Abstract
With a growing number of cancer survivors, survivorship care plans (SCPs) are recommended to communicate information about late effects of treatment and follow-up care. Community oncology practices follow 85% of adult cancer survivors but report more difficulty in providing SCPs compared to academic centers. Our objective was to evaluate the impact of delivering SCPs in a community oncology practice by examining awareness of SCP receipt as well as how provision affects survivors’ perception of care quality and of their condition. Survivors who accepted a SCP as standard of care were recruited from a community oncology practice in the Midwest and completed surveys prior to SCP provision (baseline) and 4 weeks later (follow-up). Within-survivor changes in knowledge of SCP receipt, satisfaction and perceived care coordination were assessed. Thirty cancer survivors (breast, colon, and prostate) completed the baseline survey, while 24 completed the follow-up survey (80% response rate). Participants reported receiving SCPs and treatment summaries more frequently at follow-up after receiving a SCP. At follow-up, there was a significant increase in survivor activation and involvement in care along with satisfaction of knowledge of care. Communication about and during SCP provision may need to be clearer: 34% of survivors could not correctly identify SCP receipt in this study. This may place these survivors at a disadvantage, if this leads to less awareness of important information regarding follow-up surveillance and management. Of those aware of SCP receipt, SCP provision had positive impacts in this small, short-term study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is one of the leading causes of death worldwide, comprising 8.2 of the 14 million new cases of deaths reported in 2012 [1]. However, the population of those living with cancer is also increasing: in 2016, the National Cancer Institute reported 15.5 million cancer survivors, indicating a great need for follow-up care to manage the late effects of treatment, risk of recurrence, and to provide long-term supportive care [2]. Care coordination plays an influential role in cancer survivorship, yet many cancer survivors report uncertainty regarding follow-up responsibilities such as sharing plans with their health care team, understanding necessary follow-up surveillance, and making changes in modifiable risk factors in support of resisting disease recurrence [3, 4]. Those who cannot identify a follow-up care provider are significantly less likely to report high-quality care than those who can [5]. Previous data indicate that breast cancer survivors who receive coordinated follow-up care by both specialists and primary care physicians received more routine, necessary non-cancer-related preventive services than those who are only followed by oncologists and are more likely to rate their care as high quality [5, 6]. On the other hand, extra resources may be consumed if care is redundant through duplicative procedures between oncologist and PCP, imposing unnecessary costs on the healthcare system [3, 7]. Lack of knowledge of long-term effects and recommended follow-up care may also result in decreased patient activation and participation in health care [3]. To address the increased risks after cancer treatment, survivors and/or their primary care providers (PCPs) must be well informed so that proper services can be used to alleviate these risks.
To address care coordination and knowledge, survivorship care plans (SCPs) are recommended for every cancer survivor (IOM) [2]. SCPs include guidelines for monitoring and improving a survivor’s health against late effects of cancer treatment and/or recurrence, information about diagnosis, treatment summary, lifestyle recommendations, and distinguishing between which providers to see for follow-up care [8]. SCPs are expected to increase care coordination by promoting survivor and clinician knowledge of the survivor’s diagnosis and treatment, and their awareness of the associated recommendations for follow-up. The Commission on Cancer accreditation guidelines mandate that 50% of cancer survivors receive SCPs with care planning visits by 2019. However, provision of SCPs and care planning visits to survivors has been limited due to communication barriers between oncologists and follow-up care providers, and insufficient time, staff, and other resources needed to create and use SCPs [9]. One potential strategy to improve provision includes leveraging the electronic health record (EHR) system to create, provide, and track SCPs [4, 10,11,12].
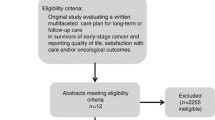
There has been a call for research to address adoption of survivorship care models within community-based practices [13]. SCP effectiveness has been studied largely in academic hospital and health system settings, limiting the generalizability of the intervention [13]. Community oncology practices report more difficulty in providing SCPs compared with academic centers, despite following 85% of adult cancer survivors [14]. Therefore, we conducted a pilot study seeking to address how SCP provision affects survivors’ perceived knowledge of care quality and of their condition in a community oncology practice. Our primary outcome is survivor awareness of SCP receipt, as prior research demonstrates that over half of survivors may not recall receiving a SCP and if survivors are unaware that they received a SCP, it becomes difficult to conclude that the SCP makes any further impact [11, 15]. Secondary outcomes in this study include changes in survivor satisfaction with knowledge, care coordination, communication post-SCP, and feedback regarding the SCP.
Methods
Study Design
The authors conducted a single-center intervention study at a community oncology practice in the Midwest. The study was approved by the institutional review boards at the author’s academic medical center and the community oncology practice (PHC).
Patient Population
PHC is a community cancer center affiliated with the author’s academic medical center and serves the southeastern part of Wisconsin. Breast, colon, and prostate cancer survivors are routinely offered an EHR-based SCP and care planning session as standard of care at this community practice; for example, in 2017, PHC treated 249 breast, 117 prostate, and 59 colorectal patients, with 207 (83%), 117 (100%), and 43 (73%) receiving SCPs respectively. Survivors eligible for participation in this study included all stage 0–3 breast cancer, and stage 1–3 prostate and colorectal cancer patients completing treatment at PHC. Eligible survivors due to receive an SCP as standard of care were approached until accrual was completed. Survivors who declined a SCP and/or visit, who received all cancer treatment elsewhere, or had metastatic cancer were not eligible.
Recruitment, SCP Creation, and Provision
Potential participants were approached during routine follow-up by research staff or members of the primary oncology care team regarding participation in this survey study. Informed consent was obtained from all eligible individuals, who were then enrolled. A member of the care team prepared an individualized SCP, generated by the EHR, for each participant. Each SCP included key elements about the survivor’s diagnosis, treatment summary, lifestyle recommendations, late effects of treatment, signs of recurrence, and distinguishing between which providers to see for follow-up procedures, imaging, and preventive care in accordance with the IOM’s recommendations [2]. Survivors met with an oncology nurse navigator at a care planning visit to receive and review the SCP, and discuss any follow-up concerns.
Data Collection
Data regarding demographics, cancer site and stage, and information about diagnosis and treatment were extracted from the medical record by research staff. At baseline, participants had not yet received a SCP or any treatment summaries. Participants were thus surveyed prior to SCP provision and 4 weeks after having received their SCP, to assess the short-term impact of providing a SCP in a community oncology practice. Participants completed the baseline survey in clinic upon enrollment and were contacted via email with a link to the 4-week follow-up online survey. Those without internet access were mailed a paper copy of the survey. Two email reminders were sent to participants to remind them to complete the follow-up survey; survivors without internet access were reminded at in-person clinic visits or via phone call. Those who completed the second survey were compensated with a $25 gift card.
Measures
For the primary outcome, the baseline survey included the question, “Have you received a Survivorship Care Plan document?” as well as two separate questions from the 2010 National Health Interview Survey (NHIS) used in a previous study to examine survivor receipt of treatment summaries. The baseline survey also included questions from the “Patient Assessment of Chronic Illness Care (PACIC)”, the Picker Institute Cancer Survey (PICS), the “Preparing for Life as a New Survivor (PLANS)” questionnaire, and questions regarding survivor satisfaction with knowledge and feedback on SCP receipt. Both PACIC and PICS are highly ranked by the National Cancer Institute’s Grid Enabled Measure (GEM) Care Planning Initiative for care planning research [16]. The PACIC evaluates care organization, and how involved and activated survivors are in their care [17]. Positive effects as assessed via the PACIC have been observed in cancer survivorship research [18]. Survivors indicate their perceived knowledge of who is responsible for their care, and quality of interactions with their clinicians via the Picker Cancer Care Survey [18, 19]. The PLANS survey assesses survivor-perceived understanding of illness diagnosis, treatment, side effects, and communication with care team and has been used in previous survivorship research [20, 21]. All baseline survey questions were repeated on the follow-up survey along with additional questions regarding SCP usability, usefulness, content, and access. The primary outcome of this study was awareness of SCP receipt, while secondary outcomes include the modified PACIC and PLANS summary scores, mean scores for individual PICS questions, a satisfaction of knowledge summary score, and feedback regarding SCP provision. Supplemental Material 1 includes a sample SCP and the questionnaires.
Analysis Plan
Analyses were performed in SAS 9.4. Descriptive statistics were generated for demographic information (age and race), clinical data (cancer site, stage, treatment), and survivor feedback regarding SCP content and provision. For pre- and post-descriptive statistics, p values were based on marginal homogeneity test for categorical variables and McNemar test for binary variables. Summary statistics for overall scales were computed as averages of the items within each, as responses for all summary scores were measured on a Likert-type scale. Higher scores indicated higher patient activation as evaluated by PACIC, higher perceived care coordination for the individual PICS items, and higher perceived knowledge of care for PLANS. A higher score also signified greater patient satisfaction of knowledge as assessed by site-specific questions. Within-survivor changes in satisfaction and perceived care coordination, as measured by mean survey scores, were assessed with Wilcoxon signed rank tests to calculate if the changes were significantly different from 0. To assess survivor-perceived usefulness of SCP content, we asked respondents why they looked at their SCP and what they liked most and what they would change about the SCP.
Results
Respondents
Thirty participants consented to the study and completed the baseline survey between September 2017 and April 2018, while 24 (80%) completed the 4-week follow-up survey. Table 1 displays the participant demographics and treatment characteristics at baseline and follow-up. There were no significant differences between baseline and follow-up participants. Only those who completed both surveys (baseline + follow-up) are included in the analyses.
Primary Outcome
As shown in Table 2, participants reported receiving SCPs and treatment summaries more frequently at follow-up. In contrast, using the NIHS question about recommendations and advice, the majority of participants (91.6%) reported receiving advice even at baseline.
Secondary Outcomes
All scale summary scores were based on Likert-scale responses (scores ranges from 1 to 5, Supplemental Material 1). Within-group overall mean scores were compared between baseline and 4-week follow-up, as well as intra-individual changes in score to examine magnitude (less than 0.5 point, between 0.5 to 1 point, and greater than 1 point) and directionality of change (Table 3). The average PACIC and PLANS scores significantly increased from baseline to 4-week follow-up (p = 0.001, p = 0.045), while no significant change was observed in the Satisfaction with Knowledge scores. In terms of effect size, most survivors had a positive change of greater than 1 point in PACIC and less than 0.5 point in PLANS summary scores from baseline to follow-up (33.3% and 29.5%). No significant differences were found for the mean score of each PICS question between baseline and 4-week follow-up (Supplemental Table 1). We also analyzed the data for those who correctly responded whether or not they received a SCP at baseline (“no”) and follow-up (“yes”), and saw no difference in results.
Feedback Regarding SCP Content and Provision
At 4-week follow-up, most survivors responded that the SCP contained information that was new to them (83%). All survivors reported having looked at the SCP at least once or twice. When asked to choose one member of the cancer team to review the SCP with, most respondents (58%) selected a cancer navigator, while 29% chose an oncologist. Regarding format of reviewing the SCP, 63% of survivors preferred reviewing it as part of a regular follow-up visit, while 29% chose a separate visit solely for reviewing the SCP. Two thirds of respondents found that a paper document at the end of the visit was most favorable, while 29% selected electronic format via the online patient portal. All survivors responded that they would like to receive their SCP either right after finishing treatment or a few months afterward rather than at later times.
Regarding what participants liked about their SCP, most responses conveyed the common theme of having all the information regarding diagnosis, treatment, and prognosis in one spot. Participants stated that it “takes the worry out of when do I have to go next [for breast imaging and follow-up],” and “it is nice to have all the information in one spot and clearly laid out.” Participants reported choosing to look at their SCP because they wanted “to know everything about my cancer treatment and my prognosis, and where to go to ask questions, and “to better understand everything.” A participant also noted “finding it comforting to be able to refer to it.” Another stated looking at the SCP because it contained a “more detailed description of [my] treatment, side effects, and maintenance.” Regarding what they liked most about the SCP, participants said that the SCP was “easy to read and make sense of,” it provided “an explanation of my cancer and the percentage chance it will recur,” and informed them “what follow-up is needed.” A participant also noted the “overall comprehensiveness” of the SCP. In terms of improvement, one respondent said they would have preferred the follow-up information contained in the SCP “as soon as each step in the treatment process is near completion so [I] can try to grasp what is next.”
Discussion
This intervention study examined survivor awareness of SCP receipt and SCP impact on perceived care quality. We demonstrated that at baseline, roughly 17% of patients incorrectly report receiving an SCP when they have not, while 17% continued to report not having received one even after it had been provided as part of a visit. Prior research reports even greater percentages of patients (53 and 66%) being unaware of SCP receipt [11, 15], which might be explained by greater awareness of receipt among our participants due to study consent. Survivors may not understand the content and purpose of SCPs, may not correctly identify the document as such, or may lose sight of the SCP as the primary document reviewed [15] if given with other paperwork.
The results of our research and prior studies highlight that communication during SCP provision may need to be clearer so that the survivor is well informed on receipt and content of the SCP in order to utilize it fully. It is important to distinguish the SCP from treatment summaries and other documents survivors receive at follow-up visits. Additionally, despite not having yet received SCPs or treatment summaries prior to baseline, 17% of participants reported having received a SCP, and 25% reported receiving a single document describing all their cancer treatments. This may be the result of survivors receiving informal written descriptions of treatment from other clinicians. Given that both the questions regarding SCP and treatment document provision trended in a positive direction at 4-week follow-up, receipt of a treatment summary may serve as good surrogate for assessing SCP receipt. On the other hand, most participants indicated that they had received advice from a provider about where to go for follow-up prior to SCP provision. This question seems unlikely to be a useful indicator of SCP receipt given the ceilinged response rate at baseline.
The increase in survivor activation and involvement in care along with perceived satisfaction of knowledge of care as evaluated by PACIC and PLANS was statistically significant at 4-week follow-up. In terms of clinical meaningfulness, more survivors demonstrated positive intra-individual changes in PACIC and PLANS summary scores than negative changes. Other investigators conducted similar studies in which they also self-selected questions from the PACIC, PICS, and PLANS and observed positive effects in survivor-perceived care quality, coordination, and knowledge of care [18, 20, 22, 23]. Because our findings could have been a result of the SCP document, the care planning visit reviewing the SCP, survivors’ knowledge of participating in a research survey, or a combination of these factors, more research is warranted to determine how SCPs and care planning visits impact these outcomes. Although statistically significant, it is unclear whether the results are clinically meaningful. The Satisfaction with Knowledge score did not significantly change at follow-up. This may be due to each survivor’s significant contact with oncology navigators, which could have increased their knowledge of their conditions and preventive behaviors at baseline. Conversely, survivors may be satisfied with knowledge despite lacking knowledge of important details [21].
Strengths of our study include the mix of cancer types, as previous studies tend to focus their observations on one cancer site, which may impact results depending on how prevalent a cancer is and subsequently how informed a patient may be [24]. Furthermore, other studies relied on research staff to determine receipt of SCPs, while our study utilized research staff, the oncology care team, and the medical record to verify receipt (yes/no) [18, 20]. This may explain why more of our participants were able to correctly identify SCP receipt compared to other studies [11, 15], although other possible explanations include shorter time frame of 4 weeks (vs. 6, 12, 24 months) or shorter time since diagnosis (within a year vs. over a year). As noted by previous investigators, few studies have focused on the patient experience and obtaining feedback related to patients’ views and use of the SCP [10, 25]. We therefore included numerous questions inquiring survivors for feedback regarding SCP provision, delivery, and receipt. Qualitative responses are extremely valuable in this aspect as they reveal insight that cannot be extrapolated from Likert-scale responses. Additionally, asking survivors if they were aware of SCP receipt and if they had looked at their SCP increases the likelihood that changes in survivor-reported outcomes may be related to SCP provision, enhancing validity of the data [15]. As indicated by a previous study, most research do not directly inquire survivors if they received an SCP and therefore data about treatment summaries and follow-up care may not reflect use of the SCP [24]. Lastly, our study is community-based, demonstrating the feasibility of delivering SCPs in a non-hospital setting and increasing the generalizability of the intervention.
Our research has several limitations. First, a small sample size of primarily Caucasian survivors makes it difficult to generalize findings to other populations as well as draw definitive conclusions about SCP impact on survivor-perceived outcomes. In order to enhance the generalizability of findings, this should be studied in a larger, more representative sample of community cancer center patients. Second, a modified version of previously validated surveys was used, with summary scores calculated based upon questions individually selected from each scale. Questions were selected for relevance with the study and to maintain clarity in the survey, as has been done by others in the survivorship context [18, 20, 21].
Despite limitations, our findings have implications for improving provision of clinically important information. As it is evident that not everyone who receives an SCP is aware that they have, providers should be explicit during follow-up visits about the information that survivors are receiving, and where they can go to access it so that they may utilize it optimally. To gain a better sense of where communication between provider and survivor is lacking, future research should delve into the reasons why not all survivors who receive SCPs are aware that they have. Because this has not been studied widely, future studies might begin by assessing this qualitatively to gather the most commonly cited reasons such that improvements can be focused on these areas. It is important that survivors recognize they are receiving information that they can employ to potentially reduce the burden of late treatment effects and manage routine follow-up surveillance and management.
References
Institute, National Cancer (2017) Cancer statistics. Accessed 2018
Medicine, Institute of, and National Research Council (2006) From cancer patient to cancer survivor: lost in transition. The National Academies Press, Washington, DC
Tremblay D, Latreille J, Bilodeau K, Samson A, Roy L, L’Italien MF, Mimeault C (2016) Improving the transition from oncology to primary care teams: a case for shared leadership. J Oncol Pract 12(11):1012–1019. https://doi.org/10.1200/JOP.2016.013771
Hill-Kayser CE, Vachani C, Hampshire MK, Jacobs LA, Metz JM (2009) An internet tool for creation of cancer survivorship care plans for survivors and health care providers: design, implementation, use and user satisfaction. J Med Internet Res 11(3):e39. https://doi.org/10.2196/jmir.1223
Weaver KE, Aziz NM, Arora NK, Forsythe LP, Hamilton AS, Oakley-Girvan I, Keel G, Bellizzi KM, Rowland JH (2014) Follow-up care experiences and perceived quality of care among long-term survivors of breast, prostate, colorectal, and gynecologic cancers. J Oncol Pract 10(4):e231–e239. https://doi.org/10.1200/jop.2013.001175
Earle CC, Burstein HJ, Winer EP, Weeks JC (2003) Quality of non–breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol 21(8):1447–1451. https://doi.org/10.1200/jco.2003.03.060
Tomasone JR, Brouwers MC, Vukmirovic M, Grunfeld E, O'Brien MA, Urquhart R, Walker M, Webster F, Fitch M (2016) Interventions to improve care coordination between primary healthcare and oncology care providers: a systematic review. ESMO Open 1(5):e000077. https://doi.org/10.1136/esmoopen-2016-000077
Society, American Cancer. 2018. Survivorship care plans. Accessed 2018.
Birken SA, Mayer DK, Weiner BJ (2013) Survivorship care plans: prevalence and barriers to use. J Cancer Educ 28(2):290–296
Brothers BM, Easley A, Salani R, Andersen BL (2013) Do survivorship care plans impact patients' evaluations of care? A randomized evaluation with gynecologic oncology patients. Gynecol Oncol 129(3):554–558. https://doi.org/10.1016/j.ygyno.2013.02.037
de Rooij BH, Ezendam NPM, Nicolaije KAH, Caroline Vos M, Pijnenborg JMA, Boll D, Boss EA, Hermans RHM, Engelhart KCM, Haartsen JE, Pijlman BM, van Loon-Baelemans IEAM, Mertens HJMM, Nolting WE, van Beek JJ, Roukema JA, Kruitwagen RFPM, van de Poll-Franse LV (2017) Effects of survivorship care plans on patient reported outcomes in ovarian cancer during 2-year follow-up - the ROGY care trial. Gynecol Oncol 145(2):319–328. https://doi.org/10.1016/j.ygyno.2017.02.041.
Tevaarwerk AJ, Wisinski KB, Buhr KA, Njiaju UO, Tun M, Donohue S, Sekhon N, Yen T, Wiegmann DA, Sesto ME (2014) Leveraging electronic health record systems to create and provide electronic cancer survivorship care plans: a pilot study. J Oncol Pract 10(3):e150–e159
Jacobsen PB, Derosa AP, Henderson TO, Mayer D, Moskowitz CS, Paskett ED, Rowland JH (2018) Impact of cancer survivorship care plans (SCPs) on health outcomes and health care delivery: a systematic review. J Clin Oncol 36(7_suppl):2–2. https://doi.org/10.1200/JCO.2018.36.7_suppl.2
Forsythe LP, Parry C, Alfano CM, Kent EE, Leach CR, Haggstrom DA, Ganz PA, Aziz N, Rowland JH (2013) Use of survivorship care plans in the United States: associations with survivorship care. J Natl Cancer Inst 105(20):1579–1587. https://doi.org/10.1093/jnci/djt258
Dietrich L, Smith AL, Watral A, Borgert AJ, Al-Hamadani M, Van Oosbree M, Meyer CM (2016) Effectiveness of a survivorship program: an assessment of patients with breast cancer in a community setting. J Oncol Pract 12(6):e688–e696. https://doi.org/10.1200/JOP.2015.010413
Parry C, Beckjord E, Moser RP, Vieux SN, Padgett LS, Hesse BW (2015) It takes a (virtual) village: crowdsourcing measurement consensus to advance survivorship care planning. Transl Behav Med 5(1):53–59
Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM (2005) Development and validation of the patient assessment of chronic illness care (PACIC). Med Care 43(5):436–444
Mayer DK, Deal AM, Crane JM, Chen RC, Asher GN, Hanson LC, Wheeler SB et al (2016) Using survivorship care plans to enhance communication and cancer care coordination: results of a pilot study. Oncol Nurs Forum 43(5):636–645. https://doi.org/10.1188/16.ONF.636-645.
Cleary PD, Edgman-Levitan S (1997) Health care quality. Incorporating consumer perspectives. JAMA 278(19):1608–1612
Maly RC, Liang L-J, Liu Y, Griggs JJ, Ganz PA (2017) Randomized controlled trial of survivorship care plans among low-income, predominantly Latina breast cancer survivors. J Clin Oncol 35(16):1814–1821. https://doi.org/10.1200/jco.2016.68.9497
Rocque GB, Wisinski KB, Buhr KA, Froeschner JL, Jones N, Donohue S, Wiegmann D, Sesto ME, Tevaarwerk AJ (2014) Development and evaluation of a survey to assess survivor knowledge change after survivorship care plans: WiSDOM-B (Wisconsin Survey of cancer DiagnOsis and Management in Breast cancer). J Cancer Educ 29(2):270–277. https://doi.org/10.1007/s13187-013-0591-9
Wagner EH, Ludman EJ, Bowles EJA, Penfold R, Reid RJ, Rutter CM, Chubak J, McCorkle R (2014) Nurse navigators in early cancer care: a randomized, controlled trial. J Clin Oncol 32(1):12–18. https://doi.org/10.1200/jco.2013.51.7359
Hershman DL, Greenlee H, Awad D, Kalinsky K, Maurer M, Kranwinkel G, Brafman L, Jayasena R, Tsai WY, Neugut AI, Crew KD (2013) Randomized controlled trial of a clinic-based survivorship intervention following adjuvant therapy in breast cancer survivors. Breast Cancer Res Treat 138(3):795–806. https://doi.org/10.1007/s10549-013-2486-1.
Sabatino SA, Thompson TD, Smith JL, Rowland JH, Forsythe LP, Pollack L, Hawkins NA (2013) Receipt of cancer treatment summaries and follow-up instructions among adult cancer survivors: results from a national survey. J Cancer Surviv 7(1):32–43. https://doi.org/10.1007/s11764-012-0242-x
Ayanian JZ, Zaslavsky AM, Guadagnoli E, Fuchs CS, Yost KJ, Creech CM, Cress RD, O'Connor LC, West DW, Wright WE (2005) Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol 23(27):6576–6586. https://doi.org/10.1200/jco.2005.06.102
Acknowledgments
The authors would like to thank the following: participating patients, providers, members of the UW Breast DOT (Renae Quale), and the Wisconsin Survivorship research Program (WiSP).
Funding
This work was supported by the NCI Cancer Center Support Grant P30 CA014520 and by grant UL1TR000427 to UW ICTR from NIH/NCATS. AJT received support from the Clinical and Translational Science Award (CTSA) program through the NIH National Center for Advancing Translational Sciences (NCATS), grants UL1TR000427 and KL2TR000428. The Summer Research Program was funded by institutional foundation award from the Herman and Gwen Shapiro Foundation. This work is supported in part by NIH/NCI P30CA014520, the University of Wisconsin Carbone Cancer Center Support Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the institutional review boards at the both the academic medical center and the community oncology practice (PHC).
Conflict of Interest
Hua, Alexandra—none
Sesto, Mary E—none
Tevaarwerk, Amye J—Epic Systems (family member)
Wassenaar, Timothy—none
Zhang, Xiao—none
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous Presentations
None.
Electronic supplementary material
Supplemental Material 1
Survivor surveys (PDF 524 kb)
Supplemental Table 1
PICS results (DOCX 75 kb)
Rights and permissions
About this article
Cite this article
Hua, A., Sesto, M.E., Zhang, X. et al. Impact of Survivorship Care Plans and Planning on Breast, Colon, and Prostate Cancer Survivors in a Community Oncology Practice. J Canc Educ 35, 249–255 (2020). https://doi.org/10.1007/s13187-018-1457-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-018-1457-y