Abstract
Preconditioning is a paradigm in which sublethal stress–prior to a more injurious insult–induces protection against injury. In the central nervous system (CNS), preconditioning against ischemic stroke is induced by short durations of ischemia, brief seizures, exposure to anesthetics, and other stresses. Increasing evidence supports the contribution of microRNAs (miRNAs) to the pathogenesis of cerebral ischemia and ischemic tolerance induced by preconditioning. Studies investigating miRNA changes induced by preconditioning have to date identified 562 miRNAs that change expression levels after preconditioning, and 15% of these changes were reproduced in at least one additional study. Of miRNAs assessed as changed by preconditioning in more than one study, about 40% changed in the same direction in more than one study. Most of the studies to assess the role of specific miRNAs in the neuroprotective mechanism of preconditioning were performed in vitro, with fewer studies manipulating individual miRNAs in vivo. Thus, while many miRNAs change in response to preconditioning stimuli, the mechanisms underlying their effects are not well understood. The data does suggest that miRNAs may play significant roles in preconditioning-induced neuroprotection. This review focuses on the current state of knowledge of the possible role of miRNAs in preconditioning-induced cerebral protection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral ischemia is a leading cause of death and disability worldwide, and a serious complication during the perioperative period. Preconditioning (PC) is an endogenous neuroprotective response induced by a mild stress or subthreshold stimulus in the brain, including a sublethal duration of ischemia, brief episodes of seizures, and exposure to bioactive pharmaceutical drugs (including anesthetics) given before a subsequent injurious ischemia [1,2,3,4].
It is known that PC induces neuroprotection with two possible time courses. Rapid tolerance happens within minutes after PC and is associated with posttranscriptional modification of proteins and activation of signaling pathways that converge on the mitochondria to reduce cell death [2, 5, 6]. Delayed tolerance develops more slowly with neuroprotection against subsequent injury only evident after about 24 h, peaking at 3 days and diminishing over 1 week [7,8,9]. Delayed tolerance is characterized by a dependence on de novo protein synthesis of heat shock and other proteins [10, 11] and suppression of the transcriptional response to ischemic injury [12]. PC causes a complex reprogramming of the genetic response to ischemic injury, modifying metabolic, cell-cycle regulatory, ion channel, and immunologic pathways [12,13,14].
MicroRNAs (miRNAs) are small non-coding RNAs (~20–22 nucleotides) which regulate gene expression largely at the posttranscriptional level [15,16,17]. MiRNAs modulate mRNA function mainly by binding to complementary sites in the 3′-untranslated region (3′-UTR) of target mRNAs and inhibiting translation or inducing mRNA degradation [18]. However, additional mechanisms have also been demonstrated including miRNA binding to gene promoters in some genes to induce their expression [19] or binding protein-coding regions to alter expression [20]. MiRNAs are abundant in the nervous system where they serve important roles in brain development and neuronal function including synaptic plasticity and neurogenesis as well as in neurodegeneration and neuroinflammation [21,22,23,24,25].
Emerging evidence demonstrates that miRNAs contribute to the pathogenesis of cerebral ischemia [16, 26,27,28,29,30,31,32], representing both endogenous attempts at repair, as well as contributing to pro cell-death pathways. As part of the overall epigenetic control of gene expression, miRNAs also play prominent roles in ischemic tolerance induced by PC [33, 34]. MiRNA profiling has been performed for ischemic PC [26, 35, 36] and ischemic tolerance–the protected state after ischemic injury preceded by brief ischemic or other noxious stimulation [35]–and has demonstrated miRNA-dependent regulation of a number of neuroprotective pathways.
Recent studies in cerebral ischemia models have documented miRNA changes, and modulating an array of miRNAs is neuroprotective experimentally [28, 37,38,39,40,41,42,43,44,45]. The clinical application of ischemic preconditioning in the cardiovascular and central nervous system (CNS) is readily apparent, given its ease of implementation if non-invasive (such as application of a blood pressure cuff to induce remote ischemia). A few preconditioning treatments have been tested clinically [46,47,48,49]. Slagsvold et al. [47] showed that remote ischemic PC preserved mitochondrial function and activated pro-survival kinase Akt in the left ventricle during cardiac surgery. In patients with symptomatic intracranial arterial stenosis, repetitive bilateral arm ischemic PC safely reduced stroke recurrence, protected against brain ischemia, and improved inflammation and coagulation [46]. Tian et al. [48] showed that isoflurane PC in combination with angiotensin-converting enzyme inhibitors (ACEi) additively attenuated myocardial ischemia-reperfusion injury by reducing oxidative stress and inflammation. We and the others are also currently involved in clinical trials for remote ischemic preconditioning in hemorrhagic shock.
While clinical use of PC is in its infancy, preclinical data on its efficacy is extensive. One reason why clinical data is sparse is that many of the models are not practical clinically (i.e., subthreshold seizure induction, brief cerebral ischemia). If the mechanisms of neuroprotection by PC can be parsed out, the eventual goal would be to mimic the effects of PC by directly manipulating the pathways involved pharmacologically. In this review, we sought to clarify the role of miRNAs in PC-induced cerebral protection in preclinical models and evaluate the current state of the field. The paper is organized according to the method of preconditioning used: ischemia, 3-nitropropionic acid (3-NPA), exposure to anesthetic, brief seizures, and hibernation. The potential clinical use of miRNAs to mimic PC for cerebral protection is highlighted.
Ischemic Preconditioning
Several preclinical studies have investigated miRNA changes in ischemic PC (IPC) (Table 1), and while these are summarized in the accompanying tables, we will discuss the salient findings here. Dharap et al. [36] used hypertensive rats subjected to brief middle cerebral artery occlusion (MCAO) to identify miRNAs that change in response to IPC. Of the 265 miRNAs analyzed, 28 were uniquely changed only at 6 h, while 13 miRNAs showed increased expression and 10 miRNAs decreased expression up to 3 days after PC. Of these 23, 3 miRNAs were no longer significantly changed at the 72-h timepoint. Overall miRNA expression changed with time following IPC. Bioinformatic investigation of possible mRNA targets identified Fragile X mental retardation 1, disheveled-axin domain containing 1 (DIXDC1), a protein controlling Wnt signaling and synaptic structure, and ubiquitin carboxyl-terminal hydrolase 1(UCHL1), an emerging neuroinjury biomarker responsible for protein degradation targeted by several miRNAs upregulated by PC [36]. These likely play a role in IPC-induced ischemic tolerance and possibly neurogenesis. MiRNAs downregulated after IPC targeted methyl CpG-binding protein 2 (MeCP2) and Fas ligand (Faslg) 1L [36]. These changes might also play a role in PC-induced neuroprotection [50, 51]. Notably, Wnt signaling plays a critical role in cell survival during neuronal development, making epigenetic modulation of this pathway by PC intriguing [52, 53]. MiRNA-21, one of the upregulated miRNAs identified by Dharap and colleagues, was also shown to be upregulated in rat MCAO by another group [38]. Buller et al. found that overexpression of miR-21 protects against ischemic neuronal death through downregulation of Faslg, an important cell death-inducing ligand targeted by miR-21 in vitro [38].
Sun et al. [54] identified several miRNAs that increased with a preconditioning stimulus of sublethal global ischemia in gerbils. Their work identified 43 kDa transactivation response DNA-binding protein (TDP43), fused in sarcoma/translocated in liposarcoma (FUS/TLS), and heat shock protein 70 kDa (HSP70) as potential mRNA targets. This group demonstrated the neuroprotective role of these proteins in a previous investigation [55]. Other corroborative work has shown that miR-132, which targets FUS/TLS, increased and peaked at post-injury day 1, but was subsequently downregulated from 7 days to 6 months after ischemia [54]. Of interest, this investigation found that three repeated episodes of preconditioning more rapidly induced miRNA expression; however, this three-dose protocol also led to neuronal loss in CA1 of the hippocampus, in contrast to a single exposure. This complicates interpretation of the data, as their findings with the three-dose protocol may be more related to miRNAs involved in neuronal death, rather than protection.
In a study investigating the miRNA profile in mouse cortex following IPC, Lee et al. found that the miR-200 family (miR-200a, miR-200b, miR-200c, miR-141, and miR-429) and the miR-182 family (miR-182, miR-183, and miR-96) were upregulated early (i.e., 3 h) after IPC [26] with protection linked to downregulation of prolyl hydroxylase 2 (PHD2). As the prolyl hydroxylases play a critical role in the degradation of hypoxia inducible factors (HIFs), HIF stabilization and transcription of its target proteins might have played a critical role in this investigation. In contrast, our lab demonstrated that post-stroke increases in miR-200c increased neuronal cell death through inhibiting reelin expression (an extracellular matrix glycoprotein modulating synaptogenesis and neuronal migration), while downregulation of miR-200c protected against neuronal injury by enhancing reelin expression in vivo and in vitro [28].
Liu et al. [56] demonstrated significantly altered expression of 17 miRNAs, with 4 upregulated and 13 downregulated in the cerebral cortex of hypoxic PC (HPC) mice. HPC with subsequent ischemia (HPC+MCAO) reversed the upregulation of miR-30a seen following HPC or ischemia alone. Others have suggested that downregulation of miRNA-30a alleviates neuronal injury by enhancing beclin1-mediated autophagy in N-2a cells after oxygen glucose deprivation (OGD) [41]. Downregulation of miR-30a by antagomir to miR-30a also prevented neural ischemic injury through upregulating glucose-regulated protein of 78 kDa/binding immunoglobulin protein GRP78/BIP expression in vivo and in vitro [42]. There is also a potential role for protein kinases. Bioinformatic analysis suggested 19 miRNAs were differentially expressed following HPC and MCAO including ones regulating protein kinase C (PKC) βII, PKCϒ, and nPKCε-interacting protein [56].
Another study, by Lusardi et al., investigating miRNA changes with ischemic preconditioning in mice identified transcriptional and translational regulators as prominent targets of miRNAs altered by IPC, with the largest number of miRNAs targeting methyl CpG binding protein 2 (MeCP2) [35]. These investigators reported that IPC neuroprotection is associated with downregulation of miR-132 and increased MeCP2 protein in the mouse cortex 24 h after ischemic PC without altering MeCP2 mRNA levels. The investigators suggested that IPC leads to depression of miR-132 resulting in increased synthesis of MeCP2 protein [35] which participates in down regulation of some of the transcriptional responses to ischemia. They focused on miR-132 of the 287 profiled miRNAs altered after PC, because of its effects on MeCP2 expression in neurons [57]. However, their results are not sufficient to define how important miRNA-132 is for IPC, as they did not manipulate any individual miRNAs to investigate their impact on IPC or ischemia. In contrast, Hwang et al. reported that overexpression of miR-132 affords neuroprotection against global ischemia-induced neuronal death in in vivo and in vitro models of ischemia [58].
The miR181 family of miRNAs has also garnered a lot of interest in ischemia and preconditioning. While Lusardi et al. [35] identified miR-181a, b, and c as downregulated with IPC, Lee et al. reported that miR-181a and c were upregulated [59], and Dharap et al. reported that miR-181b and d were upregulated [36]. Peng et al. [60] demonstrated neuroprotection against ischemic injury by downregulating miR-181b which in turn upregulated GRP78/BIP and UCHL1 in mice after PC. Indeed, GRP78/BIP antagonizes neuronal apoptosis induced by ischemic brain injuries [61, 62]. UCHL1 is a potential biomarker of traumatic brain injury, involved in a cellular pathway responsible for the ubiquitination and degradation of damaged proteins [63,64,65]. Intracerebroventricular (ICV) injection of miRNA-181b antagomir increased GRP78/BIP and UCHL1, decreased neuronal cell loss, and reduced neurological deficits 24 h after MCAO [60]. Further, we [40] investigated the effect of increased miR-181a and found that increased miR-181a targeted GRP78/BIP and increased injury. GRP78/BIP is a central participant in ER-dependent protein folding, being one of the three arms of the unfolded protein response, as well as having a role in autophagy and inhibition of apoptosis [66]. Consistent with this, inhibition of miR-181a provided neuroprotection from ischemia, increasing the levels of GRP78/BIP in a mouse MCAO model [40]. In rat forebrain ischemia, untreated rats showed increased miR-181a levels and decreased Bcl-2 protein in hippocampal CA1 [39]. Notably, miR-181a antagomir enhanced CA1 neuron survival, increased pro-survival Bcl-2 protein, and prevented the decrease of glutamate transporter 1 (GLT-1) characteristic of selective loss of CA1 neurons [39]. Lastly, we found [67] that post-stroke treatment with miR-181a antagomir was neuroprotective, increasing levels of the apoptotic inhibitory proteins Bcl2 and XIAP in mice. Collectively, the miR181 family appears to play an integral role in the neuronal apoptotic response to ischemia and is influenced by preconditioning stimuli.
In vitro ischemic PC is typically performed using OGD (Table 2) and is known to change a number of different cell survival pathways. Similar to PC effects of brief ischemia in whole animal preparations, sublethal in vitro OGD as a form of PC using neuroblastoma (N-2a) cells resulted in upregulation of the miR-200 family, resulting in increased cell survival and downregulated PHD2 levels, again highlighting the involvement of HIF regulatory pathways in IPC [26]. In accordance with the aforementioned animal data, another N-2a cell OGD model demonstrated that overexpression of miR-181b promoted OGD-induced cell death with decreased GRP78/BIP and UCHL1 [60]. This is also consistent with other in vitro studies of miR-181a, another member of miR-181 family, that suggest a regulatory role in cerebral ischemia. Inhibition of miR-181a was shown to provide neuroprotection by targeting GRP78/BIP [40] or Bcl-2 in vitro [39].
The migration of neural progenitor cells is also thought to play an important role in neuronal repair from ischemia. Relevant to this, Shin et al. [68] demonstrated that a decrease in miR27b after stimulation with ischemic brain extract (IBE) increased the expression of its target mRNA and protein, stromal cell-derived factor 1 (SDF-1), critical for progenitor migration. This effect was mediated, interestingly, via miR-223, which itself downregulated miR-27b. This is an interesting example of epi-epi-genetic modulation. Other investigators have highlighted SDF-1 as conferring neuroprotection and synaptic modulation after ischemic injury [69, 70] using primary rat astrocytes. Lastly, knockdown and inhibition of CXCR2, a chemokine receptor, inhibited the IBE-induced miR-223 expression and abolished IBE-mediated SDF-1 expression, suggesting that CXCR2 is required for the increased expression of miR-223 and subsequent SDF-1 induction [68].
Chemical Preconditioning with 3-Nitropropionic Acid
Chemical preconditioning using 3-NPA, an inhibitor of succinate dehydrogenase, was used by Xu et al. [71] to investigate the role of miR-199a. This form of PC was associated with downregulation of miR-199a and protection from subsequent MCAO [71]. The expression of miR-199a during ischemic PC showed region specific timecourses. In cortex and striatum, miR-199a was downregulated on the second and fourth day after PC, while in the hippocampus, it was only downregulated the second day after PC [71]. Another study investigating altered miRNA expression following PC induced by 3-NPA showed that decreased miR-33a significantly reduced infarct volume in rats [72].
Volatile Anesthetic Preconditioning
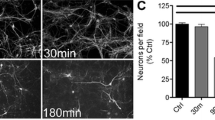
Cerebral ischemia is a serious complication that can occur in the perioperative period. Volatile anesthetics such as sevoflurane have been found to have preconditioning neuroprotective effects against ischemic injury in experimental settings [73,74,75,76]. To date, few studies have investigated a possible role for miRNAs in anesthetic PC. Cao et al. [77] showed that 2% isoflurane exposure for 1 h is neuroprotective and significantly increased miR-350 and miR-647-3p in rats. A study investigating the neuroprotective effect of sevoflurane PC with 2.4% sevoflurane for 30 min per day on four consecutive days, showed that sevoflurane PC was associated with decreased miR-15b expression and increased Bcl-2 protein in rats [78]. ICV injection of Bcl-2 inhibitor following sevoflurane PC and MCAO significantly increased infarct volume, although there was surprisingly no effect on ischemic infarct in the absence of sevoflurane PC, suggesting a role for Bcl-2 in sevoflurane PC.
Anesthetic preconditioning and its associated modulation of miRNAs have also been demonstrated in vitro. In B-35 cells, a neuroblastoma cell line, isoflurane PC significantly increased miR-203 expression, significantly reducing OGD-induced cell injury. This suggests miR-203 may be a target for isoflurane in the brain [77]. Overexpression of miRNA-203 increased phospho-Akt, a kinase important in survival signaling in response to growth factors; this mechanism might similarly mediate isoflurane-induced neuroprotection [79]. The increased activation/phosphorylation of Akt induced by miR-203 overexpression may also be a mechanism by which miR-203 increases the tolerance of cells to OGD.
Shi et al. [78] demonstrated a critical role for miR-15b in sevoflurane-dependent PC (Table 2). Ischemic injury to cortical neurons in their model upregulated miR-15b, suppressing the expression of the pro-survival protein Bcl-2; this was reversed with sevoflurane preconditioning. Sun et al. [80] further identified miRNAs altered after 30 min exposure to 2% sevoflurane using pheochromocytoma-12 (PC-12) cells, which have a characteristically neuronal phenotype [81, 82]. In this study, sevoflurane PC induced neuroprotection by downregulation of miR-101a and upregulation of miR-34b. Overexpression of miR-101a or administration of miR-34b inhibitor significantly enhanced apoptosis of hypoxic PC-12 cells [80].
Epileptic Preconditioning
Brain injury secondary to status epilepticus can also be reduced by preceding brief seizures [83]. One study profiled miRNAs in a model of epileptic tolerance, that is, mice were given intraperitoneal kainic acid to induce brief seizures for PC followed 24 h later by status epilepticus induced with intra-amygdalar kainic acid [84] and compared to mice only subjected to status epilepticus. Changes in miRNA levels were assessed 24 h after status epilepticus, and 23% of miRNA expression was increased while 77% decreased in the tolerant state compared to control [84]. This contrasted to the status epilepticus alone which compared with control had many more upregulated compared to downregulated miRNAs. With preconditioning and subsequent severe seizures (tolerance), one miRNA was uniquely upregulated (15 in the non-preconditioned mice) and eight miRNAs were uniquely downregulated. Expression of miR-27a, 200a, and 326 were increased in the injured, non-preconditioned mice, but decreased in the preconditioned animals, suggesting a specific role for these miRNAs in epileptic preconditioning-induced tolerance. MiR-132, which plays a role in regulating neuronal structure [85, 86], was upregulated after status epilepticus in the hippocampal subfield CA3, but this was prevented in preconditioned mice. When miR-132 antagomir was injected ICV, it was found to increase neuronal survival after status epilepticus [84].
McKiernan et al. profiled changes in miRNAs following preconditioning seizures alone [87]. Seizure PC increased 39 miRNAs and the most upregulated miRNA was miR-184. Upregulation of miR-184 was shown to contribute to neuroprotection by epileptic PC, as ICV injection of mir-184 antagomir increased neuronal cell death despite epileptic PC. MiR-9, another upregulated miRNA in epileptic PC, was found to be neuroprotective in mouse MCAO when upregulated and associated with decreased Bcl2-l1 protein and reduced neuronal apoptosis in OGD-treated hippocampal neurons [43].
Hibernation
Hibernation is a state of natural tolerance to ischemia. Hibernating mammals lower their energy consumption, breathing, blood flow, and body temperature, but have no cerebral ischemia despite what would under normal conditions be a lethal level of cerebral blood flow [88]. It has been reported that massive global SUMOylation, a form of posttranscriptional protein modification with the small ubiquitin-related modifier (SUMO), occurs during hibernation in the brains of ground squirrels [89]. SUMOylation is involved in ischemic tolerance in human neuroblastoma cells and primary cortical neuronal cultures in rats and mice [90, 91]. However, the ischemic tolerance level induced by SUMOylation did not reach the degree of tolerance to brain hypoperfusion seen during hibernation [89], so there are likely additional factors participating in protection in combination with SUMOylation. Lee et al. [59] showed that two miRNA families (the miR-200 and 182 families) were downregulated and miR-34 and miR-206 were upregulated in ground squirrels during hibernation torpor. They demonstrated that inhibition of the miR-200 family and/or miR-182 family in human neuroblastoma SHSY5Y cells increases protein conjugation by several ubiquitin-like protein modifiers (ULMs), which are increased in the brains of ground squirrels during hibernation torpor, and reduces OGD-induced cell death in this neuronal cell line [59].
Discussion
The above evidence suggests ischemic preconditioning has a highly heterogeneous and complex effect on miRNA expression. We have attempted to summarize the relatively large body of data, focusing on parsing out the consistencies. In total, 562 miRNAs were reported to change expression after PC in the nine studies listed in Table 3. Of these, 79 miRs were reported in two studies, 13 in three (Table 4). The single miR reported changed in four studies, miR-34b, was increased in all four, suggesting it may play an important role. Mir-34b is interesting as it plays a role in brain development [92] and in Parkinson’s disease [93] as well as regulating apoptosis of astrocytes in the setting of seizures [94]. Of 79 miRNAs reported changed in two studies, 44% reported the same direction of change (increased or decreased) in both. In the case of three reports (13 miRNAs), 38% reported change in the same direction. Thus, while there are clues from this work on possible candidate miRNAs, it remains difficult to identify a small target group of miRNAs given that bi-directionality of change was frequently observed.
The studies reviewed here used different experimental designs, including different PC stimuli, in vivo or in vitro models, different species, cell types, timing, and number of miRNAs assessed. These differences likely underlie some of these differences in outcomes. Of the different preconditioning paradigms, MCAO was used in three studies. Useful data comes from the work of Lusardi et al. [35], who used microarray probes that contained 489 miRNAs in IPC by brief MCAO in vivo. They found that 180 miRNAs were increased and 93 miRNAs were decreased, 24 h after IPC in three male mice. Another useful array study reported by Dharap et al. [36] measured 265 miRNAs at three time points (6, 24, and 72 h) after IPC (also brief MCAO) in six hypertensive male rats. Many of these miRNAs differed in the direction of change from the work done by Lusardi’s group, making firm conclusions difficult.
In addition to different designs and models, challenges have been identified in performing miRNA research. Proper validation of hybridization, amplification, and interpretation is required [95]. While a full discussion of the unique challenges of miRNA research is beyond the scope of this paper, we direct the reader to the excellent article by Witwer and Halushka for further discussion [95].
The effect of manipulation of individual miRNAs is also inconsistent across studies. Lusardi et al. [35] suggested that decreased miR-132 expression correlated with increased MeCP2 and induced neuroprotection following ischemic PC in mice. Jimenez-Mateos et al. [83] also investigated miRNA-132 and reported that it was increased after status epilepticus but not increased after status epilepticus following seizure PC. They did not test the effect of PC alone. Decreased miR-132 by the use of miR-132 antagomir ICV injection induced neuroprotection from seizure [83]. However, Hwang et al. [58] showed that miR-132 overexpression by injection of lentiviral miR-132 increased neuron survival following global ischemia in rats. They also suggested that miR-132 overexpression decreased cell death following OGD in vitro [58]. Notably, there are nuances to transfecting or introducing miRNAs or their inhibitors into cells. The supraphysiologic overexpression of miRNAs obtained by transfection may have different biologic effects [95]. Mayya et al. have shown that miRNAs work in a variable dose-dependent fashion with their mRNA binding sites [96]. If the miRNA is at a low concentration, it may modulate only a subset of genes, whereas at high concentrations, it may find additional mRNA binding sites. The effects of levels of expressions likely impact biologic pathways in different ways [95].
Reasonably consistent results supporting mechanisms for the role of three families have been identified. Both in vitro and in vivo studies have consistently demonstrated that miRNA-181 (a and b) targets the stress protein GRP78/BIP, which plays a critical role in the unfolded protein response and inhibition of apoptosis. Ischemic preconditioning from various labs, using diverse models, have shown changes in levels of miR-181-a, b, c, and d; however, the direction of changes and specific family members is not always consistent between reports (see Tables 3 and 4). Stabilization or increased levels of GRP78/BIP provide neuroprotection from subsequent lethal stimuli when exogenous miR-181 antagomirs are transfected into cells or administered ICV [39, 40, 60]. Two other compelling miRNA families affected by ischemic preconditioning that appears promising for translational therapy are the miR-200 and miR-182 families, reported changed by both hibernation and ischemic PC (see Tables 1 and 4). Both of these families are implicated in protein conjugation with ubiquitin-like protein modifiers, such as SUMO, and increased protein conjugation by these modifiers is associated with protection from ischemia, and with the resistance to ischemia seen in hibernation [26, 59]. In addition, the miR-200 family was shown to target PDH2 leading to increased levels of HIF-1α [26], an additional established protective mechanism.
Off-target effects remain an issue for therapeutic applications of miRNAs, and empiric tests for miRNAs with assessment of off-target effects are needed [97]. MiRNAs can target multiple mRNAs, but most current miRNA studies focus on one miRNA and one selected target, for which interaction and silencing is demonstrated [98]. In fact, often multiple miRNAs target a single mRNA, just as miRNAs have many different mRNA targets. Therefore, the binding of a miRNA to a target mRNA is dependent on the cell type and physiologic state [98]. Assessment of multiple pathways regulated by a particular miRNA should be performed. This is important in the development of successful miRNA-based therapeutics.
Conclusions
Several laboratories have performed miRNA profiling studies using different models of PC. However, there are still few reports demonstrating the therapeutic effects of miRNAs by artificially induced overexpression and/or inhibition of miRNAs during PC. Most of the validation studies suggesting miRNAs contribute to PC-induced cell resistance were performed in vitro. Further, many investigations identified upregulated miRNAs during preconditioning and subsequently tested those miRNAs in ischemic models. However, there is a paucity of data manipulating individual miRNAs during the preconditioning phase. Although in vitro studies provide useful information, more in vivo observations are needed to make advances towards the development of clinical therapies. MiRNA changes likely play important roles in PC-induced neuroprotection, but the limited consistent evidence is not sufficient to understand the extent of their contribution. To clarify the significance of miRNAs in PC-induced neuroprotection, further in vivo investigations for specific miRNAs are required. Once a clearer picture is obtained manipulating miRNAs in vivo, PC might eventually be mimicked via exogenous miRNA mimic or inhibitor delivery. The use of miRNAs in clinical practice is already emerging in clinical trials, so the identification of candidate miRNAs involved in PC is likely to have a high chance of clinical translation.
References
Dirnagl U, Becker K, Meisel A. Preconditioning and tolerance against cerebral ischaemia: from experimental strategies to clinical use. The Lancet Neurology. 2009;8(4):398–412. doi:10.1016/s1474-4422(09)70054-7.
Dirnagl U, Meisel A. Endogenous neuroprotection: mitochondria as gateways to cerebral preconditioning? Neuropharmacology. 2008;55(3):334–44. doi:10.1016/j.neuropharm.2008.02.017.
McDonough A, Weinstein JR. Neuroimmune response in ischemic preconditioning. Neurotherapeutics: the journal of the American Society for Experimental NeuroTherapeutics. 2016;13(4):748–61. doi:10.1007/s13311-016-0465-z.
Stevens SL, Vartanian KB, Stenzel-Poore MP. Reprogramming the response to stroke by preconditioning. Stroke. 2014;45(8):2527–31. doi:10.1161/STROKEAHA.114.002879.
Meller R, Thompson SJ, Lusardi TA, Ordonez AN, Ashley MD, Jessick V, et al. Ubiquitin proteasome-mediated synaptic reorganization: a novel mechanism underlying rapid ischemic tolerance. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2008;28(1):50–9. doi:10.1523/jneurosci.3474-07.2008.
Bhuiyan MI, Kim YJ. Mechanisms and prospects of ischemic tolerance induced by cerebral preconditioning. International neurourology journal. 2010;14(4):203–12. doi:10.5213/inj.2010.14.4.203.
Kaneko T, Yokoyama K, Makita K. Late preconditioning with isoflurane in cultured rat cortical neurones. Br J Anaesth. 2005;95(5):662–8. doi:10.1093/bja/aei228.
Stenzel-Poore MP, Stevens SL, King JS, Simon RP. Preconditioning reprograms the response to ischemic injury and primes the emergence of unique endogenous neuroprotective phenotypes: a speculative synthesis. Stroke. 2007;38(2 Suppl):680–5. doi:10.1161/01.STR.0000251444.56487.4c.
Kitagawa K, Matsumoto M, Tagaya M, Hata R, Ueda H, Niinobe M, et al. 'Ischemic tolerance' phenomenon found in the brain. Brain Res. 1990;528(1):21–4.
Barone FC, White RF, Spera PA, Ellison J, Currie RW, Wang X, et al. Ischemic preconditioning and brain tolerance: temporal histological and functional outcomes, protein synthesis requirement, and interleukin-1 receptor antagonist and early gene expression. Stroke. 1998;29(9):1937–50. discussion 50-1
Obrenovitch TP. Molecular physiology of preconditioning-induced brain tolerance to ischemia. Physiol Rev. 2008;88(1):211–47. doi:10.1152/physrev.00039.2006.
Stenzel-Poore MP, Stevens SL, Xiong Z, Lessov NS, Harrington CA, Mori M, et al. Effect of ischaemic preconditioning on genomic response to cerebral ischaemia: similarity to neuroprotective strategies in hibernation and hypoxia-tolerant states. Lancet (London, England). 2003;362(9389):1028–37. doi:10.1016/s0140-6736(03)14412-1.
Stenzel-Poore MP, Stevens SL, Simon RP. Genomics of preconditioning. Stroke. 2004;35(11 Suppl 1):2683–6. doi:10.1161/01.STR.0000143735.89281.bb.
Garcia-Bonilla L, Benakis C, Moore J, Iadecola C, Anrather J. Immune mechanisms in cerebral ischemic tolerance. Front Neurosci. 2014;8:44. doi:10.3389/fnins.2014.00044.
Ambros V. The functions of animal microRNAs. Nature. 2004;431(7006):350–5. doi:10.1038/nature02871.
Ouyang YB, Stary CM, Yang GY, Giffard R. MicroRNAs: innovative targets for cerebral ischemia and stroke. Curr Drug Targets. 2013;14(1):90–101.
Barwari T, Joshi A, Mayr M. MicroRNAs in cardiovascular disease. J Am Coll Cardiol. 2016;68(23):2577–84. doi:10.1016/j.jacc.2016.09.945.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–33. doi:10.1016/j.cell.2009.01.002.
Place RF, Li LC, Pookot D, Noonan EJ, Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc Natl Acad Sci U S A. 2008;105(5):1608–13. doi:10.1073/pnas.0707594105.
Duursma AM, Kedde M, Schrier M, le Sage C, Agami R. MiR-148 targets human DNMT3b protein coding region. RNA (New York, NY). 2008;14(5):872–7. doi:10.1261/rna.972008.
Cardoso AL, Guedes JR, de Lima MC. Role of microRNAs in the regulation of innate immune cells under neuroinflammatory conditions. Curr Opin Pharmacol. 2016;26:1–9. doi:10.1016/j.coph.2015.09.001.
Meza-Sosa KF, Pedraza-Alva G, Perez-Martinez L. MicroRNAs: key triggers of neuronal cell fate. Front Cell Neurosci. 2014;8:175. doi:10.3389/fncel.2014.00175.
Stappert L, Roese-Koerner B, Brustle O. The role of microRNAs in human neural stem cells, neuronal differentiation and subtype specification. Cell Tissue Res. 2015;359(1):47–64. doi:10.1007/s00441-014-1981-y.
Su W, Aloi MS, Garden GA. MicroRNAs mediating CNS inflammation: small regulators with powerful potential. Brain Behav Immun. 2016;52:1–8. doi:10.1016/j.bbi.2015.07.003.
Singh T, Jauhari A, Pandey A, Singh P, Pant AB, Parmar D, et al. Regulatory triangle of neurodegeneration, adult neurogenesis and microRNAs. CNS & neurological disorders drug targets. 2014;13(1):96–103.
Lee ST, Chu K, Jung KH, Yoon HJ, Jeon D, Kang KM, et al. MicroRNAs induced during ischemic preconditioning. Stroke. 2010;41(8):1646–51. doi:10.1161/strokeaha.110.579649.
Ouyang YB, Giffard RG. MicroRNAs regulate the chaperone network in cerebral ischemia. Transl Stroke Res. 2013;4(6):693–703. doi:10.1007/s12975-013-0280-3.
Stary CM, Xu L, Sun X, Ouyang YB, White RE, Leong J, et al. MicroRNA-200c contributes to injury from transient focal cerebral ischemia by targeting Reelin. Stroke. 2015;46(2):551–6. doi:10.1161/strokeaha.114.007041.
Zeng L, Liu J, Wang Y, Wang L, Weng S, Tang Y, et al. MicroRNA-210 as a novel blood biomarker in acute cerebral ischemia. Frontiers in bioscience (Elite edition). 2011;3:1265–72.
Ziu M, Fletcher L, Rana S, Jimenez DF, Digicaylioglu M. Temporal differences in microRNA expression patterns in astrocytes and neurons after ischemic injury. PLoS One. 2011;6(2):e14724. doi:10.1371/journal.pone.0014724.
Dharap A, Bowen K, Place R, Li LC, Vemuganti R. Transient focal ischemia induces extensive temporal changes in rat cerebral microRNAome. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2009;29(4):675–87. doi:10.1038/jcbfm.2008.157.
Saugstad JA. Non-coding RNAs in stroke and neuroprotection. Front Neurol. 2015;6:50. doi:10.3389/fneur.2015.00050.
Jimenez-Mateos EM. Role of microRNAs in innate neuroprotection mechanisms due to preconditioning of the brain. Front Neurosci. 2015;9:118. doi:10.3389/fnins.2015.00118.
Thompson JW, Dave KR, Young JI, Perez-Pinzon MA. Ischemic preconditioning alters the epigenetic profile of the brain from ischemic intolerance to ischemic tolerance. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 2013;10(4):789–97. doi:10.1007/s13311-013-0202-9.
Lusardi TA, Farr CD, Faulkner CL, Pignataro G, Yang T, Lan J, et al. Ischemic preconditioning regulates expression of microRNAs and a predicted target, MeCP2, in mouse cortex. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2010;30(4):744–56. doi:10.1038/jcbfm.2009.253.
Dharap A, Vemuganti R. Ischemic pre-conditioning alters cerebral microRNAs that are upstream to neuroprotective signaling pathways. J Neurochem. 2010;113(6):1685–91. doi:10.1111/j.1471-4159.2010.06735.x.
Hu K, Xie YY, Zhang C, Ouyang DS, Long HY, Sun DN, et al. MicroRNA expression profile of the hippocampus in a rat model of temporal lobe epilepsy and miR-34a-targeted neuroprotection against hippocampal neurone cell apoptosis post-status epilepticus. BMC Neurosci. 2012;13:115. doi:10.1186/1471-2202-13-115.
Buller B, Liu X, Wang X, Zhang RL, Zhang L, Hozeska-Solgot A, et al. MicroRNA-21 protects neurons from ischemic death. FEBS J. 2010;277(20):4299–307. doi:10.1111/j.1742-4658.2010.07818.x.
Moon JM, Xu L, Giffard RG. Inhibition of microRNA-181 reduces forebrain ischemia-induced neuronal loss. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2013;33(12):1976–82. doi:10.1038/jcbfm.2013.157.
Ouyang YB, Lu Y, Yue S, Xu LJ, Xiong XX, White RE, et al. MiR-181 regulates GRP78 and influences outcome from cerebral ischemia in vitro and in vivo. Neurobiol Dis. 2012;45(1):555–63. doi:10.1016/j.nbd.2011.09.012.
Wang P, Liang J, Li Y, Li J, Yang X, Zhang X, et al. Down-regulation of miRNA-30a alleviates cerebral ischemic injury through enhancing beclin 1-mediated autophagy. Neurochem Res. 2014;39(7):1279–91. doi:10.1007/s11064-014-1310-6.
Wang P, Zhang N, Liang J, Li J, Han S, Li J. Micro-RNA-30a regulates ischemia-induced cell death by targeting heat shock protein HSPA5 in primary cultured cortical neurons and mouse brain after stroke. J Neurosci Res. 2015;93(11):1756–68. doi:10.1002/jnr.23637.
Wei N, Xiao L, Xue R, Zhang D, Zhou J, Ren H, et al. MicroRNA-9 mediates the cell apoptosis by targeting Bcl2l11 in ischemic stroke. Mol Neurobiol. 2015; doi:10.1007/s12035-015-9605-4.
Zhou X, Su S, Li S, Pang X, Chen C, Li J, et al. MicroRNA-146a down-regulation correlates with neuroprotection and targets pro-apoptotic genes in cerebral ischemic injury in vitro. Brain Res. 2016;1648(Pt A):136–43. doi:10.1016/j.brainres.2016.07.034.
Duris K, Lipkova J. The role of microRNA in ischemic and hemorrhagic stroke. Current drug delivery 2016.
Meng R, Ding Y, Asmaro K, Brogan D, Meng L, Sui M, et al. Ischemic conditioning is safe and effective for octo- and nonagenarians in stroke prevention and treatment. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. 2015;12(3):667–77. doi:10.1007/s13311-015-0358-6.
Slagsvold KH, Moreira JB, Rognmo O, Hoydal M, Bye A, Wisloff U, et al. Remote ischemic preconditioning preserves mitochondrial function and activates pro-survival protein kinase Akt in the left ventricle during cardiac surgery: a randomized trial. Int J Cardiol. 2014;177(2):409–17. doi:10.1016/j.ijcard.2014.09.206.
Tian Y, Li H, Liu P, Xu JM, Irwin MG, Xia Z, et al. Captopril pretreatment produces an additive cardioprotection to isoflurane preconditioning in attenuating myocardial ischemia reperfusion injury in rabbits and in humans. Mediat Inflamm. 2015;2015:819232. doi:10.1155/2015/819232.
Wang Y, Reis C, Applegate R 2nd, Stier G, Martin R, Zhang JH. Ischemic conditioning-induced endogenous brain protection: applications pre-, per- or post-stroke. Exp Neurol. 2015;272:26–40. doi:10.1016/j.expneurol.2015.04.009.
Guicciardi ME, Gores GJ. Life and death by death receptors. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2009;23(6):1625–37. doi:10.1096/fj.08-111005.
Urdinguio RG, Sanchez-Mut JV, Esteller M. Epigenetic mechanisms in neurological diseases: genes, syndromes, and therapies. The Lancet Neurology. 2009;8(11):1056–72. doi:10.1016/s1474-4422(09)70262-5.
Chen S, Guttridge DC, You Z, Zhang Z, Fribley A, Mayo MW, et al. Wnt-1 signaling inhibits apoptosis by activating beta-catenin/T cell factor-mediated transcription. J Cell Biol. 2001;152(1):87–96.
Li F, Chong ZZ, Maiese K. Winding through the WNT pathway during cellular development and demise. Histol Histopathol. 2006;21(1):103–24.
Sun M, Yamashita T, Shang J, Liu N, Deguchi K, Feng J, et al. Time-dependent profiles of microRNA expression induced by ischemic preconditioning in the gerbil hippocampus. Cell Transplant. 2015;24(3):367–76. doi:10.3727/096368915x686869.
Sun M, Yamashita T, Shang J, Liu N, Deguchi K, Liu W, et al. Acceleration of TDP43 and FUS/TLS protein expressions in the preconditioned hippocampus following repeated transient ischemia. J Neurosci Res. 2014;92(1):54–63. doi:10.1002/jnr.23301.
Liu C, Peng Z, Zhang N, Yu L, Han S, Li D, et al. Identification of differentially expressed microRNAs and their PKC-isoform specific gene network prediction during hypoxic pre-conditioning and focal cerebral ischemia of mice. J Neurochem. 2012;120(5):830–41. doi:10.1111/j.1471-4159.2011.07624.x.
Klein ME, Lioy DT, Ma L, Impey S, Mandel G, Goodman RH. Homeostatic regulation of MeCP2 expression by a CREB-induced microRNA. Nat Neurosci. 2007;10(12):1513–4. doi:10.1038/nn2010.
Hwang JY, Kaneko N, Noh KM, Pontarelli F, Zukin RS. The gene silencing transcription factor REST represses miR-132 expression in hippocampal neurons destined to die. J Mol Biol. 2014;426(20):3454–66. doi:10.1016/j.jmb.2014.07.032.
Lee YJ, Johnson KR, Hallenbeck JM. Global protein conjugation by ubiquitin-like-modifiers during ischemic stress is regulated by microRNAs and confers robust tolerance to ischemia. PLoS One. 2012;7(10):e47787. doi:10.1371/journal.pone.0047787.
Peng Z, Li J, Li Y, Yang X, Feng S, Han S, et al. Downregulation of miR-181b in mouse brain following ischemic stroke induces neuroprotection against ischemic injury through targeting heat shock protein A5 and ubiquitin carboxyl-terminal hydrolase isozyme L1. J Neurosci Res. 2013;91(10):1349–62. doi:10.1002/jnr.23255.
Choi AY, Choi JH, Yoon H, Hwang KY, Noh MH, Choe W, et al. Luteolin induces apoptosis through endoplasmic reticulum stress and mitochondrial dysfunction in neuro-2a mouse neuroblastoma cells. Eur J Pharmacol. 2011;668(1–2):115–26. doi:10.1016/j.ejphar.2011.06.047.
Yuan Y, Guo Q, Ye Z, Pingping X, Wang N, Song Z. Ischemic postconditioning protects brain from ischemia/reperfusion injury by attenuating endoplasmic reticulum stress-induced apoptosis through PI3K-Akt pathway. Brain Res. 2011;1367:85–93. doi:10.1016/j.brainres.2010.10.017.
Ciechanover A, Brundin P. The ubiquitin proteasome system in neurodegenerative diseases: sometimes the chicken, sometimes the egg. Neuron. 2003;40(2):427–46.
Dennissen FJ, Kholod N, van Leeuwen FW. The ubiquitin proteasome system in neurodegenerative diseases: culprit, accomplice or victim? Prog Neurobiol. 2012;96(2):190–207. doi:10.1016/j.pneurobio.2012.01.003.
Papa L, Akinyi L, Liu MC, Pineda JA, Tepas JJ 3rd, Oli MW, et al. Ubiquitin C-terminal hydrolase is a novel biomarker in humans for severe traumatic brain injury. Crit Care Med. 2010;38(1):138–44. doi:10.1097/CCM.0b013e3181b788ab.
Ni M, Zhang Y, Lee AS. Beyond the endoplasmic reticulum: atypical GRP78 in cell viability, signalling and therapeutic targeting. The Biochemical journal. 2011;434(2):181–8. doi:10.1042/bj20101569.
Xu LJ, Ouyang YB, Xiong X, Stary CM, Giffard RG. Post-stroke treatment with miR-181 antagomir reduces injury and improves long-term behavioral recovery in mice after focal cerebral ischemia. Exp Neurol. 2015;264:1–7. doi:10.1016/j.expneurol.2014.11.007.
Shin JH, Park YM, Kim DH, Moon GJ, Bang OY, Ohn T, et al. Ischemic brain extract increases SDF-1 expression in astrocytes through the CXCR2/miR-223/miR-27b pathway. Biochim Biophys Acta. 2014;1839(9):826–36. doi:10.1016/j.bbagrm.2014.06.019.
Ardelt AA, Bhattacharyya BJ, Belmadani A, Ren D, Miller RJ. Stromal derived growth factor-1 (CXCL12) modulates synaptic transmission to immature neurons during post-ischemic cerebral repair. Exp Neurol. 2013;248:246–53. doi:10.1016/j.expneurol.2013.06.017.
Miller JT, Bartley JH, Wimborne HJ, Walker AL, Hess DC, Hill WD, et al. The neuroblast and angioblast chemotaxic factor SDF-1 (CXCL12) expression is briefly up regulated by reactive astrocytes in brain following neonatal hypoxic-ischemic injury. BMC Neurosci. 2005;6:63. doi:10.1186/1471-2202-6-63.
Xu WH, Yao XY, Yu HJ, Huang JW, Cui LY. Downregulation of miR-199a may play a role in 3-nitropropionic acid induced ischemic tolerance in rat brain. Brain Res. 2012;1429:116–23. doi:10.1016/j.brainres.2011.10.007.
Feng Y, Li W, Wang JQ. MicroRNA-33A expression is reduced in cerebral cortex in a rat model of ischemic tolerance. Cellular and molecular biology (Noisy-le-Grand, France). 2015;61(3):24–9.
Payne RS, Akca O, Roewer N, Schurr A, Kehl F. Sevoflurane-induced preconditioning protects against cerebral ischemic neuronal damage in rats. Brain Res. 2005;1034(1–2):147–52. doi:10.1016/j.brainres.2004.12.006.
Wang H, Lu S, Yu Q, Liang W, Gao H, Li P, et al. Sevoflurane preconditioning confers neuroprotection via anti-inflammatory effects. Frontiers in bioscience (Elite edition). 2011;3:604–15.
Yang Q, Dong H, Deng J, Wang Q, Ye R, Li X, et al. Sevoflurane preconditioning induces neuroprotection through reactive oxygen species-mediated up-regulation of antioxidant enzymes in rats. Anesth Analg. 2011;112(4):931–7. doi:10.1213/ANE.0b013e31820bcfa4.
Yu Q, Chu M, Wang H, Lu S, Gao H, Li P, et al. Sevoflurane preconditioning protects blood-brain-barrier against brain ischemia. Frontiers in bioscience (Elite edition). 2011;3:978–88.
Cao L, Feng C, Li L, Zuo Z. Contribution of microRNA-203 to the isoflurane preconditioning-induced neuroprotection. Brain Res Bull. 2012;88(5):525–8. doi:10.1016/j.brainresbull.2012.05.009.
Shi H, Sun BL, Zhang J, Lu S, Zhang P, Wang H, et al. MiR-15b suppression of Bcl-2 contributes to cerebral ischemic injury and is reversed by sevoflurane preconditioning. CNS & neurological disorders drug targets. 2013;12(3):381–91.
Li L, Zuo Z. Isoflurane postconditioning induces neuroprotection via Akt activation and attenuation of increased mitochondrial membrane permeability. Neuroscience. 2011;199:44–50. doi:10.1016/j.neuroscience.2011.10.022.
Sun Y, Li Y, Liu L, Wang Y, Xia Y, Zhang L, et al. Identification of miRNAs involved in the protective effect of sevoflurane preconditioning against hypoxic injury in PC12 cells. Cell Mol Neurobiol. 2015;35(8):1117–25. doi:10.1007/s10571-015-0205-7.
Das KP, Freudenrich TM, Mundy WR. Assessment of PC12 cell differentiation and neurite growth: a comparison of morphological and neurochemical measures. Neurotoxicol Teratol. 2004;26(3):397–406. doi:10.1016/j.ntt.2004.02.006.
Gozal E, Sachleben LR Jr, Rane MJ, Vega C, Gozal D. Mild sustained and intermittent hypoxia induce apoptosis in PC-12 cells via different mechanisms. Am J Physiol Cell Physiol. 2005;288(3):C535–42. doi:10.1152/ajpcell.00270.2004.
Jimenez-Mateos EM, Henshall DC. Seizure preconditioning and epileptic tolerance: models and mechanisms. Int J Physiol Pathophysiol pharmacol. 2009;1(2):180–91.
Jimenez-Mateos EM, Bray I, Sanz-Rodriguez A, Engel T, McKiernan RC, Mouri G, et al. miRNA expression profile after status epilepticus and hippocampal neuroprotection by targeting miR-132. Am J Pathol. 2011;179(5):2519–32. doi:10.1016/j.ajpath.2011.07.036.
Edbauer D, Neilson JR, Foster KA, Wang CF, Seeburg DP, Batterton MN, et al. Regulation of synaptic structure and function by FMRP-associated microRNAs miR-125b and miR-132. Neuron. 2010;65(3):373–84. doi:10.1016/j.neuron.2010.01.005.
Magill ST, Cambronne XA, Luikart BW, Lioy DT, Leighton BH, Westbrook GL, et al. MicroRNA-132 regulates dendritic growth and arborization of newborn neurons in the adult hippocampus. Proc Natl Acad Sci U S A. 2010;107(47):20382–7. doi:10.1073/pnas.1015691107.
McKiernan RC, Jimenez-Mateos EM, Sano T, Bray I, Stallings RL, Simon RP, et al. Expression profiling the microRNA response to epileptic preconditioning identifies miR-184 as a modulator of seizure-induced neuronal death. Exp Neurol. 2012;237(2):346–54. doi:10.1016/j.expneurol.2012.06.029.
Frerichs KU, Hallenbeck JM. Hibernation in ground squirrels induces state and species-specific tolerance to hypoxia and aglycemia: an in vitro study in hippocampal slices. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 1998;18(2):168–75. doi:10.1097/00004647-199802000-00007.
Lee YJ, Miyake S, Wakita H, McMullen DC, Azuma Y, Auh S, et al. Protein SUMOylation is massively increased in hibernation torpor and is critical for the cytoprotection provided by ischemic preconditioning and hypothermia in SHSY5Y cells. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2007;27(5):950–62. doi:10.1038/sj.jcbfm.9600395.
Lee YJ, Castri P, Bembry J, Maric D, Auh S, Hallenbeck JM. SUMOylation participates in induction of ischemic tolerance. J Neurochem. 2009;109(1):257–67. doi:10.1111/j.1471-4159.2009.05957.x.
Lee YJ, Mou Y, Maric D, Klimanis D, Auh S, Hallenbeck JM. Elevated global SUMOylation in Ubc9 transgenic mice protects their brains against focal cerebral ischemic damage. PLoS One. 2011;6(10):e25852. doi:10.1371/journal.pone.0025852.
Wu J, Bao J, Kim M, Yuan S, Tang C, Zheng H, et al. Two miRNA clusters, miR-34b/c and miR-449, are essential for normal brain development, motile ciliogenesis, and spermatogenesis. Proc Natl Acad Sci U S A. 2014;111(28):E2851–7. doi:10.1073/pnas.1407777111.
Mouradian MM. MicroRNAs in Parkinson's disease. Neurobiol Dis. 2012;46(2):279–84. doi:10.1016/j.nbd.2011.12.046.
Liu L, Liu L, Shi J, Tan M, Xiong J, Li X, et al. MicroRNA-34b mediates hippocampal astrocyte apoptosis in a rat model of recurrent seizures. BMC Neurosci. 2016;17(1):56. doi:10.1186/s12868-016-0291-6.
Witwer KW, Halushka MK. Towards the promise of microRNAs - enhancing reproducibility and rigor in microRNA research. RNA Biol. 2016; doi:10.1080/15476286.2016.1236172.
Mayya VK, Duchaine TF. On the availability of microRNA-induced silencing complexes, saturation of microRNA-binding sites and stoichiometry. Nucleic Acids Res. 2015;43(15):7556–65. doi:10.1093/nar/gkv720.
Aagaard L, Rossi JJ. RNAi therapeutics: principles, prospects and challenges. Adv Drug Deliv Rev. 2007;59(2–3):75–86. doi:10.1016/j.addr.2007.03.005.
Greenberg DS, Soreq H. MicroRNA therapeutics in neurological disease. Curr Pharm Des. 2014;20(38):6022–7.
Acknowledgements
This study was funded by R01 NS 084396, R01 NS 053898, and R01 NS 080177 to Dr. Rona G. Giffard Ph.D. M.D.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Bell, J.D., Cho, JE. & Giffard, R.G. MicroRNA Changes in Preconditioning-Induced Neuroprotection. Transl. Stroke Res. 8, 585–596 (2017). https://doi.org/10.1007/s12975-017-0547-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-017-0547-1