Abstract
Medication adherence plays an important role in optimizing the outcomes of many treatment and preventive regimens in chronic illness. Self-report is the most common method for assessing adherence behavior in research and clinical care, but there are questions about its validity and precision. The NIH Adherence Network assembled a panel of adherence research experts working across various chronic illnesses to review self-report medication adherence measures and research on their validity. Self-report medication adherence measures vary substantially in their question phrasing, recall periods, and response items. Self-reports tend to overestimate adherence behavior compared with other assessment methods and generally have high specificity but low sensitivity. Most evidence indicates that self-report adherence measures show moderate correspondence to other adherence measures and can significantly predict clinical outcomes. The quality of self-report adherence measures may be enhanced through efforts to use validated scales, assess the proper construct, improve estimation, facilitate recall, reduce social desirability bias, and employ technologic delivery. Self-report medication adherence measures can provide actionable information despite their limitations. They are preferred when speed, efficiency, and low-cost measures are required, as is often the case in clinical care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Valid measurement of medication adherence plays a crucial role in healthcare and health research. When a patient is not benefiting from a medication regimen, clinicians need sound adherence information to determine whether the medication is ineffective or not being taken as prescribed. Assessing medication adherence during routine clinical care can further ensure that individuals in need of adherence support interventions receive them, ideally before deleterious outcomes occur. In the context of clinical research, proper interpretation of proof-of-concept trials testing new pharmacologic regimens requires valid adherence data, because any null findings may stem from poor adherence rather than a lack of drug efficacy. Research designed to understand and promote medication adherence also requires precise methods of adherence assessment.
Among many approaches to assessing medication adherence, patient self-report measures remain the most common method [1–6]. These measures are defined by asking respondents to characterize their medication adherence behavior. Self-report measures of medication adherence range from simple single-item questions regarding missed doses to complex multi-item assessments that incorporate reasons for nonadherence [7]. The widespread use of self-report adherence measures in clinical care and research reflects their low cost and ease of implementation across a large variety of medication regimens.
There are two primary challenges related to self-report measures of medication adherence. First, there are longstanding concerns about the validity of these measures due to their vulnerability to social desirability and memory biases that tend to overestimate the degree to which patients execute medication regimens, relative to other assessment methods. Second, there is a paucity of research on how to optimize the validity of self-report adherence measures in clinical care or health research. The myriad of self-report adherence measures that are available in the research literature contain substantial variation in their question phrasing, response scale formats, time intervals for recall, and modes of administration [1, 5, 7, 8]. Few studies have empirically tested the comparative validity of these varied methodologic choices [9], and most self-report adherence measures have only been validated within single areas of chronic illness [7].
This paper reviews the current evidence-base behind self-report measures of medication adherence with an eye toward optimizing their selection and use. The paper was the result of the deliberation of a panel of medication adherence research experts from across the disease spectrum, which was assembled by the NIH Adherence Network—a consortium of science officers working at many different NIH institutes, centers, and offices. The panel met in October 2011 and was charged with reviewing the evidence base for self-report measures across major fields of chronic illness prevention and treatment and making best practice recommendations. The conclusions and recommendations of the panel are reported here, along with key directions for future research to strengthen self-report medication adherence assessments.
DEFINING MEDICATION ADHERENCE BEHAVIOR
Medication adherence has been defined as “the extent to which patients take medications as prescribed by their health care providers” [10]. A scientific consensus group described the primary components of medication adherence as initiation (i.e., starting a recommended medication regimen), implementation (i.e., executing the prescribed dosage schedule), and persistence (i.e., length of time on regimen before discontinuation) [11]. Regimen implementation has been the focus of much research and is commonly defined as the percentage of prescribed medication doses taken over a specific time interval [10].
Adherence behavior is distinct from several other related constructs, such as reasons for nonadherence, patient knowledge or understanding of a medication regimen, perceived adherence barriers or facilitators, adherence self-efficacy, and attitudes or beliefs about medications. These domains may be better conceptualized as antecedents or consequences of medication adherence behavior [12].
IMPACT OF MEDICATION ADHERENCE
Across many chronic medical conditions, adherence has been associated with positive clinical outcomes including improved disease control, reduced symptoms, and decreased complications, hospitalization, and mortality [13–20]. Even modest nonadherence (e.g., 10–20 %) has been linked with clinically significant deteriorations in health outcomes, such as glycemic control, low-density lipoprotein cholesterol levels, and risk for coronary disease [21, 22], as well as failure to achieve health improvements [23], leading to higher healthcare costs [21, 24].
Inadequate adherence to medications is unfortunately widespread across ages, health conditions, and medication regimens [10, 25–27]. DiMatteo’s [27] seminal review of over 500 adherence studies spanning multiple chronic conditions and medication classes reported an average medication nonadherence rate of 24.8 %. Other large studies crossing multiple chronic conditions and drug classes report nonadherence rates around 40–60 % [25, 28, 29], suggesting that approximately one of every two prescription doses are missed. Medication adherence tends to decline over time [30, 31] and discontinuation (nonpersistence) is common [13].
ADVANTAGES AND DISADVANTAGES OF SELF-REPORT ADHERENCE MEASURES
Every method of assessing medication adherence presents advantages and disadvantages [32], and there is no agreement on a single gold standard approach [1, 33–35]. Self-report measures present some specialized advantages and uses for medication adherence assessment. Key advantages include low-cost, noninvasiveness, minimal patient burden, ease of administration, and flexibility in timing and mode of administration. Self-report medication adherence measures are almost certainly the most practical method of measuring adherence in the context of clinical care and can provide information to providers about nonadherence prior to development of adverse clinical outcomes [1, 10, 36–39]. In addition to providing estimates of medication dose-taking behavior, self-reports can uniquely provide information about adherence determinants such as understanding of the medication regimen, reasons for nonadherence, attitudes and beliefs toward medicines, and other psychosocial factors. In clinical research settings, self-reports are frequently one component of triangulation strategies that combine multiple forms of adherence measurement [40], such as using self-report adherence measures to refine adherence data from electronic drug monitors (EDM) [32].
Self-report measures of adherence have several potential disadvantages as well. These include the contestable assumptions that medication adherence behavior can be accurately recalled or reported without deference to social desirability concerns that encourage over-reporting (for a review, see [9]). Social desirability and memory biases can lead to ceiling effects in self-report scales where an unrealistic majority of respondents indicate perfect adherence [41]. In contrast to EDM data, self-report measures seldom provide time-stamped data for adherence behavior, which limits precision when assessing timing or patterns of dose-taking.
AVAILABLE SELF-REPORT ADHERENCE MEASURES
Numerous self-report medication adherence measures have been developed and reported in health research on chronic illness to date. Examples of some of the more commonly used measures include the Morisky scale [42] and variations of the adult AIDS Clinical Trials Group (ACTG) adherence assessment [43]. Three primary components of most self-report measures are the question stem, recall period, and response options [44]. These three elements are operationalized differently across various adherence measures. Many of the most common measures employ count- or estimation-based recall [35]. Count-based measures ask respondents to report the number of medication doses missed or taken in a certain interval, whereas estimation measures ask respondents to characterize their overall degree of regimen execution in terms of ratings or visual analog scales. The number of items on self-report adherence measures varies from single-item questions to more elaborate multi-item scales [1, 5, 45]. The number of items often reflects the degree to which the measure is seeking to capture a variety of adherence-related factors, such as reasons for nonadherence.
A set of commonly-used self-report medication adherence measures with available validation data is provided in Appendix. To identify these measures, the terms “adherence,” “compliance,” “self-report,” and “measure” were used in combination to search the electronic database PUBMED. The criteria used for study inclusion in this review were: (a) research report regarding one or more retrospective self-report measures of medication adherence behavior; (b) published in English in the last 30 years; and (c) reporting validation data relative to clinical outcomes and/or other adherence measures in one or more areas of chronic illness. Despite these search efforts, it is possible that additional studies meeting these criteria were missed.
The wide variety of self-report adherence measures is striking. The characteristics of these measures vary substantially in terms of single or multiple items, response options, and specified recall period (if any). Measures may focus on the extent of medication adherence and/or other considerations (e.g., reasons for nonadherence). A few measures have been validated in multiple chronic illness areas, but most have been validated in only one. The validity data reported for each measure also varies in strength and scope, which invites a broader look at the validity of this measurement approach as a whole.
VALIDITY OF MEDICATION ADHERENCE SELF-REPORTS
Considerable research has sought to evaluate the validity and sensitivity/specificity of self-report measures. The criterion validity of adherence measures is established through comparison with clinical outcomes and biological endpoints likely affected by adherence [32]. Convergent validity has been tested through comparison of self-report measures to other medication adherence measures, such as EDM and pharmacy refill measures [32].
Criterion validity
Research generally shows low-to-moderate correspondence between self-report adherence measures and clinical outcomes, and estimates are highly variable by chronic disease area and measure [46]. Two syntheses of research conducted with adult HIV/AIDS patients offer strong evidence that self-report medication adherence measures can significantly and meaningfully predict clinical outcomes [5, 47]. Across pooled studies containing over 15,000 HIV patients, Nieuwkerk and Oort [47] determined that those who self-report nonadherence (at any cutoff level) were 2.31 times more likely to have clinically detectable HIV viral load than those who self-report high adherence. Simoni and colleagues [5] examined 77 studies and found statistically significant correlations between self-report adherence rates and viral load in 84 % of assessment intervals, with correlation coefficients ranging from 0.30 to 0.60. The consistent correspondence of self-report adherence to HIV viral load led Simoni et al. to conclude that “even brief self-report measures of antiretroviral adherence can be robust” (p. 227). Recent meta-analyses further support the criterion validity of self-report adherence measures in HIV/AIDS when used with pediatric, child, and adolescent patients and their caregivers [48, 49].
The criterion validity of self-report medication adherence measures in chronic illnesses other than HIV/AIDS has mostly been lower or more variable. For example, hypertension studies report associations between blood pressure and various self-report measures of antihypertensive medication adherence that range from very weak [50] to a modest yet statistically significant relationship [51, 52]. In type 2 diabetes, few studies have tested the relationship between glycemic control and self-report of medication adherence [2]. Although some diabetes research supports the validity of self-report measures [19, 53], a review of diabetes treatment adherence studies found that just 42.9 % (6 of 14) of studies that used self-report measures found a statistically significant relationship with HbA1c levels [18].
Variable correspondence between self-report adherence and clinical outcomes across chronic conditions may reflect variation in the strength of the adherence-outcomes relationship across different illnesses. In type 2 diabetes adherence research, Gonzalez and colleagues [53] noted that modest relationships between self-report measures and clinical outcomes may partially reflect a modest effect of medication (even when regularly taken) on clinical outcomes. Most evidence shows that medication adherence plays an important role in glycemic control, but many other factors can affect glycemic control besides medication-taking (e.g., diet, exercise, extent of insulin deficiency, and adequacy of the prescribed regimen), so comparisons of self-report medication adherence measures to the clinical outcome of HbA1c levels should show a modest relationship at best. Expectations regarding the ability of self-report measures to predict clinical outcomes should be set accordingly [2, 53].
Simultaneous comparison of multiple adherence measurement approaches with clinical outcomes is helpful for judging their comparative validity. Research typically indicates that self-report measures have weaker or less consistent relations with clinical outcomes relative to other measures of adherence [18, 51, 54]. A review of type 2 diabetes research found that significant relationships between medication adherence and glycemic control occurred more frequently in studies measuring adherence via prescription refill rather than various self-report measures [18]. A review of type 1 diabetes research found that the relation between adherence to diabetes management behaviors and glycemic control in type 1 diabetes showed no overall differences when using either self-reports or blood glucose meter downloads, but studies using self-report measures showed significant heterogeneity in their effect size estimates, whereas meters showed little variability [19]. In HIV research, Arnsten and colleagues [54] concluded that both self-reports and EDM devices show strong correspondence to HIV viral load, but EDMs were more sensitive for detecting nonadherence than self-report. These reports indicate that self-report measures contain value for predicting clinical outcomes, but this value may be limited relative to more precise yet resource-intensive electronic instruments.
Convergent validity
Syntheses of chronic illness research have generally demonstrated moderate relationships between self-report medication adherence measures and other adherence assessments. In a review of 41 medication adherence studies, Shi and colleagues [55] determined that a majority of studies (68 %) report correlations between self-report and EDM adherence measures that are either high (27 %), moderate (29 %), or low yet statistically significant (12 %). A related meta-analysis estimated that the pooled correlation coefficient between self-report and electronically monitored adherence was 0.45 (95 % CI, 0.34–0.56) [56]. Moderate correlations between self-report and electronic monitoring reflect the performance of both adherence measures, and as such, may reflect limitations in self-reports as well as logistic challenges in EDM [57].
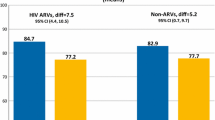
Research on the convergent validity of self-report adherence measures shows clear evidence that they tend to overestimate the extent of regimen execution relative to other adherence assessments [32, 46]. In an examination of 57 studies across many chronic illnesses, Garber and colleagues [8] found high concordance between self-report and other adherence assessments in 43 % of comparisons. Among comparisons that were not highly concordant, self-reports produced higher estimates of adherence than other assessment methods 92 % of the time (45 out of 49 comparisons). A meta-analysis showed the estimated degree of regimen execution is approximately 15 % higher by self-report when compared with EDM devices [56], which is consonant with estimates in other reviews and syntheses [5, 35, 56, 58].
Sensitivity and specificity
Because of potential over-reporting, self-report adherence measures are considered to have good specificity (i.e., positive predictive value) and weak sensitivity (i.e., negative predictive value) for detecting poor adherence [5, 32, 46]. Stated simply, self-reports of nonadherence can be trusted; self-reports of adherence less so. Osterberg and Blaschke [10] explained that “a patient who admits to poor adherence is generally being candid.”
A review of self-report measures found that only 12 of 43 scales reported sensitivity and specificity data [7]. Sensitivity and specificity may be infrequently calculated because it requires comparison with a “gold-standard” clinical outcome or adherence measure, as well as establishment of an appropriate cut-off for determining nonadherence—and there is lack of consensus on neither point. In light of the strong tendency for over-reporting with self-report adherence, it has been recommended that any dichotomization occur at the 100 % mark (i.e., perfect vs. imperfect self-report adherence) [5, 58].
RECOMMENDATIONS FOR OPTIMIZING THE VALIDITY OF SELF-REPORT MEASURES
Although self-report measures can show valid correspondence to health outcomes and other adherence assessment methods, the limitations of this assessment approach are evident in its routine overestimation of adherence. Evidence-based steps to strengthen the validity and precision of self-report measures are discussed below and further summarized in Table 1.
Use a validated self-report measure where possible
Failure to use standardized and validated self-report measures is a common problem in much of health research and clinical practice [1, 35]. A review of 41 studies of the agreement between adherence self-report measures and EDM devices identified 19 publications that failed to name or describe the particular self-report measure used in the study; these studies showed significantly lower correspondence between self-report and electronically monitored adherence when compared with studies that used named, standardized self-report measures [55]. With many validated self-report scales available for clinical or research use, there are sound options from which to choose (see Appendix). It is recommended that researchers and clinicians select a self-report measure that has prior validation data within the relevant chronic illness area and preferably one that has demonstrated both concurrent and criterion validity [35]. To help improve available information on measures, adherence-related publications should include a clear description of any self-report measure and its administration method, along with descriptive data resulting from the measure (e.g., mean, median, standard deviation) [9, 35].
Define the adherence construct you want to assess
It is important to define the specific construct of interest when conducting medication adherence assessments and to select an appropriately corresponding measure [7, 52, 59, 60]. Voils and colleagues [12, 52, 61] have argued that self-report adherence measures often conflate two distinct constructs—the extent of nonadherence and reasons for nonadherence—and this conflation may be one factor that has limited the psychometric properties and validity of many existing self-report measures. For example, many commonly used self-report measures of medication adherence in hypertension [62–66] are wholly or partially composed of items concerning reasons for missed doses (e.g., due to forgetfulness, side effects, attitudes toward medicines). Voils and colleagues maintained that reasons for nonadherence represent a conceptually distinct antecedent to adherence behavior, and that different measurement models and validation methods are appropriate for each.
When selecting validated self-report measures, researchers and clinicians should consider if they wish to assess extent of medication adherence, reasons for nonadherence, or both—and a scale matched to the particular clinical or research need should be selected. Voils’ group has developed two self-report adherence measures for use in hypertension research or clinical care that provide discrete assessment of the extent of medication adherence (3 items) and reasons for nonadherence (21 items), and the scales have shown promising psychometric properties and convergent and critierion validity [52]. Since many chronic conditions involve multiple forms of health behavior (e.g., medication dose-taking, dietary guidelines, exercise, prescription refills), researchers and clinicians should additionally be clear about the specific adherence behavior that they seek to assess when selecting an adherence measure [60, 67].
Optimize response options and recall periods to reduce ceiling effects
Research is yielding new insights into optimal response options and recall periods for self-report measures of medication adherence. Wilson and colleagues have argued that individuals completing self-report scales typically make estimates of their adherence behavior rather than conscientiously remembering and counting doses taken or missed [9]. Self-report measures that ask participants to make global estimates of their adherence behavior instead of reporting doses missed or doses taken may therefore be helpful. A series of HIV studies [44, 68–70] have determined that self-report measures with rating scales as response options (e.g., “In the last 30 days, how good a job did you do at taking HIV medicines in the way you were supposed to? Never, rarely, sometimes, usually, almost always, always”) yield greater variability and reduced ceiling effects (i.e., reports of perfect adherence) than measures asking about a specific number of missed doses. Similar findings have emerged in hypertension studies, although Gonzales and colleagues [53] found the best performance when asking for an estimate of the percentage of doses taken, rather than rating adherence on a Likert-type scale. This evidence suggests that self-report measures that ask for global estimates of adherence may be preferable.
Self-report adherence measures which specify a time frame for recall of adherence behavior are helpful when conducting longitudinal assessments that examine adherence trends over time [1, 5, 12]. Determining the optimal recall period requires balancing shorter intervals (to improve recall/estimation) with longer intervals (to increase the representativeness of the sampled time period and capture cases of infrequent nonadherence). Studies comparing self-report measures with different recall time frames have determined that 30-day recall intervals reduce ceiling effects relative to shorter intervals [44, 68, 69, 71]. A single-item rating of medication adherence over the last 30 days has been validated against viral load in large HIV patient samples and showed the smallest ceiling effect relative to other self-report measures [44, 68, 69]. Cognitive testing of adherence items indicates that the phrase “30 days” is preferable to “the last month” because the latter can be misunderstood as reflecting the calendar month [70].
Although these findings suggest that estimated adherence over 30-day periods may be optimal, this approach could present concerns when working with populations characterized by significant cognitive impairment or memory problems, such as persons with severe mental illness or dementia. Basic approaches to assist recall include use of medication lists and pill diagrams, as well as anchoring recall to salient events through a timeline follow-back method [5, 9]. Assessment of self-reported medication adherence among cognitively compromised populations may additionally benefit from more specialized techniques such as the conduct of daily or periodic ecologic assessments via text message or interactive voice response surveys regarding medication adherence over the last 24 h [72]. For groups characterized by severe cognitive impairment and memory deficits, the use of adherence measures other than self-report (e.g., pill counts, EDM, or drug levels) may be preferred.
Address social desirability concerns
Efforts to reduce social desirability concerns among individuals completing self-report adherence measures should help to improve their validity. Nieuwkerk et al. [71] used a social desirability scale to stratify a large sample of Dutch HIV patients into those reporting lower vs. higher social desirability concerns. The team found that the relationship between self-report medication adherence and viral load was statistically significant for patients indicating low social desirability concerns, but not for those indicating high social desirability concerns.
Several techniques may help address social desirability concerns. Regardless of the assessment modality or setting, it is usually beneficial to introduce adherence items with a statement which normalizes nonadherence by acknowledging the widespread nature of nonadherence and/or the difficulty of always taking all medications [5, 10, 32, 35]. Providers should approach adherence questions with patients in a nonjudgmental manner. A research staff member who interviews a patient to obtain self-report adherence data should not be the same person who is delivering an adherence counseling intervention to that research participant. Another important approach is to avoid administration of self-report adherence measures through face-to-face interviews in favor of utilizing computer or paper-based self-administration of questionnaires. Finally, a validated measure of social desirability could be included in research studies to provide a means of statistically adjusting adherence estimates for each participant’s individual level of social desirability, thus potentially minimizing its effect upon associations between adherence and outcomes.
Consider computer administration
Computer technology has the potential to improve accuracy of self-report by reducing biases caused by social desirability, interviewer characteristics, and questionnaire structure. Studies in many domains have demonstrated that computer administration of sensitive questions has been shown to increase reporting levels of sensitive behaviors, particularly in comparison with interviewer-based administration [73, 74] as patients prefer and are more willing to disclose sensitive information to a computer rather than an interviewer [74–87]. Direct computer entry further enhances the quality of data by not allowing double or ambiguous answers [88], and it is often associated with a lower rate of unanswered questions than paper forms [80, 82, 85, 88, 89] because patients must provide a valid response to a question and/or press the “next” button to move on.
Besides computer administration, several other alternatives to interviewer-based collection of adherence information are available. These include paper questionnaires, diaries, interactive voice response (IVR) calls, and text messaging. When reviewing the validity of self-report adherence measures, Garber and colleagues [8] determined that questionnaire or diary measures were superior to in-person interviews in terms of their correspondence to objective adherence measures like EDM and pharmacy refill measures [8]. Although little research is available regarding use of IVR for adherence measurement in comparison with other assessment modalities, some research has been conducted on the use of IVR to increase adherence, with mixed results [90–92]. The viability of interactive text-messaging for monitoring medication adherence remains unclear. This method appears to overestimate adherence when compared with MEMS or laboratory-based measures of symptom status and functioning [93, 94]. One study found text message reminders to be feasible and acceptable, however, response rates to requests about adherence were low (48 %) [95]. More research is needed on the use of these modalities for adherence measurement and intervention.
Technology is not a panacea for self-report validity concerns. For example, randomization of children with asthma and their caregivers to either audio computer-assisted self-interviewing (ACASI), face-to-face interviews, or paper questionnaire versions of a self-report adherence measure made no appreciable difference in adherence estimates compared with electronic adherence data from metered-dose inhalers, and each modality represented an overestimate compared with objectively monitored adherence [96]. Most evidence nonetheless indicates that computer administration of self-report adherence measures should improve their validity.
CONTEXTUAL CONSIDERATIONS IN SELF-REPORT ADHERENCE MEASURES
The contributions that self-report medication adherence measures can make to health research and practice vary according to the context and purpose of their use. What is chosen for screening in clinical care will likely be different from what is chosen for assessment in a clinical trial with adherence as a primary outcome variable. Below some specialized applications and recommendations for self-report measures in different contexts are considered.
In clinical trials and research
The large number of patients and complex protocols used in many clinical trials create a need for low-cost, low-burden adherence measures. Adherence assessment may be needed at several junctures during clinical trials. At screening, measures may be needed to assess risk of nonadherence prior to randomization to allow exclusion of participants likely to have problems adhering to the protocol. At baseline, adherence assessment will allow early identification of potential problems so that study resources can be devoted to improving adherence and retention for those likely to have problems adhering. Throughout any trial, monitoring adherence can aid in determining proper drug dosages and identifying low adherence so that staff can intervene to address problems as they develop.
Self-report adherence measures are readily integrated into clinical research visits and represent a low burden assessment approach that may be more acceptable to patients than alternatives. Unique types of self-report measures may be needed at different junctures within a clinical trial. For example, single-item measures including Visual Analogue Scales (VAS) can be useful as brief adherence screens at medication management visits [97–99]. Self-report measures that can indicate reasons for nonadherence such as the Morisky adherence measure [42, 63] may be administered at baseline and during selected visits to ascertain adherence barriers to inform interventions to address and improve these challenges. If it is feasible to implement self-report measures through technologic approaches such as ACASI, this may also benefit the validity of the adherence assessments in clinical research.
In medication adherence research
Self-report measures may be disadvantageous when used as the primary outcome in clinical trials testing counseling and behavioral interventions to improve medication adherence, because intervention participants may be disproportionately influenced to self-report faithful adherence relative to comparison arm participants. The evidence for this is mixed, however. A study combining data from multiple randomized trials of HIV treatment adherence interventions found no moderation by arm of the association between self-report medication adherence and other estimates of the intervention’s effects, including biological outcomes and EDM data [100]. Further research is needed to determine whether self-report can be a valid indicator of adherence intervention effects. Until then, randomized controlled trials of adherence interventions would benefit from a more objective method of adherence assessment as the primary study outcome (e.g., EDM devices, prescription refill measures, or multiple measures with complementary properties, such as self-report and adherence biomarkers). Use of multiple measures in adherence research can triangulate intervention effects [34, 72] and advance measurement science through comparisons with one another.
In health care settings
Medication adherence is not consistently and reliably assessed as a part of routine primary and specialty healthcare. Although many clinicians believe they can accurately estimate patient adherence, research shows that clinician estimates of patient adherence are often inaccurate [101–105]. Brief, validated self-report measures of adherence therefore have an important role to play in clinical practice, and some clinical guidelines recommend routine assessment of adherence by validated self-report measures [106].
The ideal adherence assessment for clinical care involves single-item or other short self-report or measures that can be administered by the clinician, support staff, or electronic systems prior to or during the office visit. Clinician inquiries about patient adherence could help strengthen the patient-clinician alliance by conveying respect and interest in the patient’s point of view. Computer-assisted methods may enable patients to report potentially “sensitive” issues in privacy, possibly leading to greater disclosure of nonadherence and barriers to adherence. Direct integration of data from computer-based self-report measures into electronic medical records further allows results to be immediately available for use by providers to improve care, and it decreases staff burden through elimination of a data entry step that could otherwise result in delays, costs, and errors.
In recent years, electronic collection of patient-reported outcomes such as medication adherence has become more feasible with reduced costs, development of touch-screens, and more common use of computers in everyday life (e.g., bank ATM, grocery store cashier, etc.). Electronic data collection such as ACASI is less expensive than interviews [107] but associated with greater start-up costs than paper-based assessment. Despite the larger start-up costs, touch screen-based electronic collection of self-report data has been found to be less expensive per assessment in clinical settings doing six or more assessments per day [108], and continued reductions in the prices of touch-screen computers have made electronic collection even more economical over time. Touch-screen data entry eliminates the need for typing and avoids using mouse-based data entry systems that have not been universally successful [109–111]. An example of routine computer-assisted collection of self-report adherence from patients in clinical settings is provided by Feldman and colleagues [112]. More than 2300 HIV-infected patients completed touch-screen tablet-based computer assessments of a single self-rating scale item (SRSI) for medication adherence during routine clinic visits. The measure was significantly correlated with other self-report adherence items and inversely correlated with known predictors of medication nonadherence, such as illicit substance use and depression, indicating validity of the SRSI for measuring adherence. The SRSI also predicted CD4+ cell count and viral load as well or better than other adherence items, indicating good criterion validity. Findings suggest that the SRSI may be an effective, brief way to routinely measure self-report adherence in clinical settings with minimal workflow disruption and patient burden.
CONCLUSION AND PRIORITIES FOR FUTURE RESEARCH
This review indicates that self-report measures are imperfect, in that they tend to overestimate adherence compared with other assessment approaches. Self-reports of imperfect adherence can be trusted, however, and rigorously developed and well-validated self-report measures show expected relationships with both clinical outcomes and other forms of adherence assessment. A number of steps can be undertaken to strengthen the validity and precision of self-report measures of medication adherence (see Table 1). These include using well-validated scales, defining the specific adherence construct of interest, using optimized question response formats and recall periods, taking steps to address social desirability concerns, and avoiding interview-based assessments. The growing ease with which self-report measures may be administered through computer- or technology-assisted approaches also brings fresh opportunities for improved administration.
The rigorous development and testing of self-report measures of adherence should be a research priority. While numerous self-report measures are available, there is a relative dearth of measures that have been rigorously tested for convergent or criterion validity, internal consistency, and test-retest reliability. Few measures have been systematically developed for populations with self-report challenges such as impaired cognitive functioning. Research is also needed to better understand how to best assess adherence among patients taking multiple medications, particularly because many individuals have two or more chronic conditions.
Future efforts to develop self-report measures of adherence behavior would benefit from approaches such as item response theory to improve efficient and accurate assessment, as well as cognitive testing to ensure sound item understanding and comprehension [9, 70]. It is important to test the criterion validity of self-report measures through comparisons with biomarkers or clinical treatment outcomes, but caution should be used because many factors may affect this relationship, and the impact of any recent adherence behavior on biologic outcomes may lag [5, 9]. When comparisons with clinical outcomes are made, it may be helpful to test self-report alongside other adherence assessment methods, to gauge their comparative strength and concurrent/criterion validity. One example is provided by Dunbar-Jacob and colleagues [51] who examined how multiple self-report and EDM measures corresponded to cholesterol levels in a trial testing cholesterol-reducing medication strategies.
Research on self-report adherence measures is also needed to inform evidence-based strategies to further mitigate ceiling effects and social desirability concerns. Studies should build on the promising directions noted here regarding 30-day recall intervals and global adherence estimates by further testing optimized self-report question phrasing, recall periods, and response item formats. There is also a need for continued research on brief measures of medication adherence for use as a patient-reported outcome in routine clinical care, and for integration into electronic health records. Administration of self-report measures through innovative methods such as IVR and text messaging is another important direction for future research. There may be utility to text messaging or smart phone applications that allow an individual to report when they have taken their dose, or IVR applications that allow a patient to remotely record whether their medication has been taken for the day. In addition to the promise of being simple to use, these eHealth options can provide a wealth of data to better understand patterns and predictors of adherence. These applications may be particularly useful for groups with cognitive impairment who may be less accurate at reporting about behavior over longer periods of time.
Understanding and addressing adherence problems are important keys to improving health care delivery. Given the longstanding ubiquity of self-report medication adherence measures in research and practice, further research to improve and optimize these measures should provide benefits to health care and health research more generally.
References
Garfield S, Clifford S, Eliasson L, Barber N, Willson A. Suitability of measures of self-reported medication adherence for routine clinical use: a systematic review. BMC Medical Research Methodology. 2011; 11: 149.
Gonzalez JS, Schneider HE. Methodological issues in the assessment of diabetes treatment adherence. Current Diabetes Reports. 2011; 11: 472-479.
Hall KS, White KO, Reame N, Westhoff C. Studying the use of oral contraception: a review of measurement approaches. Journal of Women's Health. 2010; 19: 2203-2210.
Paschal AM, Hawley SR, St Romain T, Ablah E. Measures of adherence to epilepsy treatment: review of present practices and recommendations for future directions. Epilepsia. 2008; 49: 1115-1122.
Simoni JM, Kurth AE, Pearson CR, et al. Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS and Behavior. 2006; 10: 227-245.
Velligan DI, Lam YW, Glahn DC, et al. Defining and assessing adherence to oral antipsychotics: a review of the literature. Schizophrenia Bulletin. 2006; 32: 724-742.
Nguyen TM, Caze AL, Cottrell N. (2013) What are validated self-report adherence scales really measuring?: a systematic review. British Journal of Clinical Pharmacology
Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Medical Care. 2004; 42: 649-652.
Wilson IB, Carter AE, Berg KM. Improving the self-report of HIV antiretroviral medication adherence: is the glass half full or half empty? Current HIV/AIDS Reports. 2009; 6: 177-186.
Osterberg L, Blaschke T. Adherence to medication. The New England Journal of Medicine. 2005; 353: 487-497.
Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. British Journal of Clinical Pharmacology. 2012; 73: 691-705.
Voils CI, Hoyle RH, Thorpe CT, Maciejewski ML, Yancy WS Jr. Improving the measurement of self-reported medication nonadherence. Journal of Clinical Epidemiology. 2011; 64: 250-254.
Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. International Journal of Clinical Practice. 2008; 62: 76-87.
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Medical Care. 2002; 40: 794-811.
Granger BB, Swedberg K, Ekman I, et al. Adherence to candesartan and placebo and outcomes in chronic heart failure in the CHARM programme: double-blind, randomised, controlled clinical trial. Lancet. 2005; 366: 2005-2011.
Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007; 297: 177-186.
Simpson SH, Eurich DT, Majumdar SR, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ. 2006; 333: 15.
Asche C, LaFleur J, Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clinical Therapeutics. 2011; 33: 74-109.
Hood KK, Peterson CM, Rohan JM, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics. 2009; 124: e1171-e1179.
Riegel B, Knafl GJ. Electronically monitored medication adherence predicts hospitalization in heart failure patients. Patient Prefer Adherence. 2013; 8: 1-13.
Dragomir A, Cote R, Roy L, et al. Impact of adherence to antihypertensive agents on clinical outcomes and hospitalization costs. Medical Care. 2010; 48: 418-425.
Pladevall M, Williams LK, Potts LA, et al. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004; 27: 2800-2805.
Marin D, Bazeos A, Mahon FX, et al. Adherence is the critical factor for achieving molecular responses in patients with chronic myeloid leukemia who achieve complete cytogenetic responses on imatinib. Journal of Clinical Oncology. 2010; 28: 2381-2388.
Dragomir A, Cote R, White M, et al. Relationship between adherence level to statins, clinical issues and health-care costs in real-life clinical setting. Value in Health. 2010; 13: 87-94.
Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy. 2008; 28: 437-443.
Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004; 27: 1218-1224.
DiMatteo MR. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Medical Care. 2004; 42: 200-209.
Vink NM, Klungel OH, Stolk RP, Denig P. Comparison of various measures for assessing medication refill adherence using prescription data. Pharmacoepidemiology and Drug Safety. 2009; 18: 159-165.
Yeaw J, Benner JS, Walt JG, Sian S, Smith DB. Comparing adherence and persistence across 6 chronic medication classes. Journal of Managed Care Pharmacy. 2009; 15: 728-740.
de Klerk E, van der Heijde D, Landewe R, et al. Patient compliance in rheumatoid arthritis, polymyalgia rheumatica, and gout. Journal of Rheumatology. 2003; 30: 44-54.
Mannheimer S, Thackeray L, Huppler Hullsiek K, et al. A randomized comparison of two instruments for measuring self-reported antiretroviral adherence. AIDS Care. 2008; 20: 161-169.
Berg KM, Arnsten JH. Practical and conceptual challenges in measuring antiretroviral adherence. Journal of Acquired Immune Deficiency Syndromes. 2006; 43(Suppl 1): S79-S87.
Chesney MA. The elusive gold standard. Future perspectives for HIV adherence assessment and intervention. Journal of Acquired Immune Deficiency Syndromes. 2006; 43(Suppl 1): S149-S155.
Quittner AL, Modi AC, Lemanek KL, Ievers-Landis CE, Rapoff MA. Evidence-based assessment of adherence to medical treatments in pediatric psychology. Journal of Pediatric Psychology. 2008; 33: 916-936. discussion 937–918.
Williams AB, Amico KR, Bova C, Womack JA. A proposal for quality standards for measuring medication adherence in research. AIDS and Behavior. 2013; 17: 284-297.
Kimmerling M, Wagner G, Ghosh-Dastidar B. Factors associated with accurate self-reported adherence to HIV antiretrovirals. International Journal of STD and AIDS. 2003; 14: 281-284.
Knobel H, Alonso J, Casado JL, et al. Validation of a simplified medication adherence questionnaire in a large cohort of HIV-infected patients: the GEEMA Study. AIDS. 2002; 16: 605-613.
Wagner G. Utility of self-reported antiretroviral adherence: Comment on Simoni et al. (2006). AIDS and Behavior. 2006; 10: 247-248.
Simoni JM, Montgomery A, Martin E, et al. Adherence to antiretroviral therapy for pediatric HIV infection: a qualitative systematic review with recommendations for research and clinical management. Pediatrics. 2007; 119: e1371-e1383.
Dobbels F, Berben L, De Geest S, et al. The psychometric properties and practicability of self-report instruments to identify medication nonadherence in adult transplant patients: a systematic review. Transplantation. 2010; 90: 205-219.
Bangsberg DR. Monitoring adherence to HIV antiretroviral therapy in routine clinical practice: the past, the present, and the future. AIDS and Behavior. 2006; 10: 249-251.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. Journal of Clinical Hypertension. 2008; 10: 348-354.
Chesney MA, Ickovics JR, Chambers DB, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care. 2000; 12: 255-266.
Berg KM, Wilson IB, Li X, Arnsten JH. Comparison of antiretroviral adherence questions. AIDS and Behavior. 2012; 16: 461-468.
Greenlaw SM, Yentzer BA, O'Neill JL, Balkrishnan R, Feldman SR. Assessing adherence to dermatology treatments: a review of self-report and electronic measures. Skin Research and Technology. 2010; 16: 253-258.
Rand CS. "I Took the Medicine Like You Told Me, Doctor": Self-Report of Adherence with Medical Regimens. In: Stone AA, Turkkan JS, Bachrach CA, et al., eds. The science of self-report: Implications for research and practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2000: 257-276.
Nieuwkerk PT, Oort FJ. Self-reported adherence to antiretroviral therapy for HIV-1 infection and virologic treatment response: a meta-analysis. Journal of Acquired Immune Deficiency Syndromes. 2005; 38: 445-448.
Kahana SY, Rohan J, Allison S, Frazier TW, Drotar D. A meta-analysis of adherence to antiretroviral therapy and virologic responses in HIV-infected children, adolescents, and young adults. AIDS and Behavior. 2013; 17: 41-60.
Usitalo A, Leister E, Tassiopoulos K, et al. Relationship between viral load and self-report measures of medication adherence among youth with perinatal HIV infection. AIDS Care. 2014; 26: 107-115.
Koschack J, Marx G, Schnakenberg J, Kochen MM, Himmel W. Comparison of two self-rating instruments for medication adherence assessment in hypertension revealed insufficient psychometric properties. Journal of Clinical Epidemiology. 2010; 63: 299-306.
Dunbar-Jacob J, Sereika SM, Houze M, Luyster FS, Callan JA. Accuracy of measures of medication adherence in a cholesterol-lowering regimen. Western Journal of Nursing Research. 2012; 34: 578-597.
Voils CI, Maciejewski ML, Hoyle RH, et al. Initial validation of a self-report measure of the extent of and reasons for medication nonadherence. Medical Care. 2012; 50: 1013-1019.
Gonzalez JS, Schneider HE, Wexler DJ, et al. Validity of medication adherence self-reports in adults with type 2 diabetes. Diabetes Care. 2013; 36: 831-837.
Arnsten JH, Demas PA, Farzadegan H, et al. Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: comparison of self-report and electronic monitoring. Clinical Infectious Diseases. 2001; 33: 1417-1423.
Shi L, Liu J, Koleva Y, et al. Concordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devices. PharmacoEconomics. 2010; 28: 1097-1107.
Shi L, Liu J, Fonseca V, et al. Correlation between adherence rates measured by MEMS and self-reported questionnaires: a meta-analysis. Health and Quality of Life Outcomes. 2010; 8: 99.
Bova CA, Fennie KP, Knafl GJ, et al. Use of electronic monitoring devices to measure antiretroviral adherence: practical considerations. AIDS and Behavior. 2005; 9: 103-110.
Pearson CR, Simoni JM, Hoff P, Kurth AE, Martin DP. Assessing antiretroviral adherence via electronic drug monitoring and self-report: an examination of key methodological issues. AIDS Behavior. 2006.
Sajatovic M, Velligan DI, Weiden PJ, Valenstein MA, Ogedegbe G. Measurement of psychiatric treatment adherence. Journal of Psychosomatic Research. 2010; 69: 591-599.
Steiner JF. Self-reported adherence measures: what do they assess and how should we use them? Medical Care. 2012; 50: 1011-1012.
Voils CI, Hoyle RH, Thorpe CT, Maciejewski ML, Yancy WS Jr. Response to Morisky & DiMatteo: Improving the measurement of self-reported medication nonadherence. Journal of Clinical Epidemiology. 2011; 64: 250-254.
Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy Scale. Progress in Cardiovascular Nursing. 2000; 15: 90-96.
Krousel-Wood M, Islam T, Webber LS, et al. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. The American Journal of Managed Care. 2009; 15: 59-66.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986; 24: 67-74.
Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Correlates of nonadherence to hypertension treatment in an inner-city minority population. American Journal of Public Health. 1992; 82: 1607-1612.
Svarstad BL, Chewning BA, Sleath BL, Claesson C. The Brief Medication Questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Education and Counseling. 1999; 37: 113-124.
Steiner JF. Rethinking adherence. Annals of Internal Medicine. 2012; 157: 580-585.
Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS and Behavior. 2013; 17: 307-318.
Lu M, Safren SA, Skolnik PR, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS and Behavior. 2008; 12: 86-94.
Wilson IB, Fowler FJ, Jr., Cosenza CA, et al. (2013) Cognitive and Field Testing of a New Set of Medication Adherence Self-Report Items for HIV Care. AIDS Behavior.
Nieuwkerk PT, de Boer-van der Kolk IM, Prins JM, Locadia M, Sprangers MA. Self-reported adherence is more predictive of virological treatment response among patients with a lower tendency towards socially desirable responding. Antivir Ther. 2010; 15: 913-916.
Velligan DI, Weiden PJ, Sajatovic M, et al. Assessment of adherence problems in patients with serious and persistent mental illness: recommendations from the Expert Consensus Guidelines. Journal of Psychiatric Practice. 2010; 16: 34-45.
Tourangeau R, Smith TW. Asking sensitive questions: the impact of data collection mode, question format, and question context. Public Opinion Quarterly. 1996; 2: 275-304.
Islam MM, Topp L, Conigrave KM, et al. The reliability of sensitive information provided by injecting drug users in a clinical setting: clinician-administered versus audio computer-assisted self-interviewing (ACASI). AIDS Care. 2012; 24: 1496-1503.
Newman JC, Des Jarlais DC, Turner CF, et al. The differential effects of face-to-face and computer interview modes. American Journal of Public Health. 2002; 92: 294-297.
Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999; 353: 1657-1661.
Kissinger P, Rice J, Farley T, et al. Application of computer-assisted interviews to sexual behavior research. American Journal of Epidemiology. 1999; 149: 950-954.
Locke SE, Kowaloff HB, Hoff RG, et al. Computer-based interview for screening blood donors for risk of HIV transmission. JAMA. 1992; 268: 1301-1305.
Sanders GD, Owens DK, Padian N, et al. A computer-based interview to identify HIV risk behaviors and to assess patient preferences for HIV-related health states. Proceedings of the Annual Symposium on Computer Applications in Medical Care. 1994:20–24.
Wilson AS, Kitas GD, Carruthers DM, et al. Computerized information-gathering in specialist rheumatology clinics: an initial evaluation of an electronic version of the Short Form 36. Rheumatology (Oxford). 2002; 41: 268-273.
Velikova G, Wright EP, Smith AB, et al. Automated collection of quality-of-life data: a comparison of paper and computer touch-screen questionnaires. Journal of Clinical Oncology. 1999; 17: 998-1007.
Aiello EJ, Taplin S, Reid R, et al. In a randomized controlled trial, patients preferred electronic data collection of breast cancer risk-factor information in a mammography setting. Journal of Clinical Epidemiology. 2006; 59: 77-81.
Chinman M, Young AS, Schell T, Hassell J, Mintz J. Computer-assisted self-assessment in persons with severe mental illness. Journal of Clinical Psychiatry. 2004; 65: 1343-1351.
Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004; 99: 885-896.
Kurth AE, Martin DP, Golden MR, et al. A comparison between audio computer-assisted self-interviews and clinician interviews for obtaining the sexual history. Sexually Transmitted Diseases. 2004; 31: 719-726.
Metzger DS, Koblin B, Turner C, et al. Randomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol Team. American Journal of Epidemiology. 2000; 152: 99-106.
Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sexually Transmitted Infections. 2005; 81: 421-425.
Hanscom B, Lurie JD, Homa K, Weinstein JN. Computerized questionnaires and the quality of survey data. Spine. 2002; 27: 1797-1801.
Bock B, Niaura R, Fontes A, Bock F. Acceptability of computer assessments among ethnically diverse, low-income smokers. American Journal of Health Promotion. 1999; 13: 299-304.
Castle T, Cunningham MA, Marsh GM. Antidepressant medication adherence via interactive voice response telephone calls. The American Journal of Managed Care. 2012; 18: e346-e355.
Vollmer WM, Feldstein A, Smith DH, et al. Use of health information technology to improve medication adherence. The American Journal of Managed Care. 2011; 17: SP79-SP87.
Hettema JE, Hosseinbor S, Ingersoll KS. Feasibility and reliability of interactive voice response assessment of HIV medication adherence: research and clinical implications. HIV Clin Trials. 2012; 13: 271-277.
Harris LT, Lehavot K, Huh D, et al. Two-way text messaging for health behavior change among human immunodeficiency virus-positive individuals. Telemed J E Health. 2010; 16: 1024-1029.
Granholm E, Ben-Zeev D, Link PC, Bradshaw KR, Holden JL. Mobile assessment and treatment for schizophrenia (MATS): a pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophrenia Bulletin. 2012; 38: 414-425.
Dowshen N, Kuhns LM, Johnson A, Holoyda BJ, Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. Journal of Medical Internet Research. 2012; 14: e51.
Bender BG, Bartlett SJ, Rand CS, et al. Impact of interview mode on accuracy of child and parent report of adherence with asthma-controller medication. Pediatrics. 2007; 120: e471-e477.
Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsberg DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clinical Trials. 2004; 5: 74-79.
Kalichman SC, Amaral CM, Swetzes C, et al. A simple single-item rating scale to measure medication adherence: further evidence for convergent validity. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill). 2009; 8: 367-374.
Walsh JC, Dalton M, Gazzard BG. Adherence to combination antiretroviral therapy assessed by anonymous patient self-report. AIDS. 1998; 12: 2361-2363.
Simoni J, Huh D, Wang Y, et al. The validity of self-reported medication adherence as an outcome in clinical trials of adherence-promotion interventions: findings from the MACH14 study. AIDS Behav. 2014; 18: 2285-2290.
Bangsberg DR, Hecht FM, Clague H, et al. Provider assessment of adherence to HIV antiretroviral therapy. Journal of Acquired Immune Deficiency Syndromes. 2001; 26: 435-442.
Byerly M, Fisher R, Whatley K, et al. A comparison of electronic monitoring vs. clinician rating of antipsychotic adherence in outpatients with schizophrenia. Psychiatry Research. 2005; 133: 129-133.
Miller LG, Liu H, Hays RD, et al. How well do clinicians estimate patients' adherence to combination antiretroviral therapy? Journal of General Internal Medicine. 2002; 17: 1-11.
Ose D, Mahler C, Vogel I, et al. Let's talk about medication: concordance in rating medication adherence among multimorbid patients and their general practitioners. Patient Prefer Adherence. 2012; 6: 839-845.
Velligan DI, Wang M, Diamond P, et al. Relationships among subjective and objective measures of adherence to oral antipsychotic medications. Psychiatric Services. 2007; 58: 1187-1192.
Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Annals of Internal Medicine. 2012; 156: 817-833.
Wolford G, Rosenberg SD, Rosenberg HJ, et al. A clinical trial comparing interviewer and computer-assisted assessment among clients with severe mental illness. Psychiatric Services. 2008; 59: 769-775.
Lofland JH, Schaffer M, Goldfarb N. Evaluating health-related quality of life: cost comparison of computerized touch-screen technology and traditional paper systems. Pharmacotherapy. 2000; 20: 1390-1395.
Williams CA, Templin T, Mosley-Williams AD. Usability of a computer-assisted interview system for the unaided self-entry of patient data in an urban rheumatology clinic. Journal of the American Medical Informatics Association. 2004; 11: 249-259.
Smith MW, Sharit J, Czaja SJ. Aging, motor control, and the performance of computer mouse tasks. Human Factors. 1999; 41: 389-396.
Kim J, Trace D, Meyers K, Evens M. An empirical study of the Health Status Questionnaire System for use in patient-computer interaction. Proceedings AMIA Annual Fall Symptom. 1997:86–90.
Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behavior. 2012.
Erickson SR, Coombs JH, Kirking DM, Azimi AR. Compliance from self-reported versus pharmacy claims data with metered-dose inhalers. Annals of Pharmacotherapy. 2001; 35: 997-1003.
Duncan NA, Kronenberger WG, Roberson CP, Shapiro AD. VERITAS-PRN: a new measure of adherence to episodic treatment regimens in haemophilia. Haemophilia. 2010; 16: 47-53.
Reynolds NR, Sun J, Nagaraja HN, et al. Optimizing measurement of self-reported adherence with the ACTG Adherence Questionnaire: a cross-protocol analysis. Journal of Acquired Immune Deficiency Syndromes. 2007; 46: 402-409.
Munoz-Moreno JA, Fumaz CR, Ferrer MJ, et al. Assessing self-reported adherence to HIV therapy by questionnaire: the SERAD (Self-Reported Adherence) Study. AIDS Research and Human Retroviruses. 2007; 23: 1166-1175.
Godin G, Gagne C, Naccache H. Validation of a self-reported questionnaire assessing adherence to antiretroviral medication. AIDS Patient Care and STDs. 2003; 17: 325-332.
Amico KR, Fisher WA, Cornman DH, et al. Visual analog scale of ART adherence: association with 3-day self-report and adherence barriers. Journal of Acquired Immune Deficiency Syndromes. 2006; 42: 455-459.
Schroeder K, Fahey T, Hay AD, Montgomery A, Peters TJ. Adherence to antihypertensive medication assessed by self-report was associated with electronic monitoring compliance. Journal of Clinical Epidemiology. 2006; 59: 650-651.
Zeller A, Schroeder K, Peters TJ. An adherence self-report questionnaire facilitated the differentiation between nonadherence and nonresponse to antihypertensive treatment. Journal of Clinical Epidemiology. 2008; 61: 282-288.
Frazier PA, Davis-Ali SH, Dahl KE. Correlates of noncompliance among renal transplant recipients. Clinical Transplantation. 1994; 8: 550-557.
Tucker CM, Petersen S, Herman KC, et al. Self-regulation predictors of medication adherence among ethnically different pediatric patients with renal transplants. Journal of Pediatric Psychology. 2001; 26: 455-464.
Chisholm MA, Lance CE, Williamson GM, Mulloy LL. Development and validation of the immunosuppressant therapy adherence instrument (ITAS). Patient Education and Counseling. 2005; 59: 13-20.
Cukor D, Rosenthal DS, Jindal RM, Brown CD, Kimmel PL. Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients. Kidney International. 2009; 75: 1223-1229.
Byerly MJ, Nakonezny PA, Rush AJ. The Brief Adherence Rating Scale (BARS) validated against electronic monitoring in assessing the antipsychotic medication adherence of outpatients with schizophrenia and schizoaffective disorder. Schizophrenia Research. 2008; 100: 60-69.
Scott J, Pope M. Self-reported adherence to treatment with mood stabilizers, plasma levels, and psychiatric hospitalization. The American Journal of Psychiatry. 2002; 159: 1927-1929.
Wicks P, Massagli M, Kulkarni A, Dastani H. Use of an online community to develop patient-reported outcome instruments: the Multiple Sclerosis Treatment Adherence Questionnaire (MS-TAQ). Journal of Medical Internet Research. 2011; 13, e12.
Breuil V, Cortet B, Cotte FE, et al. Validation of the adherence evaluation of osteoporosis treatment (ADEOS) questionnaire for osteoporotic post-menopausal women. Osteoporosis International. 2012; 23: 445-455.
de Klerk E, van der Heijde D, van der Tempel H, van der Linden S. Development of a questionnaire to investigate patient compliance with antirheumatic drug therapy. Journal of Rheumatology. 1999; 26: 2635-2641.
McHorney CA, Victor Spain C, Alexander CM, Simmons J. Validity of the adherence estimator in the prediction of 9-month persistence with medications prescribed for chronic diseases: a prospective analysis of data from pharmacy claims. Clinical Therapeutics. 2009; 31: 2584-2607.
Kripalani S, Risser J, Gatti ME, Jacobson TA. Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low-literacy patients with chronic disease. Value in Health. 2009; 12: 118-123.
DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians' characteristics influence patients' adherence to medical treatment: results from the Medical Outcomes Study. Health Psychology. 1993; 12: 93-102.
Wu JR, Chung M, Lennie TA, Hall LA, Moser DK. Testing the psychometric properties of the Medication Adherence Scale in patients with heart failure. Heart and Lung. 2008; 37: 334-343.
Orwig D, Brandt N, Gruber-Baldini AL. Medication management assessment for older adults in the community. Gerontologist. 2006; 46: 661-668.
Zelikovsky N, Schast AP. Eliciting accurate reports of adherence in a clinical interview: development of the Medical Adherence Measure. Pediatric Nursing. 2008; 34: 141-146.
Acknowledgments
The paper is based in part on an NIH Adherence Network meeting on “Advancing the Science of Adherence Assessment: A Working Meeting on Self-Report Measures,” sponsored by the NIH Office of Behavioral and Social Sciences (OBSSR) and held 17 October 2011. We are grateful to Shoshana Kahana for her contributions, to Janet de Moor, Martha Hare, Donna McCloskey, and Anne Trontell for their paper feedback, and to all members of the NIH Adherence Network for their support.
Source of funding
This paper was supported by the National Institutes of Health (NIH) Office of Behavioral and Social Sciences Research (OBSSR) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) through award number U01AR057954 (Crane). Additional support was provided through National Institute of Nursing Research (NINR) grant PO1NR010949 (Dunbar-Jacob), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant K12DK097696 (Hilliard), National Heart, Lung, and Blood Institute (NHLBI) grant K24HL111315 (Ogedegbe), and National Institute of Mental Health (NIMH) grants K24MH093243 (Simoni) and R01MH084759 (Crane). Further support (for Simoni and Crane) was provided by the University of Washington Center for AIDS Research (CFAR), an NIH-funded centers program (P30AI27757) which is collaboratively supported by NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, and NIA.
Authors’ statement of conflict of interest and adherence to ethical standards
The authors declare that they have no conflict of interest. All procedures were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Disclaimer
The views expressed in this article are those of the authors and should not be interpreted as the official recommendations or policy of the NIH, its constituent institutes, or other author-affiliated organizations.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Practice: Routine assessment of medication adherence in clinical settings through brief, validated self-report measures can provide actionable information to medical providers about patient nonadherence.
Policy: Clinical guidelines should recommend routine assessment of medication adherence in clinical settings through validated self-report measures, and healthcare policies should support integration of this patient-reported outcome into electronic health records.
Research: The validity of self-report adherence measures may be enhanced through efforts to use validated scales, assess the proper construct, improve estimation, facilitate recall, reduce social desirability bias, and employ technologic delivery; further research to strengthen self-report adherence measures is needed.
Appendix
Appendix
About this article
Cite this article
Stirratt, M.J., Dunbar-Jacob, J., Crane, H.M. et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Behav. Med. Pract. Policy Res. 5, 470–482 (2015). https://doi.org/10.1007/s13142-015-0315-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-015-0315-2