Abstract
The aim of this study was to evaluate the knowledge and awareness levels of 18-year-old and older women and men on HPV infection, HPV vaccine, and the potential risk factors in Hatay, Turkey. In our study, it was found that overall 27.0 and 23.2% of the participants reported having heard of HPV infection and HPV vaccine. The rate of participants who had heard of HPV infection and HPV vaccine was higher in women than in men (p < 0.000). Thirteen percent of the participants was aware of the fact that HPV triggers cervical cancer, 10.2% penile cancer, and 16.7% genital warts, respectively. The overall vaccination rate of the participants was 2.7%. When the total knowledge score of the participants about HPV infection and HPV vaccine was evaluated according to independent variables, it was found that being a woman, urbanization, and having a high level of education had a positive effect on knowledge score, while never having heard of HPV infection and HPV vaccine had a negative effect on knowledge score (p < 0.000). It was determined in the linear regression model that gender, educational status, residential area, and having heard of HPV infection before influenced knowledge levels. It was determined that the relation between these variables and the total knowledge scores of the participants was statistically significant (p < 0.05). It was also determined that women who had higher educational levels, those who were living in urban areas, and those who had heard HPV infection before had higher knowledge levels. The level of knowledge of the participants about HPV infection and HPV vaccine was found to be very low. Having adequate knowledge about HPV infection and increasing the acceptance of HPV vaccination in public will play an important role in decreasing the rate of mortality and morbidity of the different HPV-associated cancers in women and men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human papillomavirus (HPV) is one of the most common sexually transmitted infections around the globe [1]. While about 80–90% of the infections are asymptomatic and transient and are eliminated within 2 years, persistent oncogenic (high-risk) infections have been linked to oropharyngeal, anal, cervical, vaginal, vulvar, and penile cancers [2].
The most important clinical consequence of HPV infection is cervical cancer. Centers for Disease Control and Prevention (CDC) reported that by age of 50, at least 4 out of every 5 women will have been infected with HPV at one time in their lives [1].
Cervical cancer, with the death of approximately 266,000 women each year worldwide, remains one of the leading causes of cancer-related mortality in women. Most cervical cancer-related mortality occurs in countries where there is no routine cervical screening. Conversely, developed countries have successfully reduced death from cervical cancer through effective screening programs [3].
Genital HPV infection is very common in men and infections may progress to external genital lesions, mostly condylomata acuminata and penile intraepithelial neoplasia which are considered to precede penile cancer [4]. Recent research reported high-risk HPV in 48% of penile cancers in men. A systematic review of worldwide HPV prevalence in men found a prevalence range between 1.3 and 72.9% [5].
In order to reduce morbidity and mortality rates related to HPV infection, primary protection measures are very important. These primary protections involve eliminating the sexual risk factors and application of prophylactic vaccines. It was reported that vaccines significantly reduce the influence of disease before sexual activities. There are two types of HPV vaccination: bivalent Vaccine (Cervarix) is effective for HPV-16 and -18, while quadrivalent vaccine (Gardasil) is effective for HPV-6, -11, -16, and -18. Both vaccines provide protection against cancer while Gardasil is additionally efficient against genital warts and is recommended for men [6].
Public health research suggests that awareness and knowledge of HPV are important for acceptance [2], because the burden of HPV-associated diseases is higher in women. Much of the research on HPV awareness and knowledge has focused primarily on women. A systematic review of 39 studies worldwide found women’s knowledge to be poor ranging between 15 and 31% [7]. However, male HPV infection is also important. HPV infections have the potential to cause various adverse health outcomes in males including genital warts and some types of cancer (anal, penile, and oral cancers). HPV concordance levels are high among sexual partners, so infected males also put their female partners at increased risk of cervical disease [8]. One study had demonstrated a five-fold increased risk of cervical cancer in women who had a male partner infected with penile HPV [9]. Studies of knowledge of HPV among males also have shown a low level of awareness of the existence of HPV including poor knowledge about HPV infection and mode of transmission. Another study reported that besides having poorer knowledge, young men were not aware that they could be the host for HPV, thereby affecting the female population or that they were at risk of some HPV-related cancers [7].
There have been several studies conducted to assess the awareness and the knowledge on HPV in Turkey; however, most of them focused on females, students studying at health sciences departments or healthcare professionals. Data on adult men’s awareness and knowledge are less common. Instructing people about HPV and HPV vaccines is significant in terms of applicability of HPV vaccination and protection against HPV infection and related diseases. We believe that assessing the awareness and knowledge of both male and female population about this concern is important to develop more effective health strategies and education.
In this study, we evaluated the awareness and knowledge on HPV infection and HPV vaccine in 18-year-old and older women and men adults, an important step in highlighting the knowledge gap that will become the focus of future vaccine uptake studies. Furthermore, the contribution of adults’ (18-year-old and older) socio-demographical characteristics to the level of knowledge was also explored.
Methods
This descriptive and cross-sectional study was carried out with 18-year-old and older women and men who referred to the Obstetrics and Gynecology Department of a private hospital in Hatay, Turkey.
The population aged 18 and over in Hatay Province was 707,387. The size of the sample was calculated as 980 people with 25% level of awareness and 3% deviation within 97% confidence interval (CI), which were reported in previous studies. Considering data losses, additional 10% was added to the sample size, and therefore, the target population was identified as 1078. The data were collected with questionnaires between August 19 and November 17, 2015. Participants who were not in acute distress, who were 18-year-old and older, and who provided oral and written consent to participate in the study were included. During the study period, a total of 1150 individuals were determined to be eligible to participate. Of these, 1097 individuals accepted the survey and 53 declined (95% participation rate). Of the 1097 surveys, 10 were excluded from analysis due to excessive missing data, and thus, a total of 1087 surveys were included in the analyses.
The data were collected using a self-administered descriptive questionnaire developed by the researchers. This questionnaire consisted of two parts: the first part consisted of “Participant Information Form,” and the second part included “HPV Knowledge Evaluation Test.” The Knowledge Evaluation Test was based on an extensive review of the literature. Content and validity of the Knowledge Evaluation Test were determined by five experts. The experts included two gynecologists, one urologist, one infectious diseases expert, and one oncologist. These professionals were selected based on their knowledge and experience regarding HPV-related cancers, HPV infection, and HPV vaccination. The Knowledge Evaluation Form was tested for appropriateness and understanding among 20 randomly chosen female and male adults, who were admitted in the same hospital, as a pre-implementation. No changes were made in the Knowledge Form following the pilot study. “Participant Information Form” contained 9 statements on the socio-demographic characteristics of the respondents such as age, education, and employment status as well as awareness about HPV infection and HPV vaccines and willingness for vaccination. “HPV Knowledge Evaluation Test” involved more detailed 10 statements about the HPV infection and vaccines. The participants’ responses were evaluated by scoring with 0 for “wrong” or “no-idea” and with 1 for “correct.” The total knowledge score was 10 points for a total of 10 statements. The reliability of statements regarding HPV infection and HPV vaccines in this sample was evaluated with the Cronbach α internal consistency coefficient. The Cronbach alpha coefficient was found to be 0.91.
Before beginning the data collection, each participant was verbally informed about the nature of the study and its objectives and was invited to participate. Participation was voluntary, and only individuals agreeing to participate completed the survey. All participants who provided oral consent to participate were asked to sign a consent form. The surveys contained no personal identifiers, and the completed surveys were collected by the researcher. The response time was estimated to be 15–20 min. In terms of ethical concerns, the study was approved by the Ethics Committee of the Medical School of Mustafa Kemal University (2015/80).
The data were analyzed using SPSS 15.0 software program. Descriptive statistics, frequency, percentage, mean, and standard deviation were used to evaluate the data. Comparative tests were performed using Chi-square, t test, and One-Way ANOVA. The knowledge level of the participants was considered as the depended variable, while other characteristics were considered as the independent variables. The relationship between the variables was assessed using the multivariate linear regression analysis. For all analyses, p < 0.05 was considered as the significance level.
Results
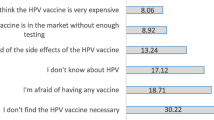
The mean age of the participants was 31.3 ± 7.9 years, 59.0% (n = 641) was women and 66.7% was married. The rate of the participants living in the city center was 57.3% (n = 623), and 38.5% (n = 419) had a university degree. It was found out that 27.0 and 23.2% of the participants reported having heard of HPV infection and HPV vaccine. The rate of knowledge about HPV infection and HPV vaccine was more in women (79.2 and 77.4%) compared to men (20.8 and 22.6%) (p < 0.000). The rate of risk perception of the participants for HPV infection was 6% (n = 65). The risk perception of women for HPV infection was much higher than that of males (p < 0.000). The vaccination rate of the participants was 2.7% (women = 25, men = 4). A total of 255 participants (23.5%) intended to have their children vaccinated. The rate of women who intended to have children vaccinated was higher than that of males (p < 0.03). The rate of the participants who recommended HPV vaccination to their family and close friends was 30.7% (n = 334). Compared to that of men, the rate of women who recommended HPV vaccination to their family and relatives was higher (p < 0.000).
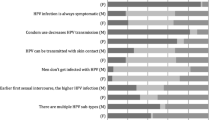
The correct comments on the statements about HPV infection and HPV vaccine are given in Table 1. Among the participants, the highest number of correct responses was given to the statements such as “the risk of HPV infection increases when numbers of sexual partner increase (31.1%),” “HPV is spread through sexual relationship (27.8%),” and “the risk of HPV infection decreases when a condom (preservative) is used during sexual intercourse (23.4%). The rate of correct responses to statements varied as follows; 20.3% of the participants correctly answered as “HPV is not only spread through women but also by men,” 16.7% of the participants knew that “HPV causes genital warts,” 14.4% knew that “HPV vaccine is not used only in girls,” 13.7% knew that “HPV vaccine can protect against cervical cancer and genital warts,” 13.0% knew that “HPV causes cervical cancer in women,” 10.2% knew that “HPV causes penile cancer in men,” and only 6.0% knew that “HPV vaccine can also be used on boys.” When the correct responses to statements about HPV infection and HPV vaccine were evaluated according to gender, it was determined that women gave more correct responses to statements. Except three statements on knowledge (penile cancers related to HPV, protective aspect of HPV vaccine, and to whom HPV vaccine is applied), there were statistically significant differences between the knowledge levels of men and women to other statements (p < 0.05). The average total knowledge score of the participants for HPV infection and HPV vaccine-related statements was 1.76 ± 2.52. A total of 178 (16.3%) participants had total knowledge score of 5 and above while only 8 (0.7%) had total knowledge score of 10.
When the total score of the participants about HPV infection and HPV vaccine was evaluated according to the independent variables, it was observed that knowledge scores were significantly affected by educational status, gender, place of residence, having heard of HPV infection and vaccine before, and risk of having HPV infection. Being a woman, urbanization, and having a high level of education had a positive effect on knowledge scores, while never having heard of HPV infection and HPV vaccine before had a negative effect on knowledge scores (p < 0.000), (Table 2).
With the multiple linear regression analysis, which was applied to purify the relation between the mean knowledge scores and some characteristics of the participants from the interaction between some independent variables, the aim was to determine the factors that were really influential. Since, in the correlation analysis, it was determined that the independent variables (having heard of HPV infection before, having heard of HPV vaccine before, and seeing oneself in the risk group in terms of HPV infection) were highly related with each other, these two independent variables were not included in the model. It was determined in the model that gender, educational status, residential area, and having heard of HPV infection before influenced knowledge level. It was determined that the relation between these variables and the total knowledge scores of the participants was statistically significant (p < 0.05). It was observed that women who had higher educational levels, who lived in urban areas, and who had heard HPV infection before had higher knowledge levels (Table 3).
Discussion
The Papanicolau (PAP) smear test is used as a secondary preventive measure against cervical cancer in women [10]. Today, however, it is virtually impossible to have prior knowledge by associating enhanced diagnostic tests to HPV-related cancers in men. In addition, HPV infection mostly does not indicate any symptoms and does not result in health problems in men [11].
The primary protection against HPV can be provided by prophylactic vaccination both in men and women [12]. It is expected that vaccination in women protects against HPV infection and decreases the necessity for the HPV scanning programs as well as the frequency of cervical cancer which requires costly medical treatments. It was reported that vaccinating men, who are known to have a high HPV transmission rate, would decrease the infection rate in turn decreasing the virus incidence in the general population. By such vaccination, anal, penile, and larynx cancers could be prevented [13].
HPV infection results in high-cost health problems in public [1]. Therefore, eliciting public awareness seems the most effective way to alleviate the economic and social encumbrance of HPV infection and related diseases. Lack of adequate knowledge is the main barrier for the prevention, diagnosis, and treatment of HPV infection and associated illnesses [10].
In the present study, the levels of knowledge and awareness of HPV infection and HPV vaccine were evaluated among 18-year-old and older women and men. There are several different studies about HPV awareness. However, awareness may vary depending on many environmental, social, educational, and economic factors. In Turkey, for example, HPV awareness rates were found to be 26.0 and 33.6% [14, 15] while in several other countries this rate ranged from 40.0 to 67.7% [16, 17]. It appears that variation existed not only within a particular region but also among regions. It was clearly shown that high awareness rates in developed countries were accompanied by high rates of public-based scanning and vaccination programs. In the present study, the rate of people with having heard of HPV infection was determined to be 27%, which is similar to the results of previous studies conducted in Turkey, and considerably lower than those of many developed countries. In the present study, 23.2% of the participants reported having heard of HPV. This rate ranged between 79 and 82% in some studies conducted in other countries [17, 18]. Previous studies in Turkey reported that having heard of HPV vaccine rates were 21.6, 24.0, and 25.1% [14, 15, 19]. Results of studies carried out in Turkey appear to be similar; however, compared to other countries, those rates are considerably low. It can be considered that reduced awareness rates of HPV infection also decrease the prior knowledge of HPV vaccine.
A study carried out in the USA reported that 39% of participants were aware of the relationship between cervical cancer and HPV, and 33.8% knew that HPV infection could cause genital warts [20]. A population-based study with 1106 people in Italy showed that the rate of participants who knew that HPV infection might cause cervical cancer was 46.6% and 58.5% of the participants knew HPV infection might cause penile cancer [21]. In our study, the rates of participants who were aware that HPV might cause cervical cancer, penile cancer, and genital warts were 13, 10.2, and 16.7%, respectively. It appears that our results are in corroboration with the results of other studies carried out in Turkey. However, compared to other developed countries, this rate is substantially low. Therefore, HPV-related infections and cancers should be the focus in public-based education.
Our results showed that only 27.8% of the participants were aware that “HPV is transmitted sexually.” In other countries, this rate was as high as 51.3 [21], 63.0 [16], and 86.0% [18], while in Turkey, it ranged between 10.8–21.0% [22, 23]. Our results seem to be higher than those of previous studies conducted in Turkey, while they are found to be lower than those of developed countries. The number of correct responses to the statements related to HPV infection and HPV vaccine was low probably due to inadequate education during adolescence period about safe sex and sexually transmitted diseases. Additionally, the rate of participants who were aware that women were not the only source transmitting the virus was 20.3%. The reason of the perception that the infection is transmitted only by females may be because cancer scanning programs mostly involve women. This wrong perception could be reversed if people are adequately informed about HPV infection during scanning treatments, thereby the infection could be controlled at a higher extent.
The results of our study indicated that a small portion of participants was aware that HPV vaccine could not only be used in girls (14.4%) but also in boys (6.0%). It was reported theoretically that vaccinating both genders is more effective compared to vaccinating only women [24]. Therefore, in educational programs, it should be indicated that HPV vaccination should be applied regardless of gender to get adequate protection against HPV infection. More research about the influence of vaccinating men should be carried out to confirm the effect of the protection.
In this study, the contribution of adults’ (18-year-old and older) socio-demographical characteristics to the level of knowledge was also investigated. It was determined that the relation between these variables and the total knowledge scores of the participants was statistically significant. It was found that being a woman, having higher education, living in urban areas, and having prior knowledge about HPV infection are the factors increasing knowledge level. Our results are in corroboration with those of the earlier studies.
In terms of knowledge about HPV infection and HPV vaccine, women are significantly different from men. Previous studies also indicated that women had higher knowledge levels compared to men [17, 21]. Being a woman seems to positively affect the knowledge level about HPV infection and HPV vaccine probably because women apply to health institutes about the reproduction-related issues more than men; they are more sensitive about health problems such as cervical cancers and have more interaction with healthcare staff during cervical cancer scanning programs. Our results suggest that more education involving HPV-related oral, penile, and anal cancers and their possible long-term results should be given to men who are known to be highly HPV transmitter.
As seen on most awareness level studies related to health, our study also showed that as the education level increased, knowledge levels on HPV infection and HPV vaccination also increased. Education level is also a significant factor influencing one’s perception about health issues as well as other issues in life. An educated person can reach information sources more easily and are expected to use them effectively. Similar to ours, most studies indicated that higher education level increased the knowledge level of people about HPV infection and vaccination [17, 20, 21].
Urban life provides more information sources and more interaction with others in the lives of people, and higher education is easier in urban areas. Therefore, urban life seems advantageous in terms of increasing knowledge level about health and other issues. Our study also indicated that urban people had higher knowledge levels compared to those in countryside. Li et al. [25] also reported that women in urban areas had more knowledge about HPV compared to those in countryside. Cates et al. [26] conducted a study on women in countryside and indicated that place of living influenced the knowledge level, and in more isolated areas, knowledge level of HPV vaccine was lower.
In conclusion, the study findings indicate that the level of knowledge regarding HPV infection and HPV vaccine in participants was remarkably low. Being a woman, having higher education, living in urban areas, and having prior knowledge about HPV infection are factors affecting the level of knowledge. There are some limitations in our study. The fact that our study was conducted only in the case group, i.e., the patients who were admitted to the outpatient clinic, is one of the limitations of our study. The study findings are not generalizable to our country. However, the study was conducted in a large sample size, and has many strong points. The study provided a better understanding on adults’ knowledge and awareness towards HPV infection and HPV vaccinations, and the findings indicate that education programs should be developed about these issues in order to prevent HPV-related cancers. Recently, there have been attempts to increase the knowledge level about HPV infection and vaccine in Turkey; however, knowledge level clearly seems much below the desired level. Therefore, there is an urgent need for personal and public education about the HPV. The incidence of HPV has been dramatically increasing, and the media sources should be quickly involved in informing people about the HPV and related diseases. Verbal and visual means and the Internet are also helpful sources to inform people about HPV infection and HPV vaccine. Men should also be involved in activities related to health issues. Correct and adequate knowledge about the HPV infection and HPV vaccine will increase the adoption of HPV vaccination; therefore, an important step could be taken to prevent cervical and penile cancer as well as other HPV-related diseases.
References
Centers for Disease Control and Prevention (2013) Basic information about HPV and cancer. https://www.cdc.gov/cancer/hpv/basic_info/index.htm. Accessed 18 Aug 2017
McBride KR, Singh S (2017) Predictors of adults’ knowledge and awareness of HPV, HPV-associated cancers, and the HPV vaccine: implications for health education. Health Educ Behav. https://doi.org/10.1177/1090198117709318
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2013) GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC Cancer Base No. 11[Internet]. Lyon, France: International Agency for Research on Cancer. https://www.iarc.fr/en/media-centre/pr/2013/pdfs/pr223_E.pdf. Accessed 19 Aug 2017
da Silva RJC, Sudenga SL, Sichero L, Baggio ML, Galan L, Cintra R, Torres BN, Stoler M, Giuliano AR, Villa LL (2017) HPV-related external genital lesions among men residing in Brazil. Braz J Infect Dis 21(4):376–385. https://doi.org/10.1016/j.bjid.2017.03.004
Tsikis S, Hoefer L, Bethimoutis G, Nicolaidou E, Paparizos V, Antoniou C, Chardalias L, Stavropoulos GE, Sharma S, Long BC, Mujacic I, Kadri S, Segal JP, Furtado LV, Schneider J, Charnot-Katsikas A (2017) Risk factors, prevalence, and site concordance of human papillomavirus in high-risk Greek men. Eur J Cancer Prev. https://doi.org/10.1097/CEJ.0000000000000366
Sahbaz A, Erol O (2014) HPV vaccination practice. J Turk Soc Obstet Gynecol 11(2):126–130. https://doi.org/10.4274/tjod.22230
Bebis H, Gulesen A, Ortabag T (2013) Knowledge and attitudes of Turkish young adult men regarding HPV and HPV related diseases. J Behav Health 2(1):52–58. https://doi.org/10.5455/jbh.20120930111151
Al-Naggar RA (2012) Acceptance and associated factors of HPV vaccination among young male Malaysians. J Community Med Health Educ 1:120. https://doi.org/10.4172/ scientificreports.120 https://www.omicsonline.org/scientific-reports/2161-0711-SR120.pdf. Accessed 19 Aug 2017
Bosch FX, Castellsagué X, Muñoz N, de Sanjosé S, Ghaffari AM, González LC, Gili M, Izarzugaza I, Viladiu P, Navarro C, Vergara A, Ascunce N, Guerrero E, Shah KV (1996) Male sexual behavior and human papillomavirus DNA: key risk factors for cervical cancer in Spain. J Natl Cancer Inst 88:1060–1067
Cetin O, Verit FF, Keskin S, Zebitay AG, Deregozu A, Usta T, Yucel O (2014) Knowledge levels of adolescent girls about human papilloma virus and its vaccine. Turk Pediatri Ars 49(2):142–147. https://doi.org/10.5152/tpa.2014.1545
Hernandez BY, Wilkens LR, Zhu X, McDuffie K, Thompson P, Shvetsov YB, Ning L, Goodman MT (2008) Circumcision and human papillomavirus infection in men: a site-specific comparison. J Infect Dis 197(6):787–794. https://doi.org/10.1086/528379
Yildirim M, Duzovali O, Kanik A, Kirik O (2009) Knowledge and attitudes of the pediatricians in Turkey regarding human papillomavirus (HPV) vaccine. J Pediatr Inf 3:62–68 http://www.cocukenfeksiyondergisi.org/upload/documents/200902/62-68.pdf Accessed 16 Sept 2017
Giuliano AR, Palefsky JM, Goldstone S, Moreira ED Jr, Penny ME, Aranda C, Vardas E, Moi H, Jessen H, Hillman R, Chang YH, Ferris D, Rouleau D, Bryan J, Marshall JB, Vuocolo S, Barr E, Radley D, Haupt RM, Guris D (2011) Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. N Engl J Med 364(5):401–411. https://doi.org/10.1056/NEJMoa0909537
Onan A, Ozkan S, Korucuoglu U, Aksal N, Taskıran C, Aygun R, Guner H (2009) Knowledge on and attitude towards human papillomavirus infection and its vaccine in a Turkish subpopulation. Turkiye Klinikleri. J Med Sci 29(3):594–598 https://www.scopus.com/record/display.uri?eid=2-s2.0-69949158530&origin=inward&txGid=f53cb0d7bf83f954ea32cfcfcc046d35. Accessed 16 Sept 2017
Tonguc E, Gungor T, Var T, Kavak E, Yucel M, Uzunlar O (2013) Knowledge about HPV, relation between HPV and cervix cancer and acceptance of HPV vaccine in women in eastern region of Turkey. J Gynecol Oncol 24(1):7–13. https://doi.org/10.3802/jgo.2013.24.1.7
Tiro JA, Meissner HI, Kobrin S, Chollette V (2007) What do women in the U.S. know about human papillomavirus and cervical cancer? Cancer Epidemiol Biomark Prev 16(2):288–294. https://doi.org/10.1158/1055-9965.EPI-06-0756
Blake KD, Ottenbacher AJ, Finney Rutten LJ, Grady MA, Kobrin SC, Jacobson RM, Hesse BW (2015) Predictors of human papillomavirus awareness and knowledge in 2013: gaps and opportunities for targeted communication strategies. Am J Prev Med 48(4):402–410. https://doi.org/10.1016/j.amepre.2014.10.024
Giles M, Garland S (2006) A study of women’s knowledge regarding human papillomavirus infection, cervical cancer and human papillomavirus vaccines. Aust N Z J Obstet Gynaecol 46(4):311–315. https://doi.org/10.1111/j.1479-828X.2006.00598.x
Reis N, Bebis H, Kose S, Sis A, Engin R, Yavan T (2012) Knowledge, behavior and beliefs related to cervical cancer and screening among Turkish women. Asian Pac J Cancer Prev 13(4):1463–1470
Holcomb B, Bailey JM, Crawford K, Ruffin MT (2004) Adults’ knowledge and behaviors related to human papillomavirus infection. J Am Board Fam Pract 17(1):26–31
Capogrosso P, Ventimiglia E, Matloob R, Colicchia M, Serino A, Castagna G, Clementi MC, La Croce G, Capitanio U, Gandaglia G, Damiano R, Mirone V, Montorsi F, Salonia A (2015) Awareness and knowledge of human papillomavirus-related diseases are still dramatically insufficient in the era of high-coverage vaccination programs. World J Urol 33(6):873–880. https://doi.org/10.1007/s00345-014-1379-1
Yanikkerem E, Piyan G, Kavlak T, Karadeniz G (2010) Assessing the role of education on Turkish university students’ knowledge about HPV and related diseases. Asian Pac J Cancer Prev 11(6):1703–1711
Bulbul S, Yalcin S, Araz NC, Turgut M, Ekici I, Doğan A, Yeltekin S (2013) Thoughts of mothers with children 0-15 years of age about cervical cancer and HPV vaccination in Anatolia. Turk J Pediatr Dis 2:73–78 http://tchdergisiorg/indexphp/tchd/article/viewFile/37/88. Accessed 16 Sept 2017
Onsuz MF, Topuzoglu A, Bilgi Z, Yılmaz M, Amuk N, Fahridin F (2011) The evaluation of the knowledge levels and attitudes of medical students who have accomplished obstetric and gynaecological diseases internship in a medical school about human papilloma virus vaccine. TAF Prev Med Bull 10(5):557–564. https://doi.org/10.5455/pmb.20110802053002
Li J, Li LK, Ma JF, Wei LH, Niyazi M, Li CQ, Xu AD, Wang JB, Liang H, Belinson J, Qiao YL (2009) Knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines among women living in metropolitan and rural regions of China. Vaccine 27(8):1210–1215. https://doi.org/10.1016/j.vaccine.2008.12.020
Cates JR, Brewer NT, Fazekas KI, Mitchell CE, Smith JS (2009) Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. J Rural Health 25(1):93–97. https://doi.org/10.1111/j.1748-0361.2009.00204.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Turhan, E., Cetin, S., Cetin, M. et al. Awareness and Knowledge Levels of 18-Year-Old and Older Individuals Regarding Human Papillomavirus (HPV) and HPV Vaccine in Hatay, Turkey. J Canc Educ 34, 234–241 (2019). https://doi.org/10.1007/s13187-017-1292-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-017-1292-6