Abstract
Our aim was to synthesise the existing empirical literature and theoretical perspectives on the physical activity (PA) promotion practices and determinants of cancer clinicians and health professionals. We conducted a narrative review of theory and evidence to develop practice recommendations for improving the promotion of PA to cancer patients. Surveyed health professionals were aware of many benefits of PA for their cancer patients, although only ~40 % promoted PA to selected cancer patients. Walking was the most commonly promoted form of PA, with this promoted to assist patients control their weight and cardiovascular health risk. Barriers to promotion of PA included lack of time and knowledge of PA and behaviour change skills. Health professionals appear interested in promoting PA to their cancer patients, yet encounter several barriers. Further research is warranted to assist health professionals improve their PA promotion. An adapted reflective-impulsive model of social behaviour shows promise for assisting health professionals overcome barriers and provides an evidence-based theoretical framework for improving communication with patients. Universities, hospitals and/or health-care accreditation organisations also have important roles to play in assisting health professionals improve their promotion of PA to patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is growing evidence demonstrating that physical activity (PA), be it aerobic, resistance (strength) or a combination thereof, produces physical and psychosocial benefits [7, 11, 16] that counteract many of the adverse effects of common cancer treatments [8, 17]. Such research has led professional organisations, including the American Cancer Society, to develop position statements outlining the importance of PA and recommending that physically inactive patients become more active. Specifically, guidelines recommend that cancer patients perform 150 min of aerobic and 60 min of resistance training per week [16].
Health professions (e.g. general practitioners, oncologists and oncology nurses) are expected to provide high-quality, evidence-based education and counselling to their patients in relation to the potential risks and benefits of cancer screening and/or treatment [20]. However, studies have shown that health professionals report numerous barriers preventing them from discussing PA with their patients and, most importantly, assisting them to make the necessary behavioural changes to accommodate recommended PA levels [5, 6, 18, 21]. We offer a narrative review of the relevant empirical work and propose practice recommendations for health professions, hospitals and universities for improving the promotion of PA to cancer patients.
Discussing Physical Activity with Cancer Patients
A recent study revealed that most cancer patients do not adhere to the PA guidelines of the American Cancer Society, and many are less active than their age-matched, non-cancer peers [10]. In light of research demonstrating the benefits of PA for cancer patients, it is clear that health professionals have a duty of care to more regularly discuss PA during their consultations. There is now considerable research that has examined the determinants of cancer patients’ PA levels in an attempt to investigate possible ways to increase their PA [9, 19, 13, 14]. Surprisingly, very little of this research has focused on the role of the health professional in supporting the PA behaviour of the patients [18, 15]. A summary of the main issues facing cancer patients post-diagnosis, the benefits of regular PA and the possible role of health professionals in assisting their patients becoming more physically active is summarised in Fig. 1.
Physical Activity Promotion Practices and Determinants of Health Professionals
Promotion of PA by health professionals has been shown to significantly improve health, physical and psychosocial outcomes for a variety of patient groups [12, 3]. The promotion of PA by a health professional to their cancer patients has demonstrated significant increases in patients’ PA levels, energy expenditure, aerobic fitness, muscular strength and quality of life as well as reduction in the number of barriers to PA [2, 4]. Jones et al. also reported significantly larger increases in PA levels if patients remembered the nature of the PA advice from the health professional [4]. However, relatively little is known about the PA promotion practices of health professionals and the factors that influence this promotion to their cancer patients [5, 6, 18, 21].
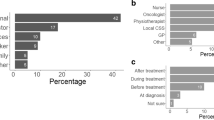
In relevant work, studies have reported that up to 40 % of health professionals only promote PA to the patients they feel would benefit from being more physically active, rather than promoting PA as a standard part of usual care for all patients [5, 6, 18, 21]. While these results are somewhat encouraging, the survey response rates were 14–62 % which may indicate a potential response bias, whereby health professionals who regularly promote PA to their patients may have more likely completed the surveys [5, 6, 18, 21]. These findings, therefore, should be interpreted with some caution. Nonetheless, the surveys revealed that many health professionals were aware that PA could reduce the physical side effects of treatment, lower the risk of developing other chronic conditions and improve physical function, mental health and quality of life. Of the health professionals who promoted PA, they also endorsed evidence-based aerobic activities such as walking for weight loss, cardiovascular health, improved mental health and quality of life [16]. Considerably fewer promoted resistance training as a form of PA to their patients, despite resistance training being more beneficial than aerobic activity in counteracting the substantial declines in muscle mass, strength and physical performance seen with common cancer treatments [7]. Most importantly, the survey data revealed that there are many barriers to PA promotion for these health professionals. For example, health professionals thought that other professionals were promoting PA to the patients, reported lacking the time needed for such discussions during patient consultations and indicated that they lacked the required knowledge in PA promotion [5, 6, 18, 21]. These barriers appeared quite similar to the concerns reported by 236 cancer patients about their regular consultations with their health professionals [1]. Brandes et al. [1] reported that patients indicated their primary barriers to discussing their concerns with health professionals related to the health professionals’ behaviour (e.g. a lack of empathy, not inviting the patients’ to identify their concerns and an inability to provide accurate information) as well as the consultation environment (e.g. lack of time to listen to concerns).
Taken together, these findings warrant health professionals being more proactive in the promotion of PA to their patients. This may be achieved by health professionals initiating such discussions with their patients, attentively responding to questions from their patients and assisting their patients develop strategies to overcome any barriers that may make regular PA difficult. However, there is still much to learn about the primary determinants influencing health professionals’ promotion of PA to their patients. If these determinants are better understood, behavioural interventions using evidence-based behavioural change models can assist health professionals’ in promoting healthy behaviours like PA and result in significantly improved outcomes for their patients.
Possible Ways to Improve the Physical Activity Promotion Practices of Health Professionals
When discussing PA and other healthy behaviours with their patients, it is recommended that health professionals utilise evidence-based behavioural change practices [3]. In an extensive review of approaches to improve patient-physician communication, Woulda and van de Weil proposed using an adapted version of the reflective-impulsive model of social behaviour [22]. While Woulda and van de Wiel [22] acknowledge that the full implementation of the reflective impulsive model requires considerable effort, they recommended its use as a benchmark for improving patient-physician communication and identified five key learning objectives and teaching methods for communication education. Specific examples of how health professionals may use this approach when discussing PA with their cancer patients are highlighted in Table 1.
As alluded to in Table 1, it is understood that the behaviour, knowledge and/or work environment of the health professional may act as facilitators or barriers to effective patient-centred communication about PA. Many health professionals may identify aspects of their own behaviour or work environment that would act as barriers to effective PA communication with their patients; therefore, we recommend the development of referral networks, whereby patients are referred to specialists in PA (e.g. exercise physiologists or physiotherapists or psychosocial/behavioural counselling).
The reflective impulsive model [22] also has major implications for training models used by universities and hospitals. It is recommended that universities and hospitals provide a series of educational experiences which progressively develop the clinical communication skills of their students, interns and staff [22, 23]. An overview of how this may be applied to improving PA promotion and counselling for cancer patients is provided in Table 2.
Conclusions
Health professionals appear interested in promoting PA to their patients, but evidence suggests that they experience several barriers to this activity. It is vital that health professionals use evidence-based behavioural change approaches in promoting the proven benefits of PA during their patient consultations. Universities, hospitals and accreditation bodies can all play important roles in assisting health professionals achieve this goal.
More research is required to continually improve practice in this area. Relevant studies may examine the following: patient benefits obtained through behavioural theory-based PA promotion programs led by primary cancer clinicians such as oncologists, the determinants and current PA promotion practices of a wider variety of health professionals, and how differences in health professional and patient characteristics may impact PA promotion and patient outcomes.
Based on the strong evidence for the benefits of PA for cancer survivorship [7, 11, 16], health professionals, universities, hospitals and national health-care accreditation organisations are encouraged to consider the conversational value and implementation processes of PA promotion as part of their usual care for all cancer patients, not just those for those who are subjectively assessed by health professionals to need it. We recommend that evidence-based practice educational modules include discussions on the benefits of PA as well the behavioural change models that may best increase PA levels for cancer patients. Hospitals should examine ways they can better encourage their primary cancer clinicians to work more collaboratively with PA and counselling specialists in this endeavour. This may be achieved by hospitals developing improved PA resources and/or referral pathways to cancer-specific PA programs that are more accessible to patients. Collectively, these approaches may improve PA promotion by health professionals and result in improved outcomes for patients [14, 19].
References
Brandes K, Linn AJ, Smit EG, van Weert JCM (2015) Patients’ reports of barriers to expressing concerns during cancer consultations. Patient Educ Couns 98(3):317–322. doi:10.1016/j.pec.2014.11.021
Damush TM, Perkins A, Miller K (2006) The implementation of an oncologist referred, exercise self-management program for older breast cancer survivors. Psycho-Oncology 15(10):884–890. doi:10.1002/pon.1020
Gagliardi AR, Faulkner G, Ciliska D, Hicks A (2015) Factors contributing to the effectiveness of physical activity counselling in primary care: a realist systematic review. Patient Educ Couns 98(4):412–419. doi:10.1016/j.pec.2014.11.020
Jones LW, Courneya KS, Fairey AS, Mackey JR (2004) Effects of an oncologist’s recommendation to exercise on self-reported exercise behavior in newly diagnosed breast cancer survivors: a single-blind, randomized controlled trial. Ann Behav Med 28(2):105–113
Jones LW, Courneya KS, Peddle C, Mackey JR (2005) Oncologists’ opinions towards recommending exercise to patients with cancer: a Canadian national survey. Support Care Cancer 13(11):929–937. doi:10.1007/s00520-005-0805-8
Karvinen KH, McGourty S, Parent T, Walker PR (2012) Physical activity promotion among oncology nurses. Cancer Nurs 35(3):E41–E48. doi:10.1097/NCC.0b013e31822d9081
Keogh JWL, MacLeod RD (2012) Body composition, physical fitness, functional performance, quality of life and fatigue benefits of exercise for prostate cancer patients: a systematic review. J Pain Symptom Manag 43(1):96–110. doi:10.1016/j.jpainsymman.2011.03.006
Keogh JWL, Patel A, MacLeod RD, Masters J (2013) Perceptions of physically active men with prostate cancer on the role of physical activity in maintaining their quality of life: possible influence of androgen deprivation therapy. Psycho-Oncology 22:2869–2875. doi:10.1002/pon.3363
Keogh JWL, Patel A, MacLeod RD, Masters J (2014) Perceived barriers and facilitators to physical activity in men with prostate cancer: possible influence of androgen deprivation therapy. Eur J Cancer Care (Engl) 23(2):263–273. doi:10.1111/ecc.12141
LeMasters TJ, Madhavan SS, Sambamoorthi U, Kurian S (2014) Health behaviors among breast, prostate, and colorectal cancer survivors: a US population-based case–control study, with comparisons by cancer type and gender. J Cancer Surviv 8(3):336–348. doi:10.1007/s11764-014-0347-5
Mishra SI, RW Scherer, PM Geigle, DR Berlanstein, O Topaloglu, CC Gotay, and C Snyder (2012) Exercise interventions on health‐related quality of life for cancer survivors. Cochrane Database Syst Rev 8. doi: 10.1002/14651858.CD007566.pub2.
Orrow G, Kinmonth A-L, Sanderson S, Sutton S (2012) Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ 344:e1389
Ottenbacher A, Sloane R, Snyder DC, Kraus W, Sprod L, Demark-Wahnefried W (2013) Cancer-specific concerns and physical activity among recently diagnosed breast and prostate cancer survivors. Integr Cancer Ther 12(3):206–212. doi:10.1177/1534735412449734
Pinto BM, Ciccolo JT (2011) Physical activity motivation and cancer survivorship. Recent Results Cancer Res 186:367–387. doi:10.1007/978-3-642-04231-7_16
Robertson L, Richards R, Egan R, Szymlek-Gay EA (2013) Promotion and support of physical activity among cancer survivors: a service provider perspective. Psycho-Oncology 22(2):441–446. doi:10.1002/pon.3032
Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV et al (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62(4):242–274. doi:10.3322/caac.21142
Schmitz KH, Speck RM, Rye SA, DiSipio T, Hayes SC (2012) Prevalence of breast cancer treatment sequelae over 6 years of follow-up. Cancer 118(S8):2217–2225. doi:10.1002/cncr.27474
Spellman C, Craike M, Livingston P (2014) Knowledge, attitudes and practices of clinicians in promoting physical activity to prostate cancer survivors. Health Educ J 73(5):566–575. doi:10.1177/0017896913508395
Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR (2015) A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv 9(2):305–338. doi:10.1007/s11764-014-0413-z
Trikalinos TA, Wieland LS, Adam GP, Zgodic A, Ntzani EE (2014) AHRQ comparative effectiveness reviews. In: Decision aids for cancer screening and treatment. Agency for Healthcare Research and Quality (US), Rockville (MD)
Williams K, RJ Beeken, A Fisher, and J Wardle. in press. Health professionals’ provision of lifestyle advice in the oncology context in the United Kingdom. Eur J Cancer Care (Engl). doi: 10.1111/ecc.12305.
Wouda JC, van de Wiel HBM (2013) Education in patient–physician communication: how to improve effectiveness? Patient Educ Couns 90(1):46–53. doi:10.1016/j.pec.2012.09.005
Wouda JC, van de Wiel HBM (2014) The effects of self-assessment and supervisor feedback on residents’ patient-education competency using videoed outpatient consultations. Patient Educ Couns 97(1):59–66. doi:10.1016/j.pec.2014.05.023
Acknowledgments
We would like to thank Elizabeth Edwards from Bond University for her constructive criticisms on this manuscript prior to submission.
Conflict of Interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keogh, J.W., Olsen, A., Climstein, M. et al. Benefits and Barriers of Cancer Practitioners Discussing Physical Activity with their Cancer Patients. J Canc Educ 32, 11–15 (2017). https://doi.org/10.1007/s13187-015-0893-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-015-0893-1