Abstract
Leukoaraiosis (LA) is associated with structural and functional cerebrovascular impairment, which may compromise the capacity of ischemic tissue to maximize reperfusion after intravenous thrombolysis (IVT). We aimed to determine whether severe LA is correlated with reperfusion inefficiency, which contributes to infarct growth and poor functional outcome. We analyzed data from our consecutive acute ischemic stroke (AIS) patients who had acquired baseline and 24-h follow-up diffusion- and perfusion-weighted imaging. Reperfusion was defined as reduction of ≥70 % of hypoperfusion lesion at 24 h from baseline. Severe LA was defined as Fazekas score 2 or 3 on FLAIR images. We investigated the relationship between severity of LA and reperfusion status. Multivariate statistical analysis was carried out for modeling the independent predictors of reperfusion, infarct growth, and functional outcome. Finally, 79 patients were included, among them 30 (37.97 %) had severe LA. Reperfusion was observed in 41 (51.89 %) patients, the proportion of reperfusion was very similar in patients with and without severe LA (53.33 vs 51.02 %, p = 1.000). Large artery occlusion was the only independent unfavorable predictor for reperfusion (OR = 0.202, 95 % confidence interval, 0.060–0.673; p = 0.014). Multiple linear regression analysis revealed that severe LA was independently associated with infarct growth (standardized coefficients = 0.191, p = 0.040). Severe LA was also an independent predictor of poor outcome (mRS ≥ 3) (OR = 4.004, 95 % confidence interval, 1.267–12.656, p = 0.018) after adjusting for reperfusion and baseline severity of stroke. Severe LA was associated with infarct growth and poor outcome independent of reperfusion status, which may expand the notion that LA contributes the intrinsic vulnerability of brain tissue to acute ischemic insults. The burden of LA may not serve as an imaging indicator of reperfusion inefficiency after IVT for AIS patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As a marker of chronic hypoperfusion, leukoaraiosis (LA), also known as white matter hyperintensities (WMH), has been associated with early neurologic deterioration and unfavorable functional outcome after acute ischemic stroke (AIS) [1, 2], but its potential mechanism is uncertain. One proposed pathophysiologic explanation is that extensive LA links to large lesion size and increased susceptibility of infarct growth after AIS [3, 4]. However, it is not clear whether this adverse connection could be modulated by reperfusion process.
Previous studies found that the degree of LA was inversely correlated with the patency of collateral flow [4, 5], which could provide retrograde blood flow for cerebral reperfusion when the main feeding artery was occluded. Subjects with severe LA also exhibited increased hypercoagulability [6], platelet activation [7], oxidative stress, and inflammation [8], which may facilitate the formation of microemboli contributing to the failure of reperfusion. In addition, cerebrovascular reactivity and dynamic autoregulation function have been suggested to be compromised in severe LA [9, 10], which was consistent with the histopathological findings of vascular changes featured with arteriolosclerosis, tortuous arterioles, venous collagenosis, and endothelium dysfunction [11–13]. Hence, it seems conceivable to speculate that chronic cerebrovascular injury marked by LA would render the ischemic brain tissue response inefficiently to the limited blood flow restored from collateral circulation or re-opened arteries, and then contributes to infarct expansion and worse clinical outcome.
Actually, for AIS patients with severe LA, the clinical outcome is still discouraging even after reperfusion therapy [14, 15]. If the burden of LA truly negates the beneficial effects of reperfusion therapy via improving reperfusion, current practice of intravenous thrombolysis (IVT) or endovascular thrombectomy may be seriously re-evaluated for patients with severe LA. Therefore, the purpose of the present study was to determine whether severe LA associates with reperfusion inefficiency after IVT, and then contributes to infarct growth and poor outcome.
Subjects and Methods
Study Subjects
We retrospectively reviewed our prospectively collected database for consecutive patients with AIS received thrombolytic therapy between September 2009 and June 2015. We then enrolled patients who (1) had a diagnosis of ischemic stroke confirmed by diffusion-weighted imaging (DWI) within anterior circulation; (2) received IVT within 6 h from symptom onset; (3) underwent admission and follow-up multimodal MRI; (4) had perfusion-weighted imaging (PWI) lesion volume ≥10 ml and ≥120 % of the DWI lesion volume; and (5) had premorbid modified Rankin scale (mRS) score ≤2; we excluded (1) patients who were treated with combined endovascular thrombectomy and IVT and (2) patients whose assessment of lesion volume was not possible due to extensive hemorrhagic conversion, massive brain edema, brain surgery (hemicraniectomy), or severe motion artifact. Intravenous rtPA (Alteplase 0.9 mg/kg up to a maximum of 90 mg) was used with 10 % of the total dosage as a bolus and the rest over 1 h.
We retrieved demographic, clinical, laboratory, and imaging data including age, sex, comorbid conditions such as history of hypertension, diabetes mellitus, hyperlipidemia, coronary heart disease, atrial fibrillation and transient ischemic attack (TIA) or stroke; time interval from stroke onset to imaging and IVT treatment; National Institutes of Health Stroke Scale (NIHSS) score, systolic blood pressure (SBP), diastolic blood pressure (DBP), serum platelet, and glucose level before IVT; and mRS score after 3 months. Poor outcome was defined as mRS ≥3 at 3 months, while good outcome as mRS <3.
MRI Acquisition
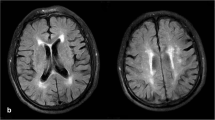
All subjects underwent multi-model MRI on a 3.0T system (Signa Excite HD, General Electric Medical System, Milwaukee, WI) equipped with an 8 channel–phased array head coil, including DWI, PWI, Fluid-attenuated-inversion-recovery (FLAIR), and time-of-flight magnetic resonance angiography (TOF-MRA). FLAIR parameters were TR = 9000 ms, TE = 150 ms, inversion time = 2250 ms, and slice thickness = 5.0 mm. DWI parameters were repetition time [TR] = 4000 ms, echo time [TE] = 69.3 ms, b value = 1000 s/mm2, slice thickness = 5.0 mm, and interslice gap = 1.0 mm. PWI were obtained using the standard bolus passage of contrast method by injecting gadolinium (0.1 mmol/kg dose via power injector). PWI parameters were TR = 1500 ms, TE = 30 ms, and slice thickness = 5.0 mm. TOF-MRA consisted of three slabs with TR = 20 ms, TE = 3.2 ms, flip angle = 15°, and slice thickness = 1.4 mm.
Image Analysis
Baseline and 24-h follow-up DWI and PWI data were reprocessed and calculated with commercial software (MIStar; Apollo Medical Imaging Technology, Melbourne, VIC, Australia). Quantitative perfusion maps of Tmax (the time until the residue function reaches its peak) were generated and Tmax ≥6 s was defined as hypoperfusion lesion. ADC <600 × 106 s/mm2 was defined as infarct lesion. Reperfusion ratio = (baseline hypoperfusion lesion volume − 24-h hypoperfusion lesion volume) / baseline hypoperfusion lesion volume. Reperfusion was defined as reperfusion ratio ≥70 % [16]. Infarct growth was calculated as the increased infarct lesion volume at 24 h from baseline. Large artery occlusion was defined as occlusion located in the responsible M1 segment of the middle cerebral artery (MCA) or internal carotid artery (ICA) identified on baseline MRA. LA severity was rated visually by using the Fazekas scale on FLAIR images [17], and severe LA was defined as either (early) confluent deep WMH (Fazekas score 2 or 3) or irregular periventricular WMH extending into the deep white matter (Fazekas score 3). DWI, PWI, and MRA data were investigated by Q.C. The classification of LA severity was completed by two observers separately, and disagreement was resolved by consensus. A single trained observer (S.Y.) evaluated and classified the LA severity of all 79 patients twice, at an interval of 3 months apart. Another observer (S.Z.) independently made the evaluation once. They were blinded to all other imaging and clinical data.
Statistical Analysis
All numeric variables were expressed as mean ± SD and median (interquartile range). Fisher exact test was used to compare the dichotomous variables between groups, whereas independent samples 2-tailed t test or Mann–Whitney U test were used for the continuous variables, as appropriate. Pearson or Spearman correlation analysis was used depending on the normality of the distribution. Variables with a p value of <0.1 in univariate analyses were included in the multivariate analysis except for the severity of LA which would be forced into multivariate analysis. A backward elimination multiple linear regression model was developed for analysis of independent association between severity of LA and the volume of infarct growth. Because the volume of infarct growth did not conform to normal distribution, it was log-transformed before being introduced to the model. Binary logistic regression analysis was carried out for modeling the independent predictors of reperfusion and poor outcome. A level of p < 0.05 was considered statistically significant. All statistical analyses were performed by IBM SPSS Statistics 21.
Results
A total of 90 patients were eligible for inclusion criteria, and 11 patients were excluded due to the following reasons: combined endovascular and IVT therapy (n = 3), hemorrhagic conversion or massive edema on the follow-up images (n = 3), hemicraniectomy (n = 2), and poor image quality due to severe motion artifact (n = 3). Thus, the remaining 79 patients were included for the final analysis. Demographic, clinical, and laboratory data were not different between included and excluded patients, except that the baseline NIHSS score was higher in excluded patients (median 8 vs 15, p = 0.021).
Among the included patients, 30 (37.97 %) had severe LA. The inter-observer and intra-observer reliabilities about the classification of LA severity were excellent (intraclassk = 0.868 and 0.894, respectively). The demographic, clinical, and imaging characteristics dichotomized by severe LA were demonstrated in Table 1. In univariate analysis, there was no significant difference of baseline NIHSS score, baseline and follow-up infarct, and hypoperfusion lesion volume between groups with and without severe LA. However, patients with severe LA had doubled proportion of patients with poor outcome at 3 month (60 vs 28.6 %, p = 0.009).
Relationship between Severity of LA and Reperfusion
Table 1 showed that there was no significant difference of reperfusion status between groups with and without severe LA in univariate analysis. Binary logistic regression model revealed that large artery occlusion was the only independent unfavorable predictor for reperfusion (OR = 0.202, 95 % confidence interval, 0.060–0.673; p = 0.014), when the severity of LA was forced into analysis (OR = 1.132; 95 % confidence interval, 0.349–3.677; p = 0.836) (Supplementary Table I).
Relationship between Severity of LA and Infarct Growth
Univariate analysis demonstrated that the median volume of infarct growth was inclined to be larger in patients with severe LA, compared to patients without severe LA (17.17 vs 5.12 ml, p = 0.168). After adjusting for baseline systolic blood pressure, baseline NIHSS score, baseline infarct volume, and reperfusion, multiple linear regression analysis confirmed the independent association between severe LA and large infarct growth (standardized coefficients = 0.191, p = 0.040) (Table 2).
Relationship between Severity of LA and Functional Outcome
Patients with poor outcome were older and had higher rate of severe LA, higher admission systolic blood pressure, higher baseline NIHSS score, larger baseline and follow-up infarct volume, and lower proportion of reperfusion in univariate analysis (Supplementary Table II). Severe LA was an independent predictor for poor outcome at 3 month (odds ratio, 4.004; 95 % confidence interval, 1.267–12.656; p = 0.018) after adjusting for above covariates in binary logistic regression model (Table 3). Reperfusion was also negatively associated with poor outcome (odds ratio, 0.235; 95 % confidence interval, 0.071–0.780; p = 0.018). Even for patients with severe LA, reperfusion was still independently associated with good outcome (OR = 4.225; 95 % confidence interval, 1.282–14.085; p = 0.018).
Discussion
To our knowledge, there is no previous work which has investigated the direct relationship between the burden of LA and reperfusion status after IVT. In this study, we firstly found that the severity of LA did not affect the level of reperfusion after IVT. Surprisingly, we further found that pre-existing severe LA was associated with infarct growth and poor outcome. Therefore, we posited that the relationship between severe LA and poor outcome was independent of reperfusion status.
It has long been speculated that the susceptibility of infarct growth in advanced LA may be due to impairment of capability of ischemic brain tissue to maximize reperfusion with limited blood flow restored spontaneously or by means of recanalization therapy. However, we did not find the relationship between severity of LA and the level of reperfusion. A couple of previous studies have adjusted recanalization status as covariates when investigating the independent relationship between the severity of LA and the size of infarct lesion or clinical outcome [4, 14]. But substantial evidences demonstrated that reperfusion outperformed recanalization in predicting infarct growth and outcomes after AIS [18]. Approximately one quarter of AIS patients with successful recanalization may fail to get adequate reperfusion [19].
The modulation process of reperfusion is complex and elusive, which depends on the elaborate coordination of microvascular reactivity and focal metabolic condition in addition to the status of recanalization. Severe LA may represent compromised vasoreactivity and endothelium dysfunction, which seems plausible to account for limited vasodilation in response to reduced blood flow [20], thus leading to reperfusion insufficiency. But an alternative scenario is that enhanced vasodilation may also happen in certain vessels with reduced vascular tone in severe LA patients, even giving rise to excessive reperfusion as the blood pressure was greatly elevated in acute phase of AIS. One may also argue that the disparity of reperfusion capability might manifest shortly after acute ischemic event before the cerebrovascular reactivity or autoregulation function is re-equalized by acute ischemic damage to the vascular wall [21], while reperfusion assessed 24 h after onset may be too late to detect the distinction. However, the comparative baseline hypoperfusion lesion size measured in patients with and without severe LA also made this explanation less likely. Actually, our results were supported by previous findings that hypoperfusion volume was not different within 24 h after onset in patients with intracranial large artery occlusion when stratified by LA severity [4].
We found that severe LA was independently associated with large infarct growth, which was consistent with a previous study which demonstrated that the burden of LA indicated the susceptibility of initially ischemic brain tissue progress to final irreversible infarcts [3]. We further revealed that this relationship between severe LA and infarct expansion was independent of reperfusion status, which indicated that LA itself may contribute the intrinsic vulnerability of brain tissue to ischemic injury. The pre-existing diffuse cerebral and vascular pathology in patients with severe LA may reduce its ischemic tolerance [11, 22]. Another possible mechanism is that acute cerebral ischemia and reperfusion injury may exacerbate the pre-existing disruption of the blood brain barrier (BBB) of severe LA patients [23, 24]. Increased permeability of the BBB would aggravate the process of edema, inflammation, and cytotoxicity, prompting infarct growth or even hemorrhagic transformation [25].
LA severity was also revealed to be a pivotal predictor of post-stroke outcome. The presence of decreased neuronal network connectivity due to demyelination, loss of axons, and cortical thinning would impair plasticity and inhibit recovery for patients with severe LA [11, 26], besides the large infarct expansion. Furthermore, LA is a well-known risk factor for premorbid or post-stroke cognitive impairment and depression [27, 28], which would also adversely affect patients’ compliance with treatment and rehabilitation programs. A recent study also gave support to this finding, which revealed that severe periventricular LA was associated with poor motor function outcome, whereas deep LA grade was inversely correlated with cognitive function outcome following inpatient convalescent rehabilitation after adjusting for initial severity and age [29]. Future translational implication may focus on the relationship between the decreased neuronal network connectivity due to severe LA and cognitive or motor function.
Actually, several studies have associated the burden of LA with poor outcome after AIS, even if they have received recanalization therapy (IVT or endovascular thrombectomy) [14, 15], which might indicate that improving reperfusion level could not adequately reverse the unfavorable destination for patients with severe LA. However, it is worth noting that this situation should not discourage any efforts to gain reperfusion for these patients, because both severity of LA and reperfusion were the two major independent predictors of clinical outcome. According to our data, the odds ratio (OR) was 4.225 for poor outcome of severe LA patients who failed to get reperfusion, compared with their counterparts achieving reperfusion. In a sense, successful reperfusion is more urgently needed for those patients with severe LA to achieve good outcome.
The strengths of our study are the evaluation of reperfusion performed at a relative fixed interval (24 h after IVT) with high-resolution PWI. By taking reperfusion status into account, our result that the negative effect of LA itself on outcome was independent of reperfusion response may expand on the evidence of intrinsic vulnerability of LA to ischemia. Besides, we classified the severity of LA on FLAIR images by the widely used “Fazekas scale,” which is easy to learn and fast to handle, with excellent inter- or intra-rater agreement. By comparison, volumetric measurement of LA lesions is time-intensive, whereas CT-based visual grading systems have the lower sensitivity than FLAIR images could offer. Furthermore, the DWI-based definition of infarct volume in the present study was much more reliable than the previously used computed tomography perfusion (CTP)-based quantification of infarct core.
Our study also has several limitations. Firstly, although we prospectively collected data using a stroke registry, our study had a retrospective design, which might pose selection bias. In order to control measurement error of reperfusion and infarct growth, we also excluded the patients with mismatch <120 % or PWI lesion volume <10 ml, which would limit the generalizability of our results. Secondly, we did not set the patients with absolute absence of LA as controls, which may limit the power to detect the effects of LA. However, it is difficult to conduct such comparison for the extremely high prevalence of LA (96.2 % in our data vs 94.6 % as reported) in ischemic stroke patients [30]. Thirdly, we could not evaluate recanalization status of each individual for the occlusion site of some patients was invisible on admission MRA. Theoretically, the results of no relationship between severity of LA and reperfusion could not be attributed to the confounding effect of recanalization, since it tends to bias the positive results other than negative ones. Finally, the study was performed at a single center with modest sample size. The complex interaction between chronic cerebrovascular injury marked by LA and reperfusion process also needs further investigation in larger cohorts.
Conclusion
Severe LA did not have an effect on the achievement of reperfusion, and its association with infarct growth and poor outcome was independent of reperfusion status after IVT. This finding may expand the notion that LA contributes the intrinsic vulnerability of brain tissue to acute ischemic insults. LA could not serve as an imaging indicator of reperfusion inefficiency after IVT for AIS patients.
References
Arsava EM, Rahman R, Rosand J, Lu J, Smith EE, Rost NS, et al. Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke. Neurology. 2009;72(16):1403–10. doi:10.1212/WNL.0b013e3181a18823.
Feng C, Tan Y, Wu YF, Xu Y, Hua T, Huang J, et al. Leukoaraiosis correlates with the neurologic deterioration after small subcortical infarction. J Stroke Cerebrovasc Dis : Off J Nat Stroke Assoc. 2014;23(6):1513–8. doi:10.1016/j.jstrokecerebrovasdis.2013.12.032.
Ay H, Arsava EM, Rosand J, Furie KL, Singhal AB, Schaefer PW, et al. Severity of leukoaraiosis and susceptibility to infarct growth in acute stroke. Stroke; J Cereb Circ. 2008;39(5):1409–13. doi:10.1161/STROKEAHA.107.501932.
Henninger N, Lin E, Haussen DC, Lehman LL, Takhtani D, Selim M, et al. Leukoaraiosis and sex predict the hyperacute ischemic core volume. Stroke; J Cereb Circ. 2013;44(1):61–7. doi:10.1161/STROKEAHA.112.679084.
Giurgiutiu DV, Yoo AJ, Fitzpatrick K, Chaudhry Z, Leslie-Mazwi T, Schwamm LH, et al. Severity of leukoaraiosis, leptomeningeal collaterals, and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke. J Neurointerventional surg. 2015;7(5):326–30. doi:10.1136/neurintsurg-2013-011083.
Tomimoto H, Akiguchi I, Wakita H, Osaki A, Hayashi M, Yamamoto Y. Coagulation activation in patients with Binswanger disease. Arch Neurol. 1999;56(9):1104–8. doi:10.1001/archneur.56.9.1104.
Iwamoto T, Kubo H, Takasaki M. Platelet activation in the cerebral-circulation in different subtypes of ischemic stroke and Binswangers-disease. Stroke; J Cereb Circ. 1995;26(1):52–6.
Xu H, Stamova B, Jickling G, Tian Y, Zhan X, Ander BP, et al. Distinctive RNA expression profiles in blood associated with white matter hyperintensities in brain. Stroke; J Cereb Circ. 2010;41(12):2744–9. doi:10.1161/STROKEAHA.110.591875.
Uh J, Yezhuvath U, Cheng Y, Lu H. In vivo vascular hallmarks of diffuse leukoaraiosis. J Magn Reson Imaging : JMRI. 2010;32(1):184–90. doi:10.1002/jmri.22209.
Purkayastha S, Fadar O, Mehregan A, Salat DH, Moscufo N, Meier DS, et al. Impaired cerebrovascular hemodynamics are associated with cerebral white matter damage. J Cereb Blood Flow Metab. 2014;34(2):228–34. doi:10.1038/jcbfm.2013.180.
Fazekas F, Kleinert R, Offenbacher H, Schmidt R, Kleinert G, Payer F, et al. Pathological correlates of incidental MRI white-matter signal hyperintensities. Neurology. 1993;43(9):1683–9.
Brown WR, Moody DM, Challa VR, Thore CR, Anstrom JA. Venous collagenosis and arteriolar tortuosity in leukoaraiosis. J Neurol Sci. 2002;203–204:159–63.
Zupan M, Sabovic M, Zaletel M, Popovic KS, Zvan B. The presence of cerebral and/or systemic endothelial dysfunction in patients with leukoaraiosis—a case control pilot study. BMC Neurol. 2015;15:158. doi:10.1186/s12883-015-0416-z.
Zhang J, Puri AS, Khan MA, Goddeau Jr RP, Henninger N. Leukoaraiosis predicts a poor 90-day outcome after endovascular stroke therapy. AJNR Am J Neuroradiol. 2014;35(11):2070–5. doi:10.3174/ajnr.A4029.
Arba F, Palumbo V, Boulanger JM, Pracucci G, Inzitari D, Buchan AM, et al. Leukoaraiosis and lacunes are associated with poor clinical outcomes in ischemic stroke patients treated with intravenous thrombolysis. Int J Stroke. 2016;11(1):62–7. doi:10.1177/1747493015607517.
Zhang S, Tang H, Yu YN, Yan SQ, Parsons MW, Lou M. Optimal magnetic resonance perfusion thresholds identifying ischemic penumbra and infarct core: a Chinese population-based study. CNS Neurosci Ther. 2015;21(3):289–95. doi:10.1111/cns.12367.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities AT 1.5-T in Alzheimer dementia and normal aging. Am J Roentgenol. 1987;149(2):351–6.
Cho TH, Nighoghossian N, Mikkelsen IK, Derex L, Hermier M, Pedraza S, et al. Reperfusion within 6 hours outperforms recanalization in predicting penumbra salvage, lesion growth, final infarct, and clinical outcome. Stroke; J Cereb Circ. 2015;46(6):1582–9. doi:10.1161/STROKEAHA.114.007964.
Dalkara T, Arsava EM. Can restoring incomplete microcirculatory reperfusion improve stroke outcome after thrombolysis? J Cereb Blood Flow Metab : Off J Int Soc Cereb Blood Flow Metab. 2012;32(12):2091–9. doi:10.1038/jcbfm.2012.139.
Heistad DD, Mayhan WG, Coyle P, Baumbach GL. Impaired dilatation of cerebral arterioles in chronic hypertension. Blood Vessels. 1990;27(2–5):258–62.
del Zoppo GJ, Mabuchi T. Cerebral microvessel responses to focal ischemia. J Cereb Blood Flow Metab : Off J Int Soc Cereb Blood Flow Metab. 2003;23(8):879–94. doi:10.1097/01.WCB.0000078322.96027.78.
Moody DM, Thore CR, Anstrom JA, Challa VR, Langefeld CD, Brown WR. Quantification of afferent vessels shows reduced brain vascular density in subjects with leukoaraiosis. Radiology. 2004;233(3):883–90. doi:10.1148/radiol.2333020981.
Warach S, Latour LL. Evidence of reperfusion injury, exacerbated by thrombolytic therapy, in human focal brain ischemia using a novel imaging marker of early blood–brain barrier disruption. Stroke; J Cereb Circ. 2004;35(11):2659–61. doi:10.1161/01.str.0000144051.32131.09.
Topakian R, Barrick TR, Howe FA, Markus HS. Blood–brain barrier permeability is increased in normal-appearing white matter in patients with lacunar stroke and leucoaraiosis. J Neurol Neurosurg Psychiatry. 2010;81(2):192–7. doi:10.1136/jnnp.2009.172072.
Chen B, Friedman B, Cheng Q, Tsai P, Schim E, Kleinfeld D, et al. Severe blood–brain barrier disruption and surrounding tissue injury. Stroke; J Cereb Circ. 2009;40(12):e666–74. doi:10.1161/STROKEAHA.109.551341.
Tuladhar AM, Reid AT, Shumskaya E, de Laat KF, van Norden AG, van Dijk EJ, et al. Relationship between white matter hyperintensities, cortical thickness, and cognition. Stroke; J Cereb Circ. 2015. doi:10.1161/STROKEAHA.114.007146.
Kim JT, Park MS, Yoon GJ, Jung HJ, Choi KH, Nam TS, et al. White matter hyperintensity as a factor associated with delayed mood disorders in patients with acute ischemic stroke. Eur Neurol. 2011;66(6):343–9. doi:10.1159/000332585.
Yamawaki M, Wada-Isoe K, Yamamoto M, Nakashita S, Uemura Y, Takahashi Y et al. Association of cerebral white matter lesions with cognitive function and mood in Japanese elderly people: a population-based study. Brain and Behavior. 2015;5(3). doi:10.1002/brb3.315.
Senda J, Ito K, Kotake T, Kanamori M, Kishimoto H, Kadono I, et al. Association of leukoaraiosis with convalescent rehabilitation outcome in patients with ischemic stroke. Stroke; J Cereb Circ. 2015. doi:10.1161/STROKEAHA.115.010682.
Zhang C, Wang Y, Zhao X, Wang C, Liu L, Pu Y, et al. Factors associated with severity of leukoaraiosis in first-ever lacunar stroke and atherosclerotic ischemic stroke patients. J Stroke Cerebrovasc Dis : Off J Nat Stroke Assoc. 2014;23(10):2862–8. doi:10.1016/j.jstrokecerebrovasdis.2014.07.021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethics Requirements
The study procedures were in accordance with the Helsinki Declaration of 1975. Informed consent was obtained from all individual participants included in the study. The protocol of this study had been approved by the human ethics committee of a local hospital.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Zhong, G., Yan, S., Zhang, S. et al. Association between Leukoaraiosis and Poor Outcome is not due to Reperfusion Inefficiency after Intravenous Thrombolysis. Transl. Stroke Res. 7, 439–445 (2016). https://doi.org/10.1007/s12975-016-0473-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-016-0473-7