patients with unresectable stage III NSCLC with adequate performance status who do not have a significant weight loss prior to treatment initiation. Neither neoadjuvant nor adjuvant chemotherapy confers additional benefit to patients who undergo concurrent CRT, while increasing treatment-related toxicity [7,8,9,10].
In Russia, surgery continues to be the leading modality, either as monotherapy or in combination with adjuvant or pre-operative therapies, for patients with stage III NSCLC. At the same time, the frequency of definitive chemoRT continues to decline in Russia—from 3.1% in 2016 down to 2.5% in 2018 [12]. These official numbers provided by the Russian Association of Oncologists are extremely inaccurate and cannot reliably portray the current patterns of care for several reasons. These numbers reflect management of all patients with lung cancer, both NSCLC and SCLC. In addition, only definitive therapies are reflected in these numbers—and since surgery is often assumed to be the only curative treatment modality in Russia for many non-hematologic malignancies, combination of chemotherapy and radiation therapy without surgery is often considered palliative and is excluded from statistical analysis. Finally, clinical data provided by Russian cancer centers is often inaccurate as data managers frequently lack training and are not able to distinguish between consecutive vs concurrent administration of chemotherapy and radiation therapy, and often assume that definition of combined therapy is only applicable to combination of surgery with another treatment modality. In the absence of centralized cancer registry with adequate data processing and analysis, epidemiological reports cannot be considered reliable.
This survey of practicing radiation oncologists is extremely relevant in this context. It reveals that concurrent CRT is still rarely used in Russia for patients with locally advanced NSCLC. More practicing ROs in Russia choose sequential rather than concurrent chemoradiation therapy for stage III NSCLC, despite clinical evidence from randomized trials showing superiority to a combination of two treatment modalities. It is apparent that this practice stems from concerns over increased toxicity from combination therapy. One strategy to minimize toxicity is to address current technical aspects of radiation therapy delivery in these patients. The vast majority of respondents (86%) practice elective lymph node coverage, which was previously shown to increase toxicity without improving tumor control or overall survival [14]. The use of non-contrast CT scan during simulation—a common practice reported by 81% of respondents—may also inadvertently lead to inclusion of normal structures, such as blood vessels, into treatment targets, leading to increased toxicity.
Our surveys reveal an enormous gap in physician education that must be met with additional contouring and planning workshops and lectures, similar to educational programs conducted under the auspices of the Russian Society of Clinical Oncology (RUSSCO) [15,16,17].
The dramatic difference between nationally reported low rate of definitive chemoRT utilization (approximately 3%) and the percentage of RO respondents willing to offer cCRT to their patients with stage III NSCLC (40%) also likely reflects the referral patterns, where many patients in Russia never undergo a multi-disciplinary evaluation and are operated first by thoracic surgeons before being referred for consideration of adjuvant therapies. It is critical to educate not only radiation oncologists but also thoracic surgeons, pulmonologists, and general practitioners in order to increase the awareness of importance of multi-disciplinary evaluation and management and ensure that patients with stage III NSCLC in Russia meet with medical and radiation oncologists prior to undergoing surgery.
A fundamental clinical education that in many countries is achieved through a dedicated residency training over several years does not exist in Russia, where physicians enter a 2-year oncology residency program, which covers all aspects of oncology care, but is most often a self-learning process with no didactic curriculum. After this, to receive a primary specialization in radiation oncology, a physician receives an additional training, which lasts from 2.5 to 4 months, with no practical training on treatment targets and normal structures contouring and treatment planning [18]. This likely explains why younger ROs in Russia have the lowest acceptance rates for utilization of cCRT, and this acceptance increases with years of independent clinical experience and life-long learning achieved, in part, by attendance of educational conferences and workshops.
The most impressive oncological outcomes in management of stage III NSCLC have been achieved in patients who received concurrent CRT with maintenance durvalumab on the PACIFIC trial [4]. Even the most favorable outcomes achieved in retrospective surgical series [19] that selected for surgical candidates have not shown numerically superior outcomes to the winning arm of the PACIFIC trial. Currently, maintenance durvalumab is allowed and practiced in Russia for patients with stage III NSCLC who complete sequential chemoradiation therapy; however, clinical evidence is lacking with this treatment strategy and for optimal outcomes patients should be offered concurrent therapy followed by maintenance IO. Analysis of oncological outcomes from Russian patients receiving sequential chemoRT with maintenance IO would be extremely enlightening and we encourage Russian cancer registries and individual cancer centers to collect and analyze this important clinical data.
We encourage further education of Russian clinicians, government officials, and patients through conferences and workshops of importance of multi-disciplinary evaluation of patients with stage III NSCLC and evidence-based treatment recommendations.
Availability of Data and Material
Fully available
Code Availability
n/a
References
Torre LA, Bray F, Siegel RL et al (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108
Kaprin AD, Starinsky VV, Petrova GV (eds) (2019) Malignant neoplasms in Russia in 2018 (morbidity and mortality). P.A. Gertzen Cancer Research Institute Moscow: Ministry of Health of Russian Federation, Moscow, Russia (book in Russian)
Chargari C, Soria JC, Deutsch E (2012) Controversies and challenges regarding the impact of radiation therapy on survival. Ann Oncol 00:1–9
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, Yokoi T, Chiappori A, Lee KH, de Wit M, Cho BC, Bourhaba M, Quantin X, Tokito T, Mekhail T, Planchard D, Kim YC, Karapetis CS, Hiret S, Ostoros G, Kubota K, Gray JE, Paz-Ares L, de Castro Carpeño J, Wadsworth C, Melillo G, Jiang H, Huang Y, Dennis PA, Özgüroğlu M (2017) Durvalumab after chemoradiotherapy in stage III non–small-cell lung cancer. N Engl J Med 377:1919–1929
O’Rourke N, Roqué I Figuls M, Farré Bernadó N, Macbeth F (2010) Concurrent chemoradiotherapy in non-small cell lung cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD002140.pub3
Auperin A, Le Pechoux С, Rolland E et al (2010) Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non–small-cell lung cancer. J Clin Oncol 28(13):2181–2190
Vokes EE, Herndon JE II, Kelley MJ et al (2007) Induction chemotherapy followed by chemoradiotherapy compared with chemoradiotherapy alone for regionally advanced unresectable stage III non–small-cell lung cancer: Cancer and Leukemia Group B. J Clin Oncol 25(13):1698–1704
Belani CP, Choy H, Bonomi P, Scott C, Travis P, Haluschak J, Curran WJ Jr (2005) Combined chemoradiotherapy regimens of paclitaxel and carboplatin for locally advanced non-small-cell lung cancer: a randomized phase II locally advanced multi-modality protocol. J Clin Oncol 23:5883–5891
Hanna N, Neubauer M, Yiannoutsos C, McGarry R, Arseneau J, Ansari R, Reynolds C, Govindan R, Melnyk A, Fisher W, Richards D, Bruetman D, Anderson T, Chowhan N, Nattam S, Mantravadi P, Johnson C, Breen T, White A, Einhorn L, Hoosier Oncology Group, US Oncology (2008) Phase III study of cisplatin, etoposide, and concurrent chest radiation with or without consolidation docetaxel in patients with inoperable stage III non-small-cell lung cancer: the Hoosier Oncology Group and U.S.Oncology. J Clin Oncol 26:5755–5760
Jalal SI, Riggs HD, Melnyk A, Richards D, Agarwala A, Neubauer M, Ansari R, Govindan R, Bruetman D, Fisher W, Breen T, Johnson CS, Yu M, Einhorn L, Hanna N (2012) Updated survival and outcomes for older adults with inoperable stage III non-small-cell lung cancer treated with cisplatin, etoposide, and concurrent chest radiation with or without consolidation docetaxel: analysis of a phase III trial from the Hoosier Oncology Group (HOG) and US Oncology. Ann Oncol 23:1730–1738
Kaprin AD, Starinsky VV, Petrova GV (eds) (2018) The state of oncological care for the population of Russia in 2017. P.A. Gertzen Cancer Research Institute Moscow: Ministry of Health of Russian Federation, Moscow, Russia (book in Russian)
Kaprin AD, Starinsky VV, Petrova GV (eds) (2019) The state of oncological care for the population of Russia in 2018. P.A. Gertzen Cancer Research Institute Moscow: Ministry of Health of Russian Federation, Moscow, Russia (book in Russian)
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66(4):271–289
Fernandes AT, Shen J, Finlay J, Mitra N, Evans T, Stevenson J, Langer C, Lin L, Hahn S, Glatstein E, Rengan R (2010) Elective nodal irradiation (ENI) vs. involved field radiotherapy (IFRT) for locally advanced non-small cell lung cancer (NSCLC): a comparative analysis of toxicities and clinical outcomes. Radiother Oncol 95(2):178–184
Mitin T, Dengina N, Chernykh M, Usychkin S, Gladkov O, Degnin C, Chen Y, Nosov D, Tsimafeyeu I, Thomas CR Jr, Tjulandin S (2020) Management of muscle invasive bladder cancer with bladder preservation in Russia: a survey-based analysis of current practice and the impact of an educational workshop on clinical expertise. J Cancer Educ. https://doi.org/10.1007/s13187-020-01728-y
Mitin T, Degnin C, Chen Y, Shirvani S, Gillespie E, Hoffe S, Latifi K, Nabavizadeh N, Dengina N, Chernich M, Usychkin S, Kharitonova E, Egorova Y, Pankratov A, Tsimafeyeu I, Thomas CR Jr, Tjulandin S, Likhacheva A (2020) Radiotherapy for hepatocellular carcinoma in Russia: a survey-based analysis of current practice and the impact of an educational workshop on clinical expertise. J Cancer Educ 35(1):105–111
McClelland S 3rd, Chernykh M, Dengina N et al (2019) Bridging the gap in global advanced radiation oncology training: impact of a web-based open-access interactive three-dimensional contouring atlas on radiation oncologist practice in Russia. J Cancer Educ 34(5):871–873
Likhacheva A et al (2017) The red beam: past, present, and future of radiation oncology in Russia. IJROBP 97(2):220–224
Aggarwal C, Li L, Borghaei H et al (2014) Multidisciplinary therapy of stage IIIA non-small-cell lung cancer: long-term outcome of chemoradiation with or without surgery. Cancer Control 21(1):57–62
Author information
Authors and Affiliations
Contributions
ND, MC, and TM designed the study; CD and YC performed data analysis; ND, MC, IT, VK, ST, KL, CRT, and TM carried out the study and reviewed the drafted manuscript, and participated in finalizing the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Oregon Health and Sciences University, IRB protocol 11149
Consent to Participate
n/a
Consent for Publication
n/a
Conflict of Interest
The authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dengina, N., Chernykh, M., Degnin, C. et al. Patterns of Care and Barriers to Utilization of Definitive Concurrent Chemoradiation Therapy for Stage III Non-Small Cell Lung Cancer in Russia. J Canc Educ 37, 1378–1384 (2022). https://doi.org/10.1007/s13187-021-01966-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-021-01966-8