Abstract
Culturally relevant health promotion is an opportunity to reduce health inequities in the cancer burden, and online learning is an emerging avenue for health promotion. To address a desire for synchronous online cancer education, a project team offered ten 1-hr cancer education webinars for Alaska’s rural tribal health workers. The project was guided by the framework of Community-Based Participatory Action Research, honored Indigenous Ways of Knowing, and was informed by Empowerment Theory. The evaluation of this community-based intervention included end-of-webinar surveys. Between February and April 2018, 41 surveys were completed by 11 unique participants. All participants reported that, as a result of the webinars, they planned both to change their own behavior to reduce cancer risk, and to talk with their patients more often about cancer prevention strategies such as screenings, physical activity, tobacco cessation, and eating healthy. While the webinars addressed desires for synchronous actions to support cancer learning, and led to intentions to positive change behaviors, the ten webinars engaged far fewer unique learners than the team’s asynchronous cancer education modules. This experience may inform other cancer educators’ efforts to develop, implement, and evaluate online learning opportunities. Despite the small numbers, these webinars resulted in increased learners’ intent to reduce cancer risk behaviors, share cancer information, and improved learners’ capacity to talk about cancer in their communities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
“I am enjoying these classes very much, and they have such great information and it’s so good just to refresh our minds.”
Background
In the USA, cancer is the second leading cause of death [1]. Cancer caused almost 600,000 deaths in 2016 alone [2]. Cancer is the leading cause of death for Alaska Native people, who are disproportionately burdened, both by cancer mortality and incidence, as well as associated risk factors [3]. Between 2009 and 2013, the cancer mortality rate for Alaska Native people was 40% higher than for US Whites [3]. The most commonly diagnosed cancers among Alaska Native people are lung, colorectal, and breast cancer, which all have modifiable behavioral risk factors [4, 5]. This presents an opportunity to reduce cancer risk through health behavior change.
Most Americans are not aware that health behaviors like physical inactivity and obesity can increase cancer risk [6]. However, these risk factors disproportionately impact Alaska Native people: in 2015–2017, 36.5% of Alaska Native adults reported currently smoking (compared with 16.1% of Alaska White adults) [7], and 36.8% reported BMI of 30 or greater (compared with 29.5% of Alaska White adults) [8]. In 2015–2017, only 14.4% of Alaska Native adults reported eating at least 5 fruits or vegetables a day (compared with 19.4% of White Alaska adults) [9].
Consequently, health promotion efforts have the potential to alleviate disparities and reduce cancer risk factors among Alaska Native people. For example, the percentage of Alaska Native adults who reported receiving a breast or colorectal cancer screening has recently attained parity with rates for both Alaska White adults and US White adults [10, 11]. Additionally, cervical cancer screening rates for Alaska Native people are now only slightly lower than Alaska White women [12].
To promote wellness in rural Alaska and reduce cancer risk factors, Alaska’s Community Health Aides/Practitioners (CHA/Ps) are vital. Alaska’s CHA/Ps are tribal primary care providers who live and work in rural Alaska. CHA/Ps are often recruited from the communities they serve, and work under the supervision and standing orders of senior medical providers. CHA/Ps are often the only health care providers in their communities, and can have an impact on the information their families and patients hear about tobacco, weight management, physical activity, cancer screenings, and nutrition.
CHA/Ps are uniquely situated to support positive behavior change in their communities. As the health care providers, they are central to each village’s health and wellness networks. This work partners with CHA/Ps to support them to share information and positive behavior change within their communities and patient networks. Patients receiving information from healthcare professionals, such as Alaska’s CHA/Ps, is a significant determinant of patient behavior. This information sharing has also been found to effectively reduce patients’ cancer risk factors. In a study of over 8000 patients, talking with a healthcare professional and hearing an adequate explanation about the need for colorectal cancer screening was significantly correlated with patients receiving that screening [13]. A meta-analysis also found that a healthcare professional sharing advice about tobacco cessation increased the rate of patients who quit tobacco [14]. Further, a systematic review found a positive correlation between patients’ physical activity and healthcare providers’ counseling about exercise [15]. The aim of shifting patient behaviors by improving CHA/P-patient education is consistent with the literature, which has documented that counseling by healthcare professionals is a significant determinant of patient behavior.
The Alaska Community Health Aide Program (CHAP) was developed in the 1960s, and remains a core component of Alaska’s healthcare delivery system [16]. Alaska’s CHA/Ps are trained to practice according to the guidelines of the Alaska Community Health Aide Manual, which details protocols to evaluate patients and provide basic and emergency medical care. To become a Community Health Practitioner, individuals engage in four 3–4-week basic training sessions, then complete a clinical skills preceptorship and examination [16]. Out of the 588.5 h of basic training, only 2 h (.3% of the total training) is dedicated to information about cancer [16].
Due to this lack of information, and the large burden of cancer in their communities, Alaska’s CHA/Ps have requested additional cancer education [17], resulting in the CHAP cancer education project team developing and instructing in-person cancer and wellness courses starting in 2001 [18]. However, the recent statewide financial crises, coupled with Alaska’s large distances, expensive airfare, remote communities, and transportation challenges, restrict CHA/Ps’ ability to receive in-person education. Fortunately, increased access to high-speed Internet in rural Alaska has provided an opportunity for CHA/Ps to learn about cancer without the cost or burden of leaving their communities [19, 20].
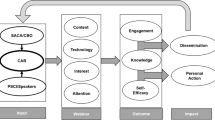
In response to CHA/Ps desires to have access to information about cancer while remaining in their own communities, the CHAP cancer education team developed a framework for culturally relevant cancer education that guided the creation of online learning modules for Alaska’s tribal rural primary care providers [21]. The team developed twelve stand-alone culturally relevant online cancer education modules: cancer basics, cancer and our genes, nutrition and physical activity, tobacco, colorectal cancer, men’s health, women and cancer, cancer treatments, cancer survivorship, cancer pain, grief and loss, and children and grief. Modules were published online as they were developed between March 2015 and June 2018. The modules were designed to inform CHA/Ps about specific cancer information, to support learners to reduce their cancer risk, and to improve learners’ capacity and intent to share cancer information with their patients, families, friends, and communities. End-of-module evaluation surveys documented that learners reported an intent to reduce their own cancer risk and share cancer information as a result of the learning [22], and changed their perceptions of comfort and capacity to engage with patients about cancer and their intent to talk with patients about cancer [23].
Additionally, the stand-alone cancer education modules were included as part of a semester-long, for-credit university course that also included synchronous sessions to connect learners via video conference. However, when the course was offered in spring 2018, no learners were able to commit to a full semester course, but several expressed a desire to participate in the course’s synchronous sessions on cancer topics. In response, the project team developed, advertised, offered, and evaluated ten 1-hr webinars for Alaska’s CHA/Ps. This manuscript describes the implementation of those webinars, and evaluation findings.
Theoretical Framework
The principles of Community-Based Participatory Action Research (CBPAR) and Empowerment Theory informed the design, delivery, and evaluation of the webinar series. CBPAR emphasizes equitable partnerships between academics/researchers and community members, with a focus on topics important to community members, aiming to result in a reduction in inequity and lasting social change [24]. The CBPAR framework informed the partnership between the project team, CHA/P supervisors and instructors, and CHA/Ps. In addition, ways of knowing that CHA/Ps have identified as resonant have been a part of CHA/P cancer education since it began [25, 26], with instructional strategies tailored to CHA/Ps, many of which are similar to the literature on Indigenous Ways of Knowing, which describes a focus on learning connected to affective domains and relationships [27, 28].
As part of this project, the CHAP cancer education team worked with CHA/Ps and members of the CHA/P community to learn how to create online cancer education in culturally relevant ways [21]. CHA/Ps shared that culturally relevant online cancer education includes collaborative development, contextualizing learning, opportunities for connection, and content delivery in relevant ways, which CHA/Ps described as including visuals, story, and locally specific information. These attributes were incorporated into the creation of the webinars. For example, each webinar featured a facilitator from Alaska who worked in cancer prevention and control that offered their knowledge in an Alaska context, engaged learners through story, and facilitated connecting conversations.
Webinars were offered and evaluated in alignment with popular education approaches and Empowerment Theory. The CBPAR framework stems from Paulo Friere’s Popular Education, which advocated for education that empowered and led to social transformation [29]. This theory has also been identified as an effective health education strategy [30]. In addition, some CBPAR theorists advocate that work with Indigenous communities focus on self-determination and empowerment, and acknowledge historical trauma and its impacts [31]. Consequently, health promotion with Indigenous communities may be more culturally relevant and effective when grounded in empowering approaches, and may be able to acknowledge and address some of the underlying causes of a particular concern. For example, for many Indigenous communities, traditional food systems and cultural practices have been disrupted, resulting in historical trauma and lifestyle changes that have been linked by some researchers to contemporary cancer disparities [32]. In this work, we have focused on cultural relevancy, cultural strength, and supporting CHA/Ps’ capacity to change the story of cancer for themselves and their communities.
Empowerment is a participatory process linked to self-determination [33]. It is intended to advance social justice and promote wellness through participant/academic collaboration [33]. Empowerment Theory articulates both empowering processes (such as those involved in CBPAR work) and empowering outcomes that we have used to guide our evaluations [34]. The authors of Empowerment Theory have acknowledged that it can be applied to a diversity of contexts, and consequently no one set of evaluation measures is appropriate [34]. Instead, they articulated three constructs to inform evaluation items and intended outcomes: intrapersonal (changes in the way an individual thinks of themselves), interactional (changes in their understandings), and behavioral (actions an individual takes to directly influence outcomes) [34]. Our evaluation surveys include items developed to measure each of these three constructs.
Methods
Learners
The webinars were offered for Alaska’s CHA/Ps; however, no master contact email list for CHA/Ps currently exists. Each tribal health organization maintains and protects the information of the CHA/Ps they employ. Consequently, the project team reached out to CHA/Ps by putting information in the CHAP Newsletter and on the CHAP website, as well as contacting previous in-person course participants, CHAP Directors, CHAP Training Center Coordinators, the CHAP Academic Liaison, and the Community Health Aide Association President. All outreach materials encouraged individuals to share information about the webinars with other CHA/Ps who might be interested in participating.
Curriculum
Each of the ten webinars was a 1-hr learning experience that CHA/Ps could engage in over their lunch hour. The webinars were designed to support CHA/Ps in their capacity as healthcare providers and community members, and to address each learner’s concerns on a specific topic in real time. Each webinar featured an Alaska facilitator with content knowledge expertise, grounded in an Alaska context. Two project team members also participated in each webinar for relationship-building continuity and to manage technical challenges. The webinars were hosted online on the Alaska Native Tribal Health Consortium (ANTHC) Distance Learning Network. Consistent with the CBPAR principles of co-learning and collaborative work [35], learners were asked for continued input both during the webinars, and on end-of-webinar evaluations, with iterative adjustments made to the webinars in response to learner comments.
Measures
After completing a webinar, learners were invited to complete an evaluation survey that included questions on perceived changes in their comfort and capacity to talk about cancer, intent to share information about cancer, and intent to reduce their own cancer risk factors, as well as demographic variables. To participate in a webinar, individuals had to create an account on the ANTHC Distance Learning Network. This process assigned a user ID to each learner, which allowed the project team to identify unique learners. Learners were required to submit their end-of-webinar evaluation survey before receiving 1 hr of approved CHAP Continuing Education. The evaluation was developed to better understand learners’ perceptions of the webinars and to measure empowerment outcome constructs. Questions measured the Empowerment Theory constructs of “intrapersonal” (changes in learners’ comfort, confidence, and preparation to talk to others about cancer), “interactional” (changes in learners’ knowledge about cancer), and “behavioral” (intent to make changes to reduce cancer risk, and intent to support others to reduce their cancer risk). Learners completed the surveys on the ANTHC Distance Learning Network. The survey data was downloaded from the network, then cleaned and summarized in Microsoft Excel 2016. The qualitative responses were open-coded in Microsoft Excel, and responses were summarized by common theme.
Results
Learners
There were 389 CHA/Ps practicing in Alaska as of July 2018 (via personal communication with the Director of CHAP Rural Health Services). As there is no CHA/P master contact list, it is unclear how many CHA/Ps were aware of the webinars, and a response/participation rate can consequently not be calculated. A total of 11 unique CHA/Ps completed 41 evaluation surveys for the ten webinars held between February and April 2018. Learners were invited to complete a survey after each webinar they participated in.
Learners Intend to Reduce Their Own Cancer Risk
Learners were asked if they intended to change the ways they took care of themselves within the next six months, as a result of participating in the webinar. Responses are summarized in Table 1.
All learners reported that, as a result of the webinars, they intended to change their behavior to reduce their own cancer risk within the next six months. Almost all learners (91%) planned to increase their physical activity and more than half planned to eat healthier (64%) and have a recommended cancer screening exam (55%).
Learners Plan to Talk with Patients More Often About Cancer Risk Reduction Behaviors
In response to a prompt about talking with their patients about cancer risk reduction behaviors, learners reported that, as a result of the webinars, they planned to talk with their patients more often about screenings, tobacco cessation, physical activity, and healthy eating. Survey responses are summarized in Table 2.
As a result of participating in the webinars, all learners reported that they planned to talk with their patients more often about cancer risk reduction behaviors. Learners shared that they planned to talk with their patients more often about cancer screenings (91%), increasing physical activity (82%), cutting down on tobacco use and tobacco cessation (82%), and eating healthy (64%). Some learners also wrote in comments about how they planned to share cancer information with their patients, such as “encourage tobacco users to stop using and make referral to the tobacco cessation with every patient that wants to quit.”
Learners Report Increased Capacity to Share Information on Cancer
Learners were asked if their perceptions of comfort, confidence, preparation, and knowledge about cancer had changed as a result of participating in a webinar. Responses are summarized in Table 3.
As a result of the webinars, learners reported feeling on average between “more” and “much more” comfortable, confident, prepared, and knowledgeable to talk about cancer.
Conclusions
Findings from the evaluation surveys suggest that the supplemental webinars supported learners to feel more comfortable, confident, knowledgeable, and prepared to share information about cancer with their patients, families, friends, and communities. Survey results indicate that the webinars inspired learners to intend to reduce their own cancer risk and talk with their patients more often about cancer. Given that healthcare providers talking with patients about modifiable cancer risk factors is a significant determinant of patient behavior, learners’ increased capacity and intent to engage with their patients about cancer is a promising indicator of future shifts in patient behaviors. In theoretical models such as the Theory of Reasoned Action, the Theory of Planned Behavior, and the Integrated Behavioral Model, intention is seen as the most important determinant of behavior [35]. However, behavioral intention (such as intent to talk about cancer screenings with patients) may not necessarily be realized in lived behavior. A systematic review found that healthcare professionals’ intentions were a significant predictor of provider behavior in 50% of examined studies, while provider beliefs about their capabilities were a significant predictor of behavior in 63% of examined studies [36]. These correlations were found despite the lack of a culturally relevant intervention to support either high levels of intent, increased beliefs in capabilities, or empowered intention of planned behavior. Additional research would be needed to assess the impact of learning on their own behavior and their interactions with patients and subsequent patient behavioral changes.
These webinars were developed to supplement online learning modules that address Alaska’s rural primary care providers’ need for online access to timely, accurate, and relevant information about cancer. Previously published evaluations of the online modules indicate that the modules have supported learners to intend to reduce their own cancer risk [22] and have supported CHA/Ps to intend to share cancer information with their patients, families, friends, and community members [23]. The findings from these webinars reveal similar results; however, the reach of the webinars was far smaller than the number of individuals engaged in the modules; a total of 264 learners had completed a module evaluation survey as of August 1, 2019, while only 11 individuals participated in the webinars. These differences in size are a valuable learned lesson, although the exact reasons for this discrepancy are unclear. While the webinars were developed in response to CHA/Ps’ requests to have synchronous sessions, few CHA/Ps were actually able to attend one of the webinars. Perhaps online educational opportunities offered at discrete times are a challenge for busy working professionals to fit into their lives, especially with unexpected patient encounters that may coincide with the timing of the education.
The lack of a master contact list makes it unclear what percentage of CHA/Ps were aware of the webinars, which may have contributed to the low number of participants. A master contact list of all CHA/P emails may have increased the reach of the webinars and been an effective strategy to increase engagement. Further research would be needed to determine both what the barriers are to engaging CHA/Ps in synchronous online learning, and whether additional efforts at synchronous online education offered to Alaska’s CHA/Ps may encounter similar challenges.
Online education such as these webinars and online modules relies on internet access, which all CHA/Ps have available in their clinics. However, many CHA/Ps do not have access to the internet at home, with only 52% of respondents to a 2015 online survey reporting daily access to the internet at home [27]. Consequently, CHA/P participation in an online educational opportunity relies on employer support of CHA/Ps engaging while at work.
Discussion
The webinars addressed CHA/Ps’ desire for supplemental synchronous interactions about cancer. As a result of the webinars, all learners intended to reduce their own cancer risk, improve the ways they talked with their patients about cancer, and 91% felt more or much more knowledgeable, prepared, comfortable, and confident talking about cancer with their patients, family, friends, and community members. However, the ten webinars engaged only 11 unique learners, while previously developed online modules [22, 23] have engaged over 250 unique learners. This experience may inform other cancer educators’ efforts to develop, implement, and evaluate online learning opportunities. Despite the relatively small numbers, these webinars resulted in increased learners’ intent to reduce cancer risk behaviors, share cancer information, and improved learners’ capacity to talk about cancer in their communities. In the words of learners:
“I am enjoying these classes very much, and they have such great information and it’s so good just to refresh our minds.”
“Screening saves lives. Colon Cancer is preventable. There are other ways to get screened, even from home. Highlights that I find important on my next patient education”
References
CDC/National Center for Health Statistics (2017) FastStats, Deaths and Mortality. [Online]. Available: https://www.cdc.gov/nchs/fastats/deaths.htm. Accessed 09 Jun 2017
Centers for Disease Control and Prevention (CDC) (2017) Leading causes of death, National Center for Health Statistics. [Online]. Available: https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Accessed 14 Jan 2019
Blake I, Holck P, Provost EM (2016) Alaska Native Mortality Update: 2009-2013. Alaska Native Epidemiology Center, Anchorage
Carmack AM, Schade TL, Sallison I, Provost EM, Kelly JJ (2015) Cancer in Alaska Native people: 1969-2013, the 45 year report. Alaska Native Tumor Registry, Alaska Native Epidemiology Center, Alaska Native Tribal Health Consortium, Anchorage
Nash SH, Redwood DG (2018) Potentially preventable cancers among Alaska Native people. Cancer Health Disparities 2
National Survey Reveals Most Americans Are Unaware of Key Cancer Risk Factors (2017) ASCO. [Online]. Available: https://www.asco.org/advocacy-policy/asco-in-action/national-survey-reveals-most-americans-are-unaware-key-cancer-risk. Accessed 14 Jan 2019
Behavioral Risk Factor Surveillance System, Alaska Department of Health and Social Services, Division of Public Health, Section of Chronic Disease Prevention and Health Promotion (2018) AK-IBIS - Query Result - Alaska’s Behavioral Risk Factors Surveillance System - (BRFSS_C) Query Module - Smoking Status. [Online]. Available: http://ibis.dhss.alaska.gov/query/result/BRFSS23/BRFSS_CM/XSMOKER.html. Accessed 14 Jan 2019
Behavioral Risk Factor Surveillance System, Alaska Department of Health and Social Services, Division of Public Health, Section of Chronic Disease Prevention and Health Promotion (2018) AK-IBIS - Query Result - Alaska’s Behavioral Risk Factors Surveillance System - (BRFSS_C) Query Module - Obesity (30+ BMI). [Online]. Available: http://ibis.dhss.alaska.gov/query/result/BRFSS23/BRFSS_C/XBMIOB.html. Accessed 14 Jan 2019
Behavioral Risk Factor Surveillance System, Alaska Department of Health and Social Services, Division of Public Health, Section of Chronic Disease Prevention and Health Promotion (2018) AK-IBIS - Query Result - Alaska’s Behavioral Risk Factors Surveillance System - (BRFSS_S) Query Module - Less than 5-A-Day Fruits and/or Vegetables. [Online]. Available: http://ibis.dhss.alaska.gov/query/result/BRFSS23/BRFSS_S/XFV5SRVR.html. Accessed 14 Jan 2019
Statewide Data: Breast Cancer Screening (2017) Alaska Native Epidemiology Center, Anchorage, Alaska
Statewide Data: Colorectal Cancer Screening (2017) Alaska Native Epidemiology Center, Anchorage, Alaska
Statewide Data: Cervical Cancer Screening (2017) Alaska Native Epidemiology Center, Anchorage, Alaska
Carcaise-Edinboro P, Bradley CJ (2008) Influence of patient-provider communication on colorectal cancer screening. Med Care 46(7):738–745
Gorin SS, Heck JE (2004) Meta-analysis of the efficacy of tobacco counseling by health care providers. Cancer Epidemiol Prev Biomark 13(12):2012–2022
Petrella RJ, Lattanzio CN (2002) Does counseling help patients get active? Systematic review of the literature. Can Fam Physician 48(1):72–80
Alaska CHAP (2017) Alaska Community Health Aides - About CHAP. [Online]. Available: http://www.akchap.org/html/about-chap.html. Accessed 05 May 2017
Cueva M, Kuhnley R, Cueva K (2012) Enhancing cancer education through the arts: building connections with Alaska Native people, cultures and communities. Int J Lifelong Educ 31(3)
Cueva M, Lanier AP, Kuhnley R, Dignan M (2008) Cancer education: a catalyst for dialogue and action. IHS Prim Care Provid 33
2015 Broadband Progress Report (2015) Federal Communications Commission
2016 Broadband Progress Report (2016) Federal Communications Commission
Cueva K et al (2018) A framework for culturally relevant online learning: lessons from Alaska’s tribal health workers. J Cancer Educ Off J Am Assoc Cancer Educ
Cueva K et al (2017) Culturally-relevant online cancer education modules empower Alaska’s community health aides/practitioners to disseminate cancer information and reduce cancer risk. J Cancer Educ Off J Am Assoc Cancer Educ
Cueva K, Cueva M, Revels L, Dignan M (2018) Culturally-relevant online education improves health workers’ capacity and intent to address cancer. J Community Health:1–7
Glanz K, Rimer BK, Viswanath K (eds) (2015) Health Behavior: Theory, Research, and Practice, 5th edn. Jossey-Bass, San Francisco
Cueva M, Lanier A, Dignan M, Kuhnley R, Jenkins C (2005) Cancer education for community health aides/practitioners (CHA/Ps) in Alaska assessing comfort with cancer. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 20(2):85–88
Kelly JJ, Schade TL, Starkey BM, Ashokkumar R, Lanier AP (2012) Cancer in Alaska Native people: 1969-2008: 40-year report. Alaska Native Tribal Health Consortium, Office of Community Health Services
Cueva K, Revels L, Kuhnley, R, Cueva M, Lanier A, Dignan M 2015 Co-creating a culturally responsive distance education cancer course with, and for, Alaska’s community health workers: motivations from a survey of key stakeholders. J Cancer Educ Off J Am Assoc Cancer Educ
Cajete G (1994) Look to the mountain: an ecology of indigenous education, 1st edn. Kivaki Press, Skyand 585 E
Freire P (2000) Pedagogy of the oppressed, 30th anniversary ed. Continuum, New York
Wallerstein N, Bernstein E (1988) Empowerment education: Freire’s ideas adapted to health education. Health Educ Q 15(4):379–394
Chávez V, Minkler M, Wallerstein N, Spencer M (2010) Community organizing for health and social justice. In: Prevention is Primary, 2nd edn, pp 87–112
Prussing E (2014) Historical trauma: politics of a conceptual framework. Transcult Psychiatry 51(3):436–458
Perkins DD, Zimmerman MA (1995) Empowerment theory, research, and application. Am J Community Psychol 23(5):569–579
Zimmerman MA (1995) Psychological empowerment: issues and illustrations. Am J Community Psychol 23(5):581–599
Israel B, Schulz A, Parker E, Becker BA, Allen A, Guzmán J (2008) Critical issues in developing and following community-based participatory research principles. In: Community-Based Participatory Research for Health
Godin G, Bélanger-Gravel A, Eccles M, Grimshaw J (2008) Healthcare professionals’ intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci 3:36
Funding
This work is part of “Distance Education to Engage Alaskan Community Health Aides in Cancer Control,” supported by the National Cancer Institute of the National Institutes of Health (NIH), award R25CA186882.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
In accordance with the procedure recommended and approved by the Alaska Area Institutional Review Board, the University of Alaska Anchorage Institutional Review Board, and the Southcentral Foundation (SCF) Executive Committee, the cancer education evaluation surveys are research that involve the study of acceptable educational practices in a normal educational setting and are consequently not required to include informed consent.
Conflict of Interest
The authors declare that they have no conflict of interest.
Disclaimer
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number R25CA186882. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cueva, K., Cueva, M., Revels, L. et al. An Evaluation of Cancer Education Webinars in Alaska. J Canc Educ 36, 484–490 (2021). https://doi.org/10.1007/s13187-019-01651-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-019-01651-x