Abstract
The importance of mentorship in medicine and its impact on academic and professional development has been widely studied. However, mentorship for medical students in the field of radiation oncology is limited. Our radiation oncology department developed a formal medical student mentorship program in 2004. This program included both clinical and research mentoring pathways. Our study aims to gain feedback and perspective from former medical student participants who subsequently entered into a radiation oncology residency program. An anonymous survey was sent to 22 former students in the mentorship program from 2005 to 2016 who entered a radiation oncology residency program. The survey included Likert scales (1–5), multiple choice, strength category rankings, and free responses. Data was compiled and analyzed with Qualtrics data software. The survey response rate was 100%. Seventeen (77.3%) participants reported that the mentorship program strongly affected their career choice and a majority reported that their research experience strongly (45.5%) or moderately affected (31.8%) their career choice. Fourteen (63.6%) respondents reported that the mentorship program was very effective and 8 (36.4%) reported it as being effective. Eighteen (81.8%) respondents reported that mentorship was extremely important to their career. Students participating in the research pathway also reported improvement in valuable skills such as presentations, abstract writing, manuscript writing, statistical analysis, and coordination with colleagues. A total of 66.7% of attending radiation oncologists who previously participated in this program now practice in an academic setting. Our institution successfully developed a formalized mentorship program for medical students interested in radiation oncology. Participants in this program reported high levels of satisfaction and emphasized the importance of mentorship in the development of valuable research competencies and on their overall career path. This program can serve as a model for future mentorship initiative in medical school.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mentorship in medicine has been widely acknowledged to impact academic and professional development for mentees throughout their careers [1,2,3]. A mentoring relationship should be mutually beneficial, providing the mentor with improved leadership ability, self-esteem, and personal satisfaction [2]. Previous qualitative studies suggest that an ideal mentor should be a career guide, make a time commitment to the mentee, support a balance in personal and professional life, and possess qualities such as enthusiasm and compassion [4]. As mentorships require the participation of two individuals, the basis of successful mentoring relationships should be built on mutual goals and principles of respect, reciprocity, and commitment [5]. Across medicine, robust mentorship programs have been associated with higher rates of academics as a career choice [6, 7], higher retention of physicians in academic practice [8], and increased research productivity [9,10,11]. Within the field of radiation oncology, mentorship is associated with increased research productivity and a longer career duration [12]. Mentoring of residents also impacts the quality of residency training and formal residency mentoring programs are associated with greater overall satisfaction with the mentorship process. However, only 50% of residents report having a mentor [13].
The aforementioned studies have primarily assessed the role of mentorship in residents, fellows, and junior faculty members with little emphasis on the benefits of mentorship for medical students, particularly within the field of radiation oncology. At our institution, we have offered a formalized radiation oncology mentorship initiative (ROMI) since 2004. This initiative pairs students with radiation oncology faculty at our institution for a clinical mentorship track, a research mentorship track, or a combined track. The clinical track includes one or more formal rotations in the radiation oncology department, either as an introduction to clinical medicine course in the preclinical years or an elective rotation in the clinical years. Further clinical opportunities are offered through a partnership with the medical school student oncology society. The research track provides an opportunity for students to develop their own project or join ongoing research projects within the department. Research is conducted throughout the year alongside course work, during a dedicated research block, or during a summer research program. Students are mentored and supported in the development of abstracts, poster presentations, and manuscripts for submission to academic journals. Both tracks also involve regularly scheduled meetings with their faculty mentor to discuss progress and work on professional development [14]. Informal mentorship is also provided through a radiation oncologist–led, preclinical oncology module and an optional week-long radiation oncology experience during the required radiology clerkship for third-year medical students [15]. At our institution, mentorship in radiation oncology has had a positive impact on specialty selection as well as the research productivity of students and faculty participating in ROMI [14]. In this study, we sought to gain direct feedback and perspectives of former program mentees who entered into a radiation oncology residency. We describe the mentee-reported efficacy of the mentorship program and aim to utilize the collected data to optimize ROMI.
Methods and Materials
This study was deemed exempt from our Institutional Review Board. Radiation oncology faculty voluntarily participated in the approval and administration of surveys for this study. Using publicly available National Residency Match Program and our ROMI student registry from 2005 to 2016, we identified 22 former medical students as participants in ROMI who subsequently entered a radiation oncology residency program. A Qualtrics Internet-based, anonymous, voluntary survey was sent to all 22 former medical students from our institution. Consent was solicited on the cover page, emphasizing that participation was voluntary and anonymous. Participants were permitted to skip questions. The survey used free-response, Likert scale, multiple choice, and strength category rankings. The Likert scales all included ranges from 1 to 5, but varied in terminology as follows to suit individual questions: None–All, Very Poor–Very Good, Poor–Excellent, Very Dissatisfied–Very Satisfied, Very Ineffective–Very Effective, and Not at all Important–Extremely Important. The results were compiled and analyzed using Qualtrics data software.
Results
The survey response rate was 100% (n = 22). The characteristics of respondents are seen in Table 1. Of the 9 respondents who were attending radiation oncologists, 6 (66.7%) remained in academia and 3 (33.3%) were in private practice.
All 22 (100%) participants reported taking a radiation oncology elective within our department while in medical school. Sixteen (72.7%) reported being very satisfied, 5 (22.7%) reported being satisfied, and 1 (4.5%) had a neutral attitude towards the rotation (Likert average 4.68, “satisfied” towards “very satisfied”). When asked how well medical school educated them on the role of a radiation oncologist, 13 (59.1%) reported it was effective or very effective (Likert average 3.5, “neither effective nor ineffective” to “effective”). Fourteen (63.6%) respondents reported they felt good or very good about their competitiveness when applying for residency programs (Likert average = 3.64, “fair” to “good”).
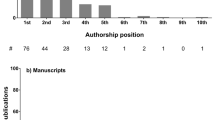
Seventeen (77.3%) participants reported that their experience with radiation oncology mentorship strongly affected their career choice, while 2 (9.1%) reported it had a moderately affected their decision. The majority of respondents also identified their research experience as strongly affecting (45.5%) or moderately affecting (31.8%) their career choice. Seventeen (77.3%) respondents reported that a faculty member at our institution had the greatest influence on their decision to apply for radiation oncology and 2 (9.1%) respondents reported that a faculty member at another institution had the greatest influence on their decision. When asked how important mentorship is to their career, 18 (81.8%) reported it as extremely important and 4 (18.2%) reported it as very important (Likert average = 4.82, “very important” to “extremely important”). Fourteen (63.6%) respondents reported that mentorship at our institution was very effective, while 8 (36.4%) reported that it was effective (Likert average = 4.64, “effective” to “very effective”). Eighteen (81.8%) respondents felt that the mentorship was very useful for the residency application process, while 3 (13.6%) felt it was useful (Likert average = 4.71, “useful” to “very useful”). The 18 students participating in the research track reported that mentorship positively affected a number of important research competencies, particularly research coordination and writing (Table 2). Free text responses on the most effective aspect of radiation oncology education yielded 8 (75%) comments on the mentorship offered by ROMI at our institution.
Discussion
The mentor-mentee relationship is highly valued in medicine, particularly within the field of radiation oncology due to its small community. However, the vast majority of studies, reviews, and guidelines pertaining to mentorship across all medical specialties focus on residents, fellows, and faculty members [16]. Only 36% of medical students in the clinical years have mentors [17]. This percentage is far lower than the reported 53% of radiation oncology residents with mentors, 87% of whom reported it was critical to their training [13]. There have been many recent studies that describe an increased focus on radiation oncology education within the medical school curriculum [18,19,20,21,22]. This focus on improving exposure and education for medical students is well-founded and supported by our own research, which indicates that radiation oncology mentorship during medical school is critical to the success of students interested in the field.
Our formal medical student mentoring initiative had high satisfaction rates, consistent with those seen in formal residency mentoring programs [13]. This program demonstrates the positive impact of mentorship on career choice in radiation oncology. The results of the survey indicate that ROMI also increased exposure to the field of radiation oncology. However, students reported that the medical school was only moderately effective in educating them on the role of a radiation oncologist. This finding is not unique to our institution [19, 23, 24]. In addition to the mentorship program, our radiation oncology department has increased its presence in the medical school through involvement in a student oncology interest group and a radiation oncologist–led preclinical oncology course [25, 26]. We expect that through these formal and informal initiatives, medical student feedback on education in radiation oncology will improve over time. Another significant finding was that mentorship improved the residency application process for students and increased perceived competitiveness when applying for residency. The multifaceted benefits of a formal mentorship program rely on the positive relationships formed between the mentors and mentees. Radiation oncology faculty members should be adequately trained and supported as mentors to allow for the greatest possible impact on their mentees.
Radiation oncology residency programs highly value research experience prior to residency application [27]. Our initiative improved mentee confidence in a number of core research competencies, including abstract writing, manuscript writing, presentations, and coordination with colleagues. These are highly valued skills in medicine, and the ability of formal mentorship initiatives to improve confidence in these areas should not be overlooked. Although only a small proportion of respondents were at the attending level, 67% remained in academics while only 33% entered a private practice. Our findings are consistent with previous studies showing mentorship and research experience increased rates of academic practice among physicians [6, 7].
This study was limited to the mentorship experience of a single institution with no affiliated radiation oncology residency program. Although the survey response was 100%, not all respondents answered every prompt, which could contribute to response bias. Recall bias is inherent in the survey, especially for respondents who graduated from medical school several years ago. In addition, our study lacks a control group for comparison of survey responses.
The radiation oncology mentoring initiative at our institution has been demonstrated to be a model of success for formal mentoring programs in medical school. Formal mentoring programs have also been shown to maximize benefit for the mentoring relationship compared with informal programs [13]. The positive results from our institution should be used as a guide for the development of medical student mentorship programs by radiation oncology departments nationwide. Widespread implementation of formal mentoring initiatives would enable more rigorous research to be conducted on the benefits to both mentees and mentors.
References
Thomas-Maclean R, Hamoline R, Quinlan E, Ramsden VR, Kuzmicz J (2010) Discussing mentorship: an ongoing study for the development of a mentorship program in Saskatchewan. Can Fam Physician 56(7):e263–e272
Toklu HZ, Fuller JC (2017) Mentor-mentee relationship: a win-win contract in graduate medical education. Cureus. 9(12):e1908
Sambunjak D, Straus SE, Marusić A (2006) Mentoring in academic medicine: a systematic review. JAMA 296(9):1103–1115
Cho CS, Ramanan RA, Feldman MD (2011) Defining the ideal qualities of mentorship: a qualitative analysis of the characteristics of outstanding mentors. Am J Med 124(5):453–458
Straus SE, Johnson MO, Marquez C, Feldman MD (2013) Characteristics of successful and failed mentoring relationships: a qualitative study across two academic health centers. Acad Med 88(1):82–89
Miller CJ, Wood GC, Miller JJ, Marks VJ (2006) Academics or private practice? The future of dermatologic surgery education. Dermatol Surg 32(1):70–75
Sciscione AC, Colmorgen GH, D’Alton ME (1998) Factors affecting fellowship satisfaction, thesis completion, and career direction among maternal-fetal medicine fellows. Obstet Gynecol 91:1023–1026
Wingard DL, Garman KA, Reznik V (2004) Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine. Acad Med 79(10 suppl):S9–S11
Illes J, Glover GH, Wexler L, Leung AN, Glazer GM (2000) A model for faculty mentoring in academic radiology. Acad Radiol 7:717–724 Erratum appears in Acad Radiol . 2000;7:959
Ramondetta LM, Bodurka DC, Tortolero-Luna G, Gordinier M, Wolf JK, Gershenson DM (2003) Mentorship and productivity among gynecologic oncology fellows. J Cancer Educ 18:15–19
Rivera JA, Levine RB, Wright SM (2005) Completing a scholarly project during residency training: perspectives of residents who have been successful. J Gen Intern Med 20:366–369
Holliday EB, Jagsi R, Thomas CR, Wilson LD, Fuller CD (2014) Standing on the shoulders of giants: results from the Radiation Oncology Academic Development and Mentorship Assessment Project (ROADMAP). Int J Radiat Oncol Biol Phys 88(1):18–24
Dhami G, Gao W, Gensheimer MF, Trister AD, Kane G, Zeng J (2016) Mentorship programs in radiation oncology residency training programs: a critical unmet need. Int J Radiat Oncol Biol Phys 94(1):27–30
Hirsch AE, Agarwal A, Rand AE, DeNunzio NJ, Patel KR, Truong MT, Russo GA, Kachnic LA (2015) Medical student mentorship in radiation oncology at a single academic institution: a 10-year analysis. Pract Radiat Oncol 5(3):e163–e168
Agarwal A, Shah A, Shah B, Koottappillil B, Hirsch AE (2017) The impact of a radiation oncologist led oncology curriculum on medical student knowledge. J Cancer Educ
Denunzio N, Parekh A, Hirsch AE (2010) Mentoring medical students in radiation oncology. J Am Coll Radiol 7(9):722–728
Aagaard EM, Hauer KE (2003) A cross-sectional descriptive study of mentoring relationships formed by medical students. J Gen Intern Med 18:298–302
Agarwal A, Denunzio NJ, Ahuja D, Hirsch AE (2014) Beyond the standard curriculum: a review of available opportunities for medical students to prepare for a career in radiation oncology. Int J Radiat Oncol Biol Phys 88:39–44
Golden DW, Raleigh DR, Chmura SJ, Koshy M, Howard AR (2013) Radiation oncology fourth-year medical student clerkships: a targeted needs assessment. Int J Radiat Oncol Biol Phys 85:296–297
Zaorsky NG, Malatesta TM, Showalter TN, den RB, Shi W, Anne PR, Werner-Wasik M, Dicker AP, Bar-Ad V (2013) Impact of a radiation oncology elective on the careers of young physicians: update on a prospective cohort study. Int J Radiat Oncol Biol Phys 86:214–215
Clayton R, Trotter T (2013) The impact of undergraduate education in radiation oncology. J Cancer Educ 28:192–196
Golden DW, Spektor A, Rudra S, Ranck MC, Krishnan MS, Jimenez RB, Viswanathan AN, Koshy M, Howard AR, Chmura SJ (2014) Radiation oncology medical student clerkship: implementation and evaluation of a bi-institutional pilot curriculum. Int J Radiat Oncol Biol Phys 88:45–50
Mattes MD, Small W, Vapiwala N (2018) Out of the basement and into the classroom: pathways for expanding the role of radiation oncologists in medical student education. J Am Coll Radiol 15:1620–1623
Neeley BC, Golden DW, Brower JV, Braunstein SE, Hirsch AE, Mattes MD (2017) Student perspectives on oncology curricula at United States medical schools. J Cancer Educ
Agarwal A, Shah A, Byler S, Hirsch AE (2017) Cultivating interest in oncology through a medical student oncology society. J Cancer Educ 32(1):31–34
Agarwal A, Koottappillil B, Shah B, Ahuja D, Hirsch AE (2015) Medical student--reported outcomes of a radiation oncologist--led preclinical course in oncology: a five-year analysis. Int J Radiat Oncol Biol Phys 92(4):735–739
National Resident Matching Program. Charting outcomes in the match for U.S. allopathic seniors. https://www.nrmp.org/wp-content/uploads/ 2016/09/Charting-Outcomes-US-Allopathic-Seniors-2016.pdf. Accessed April 19, 2018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
No disclaimers. There was no source of financial support for this research.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boyd, G.H., Rand, A.E., DeNunzio, N.J. et al. The Radiation Oncology Mentorship Initiative: Analysis of a Formal Mentoring Initiative for Medical Students Interested in Radiation Oncology. J Canc Educ 35, 893–896 (2020). https://doi.org/10.1007/s13187-019-01539-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-019-01539-w