Abstract
Purpose
177Lu-DKFZ-PSMA-617 is a promising treatment for patients with metastatic prostate cancer. Specific dosimetry for each patient is an important factor in planning the patient’s treatment process. This study aimed to perform an image-based absorbed dose calculation for the treatment of metastatic prostate cancer with 177Lu-DKFZ-PSMA-617.
Methods
The individualized patient dosimetry calculations were based on whole-body planar scintigraphy images acquired in 10 patients with a mean age of 71.4 ± 6.07 years (range 63–85 years) at approximately 0–2 h, 4–6 h, 18–24 h, and 36–48 h after administration of the mean 6253 ± 826.4 MBq (range 5500–7400 MBq) of 177Lu-DKFZ-PSMA-617. Time-activity curves were generated for various organs. For count conversion to activities, calibration factors were calculated. Finally, the absorbed dose for an individual cycle was calculated using IDIAC-DOSE 2.1 software.
Results
On average, the calculated absorbed dose for the kidneys and salivary glands were 0.46 ± 0.09 mGy/MBq and 0.62 ± 0.07 mGy/MBq, respectively.
Conclusions
Based on the results, the177Lu-PSMA-617 therapy is a safe method for the treatment of castration-resistant prostate cancer patients. Large inter-individual variations in organ dose were found, demonstrating the need for patient-specific dosimetry and treatment planning.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most common type of cancer in men worldwide [1, 2]. Despite several treatment options such as chemotherapy, hormone, and radiation therapy, more than 250,000 men are still dying from prostate cancer each year around the world [3]. The basic principle of radioligand therapy (RLT) is to give the maximum justifiable dose to the tumor tissue, which does not cause serious toxicity to the organ at risk. Prostate-specific membrane antigen (PSMA) has been considered as a target in the treatment of metastatic prostate cancer radionuclide [4,5,6]. In other words, PSMA has gained attention as a new target for molecular imaging and targeted therapy [7,8,9,10]. Recently, a new PSMA ligand called 177Lu-DKFZ-PSMA-617 was tested for prostate metastatic cancer [11]. For the assessment of a new therapy method, dosimetry (for tumors and organs at risk) is essential to aim for the optimal therapeutic response with limited side effects. Some results in case of dose estimation for patients treated with 177Lu-DKFZ-PSMA-617 have previously been published [12,13,14,15,16]. Results from these publications demonstrate variation in absorbed dose to the organs (kidneys, liver, spleen, bladder, salivary glands, and whole-body). IDIAC-DOSE 2.1 (internal dose assessment by computer) is a recent program, which implements the MIRD standard phantom-based metrology developed for the dosimetric purpose. Several studies have reported dosimetry data for organs based on OLINDA software [16,17,18,19,20,21]. Absorbed doses for different organs were calculated, using a combination of linear approximation, exponential fit, and specific S values target according to the MIRD scheme by Deklera et al. [12]. This study showed that the salivary glands and kidneys received a high absorbed dose, but were not critical after treatment with 177Lu-DKFZ-PSMA-617. In a study conducted by Hohberg et al. [14], nine patients with a history of prostate cancer documented by radiological evidence of metastatic diseases underwent radioligand therapy with 177Lu-DKFZ-PSMA-617. The mean absorbed doses were estimated using OLINDA/EXM 1.1. The study was stated that the absorbed doses of 177Lu-PSMA-617 therapy may not be critical for the kidneys, salivary glands, and the nasal mucous membrane. The OLINDA/EXM 1.1 dosimetry program was used to calculate the absorbed dose by Kabasakal et al. [15]. The results showed a substantial variation in the absorbed dose for each organ. The highest radiation dose was reported for the parotid glands and kidneys. In this study, we were looking for a simple, fast, and accurate computation method that can be easily used in clinics. The current study aimed to estimate image-based absorbed dose calculation for critical and non-target organs during the first cycle of 177Lu-DKFZ-PSMA-617 therapy for patients with prostate cancer using the IDIAC-DOSE 2.1 software.
Materials and Methods
Data analysis was performed on ten patients with distant metastases and progressive disease, aged 63 to 85 years (mean 71.4 ± 6.07 years) and adequate hematological, liver, and renal function, who were treated with 177Lu-DKFZ-PSMA-617 between April 2020 and September 2020 in Shohada-e-Tajrish Hospital, Tehran, Iran. Most patients, before the intervention to assess the state of expression of PSMA metastases, underwent PSMA positron emission tomography/computed tomography (PET/CT). A summary of the treatment history for patients is shown in Table 1. The physician determined the specific activity to be administered, according to the dosimetric results and the patient’s clinical conditions. During the first cycle, patients were evaluated for dosimetry with 177Lu-DKFZ-PSMA-617. The mean activity of 6253 ± 826.4 (range 5500–7400 MBq) was used. The radiopharmaceutical was infused intravenously in an injection room using a dedicated pump system. In order to reduce blood flow and tracer uptake in the salivary gland and parotic, ice packs were placed at each side of the neck 30 min before, during infusion, and up to 4 h after administration of 177Lu-DKFZ-PSMA-617. The time interval between the treatment cycles was usually 8–12 weeks. Patients underwent 4 cycles, and up to 2 additional cycles were administered if there was no evidence of disease progression and treatment could clinically benefit the patient. Patients underwent follow-up examinations, including routine blood tests, 2 to 4 weeks after RLT. All patients signed a written informed consent form for anonymized evaluation and publication of their data. Following injection of 177Lu-DKFZ-PSMA-617, patients underwent imaging at 0–2 h, 4–6 h, 18–20 h, and 36–48 h in the form of whole-body planar acquisition. Planar imaging was used to measure the whole body and organ activity over a number of days. All data were acquired on a dual-head gamma camera (Symbia Evo Excel SIEMENS) equipped with a low-energy high-resolution (LEHR) collimator and with 3/8-in. thick NaI (Tl) crystals. Anterior and posterior views were acquired with a 16 cm/min scan speed, with an energy window of 20% for a double peak at 113 and 208 keV. The first whole-body image was performed before bladder voiding because the total counts were used to calculate the time-activity curves. The whole-body image was 1024 × 1024 pixel matrix dimensions of 2.4 × 2.4 cm2. Single-photon emission computed tomography (SPECT) image was used for the localization of regions with specific or non-specific 177Lu-DKFZ-PSMA-617 uptake. A 177Lu source (25 ml, 296 MBq) was positioned as a point source. The static image was acquired for 300 s, using the same matrix, pixel size, and energy setting as for the whole-body image. The number of counts in a region of interest (ROI) around the source in the image was determined and divided by scanning time. The system calibration factor for 177Lu was determined in counts per second per MBq (cps/MBq) using Eq. 1 [22].
The organ may receive radiation directly from the injected radionuclide or from other organs around them. Both detector heads were used to acquire the subject data so that a geometric mean (GM) whole-body planar image was produced during the analysis, as described in the MIRD methodology. The standard method for quantification of organ activities and the redistribution with time between different organs are the conjugate view methods. This method is based on measuring a source located at some effective depth (d) in a medium characterized by an attenuation coefficient (µ). The count rates were measured by drawn regions of interest (ROI) for the liver, spleen, kidneys, salivary glands, and bladder on the subsequent scans. When drawing a ROI around an organ, other overlapping organs and tissues should not be included or avoided as far as is possible. The background count rate was measured close to regions of interest. Then, small and separate ROIs were also drawn near part of each organ and the whole body. The measurements are often conducted in an anterior view (RA) and in a posterior view (RB) which can be described by Eq. 2.
where L is the anterior–posterior body thickness and R0 is the counting rate that would have been obtained if the source had been in air. The result is independent from d source depth, when calculating the geometric mean of RA and RB in Eq. 3:
The activity is determined from the system sensitivity (cps/MBq) in air, C in Eq. 4.
The source organ thickness (l) can be considered in Eq. 5 as follows:
To simplify Eq. 5, Eq. 6 can be used as follows:
Finally, the activity was calculated for the whole body, liver, spleen, kidneys, salivary glands, and bladder in each time point, using Eq. 7 [14].
For paired organs (kidneys and parotid glands), the value was calculated and single time-activity curve was obtained. The curve of activity as a function of the time was drawn for each organ and fitted to bi-exponential function. The cumulative activity was calculated in each organ, separately using MATLAB (2018) program. Each organ residence time (h) was calculated by dividing cumulative activity to administered activity.
Calculation of the absorbed dose in current study have been done using two method:
First: Medical Internal Radiation Dose (MIRD) scheme provides a conventional method for estimating absorbed dose of radionuclides in internal organs. The mean absorbed dose for each organ was determined with Eq. 8.
where \(\overline{D }\) is the absorbed dose of each target, \({\tilde{A }}_{{cum}}^{{source}}\) is the cumulative activity of each source, and S value is the absorbed dose per cumulative activity for each pair source target. Dose values were computed using S-factor for Lu-177 which is derived from the Radiation Dose Assessment Resource (RADAR) website [23, 24]. Also, in this study, first we used standard organ size (mass and thickness) from ICRP 89 and MIRD No.5. [25, 26].
Second, the dose evaluation was performed according to IDIAC-DOSE 2.1 software. An internal dosimetry computer program, IDAC-Dose 2.1, was developed based on the International Commission on Radiological Protection (ICRP) absorbed fractions and computational framework of internal dose assessment given for reference adults in ICRP Publication 133. For calculation of the absorbed dose, cumulated activity in a source region divided by the administered activity. The IDIAC-DOSE 2.1 software calculates absorbed doses to all 47 target regions defined in ICRP Publication 133. The results are presented in terms of absorbed dose per administered activity (mGy/MBq) [20].
Ethics Approval and Consent to Participate
The study was approved by the hospital ethics committee, informed consent was obtained from all patients and it was carried out according to the provisions of the Declaration of Helsinki.
Statistical Analysis
All results were expressed as the mean ± SD. The complete data analysis was done using Microsoft Excel (Microsoft office professional plus 2013) and MATLAB (version 2018) software. Statistical analyses were performed using SPSS (version.16. SPSS Inc, USA, Chicago IL) software.
Results
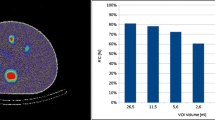
The planar images showed increased physiologic uptake in the salivary glands, kidneys, small intestine, and less pronounced in the liver and spleen. The obtained residence times are listed for each organ in Table 2. The mean values were 0.6 ± 0.08.h (range 0.5–0.7) for the salivary glands, 1.7 ± 0.4 h (range 1.3–2.2) for the kidneys, 1.2 ± 0.42 h (range 0.6–1.8) for the liver, 0.1 ± 0.06 h (range 0.08–0.2) for the bladder, and 0.08 ± 0.01 h (range 0.07–0.1) for the spleen. The total body residence time was obtained from 30.1 to 60.3 h with a mean value of 46.3 ± 10.8 h, and it showed a great variation among the patients. The whole-body residence times showed great variation resulting in absorbed dose per administered activity ranging from 0.05 to 0.09 mGy/MBq using MIRD formalism and that ranges from 0.04 to 0.20 mGy/MBq when using IDAC-DOSE 2.1 software. The values (mean, SD, and range) for absorbed dose per MBq which is calculated with IDIAC-DOSE version 2.1 program are presented in Table 2. The mean absorbed doses were 0.058 ± 0.02 mGy/MBq (range 0.05–0.08 mGy/MBq) for the liver and 0.052 ± 0.007 mGy/MBq (range 0.04–0.08 mGy/MBq) for the spleen. The calculated mean absorbed doses were 0.62 ± 0.07 mGy/MBq (range 0.55–0.75 mGy/MBq) for the salivary glands, 0.46 ± 0.09 mGy/MBq (range 0.37–0.63 mGy/MBq) for the kidneys, 0.028 ± 0.04 mGy/MBq (range 0.012–0.035 mGy/MBq) for the bladder, and 0.07 ± 0.04 mGy/MBq (range 0.05–0.09 mGy/MBq) for the whole body. The dosimetric results for all patient cohort with MIRD formalism are reported in Table 2. The highest estimated dose was calculated for the salivary glands and kidneys. Calculated mean absorbed doses were 0.83 ± 0.20 mGy/MBq (range 0.50–0.90 mGy/MBq) for the salivary glands, 0.60 ± 0.17 mGy/MBq (range 0.50–0.90 mGy/MBq) for the kidneys, 0.08 ± 0.06 mGy/MBq (range 0.07–0.1 mGy/MBq) for the liver, 0.062 ± 0.03 mGy/MBq (range 0.05–0.1 mGy/MBq) for the spleen, 0.18 ± 0.04 mGy/MBq (range 0.12–0.20 mGy/MBq) for the bladder, and 0.09 ± 0.02 mGy/MBq (range 0.04–0.20 mGy/MBq) for the whole body. The difference between the absorbed dose measured for different organs by MIRD formalism and IDIAC-DOSE 2.1 software method is shown in Fig. 1. The comparison of the mean absorbed dose in different organs with MIRD formalism (columns in gray) and IDIAC-DOSE 2.1 software (columns in black) showed variation in the results. Multiple factors could contribute to the differences in dosimetric outcomes between the two ways, which could be due to the type of phantom which is used in software. In IDIAC- DOSE 2.1 software both the kidneys and salivary glands are considered as one organ. However, the mean absorbed dose for the left and right kidney and salivary glands can be different. In addition, the dosimetric approach using organ-based dosimetry (MIRD) vs. voxel-based dosimetry is fundamentally different. In MIRD software, the S values are fixed per tissue type whereas the voxel-based approach is independent from the analyzed tissue.
Discussion
Authors introduced the first experiences with 177Lu-DKFZ-PSMA-617 in the department for the treatment of metastatic prostate cancer. 177Lu-DKFZ-PSMA-617 uptake in high-risk organs, such as the salivary glands and kidneys, may impair therapeutic efficacy by limiting injectable activity per cycle. There are two classes of failure in radiation therapy: local control not achieved and radiation-induced morbidity. The optimal treatment planning need to access a higher dose to the target and/or the irradiation of smaller volumes of non-target tissues. An important fact is that uneradicated tissues do not develop radiation-related injury. The dose to organs varies considerably for each individual patient, which gives rise to whole absorbed activity variations in organs at risk and target tissue which may cause an over exposure of dosage to patients. Therefore, the administered activity has to be given with safety margin. The absorbed dose of the normal organ for 177Lu-DKFZ-PSMA-617 was accurately estimated using planar imaging through the MIRD formalism and IDIAC-DOSE 2.1 software. Once the time integrals of activities are measured in each organ, the absorbed dose calculations in target organs are generally performed using IDIAC-DOSE 2.1 program in which the S value factor from any source to any target is integrated because they do not consider the patient’s specific differences in body shape and size, nor the uniform distribution of activity in the source organs. Significant differences were observed in the absorbed dose for different organs of different patients. The reason for this difference can be the effect of biological distribution of different radiopharmaceuticals in different patients, amount of activity uptake in different organs, and rate of excretion of radiopharmaceuticals from the body. Another reason for this difference is related to behavior of radiopharmaceuticals in different patients due to the severity of the disease. In general, it can be said that the organ radiation doses were within acceptable ranges; however, there was a substantial individual variance which indicates that patient dosimetry is necessary. The majority of the mentioned articles used OLINDA/EXAM to compute absorbed dose. IDIAC-DOSE 2.1 was used to calculate absorbed doses for intravenously administered 18F-FDG and orally administered 99mTc-pertechnetate and 131I-iodide [20]. One of the capabilities of IDIAC-DOSE 2.1 software is determining the share of the absorbed dose of each organ due to electron and photon doses. Electron and photon dose analysis showed that in source organs, the highest absorbed cycle is related to the activity in the organ. Unfortunately, there are currently no published data regarding the absorbed dose given with IDIAC-DOSE 2.1 for systemic therapy with 177Lu-DKFZ-PSMA-617 for comparison. Apart from that the mean absorbed dose to the whole body, kidneys, liver, and salivary glands which are reported in the current study are almost comparable to those previously reported by Dekler et al. [12], Hoberg et al. [14], and Kabasakal [15]. The comparison of the results presented in Table 3. The difference between values obtained in various studies which are mainly due to differences in (a) the imaging techniques: dose estimations could be based on either 2-dimensional (2D) planar gamma camera imaging or 3-dimensional (3D) imaging; (b) recording time of the image: more frequent measurements give a more accurate determination of the time-integrated radioactivity, implying a more accurate determination of the dose integral; and (c) the type of software which is used has a great impact on the evaluation and calculation of the absorbed dose in the organs. Regarding the absorbed dose of the kidney and salivary glands, protective measures taken during treatment are also very important. It is best to prevent kidney damage prior therapy, to ensure adequate renal function, and to rule out any obstructive kidney disease, and the patient can be given renal perfusion scintigraphy with [99mTc] MAG or [99mTc] DTPA. Despite the high uptake in the kidneys, low renal toxicity has been reported after PSMA-TRT but when PSMA-TRT will be used for patients in an early-stage of PCa with metastatic disease, renal may be disturbing. Accurate dosimetry data for the kidneys and parotid glands were available from the studies by Sarneli et al. [13] and Hohbeg et al. [14], while the mean dose values were reported in the study by Kabasakal et al. [15]. Therefore, a graphical comparison (based on median) was used to compare the kidney results in Fig. 2, while statistical comparisons were performed for the salivary glands in Fig. 3. The accuracy of internal dose calculations depends on activity cumulated in organs, so it is essential to choose a method that is accurate and simple without disturbing the workload of busy nuclear medicine environments. The method which is proposed in the current study is, however, a simple method that is easily implemented in any clinic with a gamma camera. Determining the absorbed dose using the MIRD formalism is time-consuming and can be solved more easily and quickly. Using software greatly reduces computational errors, but the method based on MIRD scheme dosimetry make improvement inaccuracy of the calculation of absorbed dose for the kidneys and salivary glands as compared to the calculation in software since the organ dose (left kidney, right kidney or left salivary gland, right salivary gland) maybe calculated separately. The calculation of the absorbed dose using the standard organ size (MIRD 5 and ICRP 89) instead of patient-specific organ size may cause many changes in the amount of absorb dose. Studies have shown that significant differences between the anatomy of each patient and phantoms can be, so you can improvement in the accuracy of measured doses may thus be achieved by a precise organ volume by using high-spatial-resolution imaging, such as CT or MR. The difference in the size of the organ may affect the estimated absorbed dose and indicate that it clearly demonstrate the importance of data from a late time point, especially for obtaining real time-activity curves for radionuclides with a long physical half-life such as Lu-177. In addition, the ROI position of each organ in an image may differ from the patient’s position in the camera. A 3D implementation with SPECT/CT and PET/CT dosimetry or hybrid techniques can improve the accuracy of absorbed dose assessment for each organ. Compared to SPECT/CT or PET/CT, planar scintigraphy remains to be the easiest and least time-consuming approach for whole-body imaging in terms of acquisition time, calibration, and quantification of recovery coefficients. The study was restricted to a small sample size due to a limited study time. Another factor affecting our analysis was organ overlap, such as high intestinal uptake or lesion overlap, which may compromise the obtained results. The implementation of fully 3D dosimetry or hybrid techniques could improve the accuracy of absorbed dose.
Conclusion
In this study, organs like the kidneys and salivary glands showed the highest 177Lu-DKFZ-PSMA-617 uptake and hence the highest absorbed dose whereas the liver and spleen showed a relatively lower uptake and absorbed dose. The results clearly demonstrate the importance of the individualized dosimetric calculation for critical organs for optimal treatment planning using 177Lu-DKFZ-PSMA-617.
Availability of Data and Materials
All data and information are available.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29.
Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, Bray F. International variation in prostate cancer incidence and mortality rates. Eur Urol. 2012;61:1079–92.
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of hybrid 68Ga-PSMA ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med. 2015;56:668–74.
Zechmann CM, Afshar-Oromieh A, Armor T, Stubbs JB, Mier W, Hadaschik B, et al. Radiation dosimetry and first therapy results with a (124)I/(131)I-labeled small molecule (MIP-1095) targeting PSMA for prostate cancer therapy. Eur J Nucl Med Mol Imaging. 2014;41:1280–92.
Eiber M, Nekolla SG, Maurer T, Weirich G, Wester HJ, Schwaiger M. (68) Ga-PSMA PET/MR with multimodality image analysis for primary prostate cancer. Abdom Imaging. 2015;40:1769–71.
Wright GL Jr, Haley C, Beckett ML, Schellhammer PF. Expression of prostate specific membrane antigen in normal, benign, and malignant prostate tissues. Urol Oncol. 1995;1:18–28.
Afshar-Oromieh A, Hetzheim H, Kratochwil C, Benes ova M, Eder M, Neels OC, et al. The theranostic PSMA ligand PSMA-617 in the diagnosis of prostate cancer by PET/CT: biodistribution in humans, radiation dosimetry, and first evaluation of tumor lesions. J Nucl Med. 2015;56:1697–705.
Ristau BT, O’Keefe DS, Bacich DJ. The prostate-specific membrane antigen: lessons and current clinical implications from 20 years of research. Urol Oncol. 2014;32:272–9.
Klein Nulent TJ, Valstar MH, de Keizer B, Willems SM, Smit LA, Al-Mamgani A, et al. Physiologic distribution of PSMA-ligand in salivary glands and seromucous glands of the head and neck on PET/CT. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125:478–86.
Kratochwil C, Giesel FL, Eder M, Afshar-Oromieh A, Benešová M, Mier W, Kopka K, et al. [177Lu]Lutetium-labelled PSMA ligand-induced remission in a patient with metastatic prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:987–8.
Delker A, Fendler WP, Kratochwil C, Brunegraf A, Gosewisch A, Gildehaus FJ, et al. Dosimetry for 177Lu-DKFZ-PSMA-617: a new radiopharmaceutical for the treatment of metastatic prostate cancer. Eur J Nucl Med Mol Imaging. 2016;43:42–51.
Sarnelli A, Belli ML, Di Iorio V, Mezzenga E, Celli M, Severi S, Tardelli E, Nicolini S, Oboldi D, Uccelli L, Cittanti C, Monti M, Ferrari M, Paganelli G. Dosimetry of 177Lu-PSMA-617 after mannitol infusion and glutamate tablet administration: preliminary results of EUDRACT/RSO 2016–002732-32 IRST protocol. Molecules. 2019;11(24):621.
Hohberg M, Eschner W, Schmidt M, Dietlein M, Kobe C, Fischer T, Drzezga A, Wild M. Lacrimal glands may represent organs at risk for radionuclide therapy of prostate cancer with 177 Lu DKFZ-PSMA-617. Mol Imaging Biol. 2016;18:437–45.
Kabasakal L, AbuQbeitah M, Aygün A, Yeyin N, Ocak M, Demirci E, Toklu T. Pre-therapeutic dosimetry of normal organs and tissues of (177)Lu-PSMA-617 prostate-specific membrane antigen (PSMA) inhibitor in patients with castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:1976–83.
Kabasakal L, Toklu T, Yeyin N, Demirci E, Abuqbeitah M, Ocak M, Aygün A, Karayel E, Pehlivanoğlu H, Alan SN. Lu-177-PSMA-617 prostate-specific membrane antigen inhibitor therapy in patients with castration-resistant prostate cancer: stability, bio-distribution and dosimetry. Mol Imaging Radionucl Ther. 2017;26:62–8.
Divoli A, Chiavassa S, Ferrer L, Barbet J, Flux GD, Bardiès M. Effect of patient morphology on dosimetric calculations for internal irradiation as assessed by comparisons of Monte Carlo versus conventional methodologies. J Nucl Med. 2009;50:316–23.
Howard DM, Kearfott KJ, Wilderman SJ, Dewaraja YK. Comparison of I-131 radioimmunotherapy tumor dosimetry: unit density sphere model versus patient-specific Monte Carlo calculations. Cancer Biother Radiopharm. 2011;26:615–21.
Senthamizhchelvan S, Hobbs RF, Song H, et al. Tumor dosimetry and response for 153Sm-ethylenediamine tetra methylene phosphoric acid therapy of high-risk osteosarcoma. J Nucl Med. 2012;53:215–24.
Andersson M, Johansson L, Eckerman K, Mattsson S. IDAC-Dose 2.1, an internal dosimetry program for diagnostic nuclear medicine based on the ICRP adult reference voxel phantoms. EJNMMI Res. 2017;7:88.
Miller C, Filipow L, Jackson S. A review of activity quantification by planar imaging methods. J Nucl Med Technol. 1995;23:3–9.
Stabin MG. Fundamentals of nuclear medicine dosimetry. 1st ed. New York: Springer Verlag; 2008.
Konijnenberg MW, Bijster M, Krenning EP, De Jong M. A stylized computational model of the rat for organ dosimetry in support of preclinical evaluations of peptide receptor radionuclide therapy with (90) Y, (111) In, or (177) Lu. J Nucl Med. 2004;45:1260–9 ([published correction appears in J Nucl Med 2009 Dec 50(12):2092).
Stabin MG, Siegel JA. Physical models and dose factors for use in internal dose assessment. Health Phys. 2003;85:294–310.
ICRP89. Basic anatomical and physiological data for use in radiological protection: reference values. A report of age- and gender-related differences in the anatomical and physiological characteristics of reference individuals. ICRP Publication 89. Ann ICRP. 2002;32:5–265.
Snyder WS, Fisher Jr HL, Ford MR, Warner GG. MIRD pamphlet no. 5, revised: Estimates of absorbed fractions for monoenergetic photon sources uniformly distributed in various organs of a heterogeneous phantom. J Nucl Med. 1969;Suppl 3:7–52.
Acknowledgements
This article has been extracted from the thesis written by Mrs. Elahe Mahmoudi in the School of Medicine, Shahid Beheshti University of Medical Sciences (Project No 410, 9,139).
Funding
There is no source of funding.
Author information
Authors and Affiliations
Contributions
The study was designed by Elahe Mahmoudi and Mohammad Reza Deevband. Material preparation and data collection were performed by Elahe Pirayesh, Mahasti amoui, and Mehrdad ghorbani Rad. The data analysis was performed by Elahe Mahmoudi, Mohammad Reza Deevband, Elahe Pirayesh, and Mahasti amoui. The first draft of the manuscript was written by Elahe Mahmoudi and Mohammad Reza Deevband, and all authors commented on previous versions of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interests
Elahe Mahmoudi, Elahe Pirayesh, Mohammad Reza Deevband, Mahasti Amoui, Mehrdad Ghorbani Rad and Mahdi Ghorbani declare that they have no competing interests.
Ethics Approval and Consent to Participate
The study was approved by the hospital ethics committee, informed consent was obtained from all patients, and it was carried out according to the provisions of the Declaration of Helsinki.
Consent for Publication
Informed consent was received from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahmoudi, E., Pirayesh, E., Deevband, M.R. et al. Patient-Specific Dosimetry in Radioligand Therapy (RLT) for Metastatic Prostate Cancer Using 177Lu-DKFZ-PSMA-617. Nucl Med Mol Imaging 55, 237–244 (2021). https://doi.org/10.1007/s13139-021-00713-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-021-00713-7