Abstract
The current study aimed to evaluate whether patients with different pathologic subtypes of basilar artery occlusion (BAO) stroke could affect the clinical outcome after receiving endovascular treatment (EVT). A total of 187 consecutive patients with acute BAO receiving endovascular treatment (EVT) from January 2012 to July 2018 at the Beijing Tiantan Hospital were recruited in this study. The patients were categorized into three groups: embolism without vertebral artery (VA) steno-occlusion (group 1), in situ atherosclerotic thrombosis (group 2), and embolism from tandem VA steno-occlusion (group 3). Among the 187 patients, 4 patients with embolic combined with ICAS and 1 patient with tandem VA steno-occlusion combined with ICAS were excluded. Of the remaining 182 patients (153 men and 29 women; mean age, 60 years), 43 (23.6%) had embolism without vertebral artery (VA) steno-occlusion (group 1), 116 (63.7%) showed in situ atherosclerotic thrombosis (group 2), and 23 (12.6%) had embolism from tandem VA steno-occlusion (group 3). Overall, successful recanalization (modified thrombolysis in cerebral infarction grade 2b or 3) was achieved in 95.3%, 86.2%, and 60.9% in groups 1, 2, and 3, respectively. The favorable outcome (90-day modified Rankin scale score, 0–3) in the three groups was 51.2%, 52.6%, and 30.4%, respectively. Mortality was higher in group 3 (47.8%) as compared with groups 1 (16.3%) (p = 0.009) and 2 (17.2%) (p = 0.004). Embolism from tandem VA steno-occlusion (group 3) seems to be associated with a lower rate of recanalization and significantly higher rate of mortality as compared with another pathological mechanism of BAO.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute ischemic stroke caused by basilar artery occlusion (BAO) has devastating effects on patients with high morbidity and mortality [1, 2]. Previous studies showed that early recanalization postendovascular treatment (EVT) of acute BAO improves prognosis [3,4,5,6]. However, the efficacy of EVT for patients with different pathological subtypes of BAO remains uncertain [1, 7, 8]. Moreover, acute occlusion of the ostial vertebral artery (VA) and concomitant occlusion of BA (tandem occlusion), as a special type of BAO, seem to predict unfavorable prognosis posttreatment [9,10,11]. Herein, we sought to describe the clinical characteristics and outcome of BAO according to the pathological mechanism of stroke, and assess the EVT feasibility and safety for BAO.
Methods
Patient Selection and Data Collection
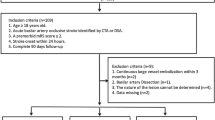
We analyzed consecutive patients with BAO treated by EVT at Beijing Tiantan Hospital from January 2012 to July 2018. Informed consent was obtained from all participants or relatives, and the protocol was approved by the Institutional Review Board of Beijing Tiantan Hospital. Intravenous thrombolysis (IVT) with tissue plasminogen activator (tPA) is given before EVT, which is consistent with the current guidelines. The modality of treatment is a consensus between the neurointerventionalist and the stroke-related caring for the patients according to the pathological mechanism underlying the tandem occlusion and concomitant significant embolic BA occlusion. The inclusion criteria were as follows: the presence of acute neurological symptoms caused by BAO identified by CTA or MRA, time from onset of symptoms to groin puncture ≤ 24 h, baseline National Institutes of Health Stroke Scale score (NIHSS) of ≥ 4, baseline modified Rankin Scale (mRS) score of ≤ 3, no intracranial hemorrhage was detected at initial CT and endovascular treatment by mechanical thrombectomy. Our exclusion criteria were as follows: BAO resulting from other causes such as arterial dissection, vasculitis, or moyamoya disease.
Baseline characteristics, such as age, sex, stroke risk factors including hypertension, diabetes mellitus, hypercholesterolemia, and current smoking, initial stroke severity as evaluated by the NIHSS score, were recorded. Moreover, imaging data, including occlusion sites, the extent of collateral supply on computed tomography (CT) angiogram, magnetic resonance (MR) findings, and postprocedural head CT scan, were also recorded. Interventional data include anesthesia type, medications used during EVT, endovascular techniques, previous use of IVT, type of EVT devices, onset to puncture time, procedure time, onset to recanalization time, and collateral status, and the patients were categorized into three groups according to different etiology. These data were reviewed and analyzed.
Classification of the Stroke Mechanism
Patients with BAO were classified into three groups according to the angiographic findings. Group 1 was defined as those with embolism without vertebral artery (VA) steno-occlusion. Group 2 was defined as those with in situ atherosclerotic thrombosis (ISAT) in the BA, moderate to severe (≥ 50%) stenosis at the target BAO site was found during angiography with or without a tendency for occlusion to recur despite recanalizations. Group 3 was defined as those with embolism from tandem VA steno-occlusion, and > 70% stenosis or occlusion of the VA with impaired distal flow or partial filling of the VA from collaterals was seen during angiography in this classification type.
Endovascular Treatment
The EVTs were performed by a neurointerventionalist with > 50 cases in neurovascular intervention in mechanical thrombectomy for acute ischemic stroke. Cerebral angiography and EVT were performed after general anesthesia, or conscious sedation was administered to the patient. Thrombectomy was selected according to the interventionalist’s discretion. Mechanical thrombectomy was performed with a stent-retriever (Solitaire, Covidien, Irvine, CA, USA; or Trevo stent, Stryker, Kalamazoo, MI, USA) or contact aspiration device (Penumbra, Alameda, Calif; or 5-F Navien intermediate catheter). Patients with tandem occlusion underwent revascularization using clean-road path and dirty-road path (Supplementary Table 1). If the dirty-road was chosen as the access road, a 6-Fr guiding catheter was placed at the proximal subclavian artery. Later, the microguide wire crossed the lesion of VA occlusion or stenosis assisted by a microcatheter or a small balloon. Predilation of the VA lesion was performed using a small balloon, and the 6F guiding catheter was navigated to the V2 segment. Then, the antegrade approach (proximal VA stenting angioplasty, followed by mechanical thrombectomy of BA occlusion) was utilized for the EVT. In the clean-road path, a 6-Fr catheter (Cordis) was passed to the V2 segment and mechanical thrombectomy of BA occlusion was performed.
Patients with tandem VA lesion or underlying BA in situ atherosclerosis undergoing angioplasty and/or stenting received a loading dose of aspirin (300 mg) and clopidogrel (300 mg) orally or via nasogastric tube immediately. Also, intraoperative bridging with intravenous IIb/IIIa inhibitor was given according to the operator’s discretion. Subsequently, dual antiplatelet therapy was maintained for at least 3 months after the procedure, followed by a lifelong monotherapy with aspirin or clopidogrel.
Image Interpretation
The pretreatment neurovascular images include pc-ASPECTS and pons-midbrain index (PMI) based on diffusion-weighted imaging (DWI) and two previous collateral scales described in the setting of BAO (posterior communicating artery (PcomA) [13], American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR)) [14], which were retrospectively interpreted by two independent trained neurointerventionalists blinded to the clinical data (Figs. 1, 2, and 3). A third neuroradiologist with 20 years of experience was involved to resolve any disagreement. All the collateral scales mentioned above were evaluated on digital subtraction angiography (DSA). All the collateral scales mentioned above were evaluated on digital subtraction angiography (DSA).
Angiograms show embolism from tandem VA steno-occlusion. a Right subclavian anteroposterior angiogram shows significant stenosis at orifice of VA (pointed by black arrow). b Left subclavian anteroposterior angiogram shows complete steno-occlusion at the orifice of VA. c Preoperative anteroposterior image of basilar artery shows occlusion of the distal segment(pointed by black arrow). d Postoperative anteroposterior image of basilar artery shows successful recanalization. e Postoperative right subclavian anteroposterior angiogram shows stent placement at the stenotic lesion at orifice of VA (pointed by white arrow)
Outcome Measurement
The primary outcome measures were functional independence and favorable outcome at 90 days after the procedure. Functional independence was defined as a mRS score < 2. The favorable outcome was defined as an mRS score < 3 based on the Basilar Artery International Cooperation Study (BASICS) definition. The mRS score was assessed by blinded trained interviewers over the phone using a standardized interview protocol. The rate of successful recanalization is defined as modified thrombolysis in cerebral ischemia (TICI) grade 2b or 3. The safety end-points were 90-day mortality and rates of any intracerebral hemorrhage and symptomatic intracerebral hemorrhage (sICH). All patients underwent plain CT immediately after endovascular therapy for the detection of intracranial hemorrhage and CT or MRI within of 18–24 h after the EVT. sICH was defined based on the European Cooperative Acute Stroke Study (ECASS) criteria.
Statistical Analysis
Data were collected on standard forms, evaluated for completeness, and double keyed into an EpiData statistics data document. The baseline and outcome data were presented as mean (standard deviation (SD)) and/or median (interquartile range (IQR)) for continuous variables. Frequency and/or proportion were used for categorical variables. The independent samples t test and/or the nonparametric test (Mann-Whitney U test) were used to compare means and/or medians, whereas Pearson’s chi-square test or Fisher’s exact test was used for comparing the frequencies and/or proportions. The logistic regression controlling for potential confounders was used to determine the adjusted odds ratio (aORs) with the corresponding 95% confidence intervals (CIs) for the purpose of assessing the successful recanalization and clinical outcome at 90 days between three groups. All tests were two-tailed and statistical significance was determined at an α level of 0.05. All statistical analyses were performed with the statistical software package R (http://www.R-project.org, The R Foundation) and Empowerstats (http://www.empowerstats.com, X&Y Solutions Inc., Boston, MA, USA).
Results
In this study, 182 patients (153 men and 29 women; mean age: 60 years) were divided into three groups: 43 (23.6%) embolism without vertebral artery (VA) steno-occlusion (group 1), 116 (63.7%) in situ atherosclerotic thrombosis (group 2), and 23 (12.6%) embolism from tandem VA steno-occlusion (group 3). Overall, successful recanalization (modified thrombolysis in cerebral infarction grade 2b or 3) was achieved in 95.3%, 86.2%, and 60.9% in group 1, group 2, and group 3, respectively. The favorable outcome (90-day mRS, 0–3) in the three groups was 51.2%, 52.6%, and 30.4%, respectively. The mortality was higher in group 3 (47.8%) as compared with groups 1 (16.3%) (p = 0.009) and 2 (17.2%) (p = 0.004). The baseline characteristics and procedural and outcome parameters are summarized in Tables 1 and 2. The median time from the last normal to puncture was 8 (IQR 4.4–13) h. In terms of procedural characteristics, stent retrievers were used more frequently (56%) than intra-arterial thrombolysis (28.0%). General anesthesia was used in 78.6% of the cases, and the median procedural length was 2 (IQR 1.5–2) h.
No significant difference was detected in the hemorrhage rate although the mortality rate was significantly increased in the BAO with tandem lesions as compared with groups 1 and 2 (group 1: 16.3%, group 2: 17.2%, group 3: 47.8%; and 1 and 2 p > 0.999, 1 and 3 p = 0.009, 2 and 3 p = 0.004). Moreover, compared with the other cases, tandem vertebrobasilar occlusions appeared as an independent predictor of mortality in patients who also presented a lower recanalization rate (TICI grade 2b or 3) (group 1: 95.3%, group 2: 86.2%, group 3: 60.9%; and group 1 vs group 2 > 0.158, group 1 vs group 3 p < 0.001, group 2 vs group 3 p = 0.007). However, no difference was observed in the favorable outcomes in patients between the three groups (Table 3). After adjustment for potential confounders, logistic regression analysis showed that groups 1 and 2 were associated with more recanalization as compared with group 3 (group 1 vs 3, aOR, 12.964, 95% CI: 2.414–69.618, p = 0.003; group 2 vs 3, aOR, 3.673, 95% CI: 1.312–10.286, p = 0.013) and less mortality (group 1 vs 3, aOR, 0.179; 95% CI: 0.049–0.661, p = 0.01; group 2 vs 3, aOR, 0.213, 95% CI: 0.07–0.646, p = 0.006), but no association was found between functional independence and favorable outcome at 90 days (Table 4).
Discussion
The treatment strategy and outcomes of mechanical thrombectomy for acute ischemic stroke in patients with BAO differed according to the pathologic mechanism. Herein, we found that embolism without VA steno-occlusion (group 1) was associated with distal occlusion, shorter procedure time, a higher rate of successful recanalization, and favorable clinical outcome, while embolism from tandem VA steno-occlusion (group 3) showed the lowest rate of successful recanalization and worse clinical outcome. Although slightly lower recanalization and lower functional independence rate was demonstrated in the in situ atherosclerotic thrombosis group compared with the embolism group, no statistical difference was found in this study.
Currently, only a few studies are available regarding the outcomes of posterior circulation (PC) stroke after endovascular treatment according to the pathological mechanism [11,12,13,14]. Recently, the embolic occlusion of the PC seemed to have benefitted with the advanced mechanical thrombectomy technique and devices and higher recanalization rate than patients with in situ atherosclerotic lesion [12, 13]. In the present study, the recanalization rate of 95.3%, good clinical outcome of 44.2%, and 51.25% of mRS 0–2 and mRS 0–3, and mortality rate of 16.3% were achieved in embolism without VA steno-occlusion group. These results were similar to those of mechanical thrombectomy in the anterior circulation [3].
Moreover, the complexity of in situ atherosclerotic lesions may lead to prolonged procedure time, resulting in poor clinical outcomes [15]. In contrast, no significant difference was detected regarding the procedural time, recanalization rate, and clinical outcome of in situ atherosclerotic lesion group as compared with embolism without VA steno-occlusion group in the present study. Atherosclerotic lesion is one of the common causes of ischemic stroke in Asian population [16,17,18,19]. Interestingly, in situ atherosclerotic lesion was identified in 63.7% of the patients in the current study, which is almost 3 times larger than reported previous study [20]. Moreover, a high recanalization rate of 86.2% was achieved in the current study, which was significantly higher than a previous study (55%) [20]. This result might be attributed to the aggressive approach in our institution, such as combined angioplasty and the use of anticoagulation in this group of patients [21]. Although the most suitable treatment strategy remains elusive in this group, the aggressive approach is safe and feasible in the in situ atherosclerotic lesion group.
The worse outcome and lowest recanalization rate were shown in embolism in the tandem VA group. Several reasonable explanations regarding this result are as follows: a relatively higher thrombus burden in this group caused by an atherosclerotic plaque at the initial segment of the vertebral artery, which results in slow vascular flow and leads to clot formation. Moreover, the occlusion of the initial segment in this group was often based on atherosclerosis and artery dissection, combined with the disadvantage of the anatomical features of the vertebral artery and subclavian artery, rendering it difficult to conduct recanalization treatments as a result of the complex procedure and prolonged procedural time.
Currently, there is no consensus for selecting the access route for the management of embolism from tandem VA steno-occlusion. Uninvolved contralateral VA (clean-road) is considerable in the absence of hypoplastic VA and may allow rapid access and recanalization. The time delay for angioplasty and hemorrhage is of concern if the involved ipsilateral VA (dirty-road) is selected as the access route, and antiplatelets are used to prevent restenosis [20]. In group 3, patients exhibit the limitation of the anatomical conditions, and hence, the recanalization treatment can only adapt the dirty-road path method in embolism from tandem VA steno-occlusion group, which is rather challenging; this might explain the lower recanalization rate and high mortality rate in this study.
Among the 19 patients treated with dirty-road path, 10 cases had contralateral vertebral artery dysplasia or occlusion, 8 cases had contralateral vertebral artery continued as posterior inferior cerebellar artery (PICA), and 1 case had balance contralateral vertebral artery but combined initial segment stenosis. Due to the limitation of the anatomical conditions, the recanalization treatment can only adapt the dirty-road path method, which is rather challenging and could lead to a significantly lower recanalization rate and mortality. Therefore, we suggested that clean-road path should be adopted if the condition allowed as in the present study, wherein 4 patients treated with clean-road path showed complete recanalization. However, additional studies focusing on mechanical thrombectomy through dirty-road path are required to improve the treatment outcome.
Nevertheless, the present study has limitations, such as an uncontrolled sample of patients of our study and the techniques and devices were at the discretion of the operation and advancement. Therefore, the bias in these results is unavoidable. Another limitation is that the underlying comorbidities are drastically different between groups and might also affect the outcome and survival. However, the relatively large number of PC stroke patients included in the current study was sufficient to analyze the characteristics of PC stroke according to the pathological mechanism. Furthermore, the current study cannot represent the global population because atherosclerosis is the main etiological stroke in the Asian population. Nonetheless, this study might provide additional information for the characteristics and outcome of EVT in the Asian population, and we hope that this information is helpful for customized clinical procedures and treatment strategies that would improve the prognosis in PC stroke.
Conclusion
The clinical characteristics and outcomes of BAO in patients who underwent mechanical thrombectomy differ according to the pathological mechanism. Embolism of the BA caused by VA tandem lesions is closely associated with a significantly low rate of recanalization and high mortality, while embolic occlusion and in situ atherosclerotic lesions showed higher recanalization and better prognosis. This classification system might benefit the endovascular treatment strategy for BAO. Nonetheless, further prospective cohort studies in different populations from multiple centers are imperative.
References
Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009;8:724–30.
Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. 2005;76:1238–41.
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15:1138–47.
Glass TA, Hennessey PM, Pazdera L, Chang HM, Wityk RJ, Dewitt LD, et al. Outcome at 30 days in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2002;59:369–76.
De Marchis GM, Kohler A, Renz N, Arnold M, Mono ML, Jung S, et al. Posterior versus anterior circulation strokes: comparison of clinical, radiological and outcome characteristics. J Neurol Neurosurg Psychiatry. 2011;82:33–7.
Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011;10:1002–14.
Singer OC, Berkefeld J, Nolte CH, Bohner G, Haring HP, Trenkler J, et al. Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol. 2015;77:415–24.
Ecker RD, Tsujiura CA, Baker CB, Cushing D. Endovascular reconstruction of vertebral artery occlusion prior to basilar thrombectomy in a series of six patients presenting with acute symptomatic basilar thrombosis. J Neurointerv Surg. 2014;6:379–83.
Hacke W, Zeumer H, Ferbert A, Bruckmann H, del Zoppo GJ. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988;19:1216–22.
Brandt T, von Kummer R, Muller-Kuppers M, Hacke W. Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke. 1996;27:875–81.
Voetsch B, DeWitt LD, Pessin MS, Caplan LR. Basilar artery occlusive disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2004;61:496–504.
Kim YW, Hong JM, Park DG, Choi JW, Kang DH, Kim YS, et al. Effect of intracranial atherosclerotic disease on endovascular treatment for patients with acute vertebrobasilar occlusion. AJNR Am J Neuroradiol. 2016;37:2072–8.
Eckert B, Kucinski T, Pfeiffer G, Groden C, Zeumer H. Endovascular therapy of acute vertebrobasilar occlusion: early treatment onset as the most important factor. Cerebrovasc Dis. 2002;14:42–50.
Lee JS, Lee SJ, Yoo JS, Hong JH, Kim CH, Kim YW, et al. Prognosis of acute intracranial atherosclerosis-related occlusion after endovascular treatment. J Stroke. 2018;20:394–403.
Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014;45:663–9.
Huang YN, Gao S, Li SW, Huang Y, Li JF, Wong KS, et al. Vascular lesions in Chinese patients with transient ischemic attacks. Neurology. 1997;48:524–5.
Mattioni A, Cenciarelli S, Biessels G, van Seeters T, Algra A, Ricci S. Prevalence of intracranial large artery stenosis and occlusion in patients with acute ischaemic stroke or TIA. Neurol Sci. 2014;35:349–55.
De Silva DA, Woon FP, Lee MP, Chen CP, Chang HM, Wong MC. South Asian patients with ischemic stroke: intracranial large arteries are the predominant site of disease. Stroke. 2007;38:2592–4.
Baik SH, Park HJ, Kim JH, Jang CK, Kim BM, Kim DJ. Mechanical thrombectomy in subtypes of basilar artery occlusion: relationship to recanalization rate and clinical outcome. Radiology. 2019;291:730–7.
Gao F, Lo WT, Sun X, Mo DP, Ma N, Miao ZR. Combined use of mechanical thrombectomy with angioplasty and stenting for acute basilar occlusions with underlying severe intracranial vertebrobasilar stenosis: preliminary experience from a single Chinese center. AJNR Am J Neuroradiol. 2015;36:1947–52.
Funding
Beijing Municipal Science and Technology Commision (Z18110000171837) and the National Key Research and Development Program of China (2016YFC1301501) funded the current study.
Author information
Authors and Affiliations
Contributions
XS, XT, YMD, GTM, LGS, LL, and XCH acquired the data. ZRM, NM, and FG were involved in the study design and data interpretation. XS and R drafted the article. XT conducted the statistical analysis. All authors commented on the manuscript regarding the intellectual content.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethics Approval
This study was reviewed and approved by our Institutional Review Board and procedures followed were in accordance with the institutional guidelines and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 37 kb)
Rights and permissions
About this article
Cite this article
Sun, X., Raynald, Tong, X. et al. Analysis of Treatment Outcome After Endovascular Treatment in Different Pathological Subtypes of Basilar Artery Occlusion: a Single Center Experience. Transl. Stroke Res. 12, 230–238 (2021). https://doi.org/10.1007/s12975-020-00833-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-020-00833-w