Abstract
Chronic thromboembolic pulmonary hypertension (CTEPH), which is classified as a group 4 pulmonary hypertension (PH), is a life-threatening complication of acute pulmonary embolism (PE). With the introduction of multidisciplinary approaches and innovative treatment strategies for CTEPH, it is currently regarded not as a fatal disease, but as a curable form of PH. Ventilation/perfusion (V/Q) scan is the preferred imaging method for screening for CTEPH, with superior sensitivity to CT pulmonary angiography. The findings and interpretations of V/Q scan in CTEPH may differ from those observed in acute PE. The use of V/Q scan in combination with SPECT or SPECT/CT is becoming more popular than planar scan alone. Comprehensive understanding of the role of V/Q scan in CTEPH will assist in providing early diagnosis, proper therapeutic decision making, and improved prognosis. This review outlines the current roles and potential clinical applications of V/Q scan in the diagnosis and evaluation of CTEPH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic thromboembolic pulmonary hypertension (CTEPH) falls under the World Health Organization (WHO) group IV category of pulmonary hypertension (PH) and is considered to be surgically curable [1]. CTEPH is generally regarded as a relatively long-term complication of acute pulmonary embolism (PE), with an estimated occurrence rate of 1%–5% in acute PE survivors [2]. A prospective long-term follow-up study reported cumulative incidences of CTEPH of 1.0% at 6 months, 3.1% at 1 year, and 3.8% at 2 years [3]; however, the rates differed across the studies, with variation being attributed to referral bias, scarcity of early symptoms, and challenges differentiating acute PE from chronic PE [4]. Low clinical awareness and a relatively long “honeymoon” period cause frequent misdiagnosis of CTEPH. In Western countries, it is estimated that only 7–29% of CTEPH cases are diagnosed, with the majority presenting in the New York Heart Association functional class III/IV at the time of diagnosis [4], suggesting that CTEPH remains significantly underdiagnosed and inadequately treated.
CTEPH is associated with several risk factors and predisposing conditions. The risk factors for CTEPH can be delineated into two distinct categories: (1) those associated with the acute phase, which pertains to the initial episode of PE; and (2) those that are more prevalent in the chronic phase of CTEPH and show a higher incidence in CTEPH patients than in idiopathic pulmonary arterial hypertension (IPAH) patients [5]. Unprovoked PE, a diagnostic delay of more than 2 weeks after the onset of symptoms, and right ventricular dysfunction during acute PE are pivotal risk factors for CTEPH. In addition, several medical conditions are more represented in CTEPH than in IPAH, including hemostatic risk factors such as antiphospholipid antibodies and lupus anticoagulants, and other associated medical conditions such as malignancy, hypothyroidism, ventriculo-atrial shunts, and chronic inflammatory disorder [6]. However, further research is needed to fully understand the mechanisms underlying the development of CTEPH.
Pathophysiology of CTEPH
The precise pathogenesis of CTEPH remains unclear. In general, CTEPH is believed to develop after a single or multiple episodes of acute PE, which mostly originate from deep vein thrombosis [7]. Information from a European international CTEPH registry revealed that 75% of CTEPH patients had a recorded history of acute PE, while 56% had prior deep vein thrombosis [8]. Of note, incomplete resolution of acute PE is not uncommon. After an initial episode of acute PE, the resolution of emboli begins within hours and continues progressively, plateauing at around 3–6 months with minimal improvement observed thereafter. One study reported that incomplete resolution of PE can be observed on V/Q scan in approximately two-thirds of patients, despite the use of anticoagulation treatment [9]. This is the basis of the current European Society of Cardiology (ESC) guidelines recommending a follow-up ventilation/perfusion (V/Q) scan at 3–6 months after diagnosis of acute PE in patients having residual dyspnea or functional limitation [10].
The organization and fibrotic transformation of intraluminal thrombus is a pathologic hallmark of CTEPH. A residual organized clot adhering to the pulmonary artery wall causes a fixed mechanical obstruction. This obstruction induces microvascular remodeling and a gradual increase in pulmonary vascular resistance (PVR), eventually leading to right heart failure [11]. Pathological specimens from patients with acute PE show fresh red clots that consist mainly of red blood cells and platelets and that are easily detached from the vascular wall. In contrast, the chronic yellowish clots present in CTEPH consist of elastin, collagen, inflammatory cells, and re-canalized vessels [7].
Besides the mechanical obstruction resulting from organized fibrotic clots, there is growing evidence that pulmonary microvasculopathy, often referred to as “small vessel” disease, plays a significant role in the development of CTEPH. Pulmonary microvasculopathy encompasses factors like pulmonary vascular remodeling and intimal fibromuscular proliferation, which show similarities to IPAH [12]. This remodeling of the pulmonary arterial vasculature results in altered pulmonary flow distribution, augmented shear stress on non-occluded pulmonary arteries, a gradual rise in PVR, and eventual manifestation of symptomatic CTEPH. The molecular mechanism of this microvasculopathy involves the prostacyclin, nitric oxide, and endothelin pathways, which are targets for medical therapy for both idiopathic PAH and CTEPH [13, 14]. In situ thrombosis in the distal pulmonary artery as a result of “small vessel” disease can also develop into CTEPH. Indeed, around 25% of CTEPH patients lack a documented history of acute PE.
Diagnostic Work-up
CTEPH should be considered in all individuals suspected of having PH, as it has a distinct management strategy. CTEPH is diagnosed on the basis of (1) hemodynamic evidence of PH; (2) one or more large V/Q mismatched perfusion defects on lung scan; and (3) specific evidence of PE on invasive pulmonary angiography or CT/MR angiography [15]. The previous ESC/European Respiratory Society (ERS) guidelines from 2015 defined PH as a mean pulmonary arterial pressure (mPAP) > 25 mmHg [16], but the recent ESC/ERS guidelines redefine it as a mPAP > 20 mmHg [17]. The definition of precapillary PH should include a PVR of > 2 Wood Units and a pulmonary arterial wedge pressure of ≤ 15 mmHg. Patients must be anticoagulated for more than 3 months before being diagnosed with CTEPH.
A diagnostic algorithm for CTEPH is shown in Fig. 1. The clinical manifestations of CTEPH often present as vague symptoms and signs indicative of PH, including fatigue, dyspnea on exertion, hemoptysis, syncope, and in more advanced cases, right heart failure. In such patients, echocardiography serves as the initial diagnostic modality for evaluating the likelihood of PH [16, 17]. The diagnostic evaluations include estimation of the peak tricuspid regurgitation velocity and examination for other indirect signs of PH suggestive of right ventricular dilatation and reduced right ventricular contractility. If echocardiography shows a high or intermediate probability of PH, chest plain radiography, pulmonary function test, and electrocardiography are typically requested to assess possible airway or parenchymal lung disease or other cardiac disorders, to distinguish between group 2 (attributed to left heart disease) and group 3 (associated with lung disease) PH. If left-side heart or lung disease diagnoses are not established, V/Q scintigraphy should be conducted for the differential diagnosis between CTEPH and PAH. If V/Q mismatched perfusion defects are shown on V/Q scan, CTEPH (group 4 PH) should be suspected. A conclusive diagnosis of CTEPH is ascertained through right heart catheterization and selective pulmonary angiography. While these latter two methods continue to be the standard methods for diagnosing CTEPH, CT pulmonary angiography can sometimes be utilized for confirmation. However, it is worth noting that CT pulmonary angiography can lead to false-negative outcomes in approximately 25% of cases [18].
Diagnostic Performance of V/Q Scintigraphy
A V/Q lung scan is recommended as a pivotal screening test in all patients with PH who are suspected of CTEPH. The interpretation of V/Q scan results is typically clear-cut for patients specifically evaluated for CTEPH. The reported sensitivities range from 90 to 100%, while specificities range from 94 to 100% [18]. The majority of CTEPH patients exhibit markedly abnormal V/Q scan results, characterized by several extensive perfusion defects without corresponding ventilation defects. According to the modified PIOPED II criteria, such findings can be conclusively categorized as indicating a high likelihood of PE. In contrast to acute PE, the size of perfusion defects in CTEPH may decrease over time [19]. Therefore, an intermediate probability V/Q scan should be considered as a positive case to increase diagnostic sensitivity, albeit at decreased specificity. A low-probability V/Q scan may reliably exclude CTEPH, with a negative predictive value reaching 100% [18]. Therefore, one or more segmental or large V/Q mismatched perfusion defects form a diagnostic criterion for CTEPH on V/Q scan [20, 21].
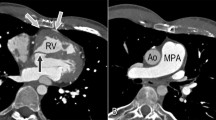
Typical CTEPH demonstrates multiple segmental wedge-shaped perfusion defects, although such findings can also appear in PH due to non-thromboembolic causes. Non-thromboembolic lesions involving pulmonary arteries, such as angiosarcoma, pulmonary vasculitis, fibrosing mediastinitis, and congenital pulmonary vascular abnormalities, can cause large mismatched perfusion defects [22,23,24,25]. Unilateral hypoperfusion or absent perfusion involving nearly the entire lung without V/Q mismatched defect in the contralateral lung is not likely to be a result of PE (Fig. 2). In PAH, a V/Q lung scan may be normal apart from small subsegmental or nonsegmental defects, a so-called “mottled” or “moth-eaten” pattern.
Imaging findings in a 36-year-old man who experienced dyspnea for 8 years a. V/Q SPECT/CT indicates V/Q mismatched defects throughout the entire right lung, whereas the left lung appears normal. CT scan exhibits severe narrowing and wall thickening of the right main pulmonary artery consistent with Takayasu arteritis involvement (red arrow). A 55-year-old woman who presented with a history of acute pulmonary embolism 5 months previous b. V/Q scintigraphy reveals V/Q mismatched hypoperfusion almost entirely within the left lung with other multiple V/Q mismatched defects in the contralateral lung (blue arrows). CT images show multifocal low attenuation filling defects in both pulmonary arteries (yellow arrows), supporting the diagnosis of chronic PE
The sensitivity of CT pulmonary angiography for CTEPH was reported to be only around 50% [26], but recent advances in CT technology have enhanced this value. The CT findings of CTEPH are distinguishable from those of acute PE: acute PE often manifests as a central or saddle thrombus situated within the main pulmonary arteries or their major branches, whereas in contrast, CTEPH is more likely to involve eccentric thrombi that are located peripherally within the pulmonary arteries and their branches. CTEPH is associated with chronic thrombotic occlusions that have organized and re-canalized, resulting in features like vessel wall thickening, webs, bands, and collateral vessel formation [16]. Moreover, CTEPH can show vascular remodeling, including hypertrophy of the pulmonary arterial tree and pruning of distal vessels. Although V/Q scan is the preferred screening method for CTEPH because of its superior sensitivity compared with CT pulmonary angiography, many centers still favor CT because of its widespread availability. Therefore, despite its efficacy, the V/Q scan is still underutilized. According to data from the Pulmonary Arterial Hypertension-Quality Enhancement Research Initiative (PAH-QuERI) registry, only 57% of patients with PAH underwent a V/Q scan for CTEPH exclusion [27].
Use of SPECT or SPECT/CT for Diagnosing CTEPH
The planar V/Q scan has a well-known pitfall, so-called “shine-through masking,” which occurs because of an overlap between an area of normal perfusion and an area of perfusion defect. SPECT or SPECT/CT can identify perfusion defects that are obscured on planar imaging, thereby reducing the underestimation of defect lesion. In this manner, V/Q SPECT is considered superior to planar scan and is noted as the modality of choice in the recent ESC/ERS guidelines for PH work-up [17]. V/Q SPECT demonstrates superior diagnostic performance to planar imaging, resulting in a decrease in non-diagnostic interpretations [28, 29]. However, a recent prospective study reported similar per-patient diagnostic accuracy between V/Q SPECT and planar scan in patients with CTEPH [30]. This result may be attributed to the fact that most CTEPH patients present with multiple large perfusion defects that can be readily diagnosed on planar images. Regarding per-segment diagnosis, SPECT shows higher sensitivity than planar scan in the detection of segmental defect [30, 31]. By contrast, in patients with group 1 PH, the likelihood of obtaining a false-positive result can increase when SPECT is used because the “mottled” or “moth-eaten” patchy defects of group 1 PH may lead to misdiagnosis as CTEPH [31].
While V/Q scintigraphy is preferred as a screening test, some institutions substitute ventilation scans with low-dose chest CT. In the setting of acute PE, the omission of ventilation scans is associated with false-positive interpretation of lung scan [32]. This phenomenon could occur during the early stages of obstructive airway diseases when the vasoconstriction is detectable by ventilation scans but not by CT scans [33]. Wang et al. reported that for diagnosing CTEPH, perfusion SPECT and low-dose CT combined showed similar sensitivity and specificity to V/Q scans [30]. However, firm evidence is still lacking, specifically for the diagnosis of CTEPH. Therefore, a conservative approach for the replacement of the ventilation scan by CT may be required, extrapolating the diagnostic performance of perfusion-only SPECT with low-dose CT in the setting of acute PE (Fig. 3).
A representative case showing the diagnostic challenges posed when substituting the ventilation scan with CT, and the risk of a false-positive interpretation of the perfusion scan that can lead to a misdiagnosis of CTEPH. A 31-year-old woman was finally diagnosed with idiopathic pulmonary hypertension. V/Q planar scintigraphy shows a large V/Q-matched defect in the apicoposterior segment of the left upper lobe (blue arrows) and a moderate V/Q-matched defect in the superior segment of the left lower lobe (red arrow) a. The three-dimensional orthogonal views of SPECT (upper panel) identify a substantial perfusion defect in the apicoposterior segment of the left upper lobe (blue arrow), but there’s no corresponding abnormality evident on the CT (middle panel) b. Fusion SPECT/CT images are shown in the lower panel
It was observed that the extent of perfusion defects on V/Q scans does not directly correlate with the severity of CTEPH. Interestingly, the prominence of these defects tends to decrease as hemodynamic compromise intensifies over time [19, 34]. Owing to their superior ability to delineate perfusion defects, SPECT and SPECT/CT are particularly effective for quantifying the extent of PE [35]. Derlin et al. [36] proposed three possible methods for using SPECT/CT to quantitatively measure the extent of perfusion defect: (1) a semi-quantitative perfusion defect score, translating the visual interpretation of each pulmonary segment into a score of 1 for segmental defect and 0.5 for subsegmental defect; (2) a perfusion lung volume map delineated using thresholds of a certain percentage of the maximal perfusion value; and (3) the perfusion lung volume divided by the CT lung volume, represented as a percentage of total lung parenchyma. All these measures showed good correlations with mPAP [36, 37]. The proposed quantitative imaging parameters of lung perfusion scintigraphy for CTEPH are summarized in Table 1.
Treatment of CTEPH
The management plan for CTEPH should incorporate a comprehensive strategy combining medical therapy, pulmonary endarterectomy (PEA), and balloon pulmonary angioplasty (BPA). Even in the absence of evidence from randomized controlled trials (RCTs), long-term anticoagulation is typically prescribed to prevent recurrent thromboembolism [17].
Surgical Treatment
Although PEA is the acknowledged treatment of choice for CTEPH when dealing with accessible lesions, about 10–50% of referred patients do not qualify for this procedure [8]. Unlike surgical embolectomy for acute PE, PEA requires a true bilateral endarterectomy that reaches both segmental and subsegmental levels, with access through the walls of the pulmonary arteries under deep hypothermic circulatory arrest, without a requirement for antegrade or retrograde cerebral perfusion [38]. Surgical eligibility depends on the proximity of thromboembolic lesions, the degree of obstruction, comorbidities, and the experience of the surgical team. In centers with a wealth of experience, resections can be conducted down to segmental and subsegmental levels. Conversely, resection may be restricted to main and lobar vessel lesions in centers with less experience.
PEA may improve the values of hemodynamic parameters such as PVR or mPAP, functional status, quality of life, and survival [39, 40]. As a result of enhanced management strategies for cardiac and pulmonary complications, the peri-operative mortality rate of PEA is currently below 2.5% at experienced surgical centers [41]. Severe reperfusion edema can lead to respiratory failure, and postoperative extracorporeal membrane oxygenation is required as standard practice for severe cases [42]. Long-term outcomes showed estimated survival at 1, 2, and 3 years of 93%, 91%, and 89%, respectively, for patients who underwent PEA, compared with 88%, 79%, and 79% for those who did not [43].
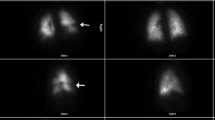
V/Q scintigraphy after PEA may show hyperperfusion, even after the resolution of the edema (Fig. 4). PEA causes preferential perfusion redistribution to the area with low vascular resistance resulting from the long-term adaptive change to previous obstruction. Segments that were previously normal might present as photopenic compared with reperfused segments, a phenomenon attributed to “vascular steal” [44]. This steal phenomenon usually resolves within 9–12 months in the majority of patients [45]. Immediate postoperative V/Q scintigraphy serves as a baseline examination for monitoring subsequent improvement and for detecting new thromboembolic events on follow-up assessments.
A vascular steal phenomenon after pulmonary endarterectomy in a 49-year-old woman who was diagnosed with CTEPH. a Initial V/Q scintigraphy shows large perfusion defects in nearly the entire right lung. b Follow-up V/Q scintigraphy after pulmonary endarterectomy shows significantly improved perfusion of the right lung and relatively decreased perfusion in the left lung
Medical Treatment
Several PAH-targeted medications, recommended on the basis of RCT studies or used off-label, have been used to treat microvasculopathy in CTEPH. Riociguat, which functions as a soluble guanylate cyclase stimulator, activates the nitric oxide pathway. This process results in the generation of cyclic guanosine monophosphate (cGMP) and impedes calcium influx, inducing vasodilation [14]. On the basis of the evidence from the CHEST-1 trial, riociguat has received FDA approval for use in inoperable cases or persistent/recurrent CTEPH post-PEA [46]. Riociguat significantly improved the 6-min walking distance (6MWD) and WHO functional class and reduced PVR by 31% relative to placebo after 16 weeks of treatment. Furthermore, a long-term extension study (CHEST-2 trial) reported that the efficacy persisted to 1 year [47].
Treprostinil, which targets the prostacyclin pathway, has proven effective in the management of PAH. In a 24-week-duration phase-3 RCT, subcutaneous treprostinil given at a high dose demonstrated an enhancement in 6MWD among patients with inoperable CTEPH or those with persistent or recurrent PH post-PEA in comparison with treprostinil administered at a lower dose [48]. Macitentan, an endothelin receptor antagonist, was investigated in a phase 2 RCT (MERIT-1) and exhibited a significant improvement in PVR in patients with inoperable CTEPH [49]. Other drugs, including sildenafil (phosphodiesterase 5 inhibitor) and bosentan (endothelin receptor antagonist), are commonly used off-label for CTEPH with severe hemodynamic compromise. To our knowledge, there is no currently available literature reporting an improvement in V/Q scans following the administration of the aforementioned drugs. Future studies are warranted to address this issue.
Interventional Treatment
The recent ESC/ERS guidelines now categorize BPA as a class I recommendation in patients with inoperable or persistent/recurrent CTEPH after PEA [17], and as many as 40% of patients with CTEPH are not considered suitable candidates for PEA [8]. BPA is unable to eliminate intravascular scars and may not be feasible if segmental arteries are entirely obstructed at the orifice [50]. A multicenter Japanese registry showed decreased mPAP, improved 6MWD, and reduced B-type natriuretic peptide levels after BPA [51]. Although the complication rates were high, including hemoptysis, lung injury, and pulmonary artery perforation, the outcomes were comparable with those of PEA, with overall survival rates of 96.8% at both 1 and 2 years and 94.5% at 3 years [51].
Pretreatment V/Q scintigraphy can help identify target vascular territories and assess thromboembolic disease severity. Although treatment often focuses on lower lobe vessels, it is imperative to image and treat all lung segments to optimize the benefits of the procedure. Generally, the lobe with the largest defect in lung perfusion scintigraphy is prioritized for treatment [52]. SPECT may provide additional information for selecting the optimal target vessel [53].
A staged approach that treats a limited number of BPA segments in each session is usually preferred. A complete treatment usually requires 4–6 separate sessions of BPA to allow remodeling to achieve the maximal hemodynamic effect [6]. Intermittent non-invasive perfusion scintigraphy is repeated to monitor perfusion changes in target regions in reference to the baseline scan. These changes generally show improvement with subsequent interventions. Therefore, perfusion SPECT or SPECT/CT may provide additional information over the planar scan for response evaluation and the optimal selection of target vessels for subsequent intervention (Fig. 5) [18]. In addition, a V/Q scan [54] or perfusion SPECT/CT without a ventilation scan [37] has demonstrated the effectiveness of BPA treatment by estimating the perfused lung volume and, in turn, the proportion of perfusion defects. Of note, the impact of ventilation scans on assessing the response to BPA by follow-up lung scans or SPECT/CT has not yet been studied. However, we speculate that incorporating a ventilation scan might not be crucial for diagnostic purposes, considering that response monitoring is primarily aimed at assessing the changes that have occurred since the initial perfusion scan.
A 79-year-old woman who was diagnosed with CTEPH 2 months prior. a The initial SPECT/CT imaging reveals large V/Q-mismatched perfusion defects in the right lung and the left lower lobe (LLL). Staged BPA was performed with the first session targeting the right upper lobe, right middle lobe, and right lower lobe, and the second BPA targeting both lower lobes. b Six months after the initial imaging, follow-up V/Q SPECT/CT demonstrates improved perfusion in the right lung (blue arrows) and LLL (red arrows)
Conclusions
The lung V/Q scan is recommended as a screening test of choice for all patients with unexplained PH. One or more large segmental V/Q mismatched defects should support further work-up for CTEPH. Various non-thromboembolic factors can mimic such image findings, and therefore nuclear medicine physicians should be aware that such an atypical distribution is distinct from the typical scintigraphic appearance of CTEPH. Management of CTEPH should be performed by a specialized multidisciplinary team with evolving therapeutic options. A V/Q scan, preferably with SPECT, may provide comprehensive information on a thromboembolic lesion, guide the optimal therapeutic decision, and allow response evaluation after surgical or interventional treatment. Hence, nuclear medicine can play a pivotal role in the management of CTEPH.
Data Availability
Data sharing does not applicable to this article as no datasets were generated or analyzed during the current study.
References
Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34-41. https://doi.org/10.1016/j.jacc.2013.10.029.
Hahn LD, Papamatheakis DG, Fernandes TM, Poch DS, Yang J, Shen J, et al. Multidisciplinary approach to chronic thromboembolic pulmonary hypertension: role of radiologists. Radiographics. 2023;43(2):e220078. https://doi.org/10.1148/rg.220078.
Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350(22):2257–64. https://doi.org/10.1056/NEJMoa032274.
Ende-Verhaar YM, Cannegieter SC, VonkNoordegraaf A, Delcroix M, Pruszczyk P, Mairuhu AT, et al. Incidence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: a contemporary view of the published literature. Eur Respir J. 2017;49(2):161792. https://doi.org/10.1183/13993003.01792-2016.
Hoeper MM, Humbert M, Souza R, Idrees M, Kawut SM, Sliwa-Hahnle K, et al. A global view of pulmonary hypertension. Lancet Respir Med. 2016;4(4):306–22. https://doi.org/10.1016/s2213-2600(15)00543-3.
Mahmud E, Madani MM, Kim NH, Poch D, Ang L, Behnamfar O, et al. Chronic thromboembolic pulmonary hypertension: evolving therapeutic approaches for operable and inoperable disease. J Am Coll Cardiol. 2018;71(21):2468–86. https://doi.org/10.1016/j.jacc.2018.04.009.
Simonneau G, Torbicki A, Dorfmüller P, Kim N. The pathophysiology of chronic thromboembolic pulmonary hypertension. Eur Respir Rev. 2017;26(143):16112. https://doi.org/10.1183/16000617.0112-2016.
Pepke-Zaba J, Delcroix M, Lang I, Mayer E, Jansa P, Ambroz D, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): results from an international prospective registry. Circulation. 2011;124(18):1973–81. https://doi.org/10.1161/circulationaha.110.015008.
Wartski M, Collignon MA. Incomplete recovery of lung perfusion after 3 months in patients with acute pulmonary embolism treated with antithrombotic agents. THESEE Study Group. Tinzaparin ou Heparin Standard: Evaluation dans l’Embolie Pulmonaire Study. J Nucl Med. 2000;41(6):1043–8.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543–603. https://doi.org/10.1093/eurheartj/ehz405.
Moser KM, Auger WR, Fedullo PF. Chronic major-vessel thromboembolic pulmonary hypertension. Circulation. 1990;81(6):1735–43. https://doi.org/10.1161/01.cir.81.6.1735.
Pietra GG, Capron F, Stewart S, Leone O, Humbert M, Robbins IM, et al. Pathologic assessment of vasculopathies in pulmonary hypertension. J Am Coll Cardiol. 2004;43(12 Suppl S):25s–32s. https://doi.org/10.1016/j.jacc.2004.02.033.
Humbert M. Pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: pathophysiology. Eur Respir Rev. 2010;19(115):59–63. https://doi.org/10.1183/09059180.00007309.
Lang IM, Gaine SP. Recent advances in targeting the prostacyclin pathway in pulmonary arterial hypertension. Eur Respir Rev. 2015;24(138):630–41. https://doi.org/10.1183/16000617.0067-2015.
Higuchi S, Ota H, Yaoita N, Kamada H, Takagi H, Satoh T, et al. Update on the roles of imaging in the management of chronic thromboembolic pulmonary hypertension. J Cardiol. 2023;81(3):297–306. https://doi.org/10.1016/j.jjcc.2022.03.001.
Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67–119. https://doi.org/10.1093/eurheartj/ehv317.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618–731. https://doi.org/10.1093/eurheartj/ehac237.
Moradi F, Morris TA, Hoh CK. Perfusion scintigraphy in diagnosis and management of thromboembolic pulmonary hypertension. Radiographics. 2019;39(1):169–85. https://doi.org/10.1148/rg.2019180074.
Skoro-Sajer N, Becherer A, Klepetko W, Kneussl MP, Maurer G, Lang IM. Longitudinal analysis of perfusion lung scintigrams of patients with unoperated chronic thromboembolic pulmonary hypertension. Thromb Haemost. 2004;92(1):201–7. https://doi.org/10.1160/th03-11-0727.
Papamatheakis DG, Poch DS, Fernandes TM, Kerr KM, Kim NH, Fedullo PF. Chronic thromboembolic pulmonary hypertension: JACC Focus Seminar. J Am Coll Cardiol. 2020;76(18):2155–69. https://doi.org/10.1016/j.jacc.2020.08.074.
Tanabe N, Sugiura T, Tatsumi K. Recent progress in the diagnosis and management of chronic thromboembolic pulmonary hypertension. Respir Investig. 2013;51(3):134–46. https://doi.org/10.1016/j.resinv.2013.02.005.
Pickhardt PJ, Fischer KC. Unilateral hypoperfusion or absent perfusion on pulmonary scintigraphy: differential diagnosis. AJR Am J Roentgenol. 1998;171(1):145–50. https://doi.org/10.2214/ajr.171.1.9648778.
Chen D, Zhu G, Wang D, Zhang Z, Fang W, Qu Z. Clinicopathological and immunohistochemical features of pulmonary artery sarcoma: a report of three cases and review of the literature. Oncol Lett. 2016;11(4):2820–6. https://doi.org/10.3892/ol.2016.4308.
Haque U, Hellmann D, Traill T, Venbrux A, Stone J. Takayasu’s arteritis involving proximal pulmonary arteries and mimicking thromboembolic disease. J Rheumatol. 1999;26(2):450–3.
Goldbach AR, Pascarella S, Dadpravarar S. Fibrosing mediastinitis: a rare cause of unilateral absent lung perfusion on a V/Q scan. Nucl Med Mol Imaging. 2018;52(5):401–4. https://doi.org/10.1007/s13139-018-0545-6.
Tunariu N, Gibbs SJ, Win Z, Gin-Sing W, Graham A, Gishen P, et al. Ventilation-perfusion scintigraphy is more sensitive than multidetector CTPA in detecting chronic thromboembolic pulmonary disease as a treatable cause of pulmonary hypertension. J Nucl Med. 2007;48(5):680–4. https://doi.org/10.2967/jnumed.106.039438.
McLaughlin VV, Langer A, Tan M, Clements PJ, Oudiz RJ, Tapson VF, et al. Contemporary trends in the diagnosis and management of pulmonary arterial hypertension: an initiative to close the care gap. Chest. 2013;143(2):324–32. https://doi.org/10.1378/chest.11-3060.
Gutte H, Mortensen J, Jensen CV, von der Recke P, Petersen CL, Kristoffersen US, et al. Comparison of V/Q SPECT and planar V/Q lung scintigraphy in diagnosing acute pulmonary embolism. Nucl Med Commun. 2010;31(1):82–6. https://doi.org/10.1097/MNM.0b013e3283336747.
Stubbs M, Chan K, McMeekin H, Navalkissoor S, Wagner T. Incidence of a single subsegmental mismatched perfusion defect in single-photon emission computed tomography and planar ventilation/perfusion scans. Nucl Med Commun. 2017;38(2):135–40. https://doi.org/10.1097/mnm.0000000000000632.
Wang L, Wang M, Yang T, Wu D, Xiong C, Fang W. A prospective, comparative study of ventilation-perfusion planar imaging and ventilation-perfusion SPECT for chronic thromboembolic pulmonary hypertension. J Nucl Med. 2020;61(12):1832–8. https://doi.org/10.2967/jnumed.120.243188.
Chan K, Ioannidis S, Coghlan JG, Hall M, Schreiber BE. Pulmonary arterial hypertension with abnormal V/Q single-photon emission computed tomography. JACC: Cardiovascular Imaging. 2018;11(10):1487–93. https://doi.org/10.1016/j.jcmg.2017.07.026.
Suh M. In the COVID-19 Era, Is it ok to perform a perfusion-only SPECT/CT for the diagnosis of pulmonary embolism? Nucl Med Mol Imaging. 2022;56(2):67–70. https://doi.org/10.1007/s13139-022-00740-y.
Palmowski K, Oltmanns U, Kreuter M, Mottaghy FM, Palmowski M, Behrendt FF. Diagnosis of pulmonary embolism: conventional ventilation/perfusion SPECT is superior to the combination of perfusion SPECT and nonenhanced CT. Respiration. 2014;88(4):291–7. https://doi.org/10.1159/000365817.
Azarian R, Wartski M, Collignon MA, Parent F, Hervé P, Sors H, et al. Lung perfusion scans and hemodynamics in acute and chronic pulmonary embolism. J Nucl Med. 1997;38(6):980–3.
Bajc M, Schümichen C, Grüning T, Lindqvist A, Le Roux PY, Alatri A, et al. EANM guideline for ventilation/perfusion single-photon emission computed tomography (SPECT) for diagnosis of pulmonary embolism and beyond. Eur J Nucl Med Mol Imaging. 2019;46(12):2429–51. https://doi.org/10.1007/s00259-019-04450-0.
Derlin T, Kelting C, Hueper K, Weiberg D, Meyer K, Olsson KM, et al. Quantitation of perfused lung volume using hybrid SPECT/CT allows refining the assessment of lung perfusion and estimating disease extent in chronic thromboembolic pulmonary hypertension. Clin Nucl Med. 2018;43(6):e170–7. https://doi.org/10.1097/rlu.0000000000002085.
Hashimoto H, Oka T, Nakanishi R, Mizumura S, Dobashi S, Hashimoto Y, et al. Evaluation of balloon pulmonary angioplasty using lung perfusion SPECT in patients with chronic thromboembolic pulmonary hypertension. J Nucl Cardiol. 2022;29(6):3392–400. https://doi.org/10.1007/s12350-022-02971-0.
Vuylsteke A, Sharples L, Charman G, Kneeshaw J, Tsui S, Dunning J, et al. Circulatory arrest versus cerebral perfusion during pulmonary endarterectomy surgery (PEACOG): a randomised controlled trial. Lancet. 2011;378(9800):1379–87. https://doi.org/10.1016/s0140-6736(11)61144-6.
D’Armini AM, Zanotti G, Ghio S, Magrini G, Pozzi M, Scelsi L, et al. Reverse right ventricular remodeling after pulmonary endarterectomy. J Thorac Cardiovasc Surg. 2007;133(1):162–8. https://doi.org/10.1016/j.jtcvs.2006.08.059.
Condliffe R, Kiely DG, Gibbs JS, Corris PA, Peacock AJ, Jenkins DP, et al. Improved outcomes in medically and surgically treated chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med. 2008;177(10):1122–7. https://doi.org/10.1164/rccm.200712-1841OC.
Lankeit M, Krieg V, Hobohm L, Kölmel S, Liebetrau C, Konstantinides S, et al. Pulmonary endarterectomy in chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant. 2017. https://doi.org/10.1016/j.healun.2017.06.011.
Thistlethwaite PA, Madani MM, Kemp AD, Hartley M, Auger WR, Jamieson SW. Venovenous extracorporeal life support after pulmonary endarterectomy: indications, techniques, and outcomes. Ann Thorac Surg. 2006;82(6):2139–45. https://doi.org/10.1016/j.athoracsur.2006.07.020.
Delcroix M, Lang I, Pepke-Zaba J, Jansa P, D’Armini AM, Snijder R, et al. Long-term outcome of patients with chronic thromboembolic pulmonary hypertension: results from an International Prospective Registry. Circulation. 2016;133(9):859–71. https://doi.org/10.1161/circulationaha.115.016522.
Olman MA, Auger WR, Fedullo PF, Moser KM. Pulmonary vascular steal in chronic thromboembolic pulmonary hypertension. Chest. 1990;98(6):1430–4. https://doi.org/10.1378/chest.98.6.1430.
Moser KM, Metersky ML, Auger WR, Fedullo PF. Resolution of vascular steal after pulmonary thromboendarterectomy. Chest. 1993;104(5):1441–4. https://doi.org/10.1378/chest.104.5.1441.
Ghofrani HA, D’Armini AM, Grimminger F, Hoeper MM, Jansa P, Kim NH, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med. 2013;369(4):319–29. https://doi.org/10.1056/NEJMoa1209657.
Simonneau G, D’Armini AM, Ghofrani HA, Grimminger F, Hoeper MM, Jansa P, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension: a long-term extension study (CHEST-2). Eur Respir J. 2015;45(5):1293–302. https://doi.org/10.1183/09031936.00087114.
Sadushi-Kolici R, Jansa P, Kopec G, Torbicki A, Skoro-Sajer N, Campean IA, et al. Subcutaneous treprostinil for the treatment of severe non-operable chronic thromboembolic pulmonary hypertension (CTREPH): a double-blind, phase 3, randomised controlled trial. Lancet Respir Med. 2019;7(3):239–48. https://doi.org/10.1016/s2213-2600(18)30367-9.
Ghofrani HA, Simonneau G, D’Armini AM, Fedullo P, Howard LS, Jaïs X, et al. Macitentan for the treatment of inoperable chronic thromboembolic pulmonary hypertension (MERIT-1): results from the multicentre, phase 2, randomised, double-blind, placebo-controlled study. Lancet Respir Med. 2017;5(10):785–94. https://doi.org/10.1016/s2213-2600(17)30305-3.
Ogawa A, Matsubara H. Balloon pulmonary angioplasty: a treatment option for inoperable patients with chronic thromboembolic pulmonary hypertension. Front Cardiovasc Med. 2015;2:4. https://doi.org/10.3389/fcvm.2015.00004.
Ogawa A, Satoh T, Fukuda T, Sugimura K, Fukumoto Y, Emoto N, et al. Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension: results of a multicenter registry. Circ Cardiovasc Qual Outcomes. 2017;10(11):e004029. https://doi.org/10.1161/circoutcomes.117.004029.
Lang I, Meyer BC, Ogo T, Matsubara H, Kurzyna M, Ghofrani HA, et al. Balloon pulmonary angioplasty in chronic thromboembolic pulmonary hypertension. Eur Respir Rev. 2017;26(143):160119. https://doi.org/10.1183/16000617.0119-2016.
Kawakami T, Kataoka M, Nakahara T, Yamada Y, Takei M, Jinzaki M, et al. Usefulness of 3D SPECT/CT fusion image in CTEPH. Int J Cardiol. 2015;194:39–40. https://doi.org/10.1016/j.ijcard.2015.05.056.
Wang L, Han X, Wang M, Ma X, Zhang H, Yan C, et al. Ventilation/perfusion imaging predicts response to balloon pulmonary angioplasty in patients with chronic thromboembolic pulmonary hypertension. Ann Nucl Med. 2022;36(6):515–22. https://doi.org/10.1007/s12149-022-01731-x.
Maruoka Y, Nagao M, Baba S, Isoda T, Kitamura Y, Yamazaki Y, et al. Three-dimensional fractal analysis of 99mTc-MAA SPECT images in chronic thromboembolic pulmonary hypertension for evaluation of response to balloon pulmonary angioplasty: association with pulmonary arterial pressure. Nucl Med Commun. 2017;38(6):480–6. https://doi.org/10.1097/mnm.0000000000000673.
Author information
Authors and Affiliations
Contributions
The study was designed by Sangwon Han. Writing the first draft of the manuscript was done by Sejin Ha. Revision and editing of the manuscript were done by Sejin Ha and Sangwon Han. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Declarations
Ethical Approval and Consent to Participate
This is a review paper for which ethics approval and consent to participate are not required.
Consent for Publication
Not applicable
Competing Interests
Sejin Ha and Sangwon Han declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ha, S., Han, S. The Role of Lung Ventilation/Perfusion Scan in the Management of Chronic Thromboembolic Pulmonary Hypertension. Nucl Med Mol Imaging (2023). https://doi.org/10.1007/s13139-023-00830-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13139-023-00830-5