Abstract
Recent cancer care delivery models and clinical practice guidelines have expanded the role of primary care providers (PCPs) in routine follow-up of cancer survivors. We conducted a cross-sectional survey of PCPs affiliated with a large healthcare system to (1) examine practices, attitudes, and beliefs regarding preparedness to provide survivorship care and (2) explore predictors of confidence managing cancer survivors. We distributed a self-administered online survey to 1069 clinical affiliates providing primary care services within the University of Pittsburgh Medical Center system. Associations between PCPs’ professional characteristics and attitudes and preparedness were evaluated. Multiple logistic regression explored predictors of confidence monitoring common cancer treatment-related symptoms. One hundred twenty-seven eligible PCPs responded. The sample was split between academic and community practice (48.0% vs. 52.0%, respectively), predominantly comprised of physicians (81.8%), and 64.6% had > 15 years direct patient care experience. The majority agreed that PCPs play a valuable role in surveillance and adverse event monitoring in survivors, though less than 25% felt their professional training prepared them to perform each of these domains. Physicians were significantly more likely than advanced practice providers to be among the 65% of PCPs who were confident monitoring ≥ 1 symptom in each of the 5 evaluated symptom clusters (OR 3.6, 95% CI 1.2–10.8). PCPs appear willing to assume an enhanced role in cancer survivorship care but feel unprepared to do so. Enhanced training and dissemination of clinical practice guidelines are needed to facilitate effective implementation of PCP-delivered survivorship care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As cancer survival rates continue to improve [1, 2], the need for providers trained in managing the posttreatment needs of cancer survivors is increasingly pressing. In response to this need, the American Cancer Society (ACS) recently published survivorship care guidelines for breast (endorsed by the American Society of Clinical Oncology, ASCO) [3], colorectal [4], prostate [5], and head and neck [6] cancers. These guidelines provide recommendations for each of the four main components of survivorship care, as defined by the seminal 2009 Institute of Medicine report that established survivorship as a unique domain within the care trajectory of a cancer patient [7]: (1) surveillance for cancer metastasis, recurrence, and new primary cancers; (2) assessment and management of physical and psychosocial late effects of cancer treatment; (3) health promotion to prevent new and recurrent cancers; and (4) care coordination to meet the broad health needs of survivors. Consistent with the Institute of Medicine’s recommendation, the ACS guidelines place the vast majority of survivorship care delivery in the hands of primary care providers (PCPs). This PCP-driven model of survivorship care reflects a major shift from the historical paradigm in which oncologists manage most cancer-related clinical follow-up, with PCPs’ involvement limited mainly to cancer prevention and early detection [8].
Recent epidemiologic trends in cancer incidence and survival underscore the importance of integrating PCPs into survivorship care in order to address the changing demands facing oncology. Due to a growing aging population, there will be an increase in the number of cancers that require active management by oncologists [9]. In addition to this uptick in diagnoses, there will be an increase in the number of cancer survivors that will require short-term and long-term follow-up for management of treatment-related symptoms and late effects [2] as well as any existing comorbidities that may worsen after cancer treatment. By assuming a larger role in cancer survivorship, PCPs have the potential to reduce the demand on oncologists [10] and improve healthcare effectiveness and efficiency. Additionally, PCPs may further enhance survivorship care given their expertise in chronic disease management and health promotion, both of which are increasingly recognized as important elements of survivorship care and cancer prevention [11].
Numerous barriers have hindered widespread implementation of the PCP model of survivorship care [12,13,14]. First, while PCPs generally express high willingness to provide survivorship care [15], few report feeling confident that they have the knowledge and skills to do so [16, 17]. This is a sentiment shared by oncologists, particularly with respect to screening for recurrence and managing late effects [18]. In addition to feeling that they lack knowledge to provide survivorship care, PCPs are challenged by increasing workloads and demands on their time [13]. Secondly, without established information systems to facilitate the transition from active to posttreatment care, PCPs have reported difficulties with the care coordination needed for survivorship care [19,20,21]. To fill these gaps and enhance PCP involvement in survivorship care, patient-specific treatment summaries accompanied by a detailed follow-up plan, called survivorship care plans, have emerged over the past decade [7]. ASCO endorsed the widespread development and implementation of survivorship care plans in 2014 [22] and in 2016 the American College of Surgeons Commission on Cancer Standards mandated that every cancer survivor receives a survivorship care plan upon completion of active treatment [23]. Data on survivorship care plan delivery are scarce, though reports prior to these endorsements demonstrate that fewer than 15% of patients received survivorship care plans and fewer than half of cancer centers delivered them [24]. Moreover, a recent systematic review suggests that survivorship care plans may have limited impact on health outcomes and patient satisfaction [25]. It is noteworthy that the ACS, ASCO, and the American College of Surgeons, organizations that have provided guidelines related to survivorship care, are not PCP-directed organizations. Additionally, patients may not be comfortable with PCPs providing follow-up cancer screening [26], especially if they were not involved in the active phase of their cancer treatment [27].
Given the recent initiatives by organizations that target cancer providers such as the ACS, ASCO, and the American College of Surgeons to expand PCPs’ roles in survivorship care, it is important to assess PCPs’ knowledge, attitudes, beliefs, and practices regarding their evolving role in this new care paradigm to determine the need for additional training and support interventions. Here, we present data from a cross-sectional survey of PCPs affiliated with a large healthcare delivery system (including academic and community practices) that has taken steps to comply with the American College of Surgeons survivorship care plan mandate. Our primary aim is to examine PCPs’ current knowledge, attitudes, beliefs, and practices regarding their preparedness to provide survivorship care. Secondarily, we also explore predictors of confidence in an attempt to identify subgroups of PCPs who may benefit from increased training and support.
Methods
Study Setting
In September 2016, we emailed a self-administered online survey to all clinical affiliates of the University of Pittsburgh Medical Center (UPMC) who provide primary care services and have valid UPMC email addresses (n = 1069). After our initial approach email, we sent three reminder emails to nonresponders over the following 2 months. The survey was housed in Qualtrics (Qualtrics, Provo, UT). The University of Pittsburgh Human Research Protection Office approved our protocol, and all respondents provided informed online consent prior to participation. PCPs were not compensated for participation in the survey.
Participants
PCPs with clinics based in any clinical service (e.g., internal medicine and its subspecialties, family medicine, obstetrics/gynecology) were eligible for participation. All provider types (e.g., physicians, nurse practitioners, physician assistants) were eligible. PCPs were ineligible if they self-identified as not providing primary care clinical services or were in training at the time of survey completion.
Survey
Our survey was based on the National Survey of Primary Care Physicians’ Recommendations and Practice for Breast, Cervical, Colorectal, and Lung Cancer Screening, a national survey conducted from 2006 to 2007 that assessed PCPs’ knowledge, attitudes, recommendations, and practices related to screening for various cancers [28] as well as the SPARCCS Study [26]. To focus our survey on attitudes and beliefs regarding preparedness to provide survivorship care, our multidisciplinary team of investigators—which included a medical oncologist-survivorship specialist, a medical oncologist, a PCP, a cancer survivor, and a geriatrics-trained epidemiologist—tailored the questions to target our areas of interest. Before distributing our survey to the study population, we piloted it among other academic physicians to ensure clarity and made adjustments where needed.
The final survey included 40 items and was estimated to take 10–20 min to complete. Professional and practice characteristics (e.g., practice setting, provider type, subspecialty, percent of clinical effort spent in primary care, years spent in direct patient care) were assessed using multiple choice and short answer formats. Prior involvement in the care of cancer survivors was assessed using a yes/no format. Attitudes toward PCP involvement in various aspects of cancer care, preparedness to provide survivorship care, awareness of survivorship guidelines, and adequacy of ongoing education about survivorship were assessed using a 4-point Likert scale reflecting level of agreement (strongly agree, somewhat agree, somewhat disagree, strongly disagree). Perceived confidence in the ability to monitor 15 of the most common cancer disease and cancer treatment-related adverse events [28] was assessed using a yes/no format.
Statistical Analysis
We report descriptive statistics using counts and percentages for each survey item. We categorized attitudes and preparedness based on whether respondents indicated that they strongly or somewhat agreed vs. strongly or somewhat disagreed with statements asking whether a PCP plays a valuable role in various aspects of cancer care (attitudes) and whether their training and ongoing education prepared them to provide each of these aspects of care (preparedness). We used the χ2 tests to evaluate whether professional and practice characteristics and prior involvement caring for cancer survivors were associated with attitudes and preparedness. To explore PCPs’ confidence in their ability to monitor specific common treatment-related adverse events, for each symptom we counted the number of respondents who answered “yes” to the question of whether they are confident that they have the skills needed to monitor that symptom. To create an overall score reflecting a PCPs’ confidence in monitoring the range of symptom clusters that are important for providing comprehensive survivorship care, we also categorized the 15 symptoms into five physiologically related symptom clusters (i.e., general symptoms, pain, neuropsychological symptoms, hormonal symptoms, late effects) and created an overall confidence score (range 0–5) by calculating the number of clusters for which a PCP reported confidence in monitoring at least one symptom. We explored possible provider-level predictors of PCPs’ overall confidence score using multiple logistic regression, with the confidence score dichotomized into PCPs who were confident in all five symptom clusters (score = 5) vs. PCPs who were confident in fewer than five clusters (score ≤ 4). A p value < 0.05 was considered statistically significant for all analyses. Analyses were conducted with Stata 14.0 (StataCorp, 2015).
Results
Of the 1069 surveys distributed, 146 were returned (13.7% response rate); of these, 19 were ineligible because the respondents were trainees or did not provide primary care services.
Professional and Practice Characteristics
PCPs in our sample were evenly split between academic and community practice settings (48.0% vs. 52.0%, respectively) (Table 1). Most were trained as physicians (81.8%) and had over 15 years of experience in direct patient care (64.6%). Nearly 80% reported past experience performing surveillance in cancer survivors, though smaller proportions reported past experience with treatment-related adverse event monitoring (64.9%) and management (62.3%) in survivors.
Attitudes Toward PCP Involvement in Cancer Care
In general, a majority of study participants agreed that a PCP plays a valuable role in all aspects of the cancer care continuum. Most felt that PCPs are valuable after completion of active treatment: 88.8% (n = 102) and 86.1% (n = 99), respectively, perceived PCPs as valuable consultants to the oncology team and as principal practitioners providing surveillance and adverse event monitoring during this period. Smaller, but still majority, proportions felt that PCPs are valuable as consultants during treatment planning (80.0%, n = 92) and active treatment (73.0%, n = 84).
Confidence in Monitoring Treatment-Related Adverse Events
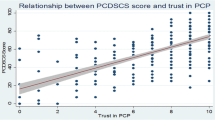
Overall, the vast majority of PCPs (81.2–91.4%) felt confident in their ability to monitor at least one symptom in each of the adverse event symptom clusters (Table 2). PCPs were most confident in monitoring the individual symptoms of depression (88.9%), anxiety (86.3%), general pain (76.1%), fatigue (79.5%), weight change (80.3%), and osteoporosis/osteopenia (83.8%). Cardiotoxicity was the only individual symptom for which less than half (41.9%) indicated confidence in monitoring. Sixty-five percent were confident monitoring at least one symptom in all of the five clusters. In a multiple regression model, the only provider-level characteristic associated with confidence in adverse event monitoring was provider type, with physicians 3.6 times more likely than advanced practice providers to report confidence in monitoring at least one symptom in all five symptom clusters (OR 3.6, 95% CI 1.2–10.8, p = 0.02) (Table 3).
Preparedness to Provide Survivorship Care and Awareness of Survivorship Guidelines
Most PCPs reported that their formal professional training did not prepare them to provide survivorship care and that ongoing education filled in these gaps in some, but not all, survivorship domains (Table 3). For instance, whereas only 20.1% felt their formal training had prepared them to perform cancer surveillance for a survivor, 65.8% perceived the current education they receive about surveillance as adequate. Likewise, 23.7% felt prepared to perform adverse event monitoring in survivors, but only 49.1% felt that current education in this area was adequate. PCPs in the community (p = 0.02) and PCPs who spend > 50% of their clinical effort in primary care (p = 0.03) were more likely to perceive their ongoing education about adverse event monitoring as adequate. Prior involvement in each of the domains of cancer care was associated with both preparedness and perception of adequate education about surveillance and monitoring (all ps < 0.03). Twenty to 35% of PCP respondents reported that they had not been involved with survivorship care at all. Only 16.5% of respondents were aware of the 2015 ACS/ASCO breast cancer survivorship care guideline, though 61.5% of those who were aware had used it in practice. Similarly, only 24.8% were aware of the term “survivorship care plan,” and of these, less than half (43.3%) understood the PCP’s role in a survivorship care plan. No professional or practice characteristic was associated with survivorship guideline or care plan awareness (all ps > 0.05).
Discussion
To the best of our knowledge, this is the first report to examine PCPs’ knowledge, attitudes, beliefs, and practices regarding preparedness to provide cancer survivorship care since the publishing of the ACS survivorship guidelines that delegate a large degree of survivorship care to PCPs. Our results corroborate findings from earlier PCP surveys [15, 16], indicating that PCPs’ views have not changed in the 2 to 4 years since the ACS guidelines were published: while PCPs largely view themselves as valuable providers of survivorship care, they continue to feel underprepared to perform the tasks needed for this role. Critically, we also demonstrate that over 75% of our respondents were unaware of the ACS/ASCO breast cancer survivorship guideline, which raises serious concerns about PCPs’ potential to implement guideline-based survivorship care for breast cancer and other common cancers effectively. The research team is unaware of any unilateral or coordinated, consistent, or large-scale efforts among the discipline of oncology to disseminate these ACS/ASCO guidelines to PCPs.
Despite much recent attention within the cancer community regarding the design and implementation of nononcologist driven survivorship care models [12, 14, 21], our results suggest that there is still a large amount of ambiguity about which provider is primarily responsible for cancer-related follow-up. Our data indicate that current practice patterns may not reflect the proposed model of PCP-driven survivorship care, as up to a third of PCPs in our sample reported no prior involvement in various aspects of survivorship care—a higher proportion than would be expected from a cohort in which a majority have been in practice for at least 5 years. Our data also indicate that the American College of Surgeons Commission on Cancer Standards directive to provide all survivors with a survivorship care plan (SCP) upon completion of active treatment may have limited penetrance; less than one-quarter of PCPs in our sample were aware of the term “survivorship care plan” and, of these, less than half understood the PCP’s role in executing them. While SCPs outline what should be done and when, they do not specify who should do which activity resulting in the bystander effect where no one does anything. SCPs should be clarified so that effective communication takes place and roles are more clearly defined between oncologists and PCPs.
It is unknown whether these discrepancies between the cancer community’s directives and PCP uptake of them are driven by dissemination barriers or an implementation gap on the part of hospital systems, oncologists, or PCPs. In any case, more effort is needed to educate and empower PCPs for their evolving role in survivorship care and to design practical care models that facilitate PCPs’ transition to this role. Data from the past decade confirm our findings that PCPs desire more education on best practices in cancer survivorship care: in two large surveys of PCPs, over 90% of PCPs reported high utility of clinical practice guidelines for follow-up of cancer survivors and over 75% favored more CME opportunities for cancer follow-up care [15, 16]. Our sample provides a more granular view of the specific education deficits that PCPs perceive, namely, monitoring and managing posttreatment adverse events and, to a lesser extent, cancer surveillance. These findings indicate that PCPs will readily embrace survivorship-related educational opportunities, and that the cancer community should strive to disseminate clinical practice guidelines and education to PCP-centric outlets. It may also be useful to leverage the electronic medical record to include individualized survivorship-specific guidelines as best practice alerts for cancer survivors; this may help to bridge the dissemination gap that likely exists between the subspecialty organizations promoting SCPs and the PCPs who are tasked with implementing them.
Optimistically, we found that the majority of our respondents felt confident in their ability to monitor most common cancer-related symptoms. PCPs were particularly strong in monitoring psychological symptoms, general symptoms such as pain, fatigue, and weight change, and bone health. This likely reflects the overlap between prevalent problems in the general population that PCPs manage daily in their typical patient panel. Interestingly, we found that physicians were more likely than advanced practice providers to feel confident monitoring all of the symptom clusters that are relevant in survivors. The reasons for this are unclear, particularly because physicians and advanced practice providers did not differ in their perception of preparedness based on their formal professional training. Nevertheless, this underscores the need for more training to target the full range of providers who deliver care to cancer survivors, particularly given that advanced practice providers comprise a sizeable and growing proportion of PCPs in this country [29].
Specifically, survivorship care guidelines need to be disseminated in a more timely, convenient, consistent, and integrated/accessible manner to not only cancer providers but also PCPs. In addition, education around the performance of adverse event monitoring is necessary, and education related to assessing and managing symptoms in the context of a cancer diagnosis is required, since more PCPs had decreased experience with monitoring and managing adverse events, yet they want to be valuable at all times during cancer treatment. Continuing education for both physicians and advanced practice providers in primary care should include not only common but also uncommon adverse effects of cancer treatments so that PCPs are aware of the range of symptoms for which they need to screen their cancer survivors. It may also be useful to expand the multidisciplinary team caring for cancer survivors to include clinical pharmacists with training in oncology, who can advise PCPs on monitoring strategies based on the treatment regimens their patients received.
Limitations
Our study has several limitations. First, our low response rate may have introduced a response bias that favored PCPs who are supportive of PCP involvement in survivorship care. However, the problem of low survey response rates among physicians [30] and particularly specialists [31] has been well documented, and work in this area suggests that nonresponse bias is less meaningful in physician surveys than in surveys of the general public [32]. Second, because we only surveyed PCPs from our hospital system, which has an integrated provider/insurer model and supports a dedicated survivorship clinic run by a medical oncologist-survivorship specialist, our findings may not be generalizable beyond our region. Third, our small sample size precluded sufficiently powered analyses of provider-level predictors of attitudes, beliefs, and guideline awareness, as well as any analyses comparing the views of PCPs and oncologists who provide survivorship care.
Conclusions
Our survey suggests that PCPs’ views on cancer survivorship have not changed in tandem with the shifting views of the oncology field, which support transitioning a large degree of survivorship care to PCPs. However, although PCPs are largely unaware of the guidelines that place a significant amount of survivorship care under their purview, they are nonetheless willing to take on that role and desire more education on how to do so effectively. To facilitate the field’s transition to increased PCP-delivered survivorship care, leaders in both oncology and primary care must strive for an enhanced collaborative effort to (1) disseminate survivorship guidelines directly to PCP audiences, (2) champion training opportunities for PCPs to develop their clinical competencies needed to provide best practices cancer survivorship care, and (3) promote the development of health information systems that support point-of-care decision-making and care coordination.
References
Group, U.S.C.S.W., United States Cancer Statistics: 1999–2013 incidence and mortality web-based report, C.f.D.C.a.P. Department of Health and Human Services, and National Cancer Institute, Editor. 2016: Atlanta (GA)
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66(4):271–289
Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, Cannady RS, Pratt-Chapman ML, Edge SB, Jacobs LA, Hurria A, Marks LB, LaMonte SJ, Warner E, Lyman GH, Ganz PA (2016) American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. J Clin Oncol 34(6):611–635
El-Shami K et al (2015) American Cancer Society Colorectal Cancer Survivorship Care Guidelines. CA Cancer J Clin 65(6):428–455
Skolarus TA, Wolf AM, Erb NL, Brooks DD, Rivers BM, Underwood W 3rd, Salner AL, Zelefsky MJ, Aragon-Ching JB, Slovin SF, Wittmann DA, Hoyt MA, Sinibaldi VJ, Chodak G, Pratt-Chapman ML, Cowens-Alvarado RL (2014) American Cancer Society prostate cancer survivorship care guidelines. CA Cancer J Clin 64(4):225–249
Cohen EE et al (2016) American Cancer Society Head and Neck Cancer Survivorship Care Guideline. CA Cancer J Clin 66(3):203–239
Hewitt M, Greenfield S, Stovall E (2006) From cancer patient to cancer survivor: lost in transition. National Academies Press, Washington, D.C
Cheung WY, Neville BA, Cameron DB, Cook EF, Earle CC (2009) Comparisons of patient and physician expectations for cancer survivorship care. J Clin Oncol 27(15):2489–2495
Rowland JH, Bellizzi KM (2014) Cancer survivorship issues: life after treatment and implications for an aging population. J Clin Oncol 32(24):2662–2668
Erikson C, Salsberg E, Forte G, Bruinooge S, Goldstein M (2007) Future supply and demand for oncologists : challenges to assuring access to oncology services. J Oncol Pract 3(2):79–86
Leach CR, Weaver KE, Aziz NM, Alfano CM, Bellizzi KM, Kent EE, Forsythe LP, Rowland JH (2015) The complex health profile of long-term cancer survivors: prevalence and predictors of comorbid conditions. J Cancer Surviv 9(2):239–251
Nekhlyudov, L., M. O’Malley D, and S.V. Hudson, Integrating primary care providers in the care of cancer survivors: gaps in evidence and future opportunities. Lancet Oncol, 2017. 18(1): p. e30-e38
Jacobs LA, Shulman LN (2017) Follow-up care of cancer survivors: challenges and solutions. Lancet Oncol 18(1):e19–e29
O’Malley D et al (2017) Learning the landscape: implementation challenges of primary care innovators around cancer survivorship care. J Cancer Surviv 11(1):13–23
Del Giudice ME et al (2009) Primary care physicians’ views of routine follow-up care of cancer survivors. J Clin Oncol 27(20):3338–3345
Bober SL, Recklitis CJ, Campbell EG, Park ER, Kutner JS, Najita JS, Diller L (2009) Caring for cancer survivors: a survey of primary care physicians. Cancer 115(18 Suppl):4409–4418
Luctkar-Flude M, Aiken A, McColl M, Tranmer J, Langley H (2015) Are primary care providers implementing evidence-based care for breast cancer survivors? Can Fam Physician 61(11):978–984
Potosky AL, Han PKJ, Rowland J, Klabunde CN, Smith T, Aziz N, Earle C, Ayanian JZ, Ganz PA, Stefanek M (2011) Differences between primary care physicians’ and oncologists’ knowledge, attitudes and practices regarding the care of cancer survivors. J Gen Intern Med 26(12):1403–1410
Sada YH et al (2011) Primary care and communication in shared cancer care: a qualitative study. Am J Manag Care 17(4):259–265
Rubinstein EB, Miller WL, Hudson SV, Howard J, O’Malley D, Tsui J, Lee HS, Bator A, Crabtree BF (2017) Cancer survivorship care in advanced primary care practices: a qualitative study of challenges and opportunities. JAMA Intern Med 177(12):1726–1732
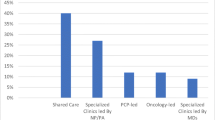
Rosenzweig MQ, Kota K, van Londen G (2017) Interprofessional management of cancer survivorship: new models of care. Semin Oncol Nurs 33(4):449–458
Mayer DK, Nekhlyudov L, Snyder CF, Merrill JK, Wollins DS, Shulman LN (2014) American Society of Clinical Oncology clinical expert statement on cancer survivorship care planning. J Oncol Pract 10(6):345–351
Surgeons, C.o.C.o.t.A.C.o., Cancer program standards: ensuring patient-centered care (2016 edition). 2015
Cowens-Alvarado R, Sharpe K, Pratt-Chapman M, Willis A, Gansler T, Ganz PA, Edge SB, McCabe M, Stein K (2013) Advancing survivorship care through the National Cancer Survivorship Resource Center: developing American Cancer Society guidelines for primary care providers. CA Cancer J Clin 63(3):147–150
Jacobsen PB et al (2018) Systematic review of the impact of cancer survivorship care plans on health outcomes and health care delivery. J Clin Oncol:Jco2018777482
Survey of physician attitudes regarding the care of cancer survivors. Available from: https://healthcaredelivery.cancer.gov/sparccs/],
Radhakrishnan, et al. (2019) Provider involvement in care during initial cancer treatment and patient preferences for provider roles after initial treatment. J Oncol Pract 15(4):e328–e337
Institute, N.C. National Cancer Institute, National survey of primary care physicians’ recommendations and practice for breast, cervical, colorectal, and lung cancer screening. Available from: https://healthcaredelivery.cancer.gov/screening_rp/
Bureau of Labor Statistics, U.S.D.o.L., Physician assistants, in Occupational outlook handbook
Cook DA et al (2016) Incentive and reminder strategies to improve response rate for Internet-based physician surveys: a randomized experiment. J Med Internet Res 18(9):e244
Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, Samuel S, Ghali WA, Sykes LL, Jetté N (2015) Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 15:32
Kellerman SE, Herold J (2001) Physician response to surveys. A review of the literature. Am J Prev Med 20(1):61–67
Funding
This work was supported by grant TL1 TR000145 from the National Center for Advancing Translational Sciences of the National Institutes of Health and grant P30 CA047904 from the National Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 85 kb)
Rights and permissions
About this article
Cite this article
Geramita, E.M., Parker, I.R., Brufsky, J.W. et al. Primary Care Providers’ Knowledge, Attitudes, Beliefs, and Practices Regarding Their Preparedness to Provide Cancer Survivorship Care. J Canc Educ 35, 1219–1226 (2020). https://doi.org/10.1007/s13187-019-01585-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-019-01585-4