Abstract
Colorectal and stomach cancers are the top ranking cancers in Oman. Most of the patients are diagnosed at advanced disease stages. The aim of this study is to explore the knowledge of risk factors, symptoms and the time needed to seek medical care for stomach cancer and colorectal cancer (CRC) among Omani participants attending 28 local health centres (LHCs) in the governorate of Muscat, the capital city of Oman. The Bowel Cancer/CRC Awareness Measure (CAM) questionnaire (translated into Arabic) was used to collect data from Omani adult participants (aged 18 years and above) who attended the LHCs during the study period. There was a total of 405 participants in the study out of the 500 who were invited (response rate = 81%). The most recognised risk factors were excessive drinking of alcohol (73.1%) and smoking (70.6%); the least recognised were doing less exercise (37.3%), eating food which was high in salt (26.8%) and a diagnosis of diabetes mellitus (24.9%). Multinomial logistic regression showed that young participants recognised more risk factors than older participants; highly educated participants recognised more risk factors than the less-educated and married participants recognised more risk factors than single participants. Participants with a high level of education were more likely to identify signs and symptoms of stomach cancer and CRC than less-educated participants. Multinomial logistic regression showed women were more likely than men to report barriers to seeking medical help (fear, difficulty in arranging transport, worried what the doctor might find). Also, participants with less education were more likely to report barriers than the highly educated (worried about wasting the doctor’s time, difficulty in arranging transport, did not feel confident talking about symptoms, embarrassed, scared, worried what doctor might find). The majority of participants (93.6%) were not aware of any CRC screening programme or had undergone any screening (98.3) for CRC. Only 52.6% of participants would have a colonoscopy if the doctors advised; the main reasons for refusal were embarrassment (40.0%), lack of trust in the doctors (33.3%) and religious or culture beliefs (21.3%). Around 39% of participants would prefer to have their colonoscopy examination abroad. There is an urgent need to increase the public’s awareness of stomach cancer and CRC in Oman, particularly with evidence emerging of an increase in the incidence. School curriculums could include sessions on cancer education and the information be reiterated to students periodically. A strategy to establish a CRC screening programme in Oman might be paramount as the incidence of CRC increased.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2015, the World Health Organisation (WHO) ranked colorectal cancer (CRC) and stomach cancer as the third and fourth, respectively, highest causes of death due to cancer after lung and liver cancers [1]. The overall incidence rates of CRC have increased in economically transitioning countries, particularly among men, compared to developed countries [2]. In the USA, CRC ranks as the third highest, after prostate and lung cancers, for newly diagnosed cases of cancer in men and for women it is the third behind breast cancer and lung cancer [3]. Among the countries of the Gulf Cooperation Council (GCC), including Oman, stomach cancer and CRC are among the most commonly diagnosed types of cancer, with approximately 60% of CRC patients and 49% of stomach cancer patients presenting in the advanced stages of the disease at the time of diagnosis [4].
Poor public awareness has been considered as the predominant reason for the delay in presentation with early cancer symptoms, ultimately leading to a poor cancer survival rate [5]. It has been found that poor public knowledge of early cancer symptoms and negative beliefs, such as “scared about what the doctor might find” and “worried about wasting the doctor’s time”, delays individuals in seeking medical help, particularly if the symptoms are atypical in nature [6]. Furthermore, sometimes members of the public misinterpret stomach cancer and CRC symptoms to non-medical causes or they may present to their doctors with non-specific symptoms such as abdominal pain, tiredness and rectal bleeding which could further delay their diagnosis [7].
Even with obvious symptoms, such as rectal bleeding, which is considered an alarming symptom, patients still seldom report these to the doctor as they assume that these symptoms are benign and do not require immediate attention [8]. Furthermore, the symptoms of stomach cancer and CRC are largely non-specific and doctors face considerable challenges when determining which symptoms warrant urgent attention, referrals and investigations [9].
The time taken in seeking medical help was found to be shorter in patients who perceived their first symptoms as serious and disclosed them to the doctors [10, 11]. Thus, it has been found that raising public awareness of the warning symptoms of cancer and encouraging them for prompt presentation could reduce patient attributable delay in the diagnosis and decrease the mortality [12, 13]. There is currently no screening programme for stomach cancer, however, the U.S. Preventive Services Task Force (USPSTF) recommends screening for CRC using faecal occult blood testing, sigmoidoscopy or a colonoscopy in adult patients, beginning at the age of 50 years and continuing until the age of 75 [14].
Oman is a developing country located at the south-eastern tip of the Arabian Peninsula and is administratively divided into four governorates and seven regions. In 2010, the national census recorded a total population of 2.7 million, of which 1.9 million were Omani [15]. Approximately 35% of Omanis were found to be below 15 years in age and only 3.5% were above 65 years old (median age 22 years). Also, approximately 21% of the total population of Omanis were found to reside in the capital city, Muscat, making it the most populated city in the country [15].
In Oman, cancer is the second highest cause of death and the third highest cause of loss of disability-adjusted life years (DALYs) [16]. Data from the National Cancer Registry (NCR) shows that the total number of cancer cases registered in Oman in 2013 was 1361. Of these, 1242 (91.2%) were among Omanis, 100 (7.4%) were non-Omanis and 19 (1.4%) were cases of carcinoma in situ [17]. The overall median age at time of cancer diagnosis for both male and female was 54 years old. However, this was higher in men (median age 60 years) compared to women (median age 50 years). In 2013, the crude incidence rates for all cancer cases among Omanis were 54.6 per 100,000 for men and 59.9 per 100,000 for women. The age standardised rate, adjusted to the world standard population, was 88.8 per 100,000 for males and 87.3 per 100,000 for females [17].
CRC is ranked as the most prevalent type of cancer diagnosed in men and second in women (after breast cancer) in 2012 [17]. The incidence of CRC has increased dramatically over the past 15 years. There were 109 patients diagnosed with CRC in Oman in 2013 [17]. Also, Oman has the highest incidence of stomach cancer among men and women compared to other GCC countries [18, 19]. Data from the NCR indicated that the total number of stomach cancer cases was the second highest in men (after CRC) and third in women (after breast cancer and CRC) in 2013. A total of 80 patients were diagnosed with stomach cancer in Oman in 2013 [17].
A recent study conducted in Oman showed that the majority of patients with CRC tend to present in the advanced stages of the disease (stage III and stage IV) and at a younger age (below the age of 40 years). Furthermore, there are no national screening programmes for CRC in Oman [19]. To the best of our knowledge, there are no previous studies conducted in Oman which have focused on exploring public knowledge of risk factors, symptoms and the time needed to seek medical help for stomach cancer and CRC.
Methods
Tool Used to Measure Stomach and CRC Awareness
The Bowel Cancer/CRC Awareness Measure (CAM) questionnaire is a validated standardised questionnaire developed by the University College London and Cancer Research UK to measure CRC awareness in the general population [20]. The questionnaire includes several items that measure the awareness of CRC risk factors. The questionnaire also includes common warning signs of CRC symptoms, anticipated time before seeking medical help and the perceived barriers to presentation. The perceived barriers to seeking medical help were further categorised into emotional, practical and services barriers [20]. Two additional risk factors for stomach cancer, such as infection with H-pylori and family history of stomach cancer, were added to the Bowel Cancer/CRC questionnaire.
The Bowel CAM has been found to meet the accepted psychometric criteria for reliability and construct validity. The internal reliability and test-retest reliability of the Bowel CAM were found to be high (Cronbach’s α = 0.84, test-retest reliability r = 0.70) [21]. The author of the Bowel CAM was contacted and the permission to use the questionnaire in our study was obtained. The questionnaire was translated from English to Arabic and back-translated into English by several people proficient in both languages.
Before embarking on data collection, a pilot study was conducted on the first 50 respondents to assess the reliability of the Arabic version of the questionnaire. Based on the standardised items, the Cronbach’s alpha of the questionnaire from the pilot study for overall Bowel and stomach CAM was 0.84 (risk factors cancer = 0.84, signs and symptoms = 0.87, barriers to seek medical help = 0.81) which shows as high a reliability as the original questionnaire.
Sample Size Calculation
A previous study conducted in the Omani community investigating the public’s awareness of warning signs and symptoms of cancer showed that the average cancer awareness among the respondents was 40.6% for all nine items of the CAM [22]. Based on the above literature on cancer awareness, a precision of 5% and taking into consideration a 5% alpha error, it was calculated that the minimum subjects needed for this study was 382. However, as this study is survey-based, so as to overcome missing data and non-respondents, we decided to distribute 500 questionnaires.
Recruitments of Participants
Local health centres (LHCs) are the main entry point for healthcare services in Oman. There are 28 LHCs in the governorate of Muscat, the capital city of Oman, providing primary healthcare services to people in specified catchment areas. Muscat can be regarded as a good representative of the Omani population, as its residents come from all over Oman. In order to cover the whole of Muscat, we have included all LHCs in our study and the subjects were recruited by obtaining systematic random sampling technique according to the adult population in each LHC catchment area.
Letters requesting the involvement of the LHCs were sent to the medical officers in charge. The co-authors (AJ, AT, AM) were trained to distribute and collect the questionnaires from the study participants. All adult patients and their attendees (age ≥ 18 years) attending the LHCs during the study period were invited to participate in the study. The aims of the study were explained to the participants by the co-authors. Participants who agreed to take part in the study and who could read and write were asked to sign a consent form and complete the questionnaire while waiting to see the doctor. The participants were also assured of the confidentiality of the collected data. Very sick patients, emergency cases and illiterate participants were excluded. The study was conducted between 15th December 2015 and 17th January 2016.
Statistical Methods
Data were analysed using the Statistical Package for the Social Sciences (SPSS), version 22 (IBM Corp, Chicago, Illinois). Descriptive statistics of the participants’ socio-demographics and a score for the recognition of risk factors, symptoms and reported barriers for stomach cancer and CRC were calculated. The chi-square test was used to find associations between the demographic factors and risk factors and symptoms and reported barriers nominal variables. Multinomial logistic regression analysis was carried out to adjust the factors.
Results
A total of 405 individuals participated in the study out of the 500 who were invited (response rate = 81%). There were 169 (41.7%) male participants and 236 (58.3%) female participants. Their ages ranged from 18 to 60 years old. The overall mean age of participants was 34.6 ± 5.1 years. The majority of participants (71.8%) were married and nearly half had completed university and postgraduate education (47.9%). A small subset of the participants (20.5%) had a family history of cancer (Table 1).
Recognition of Stomach Cancer and CRC Risk Factors
Overall recognition of risk factors by the participants for stomach cancer and CRC varied from 24.9–73.1%. The most recognised risk factors were excessive drinking of alcohol (73.1%), followed by smoking (70.6%), eating preservative products (62.4%), obesity (47.8%), a Helicobacter pylori infection (42.6%), eating food low in fibre (38.7%), doing less exercise (37.3%), a family history of stomach cancer or CRC (32.7%), eating food high in salt (26.8%) and having diabetes mellitus (24.9%) (Fig. 1).
In the multinomial logistic regression model, age group, level of education and marital status were significantly associated with the recognition of risk factors for stomach cancer and CRC. The younger age groups were more likely than the older groups to recognise that a high intake of salty food is a risk factor (OR = 2.80, 95% CI 1.12–6.99) (Table 2).
Participants with a high level of education (university and postgraduate) were more likely than literate to recognise the following as risk factors for stomach cancer and CRC: “having a family history of cancer” (OR = 4.0; CI 1.90–8.44), “smoking” (OR = 5.80; 95% CI 2.68–12.56), “excessive drinking of alcohol” (OR = 7.94, 95% CI 3.50–18.06), “eating food high in salt” (OR = 3.03; 95% CI 1.30–7.05), “eating food with low fibre” (OR = 3.33; 95% CI 1.50–7.41), “eating food with more preservative products” (OR = 9.22; 95% CI 3.12–27.26), “infection with H. pylori” (OR = 10.81; 95% CI 3.64–32.17) and “obesity” (OR = 4.17; 95% CI 1.96–8.88) (Table 2).
Also, participants with a school education were more likely than the literate participants to recognise the following as risk factors for stomach cancer and CRC: “smoking” (OR = 2.18; 95% CI 1.05–4.49), “excessive drinking of alcohol” (OR = 2.58, 95% CI 1.23–5.39), “eating food high in salt” (OR = 2.49; 95% CI 1.03–6.04) and obesity: (OR = 1.01; 95% CI 1.01–4.53) (Table 2).
Married participants recognised more than single participants the following as risk factors for stomach cancer and CRC: “having a family history of cancer" (OR = 0.51; 95% CI 0.27–0.97) and “infection with H. pylori” (OR = 0.29; 95% CI 0.12–0.72) (Table 2).
Recognition of Stomach Cancer and CRC Symptoms
The recognition of signs and symptoms of stomach cancer and CRC varies from 33.8–55.1%. The level of recognition is high with symptoms of “pallor and fatigability” (55.1%) followed by “blood in the stool” (53.2%), “blood in the vomit” (50.0%), “nausea and vomiting” (48.3%), “unexplained weight loss” (48.0), “alternative diarrhoea and constipation” (42.0%), “frequent bloating and flatulence” (36.8%) and “early satiety and abdominal fullness” (33.8%) (Fig. 2).
In the multinomial logistic regression model, gender and education level were significantly associated with the recognition of stomach cancer and CRC symptoms (see Table 3). Men were more likely to identify the symptom of “frequent bloating and flatulence” compared to women (OR = 2.54; 95% CI 1.21–5.34) (Table 3).
Participants with a high level of education (university and postgraduate) were more likely than the literate participants to identify the following as risk factors for stomach cancer and CRC: “unexplained nausea and vomiting” (OR = 5.41; 95% CI 2.02–14.51), “blood in stool” (OR = 9.62; 95% CI 3.26–28.27), “blood in the vomit” (OR = 6.96; 95% CI 2.63–18.41), “early satiety and abdominal fullness” (OR = 3.71, 95% CI 1.57–8.74), “alternative diarrhoea and constipation” (OR = 4.77; 95% CI 1.93–11.78), “frequent bloating and flatulence” (OR = 2.69; 95% CI 1.14–6.36), “unexplained weight loss” (OR = 4.55; 95% CI 1.95–10.66) and “pallor and fatigability” (OR = 7.19; 95% CI 2.78–18.58) (Table 3).
Also, participants with a school education were more likely than the literate participants to recognise the following as risk factors for stomach cancer and CRC: “blood in the vomit” (OR = 3.42; 95% CI 1.29–9.01), “unexplained weight loss” (OR = 2.61; 95% CI 1.08–6.32) and “pallor and fatigability” (OR = 3.03; 95% CI 1.18–7.79) (Table 3).
Perceived Barriers to Seeking Medical Help for Stomach and CRC
Most participants would seek medical help within the first week after noticing a possible cancer symptom, such as blood in the vomit (n = 387, 97.7%), blood in the stool (n = 380, 96.0%), unexplained nausea or vomiting (n = 368, 94.1%), alternative diarrhoea and constipation (n = 303, 81.0%), pallor and fatigue (n = 294, 75.2%), early satiety and abdominal fullness (n = 280, 73.9%), frequent bloating and flatulence (n = 266, 71.7%) and unexplained weight loss (n = 230, 62.8%).
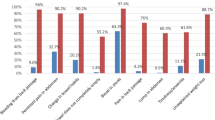
Participants reported several barriers to seeking medical help for possible stomach cancer and CRC symptoms including: “busy/don’t have time to go to the doctor” (57.3%), “worried what the doctor might find” (56.2%), “many other things to worry about” (50.6%), “scared” (46.5%), “difficult to make an appointment” (43.2%), “embarrassed” (33.2%), “difficulty talking to the doctor” (28%), “would not feel confident talking about symptoms” (27.9%), “difficulty in arranging transport” (22.3%) and “worried about wasting the doctor’s time” (16.6%) (Fig. 3).
A multinomial logistic regression model showed that the barriers to seeking medical help were significantly associated with gender, age and the education level of the participants. Women were more likely than men to report the following barriers to seeking medical help: “scared” (OR = 0.40; 95% CI 0.26–0.63), “difficulty in arranging transport” (OR = 0.36; 95% CI 0.20–0.64) and “worried what the doctor might find” (OR = 0.53; 95% CI 0.34–0.83) (Table 4).
Older participants reported more barriers to seeking medical help compared to the younger participants because of “difficulty in making an appointment” (OR = 0.41; 95% CI 0.22–0.78) Also, older participants reported more barriers to seeking medical help because of “difficulty in making an appointment” compared to the middle age participants (OR = 0.41; 95% CI 0.22–0.78). They also reported higher levels of the “difficult to talk” barrier compared to the middle-aged participants (OR = 0.49, 95% CI 0.26–0.93). On the other hand, young participants reported more barriers than older participants for: “many other things to worry about” (OR = 1.91; 95% CI 1.01–3.62) and “difficulty in arranging transport” (OR = 2.32; 95% CI 1.06–5.06) (Table 4).
Participants with no formal education were more likely than university educated and postgraduate participants to perceive the following as barriers to seek medical help: “worried about wasting the doctor’s time” (OR = 2.52; 95% CI 1.17–5.43), “difficult to talk” (OR = 2.29; 95% CI 1.2–4.30), “difficulty in arranging transport” (OR = 2.44; 95% CI 1.25–4.77) and “would not feel confident talking about symptoms” (OR = 2.07; 95% CI 1.12–3.81). Also, participants with school education were more likely than university educated and postgraduate participants to perceive the following as barriers to seeking medical help: “embarrassed” (OR = 1.76; 95% CI 1.07–2.92), “scared” (OR = 1.84; 95% CI 1.12–3.01), “worried about wasting the doctor time” (OR = 2.96; 95% CI 1.54–5.71), “difficult to talk about” (OR = 2.43; 95% CI 1.41–4.17), “difficulty in arranging transport” (OR = 1.86; 95% CI 1.02–3.39, “worried what the doctor might find” (OR = 2.03; 95% CI 1.22–3.37) and “would not feel confident talking about symptoms” (OR = 1.85; 95% CI 1.08–3.16) (Table 4).
Recognition for CRC Screening
The majority of participants (70.6%) had not heard about the CRC screening, were not aware about any methods for CRC screening (93.6%) or had undergone any CRC screening (98.8%). Only 52.6% of participants would have a colonoscopy examination if the doctor advised them due to suspicion of a CRC diagnosis. Of those who were not in favour of having a colonoscopy examination, the reasons given were feelings of embarrassment (40.0%), lack of trust in the doctors carrying out the procedure (33.3%) or due to religious and culture beliefs (21.3%). Approximately, 39% of participants would prefer to have a colonoscopy examination abroad (Table 5).
Discussion
To the best of our knowledge, there are no previous studies conducted in Oman which have focused on measuring the public’s knowledge and awareness levels of stomach cancer and CRC, concentrating on the risk factors, symptoms and barriers to seeking medical help and the perceptions of CRC screening. Most participants recognised that excessive drinking of alcohol and smoking are risks for stomach cancer and CRC, however, less recognised that a healthy lifestyle (eating a high fibre diet, eating food which is low in salt, taking part in physical activities), having a family history of cancer or a diabetes mellitus diagnosis could be also risk factors. In Arabic countries including Oman, the behavioural risk factors for cancer, such as unhealthy diets, lack of physical activity and obesity, are prevalent and have reached an alarming level, but the policy to respond to this increase has been ineffective for several years [23]. Thus, many people in Oman and other GCC countries might still be unaware of the CRC risk factors, which could contribute to the increased incidence level [4, 17].
The overall recognition level of common possible symptoms of stomach cancer and CRC was below 56%, indicating a general lack of public knowledge and awareness. A previous study conducted in Oman also showed that the public’s awareness of symptoms for the most common type of cancer was less than 50%.6 Furthermore, other similar studies conducted in developed countries have shown similar findings [24, 25]. A better level of recognition and knowledge of cancer symptoms will promote seeking medical help early and reduce the cancer delay and the mortality rate [13]. The finding that many patients in Oman and in GCC countries presented in the advanced stages of CRC (stage III and stage IV) at the time of diagnosis might be related to poor knowledge of the symptoms, leading to a delay in seeking early medical help [4, 19]. Though it should be noted that the delays in cancer diagnosis may occur throughout the different levels of the healthcare system (patient, doctor, the system itself), poor levels of awareness of early cancer symptoms has been considered the predominant reason for these delays in diagnosis [26].
The young participants and participants with a high level of education in this study were more likely than the older participants and participants with less education to recognise the risk factors and symptoms of stomach cancer and CRC. A previous study conducted in Oman to measure general awareness of common cancer signs and symptoms showed similar findings [6]. Also, another study conducted in the UK showed that the awareness levels of a poor lifestyle as risk factor for CRC was lower in participants less than 50 years old and in participants with a low level of education [27]. Indeed, the mortality rates from CRC have been found to decrease with the increasing years spent in education [28]. Individuals with a high level of education are more likely to adopt a healthy lifestyle and to engage in physical activity, eat a healthy diet, use hormone replacement therapy and participate in CRC screening than those with less education [29].
The finding in this study that married participants, compared to single participants, recognised more risks factors for stomach cancer and CRC such as “having a family history of cancer” and “infection with H. pylori” might be due to the fact that married participants are usually older and have more years of education. A previous study conducted in the UK showed that knowledge of cancer risks factors was low among individuals who are male, young, from a lower socio-economic status group and from ethnic minority groups [24].
Most of the participants in this study would seek medical advice within the first week of noticing possible symptoms of stomach cancer or CRC, however, women were more likely than men to report more barriers to seeking medical help, particularly “scared”, “difficulty in arranging transport” and “worried about what the doctor might find”. A recent study conducted in the USA showed that American-Muslim women reported delays in care-seeking due to a perceived lack of female clinicians, particularly if they had higher levels of modesty and self-rated religiousness [30]. Indeed, in Oman these delays may be due to similar reasons.
A previous study conducted among Omani women diagnosed with breast cancer showed that many of them encountered cultural barriers in seeking medical help or accessing specialised units [31]. Some Omani women travel overseas for their diagnosis to seek other treatment modalities and avoid the “cancer stigma”, all of which could delay the diagnosis of cancer [31].
Women usually fear a cancer diagnosis because the diseases is serious, involves painful symptoms, can be fatal/incurable and the potential loss of sexual characteristics when treatments (surgical, chemotherapy) start [32]. The issue of “difficulty in arranging transport” by women in this study might be because women usually prioritise work and family over their own health [33, 34]. Women in Oman may have less access to transport than men, despite the fact that many of them can drive cars.
Participants older than 40 years old reported “difficulty in booking an appointment” and “difficult to talk about” more frequently as barriers when seeking medical help. Data from Oman showed that CRC is one of the commonest malignancies and the majority of patients had stage III and IV at the time of presentation [17]. The median overall survival rate of patients is 43 months, which could indicate a delay in the cancer diagnosis due to several reasons, including difficulty in accessing healthcare systems to seek timely medical help [26, 35]. Having such barriers to obtaining an early appointment might delay the diagnosis and worsen the outcomes.
Participants who are less than 30 years of age in this study reported more barriers to seeking early medical help, including “many other things to worry about” and “difficulty in arranging transport” compared to older participants. The rates of cancer incidence has increased by 1.1% per year among men and women aged younger than 50 years and declined by 3.9% per year among adults aged 50 years and above [36]. As discussed previously, CRC in the young population appears to be more aggressive, present at a later stage and have poorer pathologic findings [37]. In Oman, the majority of the population are less than 50 years old (mean age in this study = 34.6 ± 5.1 years) which might possibly explain the high incidence of CRC and the late stage at the time of presentation [15].
Participants with no formal education or with less education (e.g. school) were more likely than university and postgraduate participants to perceive barriers to seeking medical help due to: “worried about wasting the doctor’s time”, “difficult to talk about”, “difficulty in arranging transport”, “would not feel confident talking about symptoms”, “embarrassed”, “scared”, “worried what the doctor might find” and “would not feel confident talking about symptoms”. Low cancer awareness was associated with poor cancer survival and specific barriers, such as embarrassment and difficulties in arranging transport to the clinic, were associated with lower cancer survival rates [5].
As mentioned earlier, education is linked to the knowledge of symptoms of cancer and, ultimately, for the correct help-seeking response [38]. The higher the level of education of an individual the more likely they will recognise a specific symptom as serious and engage in prompt help-seeking behaviour [39]. On the other hand, if the individual’s knowledge of cancer symptoms is low, their attitudes to cancer are more negative with lower intention levels in seeking prompt medical help or even participating in cancer screening [40].
The majority of participants in this study did know about or had undergone any CRC screening which is an expected finding as there is no official national screening programme for CRC in Oman. However, in 2012, it was reported that CRC was the most prevalent cancer affecting Omani men and the second highest affecting Omani women after breast cancer. There is no reason a national screening for CRC could not be implemented in Oman. Nevertheless, the cost-effectiveness of a screening programme could be compared to no screening to analyse if a test would entice a previously unscreened segment of the population to adhere to screening [41]. The public may worry that the instruments used in the screening could cause pain, discomfort, injury or be perceived as embarrassing and unpleasant [41, 42].
Only 52.6% of the participants in this study would have a colonoscopy examination if the doctor recommended it following a suspicion of a CRC diagnosis, as many felt embarrassed at the thought of the examination, some reported a lack of trust in the performing doctor and a few would not do it because of religious and culture beliefs. Previous studies conducted in the USA showed that unscreened subjects undergoing a colonoscopy cited lack of trust in doctors and the most common barrier to screening was fear of embarrassment during the screening, fear of finding cancer and fear that the exam might be painful [43]. Also, a study conducted among Palestinian adults showed that a decreased rate of acceptance of CRC screening was due to religious objection and perceived the test as embarrassing [44]. Indeed, approximately 39% of the participants in this study would travel abroad for a colonoscopy, which might be because of similar reasons or as a result of the influence of family, friends or following a trend in the GCC countries for so-called “medical tourism”.
Women in Oman may feel more embarrassed during a colonoscopy examination. A previous study conducted among Muslim women in the USA showed that women preferred a female healthcare provider, particularly with regard to breast, rectal and gynaecological examinations [45]. Also, a study conducted in the United Arab Emirates (UAE) showed with respect to gynaecological and abdominal problems, patients would generally refuse to be treated by male medical students [46].
This current study has limitations. First, although the study has only been conducted in the governorate of Muscat, the capital city of Oman, which could affect the generalisability of the study, we believe that this is not a major issue as most of the population in Muscat are originally from other regions of the country. Nevertheless, a larger national study with recruitment from all regions of Oman is needed for better representative sampling. Secondly, we did not recruit individuals who were illiterate to keep consistency when administering the questionnaire and to avoid any subjective bias which could have arisen if the Bowel and Stomach CAM was administered through face to face interviews with the participants. However, the majority of the population of Oman are young, so we believe that it might not affect the applicability of findings. Thirdly, although we added two additional risk factors for stomach cancer to the Bowel CAM, we do not believe that this will affect the reliability of the questionnaire, particularly as the reliability tests (Cronbach’s alpha) for the Arabic version of the combined bowel and stomach questionnaire was high.
Fourthly, the majority of patients who attended the LHCs were attending for common general practice consultations and the possibility that some of them would have a report bias regarding CRC and stomach cancer is therefore be at a minimum, but this cannot be ruled out completely. Finally, a small subset of the participants (20.5%) had a family history of cancer and, similarly, the interference or bias that they may have when responding cannot be ruled out. Nonetheless, the question is asking about any type of cancer and not specifically about bowel or stomach cancer. Furthermore, the question is part of the Bowel CAM questionnaire and it is not recommended that participants with a family history of cancer are eliminated from the analysis.
Conclusion
There is a need to increase the public’s awareness of stomach cancer and CRC in Oman, particularly in view of the noted increase in the incidence of stomach cancer and CRC in the past few years, making them the commonest type of cancer in the country. The public does not seem to be aware that the effect of a “westernised life style”, such as obesity, eating food in low fibre, doing less exercise, eating food in high salt, are all risk factors for CRC. Indeed, there is an alarming increasing trend in obesity and type 2 diabetes mellitus in GCC countries which needs immediate intervention [47].
As this study showed, the level of education of an individual plays a significant role in their recognition of stomach cancer and CRC risk factors; educational initiatives are required to improve the community’s awareness of promoting a healthy lifestyle and to increase cancer awareness. Television, radio, press, social media and leaflet materials could be distributed in the LHCs in different governorates and regions in Oman to help increase cancer awareness. Also, school curriculums could include sessions on cancer education and this information should be reiterated to students periodically.
It seems that women, less-educated individuals and the elderly were reporting barriers to seeking early medical help due to psychological/emotional barriers or physical barriers. People’s attitudes, beliefs and behaviour could influence the process of medical help-seeking behaviours. Thus, targeting these vulnerable groups through health education, community awareness and encouraging them to seek early medical intervention would help to promote early medical help seeking and improve the rate of early cancer diagnosis.
Finally, although there is currently no screening programme for CRC in Oman, a strategy to establish such a programme, like in other developed countries, is paramount as the incidence of CRC has increased in the past few years. The importance of CRC screening should be emphasised through intensive community awareness so that more people will attend and make the programme more successful. The reasons and barriers for not attending screening programmes, which includes psychosocial, cultural, beliefs and religion reasons, must be studied before the programme’s implementation. Nonetheless, the availability of resources to conduct screening within the parameters of both cost-effectiveness and cost-benefit may remain a challenge to the healthcare system in Oman.
References
World Health Organization. Cancer—fact sheet. 2015. http://www.who.int/mediacentre/factsheets/fs297/en/. Updated February 2017 (Accessed 30.5.2017)
Center MM, Jemal A, Ward E (2009) International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomark Prev 18(6):1688
Marley AR, Nan H (2016) Epidemiology of colorectal cancer. Int J Mol Epidemiol Genet 7(3):105–114
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA A Cancer Journal for Clinicians 61(2):69–90
Niksic M, Rachet B, Duffy SW, Quaresma M, Moller H, Forbes LJ (2016) Is cancer survival associated with cancer symptom awareness and barriers to seeking medical help in England? An ecological study. Br J Cancer 115(7):876–886
Al-Azri M, Al-Maskari A, Al-Matroushi S, Al-Awisi H, Davidson R, Panchatcharam SM et al (2016) Awareness of cancer symptoms and barriers to seeking medical help among adult people attending primary care settings in Oman. Health Services Research and Managerial Epidemiology 3:1–10
Oberoi DV, Jiwa M, McManus A, Hodder R (2015) Men’s help-seeking behavior with regards to lower bowel symptoms. Am J Health Behav 39(2):212–221
Pedersen AF, Hansen RP, Vedsted P (2013) Patient delay in colorectal cancer patients: associations with rectal bleeding and thoughts about cancer. PLoS One 8(7):e69700
Weller D (2006) Colorectal cancer in primary care: even with national screening, primary care can do more to cut mortality. BMJ 333(7558):54–55
Esteva M, Leiva A, Ramos MÕ, Pita-Fern_Éndez S, Gonz_Élez-Luj_Én L, Casamitjana M et al (2013). Factors related with symptom duration until diagnosis and treatment of symptomatic colorectal cancer. BMC Cancer 13(1):1–13
Adelstein BA, Macaskill P, Turner RM, Irwig L (2012) Patients who take their symptoms less seriously are more likely to have colorectal cancer. BMC Gastroenterol 12(1):1–9
MacDonald S, Macleod U, Campbell NC, Weller D, Mitchell E (2006) Systematic review of factors influencing patient and practitioner delay in diagnosis of upper gastrointestinal cancer. Br J Cancer 94(9):1272–1280
Simon AE, Waller J, Robb K, Wardle J (2010) Patient delay in presentation of possible cancer symptoms: the contribution of knowledge and attitudes in a population sample from the United Kingdom. Cancer Epidemiol Biomark Prev 19(9):2272–2277
Przybyla AG, Crockett JA, Rex JC, Culumovic PJ (2014) Current screening guidelines overlook a significant number of patients treated for colorectal cancer. Am Surg 80(6):539–543
Ministry of National Economy (2010). Oman census summary http://www.data.gov.om/ (Accessed 30.5.2017)
Al-Lawati JA, Mabry R, Mohammed AJ (2008) Addressing the threat of chronic diseases in Oman. Prev Chronic Dis 5(3):A99
Ministry of Health (2013). Cancer incidence in Oman. Department of Non-Communicable Disease. Directorate General of Primary Health care. Ministry of Health, Sultanat of Oman
Al-Madouj, Eldali A, Al-Zahrani A (2011). Ten-year cancer incidence among nationals of the GCC states 1998–2007 (prepared under the supervision of Executive Board Of Health Ministers’ Council For the Gulf Cooperation Council State
Kumar S, Burney IA, Zahid KF, Souza D, Belushi MA, Mufti TD et al (2015) Colorectal cancer patient characteristics, treatment and survival in Oman: a single center study. Asian Pac J Cancer Prev 16(12):4853–4858
Cancer Research UK University College London, King’s College London, Oxford University. Bowel Cancer Awareness Measure (CAM) toolkit version 2.1. 2011. Cancer Research UK
Power E, Simon A, Juszczyk D, Hiom S, Wardle J (2011) Assessing awareness of colorectal cancer symptoms: measure development and results from a population survey in the UK. BMC Cancer 11(1):366
Al-Azri M, Al-Hamedi I, Al-Awisi H, Al-Hinai M, Davidson R (2015) Public awareness of warning signs and symptoms of cancer in Oman: a community-based survey of adults. Asian Pac J Cancer Prev 16(7):2731–2737
Rahim HF, Sibai A, Khader Y, Hwalla N, Fadhil I, Alsiyabi H et al (2014) Non-communicable diseases in the Arab world. Lancet 383(9914):356–367
Robb K, Stubbings S, Ramirez A, Macleod U, Austoker J, Waller J et al. Public awareness of cancer in Britain: a population-based survey of adults. Br J Cancer 101(S2):S18-S23
Forbes LJL, Simon AE, Warburton F, Boniface D, Brain KE, Dessaix A et al (2013) Differences in cancer awareness and beliefs between Australia, Canada, Denmark, Norway, Sweden and the UK (the International Cancer Benchmarking Partnership): do they contribute to differences in cancer survival? Br J Cancer 108(2):292–300
Al-Azri MH (2016) Delay in cancer diagnosis: causes and possible solutions. Oman Med J 31(5):325–326
Lynes K, Kazmi SA, Robery JD, Wong S, Gilbert D, Thaha MA (2016). Public appreciation of lifestyle risk factors for colorectal cancer and awareness of bowel cancer screening: a cross-sectional study. International journal of surgery 36, part a:312-318
Albano JD, Ward E, Jemal A, Anderson R, Cokkinides VE, Murray T et al (2007) Cancer mortality in the United States by education level and race. J Natl Cancer Inst 99(18):1384–1394
Mulligan CR, Meram AD, Proctor C, Wu H, Zhu K, Marrogi AJ (2006) Unlimited access to care: effect on racial disparity and prognostic factors in lung cancer. Cancer Epidemiol Biomark Prev 15(1):25
Vu M, Azmat A, Radejko T, Padela AI (2016) Predictors of delayed healthcare seeking among American Muslim women. J Women's Health 25(6):586–593
Al-Azri M, Al-Awisi H, Al-Rasbi S, El-Shafie K, Al-Hinai M, Al-Habsi H et al (2014) Psychosocial impact of breast cancer diagnosis among Omani women. Oman Medical Journal 29(6):437
Smith LK, Pope C, Botha JL (2003) Patients’ help-seeking experiences and delay in cancer presentation: a qualitative synthesis. Lancet 366(9488):825–831
Burgess C, Hunter MS, Ramirez AJ (2001) A qualitative study of delay among women reporting symptoms of breast cancer. Br J Gen Pract 51(473):967–971
Caring demands and delay in seeking care in African American women newly diagnosed with breast cancer: an ethnographic, photographic study. 2001
Kumar S, Burney IA, Zahid KF, Souza PC, Belushi MA, Meki TDM et al (2015) Colorectal cancer patient characteristics, treatment and survival in Oman: a single center study. Asian Pac J Cancer Prev 16:4853–4858
Siegel R, DeSantis C, Jemal A (2014) Colorectal cancer statistics. CA A Cancer Journal for Clinicians 64(2):104–117
O'Connell JB, Maggard MA, Livingston EH, Yo CK (2004) Colorectal cancer in the young. Am J Surg 187(3):343–348
Macleod U, Mitchell ED, Burgess C, MacDonald S, Ramirez AJ. Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. Br J Cancer 101(S2):S92-S101
Quaife SL, Forbes LJL, Ramirez AJ, Brain KE, Donnelly C, Simon AE et al (2014) Recognition of cancer warning signs and anticipated delay in help-seeking in a population sample of adults in the UK. Br J Cancer 110(1):12–18
McCaffery K, Wardle J, Waller J (2003) Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Prev Med 36(5):525–535
Vernon SW (1997) Participation in colorectal cancer screening. A review 89(19):1406–1422
Lansdorp-Vogelaar I, Knudsen AB, Brenner H (2010) Cost-effectiveness of colorectal cancer screening: an overview. Best Pract Res Clin Gastroenterol 24(4):439–449
Bastani R, Gallardo NV, Maxwell AE (2001) Barriers to colorectal cancer screening among ethnically diverse high-and average-risk individuals. J Psychosoc Oncol 19(3–4):65–84
Qumseya BJ, Tayem YI, Dasa OY, Nahhal KW, Abu Limon IM, Hmidat AM et al (2014) Barriers to colorectal cancer screening in Palestine: a national study in a medically underserved population. Clin Gastroenterol Hepatol 12(3):463–469
Hasnain M, Connell KJ, Menon U, Tranmer PA (2010) Patient-centered care for Muslim women: provider and patient perspectives. J Women's Health 20(1):73–83
McLean M, Al Ahbabi S, Al Ameri M, Al Mansoori M, Al Yahyaei F, Bernsen R (2010) Muslim women and medical students in the clinical encounter. Med Educ 44(3):306–315
Alharbi NS, Almutari R, Jones S, Al-Daghri N, Khunti K, de Lusignan S (2014) Trends in the prevalence of type 2 diabetes mellitus and obesity in the Arabian gulf states: systematic review and meta-analysis. Diabetes Res Clin Pract 106(2):e30–e33
Acknowledgments
The authors would like to thank the participants and the Directorate General of Health Services of Muscat governorate for allowing this study to be conducted in the LHCs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study has been approved by the Medical Research and Ethics Committee of the College of Medicine and Health Sciences at Sultan Qaboos University, Muscat, Oman (MREC #1088).
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Funding
None.
Rights and permissions
About this article
Cite this article
Al-Azri, M., Al-Kindi, J., Al-Harthi, T. et al. Awareness of Stomach and Colorectal Cancer Risk Factors, Symptoms and Time Taken to Seek Medical Help Among Public Attending Primary Care Setting in Muscat Governorate, Oman. J Canc Educ 34, 423–434 (2019). https://doi.org/10.1007/s13187-017-1266-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-017-1266-8