Abstract
Purpose
Single-photon emission computed tomography/computed tomography (SPECT/CT) is an advanced hybrid nuclear medicine technology that generates both functional and anatomical images in a single study. As utilization of SPECT/CT in Korea has been increasing, the purpose of this study was to survey its application of cardiac and skeletal SPECT/CT imaging for protocol optimization.
Methods
We surveyed CT protocols established for cardiac and skeletal SPECT/CT. We searched the guidelines for the CT protocols for SPECT/CT and reviewed the literature recently published.
Results
Among 36 hybrid SPECT scanners equipped with four or more multi-channel detector CTs (MDCTs), 18 scanners were used to perform cardiac studies at both very low current CT (30–80 mA; 11.1%) and ultra-low current CT (13–30 mA; 88.9%). Among the 33 canners, very low current (≤ 80 mA) CT or low current CT (80–130 mA) was used in 23.5%, and 41.8% for spine disorders, and in 36.4% or 30.3% for foot/ankle disorders, respectively. In the CT reconstructions, slice thickness of 5 mm for cardiac studies was most commonly used (94.4%); thinner slices (0.6–1.0 mm) for spine and foot/ankle studies were used in 24.2% and 45.5%, respectively. We also reviewed the international guidelines.
Conclusions
The results and current recommendations will be helpful for optimizing CT protocols for SPECT/CT. Optimization of SPECT/CT protocols will be required for generating the proper strategy for the specific lesions and clinical purpose.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Single-photon emission computed tomography/computed tomography (SPECT/CT) provides information on the distribution of radiotracer, displaying as functional tomographic image and anatomical tomographic image in a single format. SPECT/CT can be performed on any region of the body, following acquisition of two-dimensional planar images. Utilization of SPECT/CT is increasing in hospitals throughout Korea; however, there currently exists no specific standards, methods, or protocols for obtaining images. Korean hospitals have just recently acquired SPECT/CT capability as the first SPECT/CT device was installed in 2004, though not fully adopted due to the functional limitations on CT performance compared to the dedicated diagnostic CT scanners already in use and the lack of medical reimbursement. There are a few obese patients and some cancer patients who have benefited from them for attenuation correction and localization of the metastatic lesions. As improved CT technology applied for SPECT/CT, the use of this modality continues to increase in general. Hybrid SPECT scanner with multi-slice CT scanner that requires extensive knowledge for operating it appropriately, nuclear medicine physicians should be capable of carrying out such a task.
We undertook this investigation to explore how various Korean healthcare facilities created optimal SPECT/CT protocols, as well as to understand the current status and utilization of SPECT/CT in facilities overall. A literature search was performed that focused on the application of SPECT/CT for skeletal imaging, followed by a discussion on established international guidelines and protocols that are currently in common use.
Materials and Methods
Survey of Current Status of SPECT/CT in Korea
From February to March 2020, the Quality Control Committee from Korea Society for Nuclear Medicine (KSNM) contacted 31 nuclear medicine institutes and 2 equipment companies, gathering information on equipment, slice thickness, and CT acquisition protocols pertaining to cardiac and skeletal SPECT/CT.
Search Strategy and Study Selection
We performed our search using synonymous terms. We searched PubMed (Medline), EMBASE, and OVID Medline, Cochrane Library, KoreaMed, MedRIC, and KSI KISS to identify studies published in English between Jan 1, 2017 and Mar 13, 2020. We excluded studies of cancer, metastases, malignancies, and physics. We also excluded reviews, case reports, and investigations not written in English. The search terms used were Bone SPECT/CT-related index words (“Spine SPECT/CT” OR “Hip SPECT/CT” OR “Pelvis SPECT/CT” OR “Knee SPECT/CT” OR “Foot SPECT/CT” OR “Ankle SPECT/CT” OR “Shoulder SPECT/CT” OR “Wrist SPECT/CT” OR “Bone SPECT/CT”).
Results
Survey Results of CT Settings Used for SPECT/CT
Of the 31 institutions in Korea housed with 39 hybrid SPECT scanners equipped with CT scanners, 29 institutions maintaining 36 SPECT scanners with four or more CT channels were included in this study. A total of 36 and 35 hybrid SPECT/CT scanners provided information on whether they were used for cardiac or skeletal studies, respectively. For the remaining three scanners at three institutions, two institutions did not conduct any skeletal studies and one provided information on cardiac SPECT/CT protocols only. In the end, a total of 18 and 33 CT protocols of hybrid SPECT scanners were examined for cardiac and skeletal studies, respectively (Table 1).
We found that 18 of the 36 SPECT/CT scanners were used to perform cardiac studies (50.0%); CT protocols for cardiac SPECT/CT were applied to correct attenuation and localization. These scanners featured both very low current CT (30–80 mA; 11.1%) and ultra-low current CT (13–30 mA; 88.9%).
SPECT/CT for skeletal imaging was a more common procedure and performed by 91.7% of the 33 scanners identified. In this cohort, the same protocols for SPECT/CT were used for both spine and foot/ankle studies (23/33; 69.7%). Among the applications of SPECT/CT for diagnosing spinal disorders, very low current (≤ 80 mA) CT was used in 21.2% (7/33) of the scans and low current CT (80–130 mA) in 45.5% (15/33) of the scans. For SPECT/CT utilized in foot/ankle imaging, low current (80–130 mA) or very low current (≤ 80 mA) CT was used in 36.4% (12/33) and 24.2% (8/34) of the cases, respectively. Of the total cohort, 18 SPECT/CT devices were equipped to perform iterative reconstructions. Rotation times of 0.5–0.8 s were used in all 77.8%, 78.8%, and 78.8% of the cardiac, spine, and foot/ankle reconstructions, respectively. Likewise, a pitch of 0.94:1–0.95:1 was used in 50.0%, 60.6%, and 60.6% of the cardiac, spine, and foot/ankle reconstructions, respectively.
In CT scans for reconstructions of cardiac SPECT/CT analyses, a slice thickness of 5 mm was used in 94.4% of the institutions; thinner slices (0.6–1.0 mm) were used in 24.2% (8/33) and 45.5% (15/33) of these institutions for spine and foot/ankle reconstructions, respectively. A 512 × 512 matrix size for CT was used throughout.
Literature Search and Suggestions for the CT Protocols Used in SPECT/CT
Guidelines of SPECT/CT
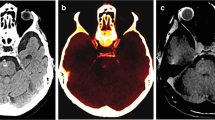
The Society of Nuclear Medicine and Molecular Imaging (SNMMI) [1], the International Atomic Energy Agency (IAEA) [2], and the European Association of Nuclear Medicine (EANM) [3] all commonly use attenuation correction for CT imaging in SPECT/CT. Table 2 summarizes the CT protocols of SPECT/CT proposed by each of these agencies. The SNMMI guideline recommended that attenuation correction or localization CT should be performed at a “low mA setting” and that diagnostic CT would follow at a “standard CT mA setting,” but no specific protocols were given. More specific guidelines has been provided by IAEA and EANM. The attenuation correction or localization protocols (i.e., those ≤ 40 mA) [1,2,3]. The EANM guideline for SPECT/CT recommended that different slice thicknesses should be used to evaluate distinct regions between extremities and the spine (Table 2). A slice or section ranging from 0.5 to 0.8 mm thick is required to achieve spatial resolution in all three dimensions [4]. Multi-slice CT images in the axial plane with thinner slice generate higher-quality coronal and sagittal images; this is the reasoning behind the application of axial images for reconstructions using multi-planar reformation (MPR) and three-dimensional (3D)-CT. In Figs. 1 and 2, post-processing MPRs using coronal and sagittal images (panel a) that were obtained with thinner slice along the axial plane shows the anatomy of the lesions much more clearly than the coronal and sagittal images (panels b) from thicker slices of along the same plane using the acquisition settings that include 120 kVp, 50–120 mA, and a rotation time of 0.95:1.
Coronal and sagittal multi-planar reconstructed (MPR) CT images (left, axial; middle, sagittal; and right, coronal) obtained from axial images of the spine in the post-processing reconstruction. Coronal and sagittal images by axial CT images using 1.25 mm slice thickness (a) show a clearer anatomy of the lesions than axial images using 5 mm slice thickness (b) in the post-processing CT reconstruction after the acquisition settings with 120 kVp, 50–120 mA, and rotation time 0.95:1
Coronal and sagittal multi-planar reconstructed (MPR) CT images (left, axial; middle, sagittal; and right, coronal) obtained from axial images of the ankle in the post-processing reconstruction. Coronal and sagittal images by axial CT images using 0.65 mm slice thickness (a) show a clearer the anatomy of the lesions than axial images using 2 mm slice thickness (b) in the post-processing CT reconstruction after the acquisition settings with120 kVp, 50–100 mA, and rotation time 0.95:1
The Korean Society of Radiology (KSR) has published two guidelines for the use of dedicated CT scanners: guidelines for the CT scan and retests [5] and guidelines for the justification and optimization of CT studies [6].
However, no organization has provided any clearly defined parameter for CT acquisition such as collimation, table increment, pitch, scan field, reconstruction field of view, and window settings. It is also desirable to obtain the optimal CT image quality while reducing radiation dose to a minimum [1,2,3,4,5].
Literature Search of Bone SPECT/CT Used Over the Past 3 Years
We reviewed 13 original articles that focused on SPECT/CT for spinal imaging [7,8,9,10,11,12,13,14,15,16,17,18,19], eight that focused on SPECT/CT of the foot and/or ankle imaging [19,20,21,22,23,24,25,26], ten that focused on SPECT/CT at the knee imaging [19,20,21, 27,28,29,30,31,32,33,34], six that focused on SPECT/CT for hip imaging [19, 35,36,37,38,39], and four that focused on SPECT/CT for wrist imaging [19, 40,41,42]. Two of the publications on spinal imaging included no information on device settings or on slice thickness, and one publication each pertaining to foot/ankle and knee imaging harbored no information on optimizing slice thickness. All studies featured SPECT/CT scanners of various makes and models, including those manufactured by Philips, General Electric (GE), and Siemens. Parameters such as tube voltage, tube current, slice thickness, and pitch differed across the board, though the matrix size was consistent at 512 × 512. Various protocols for CT were used by each institution or research facility. Diagnostic CT protocols utilizing 40–400 mA accounted for 46.1% of the reports of spine SPECT/CT and 50.0% of those focused on the wrist and shoulder. A low-dose CT protocol (≤ 100 mA) was applied in 87.5%, 81.8, and 66.7% of cases of SPECT/CT used for diagnosis of foot/ankle, knee, and hip disorders, respectively. A slice thickness of 0.33–2 mm was commonly used. These CT protocols are summarized in Table 3.
Discussion
In this study, we investigated and identified the current status of SPECT/CT for clinical use throughout Korea, primarily focusing on the use of SPECT/CT for evaluating cardiac and bone disorders. Importantly among our results, we found there was little use of cardiac SPECT with attenuation correction of CT, and this may be because there are few patients in Korea who are severely obese and typically evaluated with this modality. One guideline for SPECT/CT only commented a reconstruction parameter of CT, axial slice thickness [2], and we also investiaged axial slice thickness as a post-processing parameter in this study. We are to familiarize the CT techniques for post-processing as well as acqusition of CT in considering post-procssing reconstruction parameters affect the CT image quality. Herein, we brifely informed the readers of the post-processing as well as aqucisition of CT to help optimization of SPECT/CT protocols in clinical purpose.
Obtaining the optimal CT image while keeping the dose of radiation to a minimum can be conducted by decreasing tube voltage, tube current, and rotation time as well as increasing pitch. For implementing and evaluating optimization protocols, the report on dose information report can provide useful information for reducing radiation exposure [6]. If you reduce the tube current or tube voltage in an attempt to reduce the radiation dose excessively, you will see decrease in contrast resolution and increase in electrical noise and thus poor image quality. On the other hand, it is also critical to remember that the diagnostic performance of images that result from a higher radiation dose may be comparable to an image produced using low-dose CT, so it is necessary to design a CT protocol that takes into account all of the critical factors and identify parameters that will maintain the diagnostic value of an image at the minimum dose of radiation [6]. The automatic exposure control (AEC) used in a multiple detector CT device has different dose control methods depending on the source of the equipment; its purpose is to control the radiation dose according to the degree of attenuation. The overall patient dose can be reduced [6, 43]; however, AEC is not necessarily useful in this regard. For low-dose protocols, fixed low tube current is the best method for dose control [6].
Regardless of increasing CT dose, several change to the reconstruction parameters are necessary for improving the image quality. In reconstruction of CT, the factors that influence the quality of a CT image are slice thickness (Z-axis resolution), reconstruction algorithm, field of view, and detector efficiency [6, 43]. Multi-slice CT scanners have isotropic spatial resolution with a 0.5 mm slice thickness [4, 44]. Isotropic spatial resolution means that the spatial resolution in the transaxial plane (X-Y plane) and the longitudinal direction (Z-axis) are equivalent [44]. The isotropic resolution of a given CT image is determined by the axial slice thickness. Thus, thin-sectioned axial image reconstruction can provide high resolution of coronal and sagittal images without additional CT radiation dose. The combination of the axial image with MPR coronal and sagittal images will result in a clear display of the relevant bone structures and provide outlines of complex lesions. Post-processing of CT images create MPRs and 3D reconstructions that provide more detailed images, which are especially critical for diagnosing of traumatic injuries. The image quality of 3D reconstructions and MPR can be improved by using overlapping image reconstruction up to 50% [45].
In the musculoskeletal system, high contrast between bone and soft tissues facilitates detection of lesions using ordinary two-dimensional evaluation modalities. All manufactures provide noise-reducing technologies, such as iterative reconstruction and specific filter algorithms in post-processing of reconstruction in multi-slice CT scanners (e.g., I70f very sharp kernel for Siemens and bone plus for GE). These algorithms can improve the spatial resolution of CT images in skeletal studies. A smaller field of view with thinner slices can produce better sensitivity and diagnostic accuracy of small lesions in the foot, wrist, and orbital cavities [46,47,48]. A balance between the change in slice thickness and image noise should be considered when devising optimized protocols for these applications [49].
Conclusion
This study identified the current status of SPECT/CT of clinical use throughout Korea to provide information for optimization of the CT protocol. Per our findings, CT parameters need to be optimized for the specific regions examined and based on the diagnosis. All practitioners should recognize and understand how each of the variables impacts the radiation dose and image quality so the CT protocol of SPECT/CT can yield optimal results.
References
Delbeke D, Coleman RE, Guiberteau MJ, Brown ML, Royal HD, Siegel BA, et al. Procedure guideline for SPECT/CT imaging 1.0. J Nucl Med. 2006;47:1227–34.
Clinical applications of SPECT/CT: new hybrid nuclear medicine imaging system. IAEA-TECDOC-1597. 2008.
Van den Wyngaert T, Strobel K, Kampen WU, Kuwert T, van der Bruggen W, Mohan HK, et al. The EANM practice guidelines for bone scintigraphy. Eur J Nucl Med Mol Imaging. 2016;43:1723–38.
Dalrymple NC, Prasad SR, El-Merhi FM, Chintapalli KN. Price of isotropy in multi-detector CT. Radiographics. 2007;27:49–62.
The Korean Society of Radiology and Health Insurance Review and Assessment Service. CT Examination and Repeat CT Examination Guidelines. 2013 (Korean) http://www.hira.or.kr/title of subordinate document. Accessed 20. April 2020.
The Korean Society of Radiology and Health Insurance Review and Assessment Service. CT Examination Guidelines for Justification and Optimization. 2012 (Korean) http://nifds.go.kr/brd/title of subordinate document. Accessed 20. April 2020.
Gupta SK, Trethewey S, Brooker B, Rutherford N, Diffey J, Viswanathan S, et al. Radionuclide bone scan SPECT-CT: lowering the dose of CT significantly reduces radiation dose without impacting CT image quality. Am J Nucl Med Mol Imaging. 2017;7:63–73.
Huang K, Feng Y, Liu D, Liang W, Li L. Quantification evaluation of 99mTc-MDP concentration in the lumbar spine with SPECT/CT: compare with bone mineral density. Ann Nucl Med. 2020;34:136–43.
Gaddikeri S, Matesan M, Alvarez J, Hippe DS, Vesselle HJ. MDP-SPECT versus hybrid MDP-SPECT/CT in the evaluation of suspected pars interarticularis fracture in young athletes. J Neuroimaging. 2018;28:635–9.
Tamm AS, Abele JT. Bone and gallium single-photon emission computed tomography-computed tomography is equivalent to magnetic resonance imaging in the diagnosis of infectious spondylodiscitis: a retrospective study. Can Assoc Radiol J. 2017;68:41–6.
Russo VM, Dhawan RT, Dharmarajah N, Baudracco I, Lazzarino AI, Casey AT. Hybrid bone single photon emission computed tomography imaging in evaluation of chronic low back pain: correlation with modic changes and degenerative disc disease. World Neurosurg. 2017;104:816–23.
Russo VM, Dhawan RT, Baudracco I, Dharmarajah N, Lazzarino AI, Casey AT. Hybrid bone SPECT/CT imaging in evaluation of chronic low back pain: correlation with facet joint arthropathy. World Neurosurg. 2017;107:732–8.
Russo VM, Duits A, Dhawan RT, Casey AT. Joint arthropathy at the cranio-vertebral junction. scintigraphic patterns on bone SPECT/CT. Br J Neurosurg. 2017;31:45–9.
Van de Kelft E, Verleye G, Van de Kelft AS, Melis K, Van Goethem J. Validation of topographic hybrid single-photon emission computerized tomography with computerized tomography scan in patients with and without nonspecific chronic low back pain. A prospective comparative study. Spine J. 2017;17:1457–63.
Kato S, Demura S, Matsubara H, Inaki A, Shinmura K, Yokogawa N, et al. Utility of bone SPECT/CT to identify the primary cause of pain in elderly patients with degenerative lumbar spine disease. Orthop Surg Res. 2019;20:185.
Gnanasegaran G, Paycha F, Strobel K, van der Bruggen W, Kampen WU, Kuwert T, et al. Bone SPECT/CT in postoperative spine. Semin Nucl Med. 2018;48:410–24.
Al-Riyami K, Vöö S, Gnanasegaran G, Pressney I, Meir A, Casey A, et al. The role of bone SPECT/CT in patients with persistent or recurrent lumbar pain following lumbar spine stabilization surgery. Eur J Nucl Med Mol Imaging. 2019;46:989–98.
Zhang L, He Q, Jiang M, Zhang B, Zhong X, Zhang R. Diagnosis of insufficiency fracture after radiotherapy in patients with cervical cancer: contribution of technetium Tc 99m-labeled methylene diphosphonate single-photon emission computed tomography/computed tomography. Int J Gynecol Cancer. 2018;28:1369–76.
Duncan I, Ingold N. The clinical value of xSPECT/CT bone versus SPECT/CT. A prospective comparison of 200 scans. Eur J Hybrid Imaging. 2018;2:4.
Bhure U, Roos JE, Pérez Lago MDS, Steurer I, Grünig H, Hug U, et al. SPECT/CT arthrography. Br J Radiol. 2018;91:1082.
Bhure U, Roos JE, Perez-Lago MDS, Strobel K. Single-photon emission computed tomography/computed tomography arthrography of wrist, ankle, and knee joints. Nucl Med Commun. 2020;41:182–8.
Bae S, Kang Y, Song YS, Lee WW. Maximum standardized uptake value of foot SPECT/CT using Tc-99m HDP in patients with accessory navicular bone as a predictor of surgical treatment. Medicine (Baltimore). 2019;98:e14022.
Kampen WU, Westphal F, Van den Wyngaert T, Strobel K, Kuwert T, Van der Bruggen W. SPECT/CT in postoperative foot and ankle pain. Semin Nucl Med. 2018;48:454–68.
Alvelo JL, Papademetris X, Mena-Hurtado C, Jeon S, Sumpio BE, Sinusas AJ, et al. Radiotracer imaging allows for noninvasive detection and quantification of abnormalities in angiosome foot perfusion in diabetic patients with critical limb ischemia and nonhealing wounds. Circ Cardiovasc Imaging. 2018;11:e006932.
Chou TH, Atway SA, Bobbey AJ, Sarac TP, Go MR, Stacy MR. SPECT/CT imaging: a noninvasive approach for evaluating serial changes in angiosome foot perfusion in critical limb ischemia. Adv Wound Care (New Rochelle). 2020;9:103–10.
Claassen L, Yao D, Ettinger S, Lerch M, Daniilidis K, Stukenborg-Colsman C, et al. Relevance of SPECT-CT in complex cases of foot and ankle surgery: a comparison with MRI. Foot Ankle Spec. 2019; https://doi.org/10.1177/1938640019890987.
Lu SJ, Ul Hassan F, Vijayanathan S, Gnanasegaran G. Radionuclide bone SPECT/CT in the evaluation of knee pain: comparing two-phase bone scintigraphy. SPECT and SPECT/CT Br J Radiol. 2018;91:20180168.
Mandegaran R, Agrawal K, Vijayanathan S, Gnanasegaran G. The value of 99mTc-MDP bone SPECT/CT in evaluation of patients with painful knee prosthesis. Nucl Med Commun. 2018;39:397–404.
Verschueren J, Albert A, Carp L, Ceyssens S, Huyghe I, Stroobants, et al. Bloodpool SPECT as part of bone SPECT/CT in painful total knee arthroplasty (TKA): validation and potential biomarker of prosthesis biomechanics. Eur J Nucl Med Mol Imaging. 2019;46:1009–18.
Kim J, Lee HH, Kang Y, Kim TK, Lee SW, So Y, et al. Maximum standardised uptake value of quantitative bone SPECT/CT in patients with medial compartment osteoarthritis of the knee. Clin Radiol. 2017;72:580–9.
De Laroche R, Simon E, Suignard N, Williams T, Henry MP, Robin P, et al. Clinical interest of quantitative bone SPECT-CT in the preoperative assessment of knee osteoarthritis. Medicine (Baltimore). 2018;97:e11943.
Rechsteiner J, Hirschmann MT, Dordevic M, Falkowski AL, Testa EA, Amsler F, et al. Meniscal pathologies on MRI correlate with increased bone tracer uptake in SPECT/CT. Eur Radiol. 2018;28:4696–704.
Egloff C, Huber L, Wurm M, Pagenstert G. No added value using SPECT/CT to analyze persistent symptoms after anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg. 2019;139:807–16.
Van der Bruggen W, Hirschmann MT, Strobel K, Kampen WU, Kuwert T, Gnanasegaran G, et al. SPECT/CT in the postoperative painful knee. Semin Nucl Med. 2018;48:439–53.
Han YH, Jeong HJ, Sohn MH, Yoon SJ, Lim ST. Incidence and severity of femoral head avascularity after femoral neck or intertrochanteric fractures on preoperative bone single photon emission computed tomography/computed tomography: preliminary study. Nucl Med Commun. 2019;40:199–205.
Han S, Oh M, Yoon S, Kim J, Kim JW, Chang JS, et al. Risk stratification for avascular necrosis of the femoral head after internal fixation of femoral neck fractures by post-operative bone SPECT/CT. Nucl Med Mol Imaging. 2017;51:49–57.
Ryoo HG, Lee WW, Kim JY, Kong E, Choi WH, Yoon JK, et al. Minimum standardized uptake value from quantitative bone single-photon emission computed tomography/computed tomography for evaluation of femoral head viability in patients with femoral neck fracture. Nucl Med Mol Imaging. 2019;53:287–95.
Bäcker HC, Steurer-Dober I, Beck M, Agten CA, Decking J, Herzog RF, et al. Magnetic resonance imaging (MRI) versus single photon emission computed tomography (SPECT/CT) in painful total hip arthroplasty: a comparative multi-institutional analysis. Br J Radiol. 2020;93:20190738.
Van den Wyngaert T, Paycha F, Strobel K, Kampen WU, Kuwert T, van der Bruggen W, et al. SPECT/CT in postoperative painful hip arthroplasty. Semin Nucl Med. 2018;48:425–38.
Strobel K, van der Bruggen W, Hug U, Gnanasegaran G, Kampen WU, Kuwert T, et al. SPECT/CT in postoperative hand and wrist pain. Semin Nucl Med. 2018;48:396–409.
Arıcan P, Okudan B, Şefizade R, Naldöken S. Diagnostic value of bone SPECT/CT in patients with suspected osteomyelitis. Mol Imaging Radionucl Ther. 2019;28:89–95.
Thélu-Vanysacker M, Frédéric P, Charles-Edouard T, Alban B, Nicolas B, Tanguy B. SPECT/CT in postoperative shoulder pain. Semin Nucl Med. 2018;48:469–82.
Lee CH, Goo JM, Ye HJ, Ye SJ, Park CM, Chun EJ, et al. Radiation dose modulation techniques in the multidetector CT era: from basics to practice. Radiographics. 2008;28:1451–9.
Tsukagoshi S, Ota T, Fujii M, Kazama M, Okumura M, Johkoh T. Improvement of spatial resolution in the longitudinal direction for isotropic image in helical CT. Phys Med Biol. 2007;52:791–801.
Rogalla P, Kloeters C, Hein PA. CT technology overview: 64-slice and beyond. Radiol Clin N Am. 2009;47:1–11.
Rydberg J, Buckwalter KA, Caldemeyer KS, Phillips MD, Conces DJ, Aisen AM, et al. Multisection CT: scanning techniques and clinical applications. Radiographics. 2000;20:1787–806.
Johnson PT, Fayad LM, Fishman EK. Sixteen slice CT with volumetric analysis of foot fractures. Emerg Radiol. 2006;12:171–6.
Santos DT, Oliveira JX, Vannier MW, Cavalcanti MGP. Computed tomography imaging strategies and perspectives in orbital fractures. J Appl Oral Sci. 2007;15:135–9.
Alshipli M, Kabir NA. Effect of slice thickness on image noise and diagnostic content of single-source-dual energy computed tomography. J Physics: Conf Series. 2017;851012005:1–6.
Acknowledgments
This study was performed as one of the 2018 Quality Control Committee activities of the Korean Society of Nuclear Medicine (KSNM) with cooperation of the Korean Society of Nuclear Medicine Technology (KSNMT). We give special thanks to the members of the KSNMT for participating in this survey, Hong Jae Lee from Seoul National University Hospital, Keun Bae Choe from Hanyang University Hospital, Byung Ho Ahn from Samsung Medical Center, and Soo Young Park from the Catholic University of Korea, Seoul St. Mary’s Hospital.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study design, data collection, and discussion of the result. Data analysis and the first draft were performed by Eun Jung Lee, Ji Young Kim, and Jung Mi Park. Jung Mi Park, Joon-Kee Yoon, and Seong Min Kim commented on revision of the manuscript. All the authors read and approved the first and final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Eun Jeong Lee, Ji Young Kim, Jung Mi Park, Bong-Il Song, Hongyoon Choi, Hye-kyeong Shim, Hye Lim Park, Ho-Young Lee, Kyung Jae Lee, Joon-Kee Yoon, Seongho Seo, Seong Min Kim, Soo Bin Park, Young Seok Cho, Seong Hoon Kim declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent is not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, E.J., Kim, J.Y., Park, J.M. et al. Computed Tomography (CT) Protocols Associated with Cardiac and Bone Single-Photon Emission Computed Tomography/CT (SPECT/CT) in Korea. Nucl Med Mol Imaging 54, 139–146 (2020). https://doi.org/10.1007/s13139-020-00644-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-020-00644-9