Abstract
Post-thrombotic syndrome (PTS) occurs in 20–50% of patients with proximal deep vein thrombosis (DVT). In this study, we aimed to identify potential markers of thrombolysis success at the early stage and to clarify the relationship between early thrombolysis success and subsequent PTS development in patients with acute DVT in the iliac vein. Fifty-two consecutive patients with acute iliofemoral DVT who were treated with catheter-directed thrombolysis (CDT) within 21 days of onset were enrolled. An infusion catheter with multiple side holes was placed to cover the thrombosed vessel entirely. Urokinase solution was administered either continuously or with the pulse-spray method at a dose of 480,000–720,000 IU/day over the course of 2–7 days. During CDT, unfractionated heparin (UFH) was infused simultaneously via the access sheath to prevent thrombus formation. Early success was defined as lysis grade ≥ 50% and restoration of forward flow. PTS was diagnosed based on the Villalta scale. Based on the lysis grading method, complete lysis (grade III) was achieved in 8 of 52 (16%) limbs. Lysis grade II (50–99%) was achieved in 35 of 52 (67%) limbs. Lysis grade I (< 50%) was achieved in 9 of 52 (17%) limbs. Therefore, grade II and grade III lytic outcomes (early success) were observed in 43 patients (83%). One-year clinical follow-up was performed for 43 patients (83%). PTS occurred in seven (16%) patients. Early success was more frequently observed in patients without PTS than in those with PTS (92% vs. 43%; P < 0.01). Early success was only significantly associated with PTS in the multivariate analysis. Patients with acute symptomatic iliofemoral DVT who had early success from CDT treatment during the acute phase less frequently progressed to PTS. Patients with early success tended to undergo the pulse-spray method and had a shorter interval from symptom onset to CDT. The use of pulse-spray method and early initiation of CDT since DVT onset were potential markers of thrombolysis success.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute deep vein thrombosis (DVT) of the lower limb often results in swelling, pain, heaviness, pigmentation, and skin ulceration. These complications comprise post-thrombotic syndrome (PTS), which develops in 20–50% of patients with proximal DVT, and approximately 5–10% of those with severe PTS have a venous ulcer [1].
PTS results from a combination of residual venous obstruction and venous valve dysfunction. Ambulatory venous hypertension develops from the outflow obstruction as a result of the thrombus or valvular dysfunction. After DVT, recanalization of the thrombosed veins, which occurs through a combination of fibrinolysis, thrombus organization, neovascularization, and collateral formation, is often incomplete, thus resulting in residual venous obstruction. In this case, venous pressure reduction (while standing) is insufficient, resulting in venous hypertension [2, 3].
Current guidelines recommend anticoagulant therapy and the use of elastic compression stockings to prevent PTS [4]. Appropriate anticoagulation reduces thrombus formation and prevents embolization, recurrent venous thromboembolism (VTE), PTS, and mortality. Nevertheless, several additional and more aggressive treatments for DVT, such as catheter-directed thrombolysis (CDT), have been introduced to accelerate thrombus removal. Various studies suggested that CDT could be a highly effective clot lysis method [5,6,7,8,9,10], and some clinical benefits have been documented in randomized clinical trials. The CaVenT Study, which is the first randomized-controlled trial with long-term follow-up (5 years), has reported that additional CDT prevents PTS development [11]. In contrast, the recent ATTRACT trial, which enrolled more patients with acute proximal DVT, reported that the addition of pharmacomechanical CDT, when compared with conventional anticoagulation therapy, did not reduce PTS [12]. However, the trial had some issues. The iliac vein thrombus was documented in only half of the patients. Iliac vein obstruction is more likely to block venous return from the femoral and great saphenous veins. CDT would be preferable for DVT in the iliac vein. In fact, additional thrombus removal therapy reduced PTS in patients with iliofemoral DVT in the ATTRACT trial. Moreover, a direct examination of the relationship between acute thrombolysis success and subsequent PTS prevalence was not performed.
During this retrospective study involving two centers in Japan (Kakogawa Central City Hospital and Ohta Memorial Hospital), we aimed to identify potential markers of thrombolysis success at the early stage and to clarify the relationship between early thrombolysis success and subsequent PTS development in patients with acute DVT in the iliac vein.
Methods
Patients
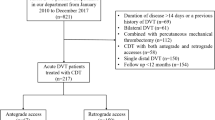
Fifty-two consecutive symptomatic patients with acute iliofemoral DVT (from October 2011 to April 2018) who were treated with CDT within 21 days from its onset at the Kakogawa Central City Hospital and Ohta Memorial Hospital were enrolled in this retrospective study. Duplex ultrasonography and computed tomography scans were used to diagnose DVT and to confirm the extent of the thrombus. The exclusion criteria for CDT included the following: age younger than 15 years; contraindication to anticoagulants and/or thrombolysis; severe anemia (hemoglobin < 8 g/dL); chronic kidney disease (eGFR < 30 mL/min); thrombocytopenia (platelet count < 150,000/cm [3]); pregnancy; uncontrolled hypertension; and previous ipsilateral DVT.
After examining the thrombus distribution, patients with CDT were eligible to participate in this study. At 6 months and at 1 year after the procedure, each patient visited the hospital and was interviewed by a physician to determine VTE recurrence or any complications. The Villalta score was also calculated. This study was approved by the institutional review board, and all patients provided written informed consent.
CDT and stenting techniques
Prior to CDT, each patient routinely received intravenous unfractionated heparin (UFH) daily after admission. UFH 5000 U was immediately infused intravenously after diagnosis. UFH was continuously administered to maintain an activated partial thromboplastin time (APTT) between 1.5- and 2.0-times the control level.
At the beginning of the procedure, a retrievable inferior vena cava filter was inserted at the right jugular vein to prevent iatrogenic pulmonary embolism (PE). Subsequently, a 4- to 7-Fr introducer sheath was inserted in the ipsilateral popliteal vein under ultrasound guidance with the patient in the prone position. Venography was performed to examine the extent of the thrombus (Fig. 1a–c).
Angiographic images of pre- and post-CDT. a–c Pre venography, d–f post venography. a–c Left iliac vein was completely occluded. d Thrombus score 0; the vein was patent and completely free of thrombus. e Thrombus score 1 stenotic lesion, and there was antegrade flow. f Thrombus score 2 completely occluded
The guidewire passed through the thrombosed lesion with the aid of a supporting 4-Fr straight catheter, which was followed by an infusion catheter with multiple side holes (Fountain® Infusion Systems; Merit Medical Systems, Inc., South Jordan, UT, USA). The catheter was placed to cover the thrombosed vessel entirely and then secured. Urokinase solution was administered either continuously or with the pulse-spray method at a dose of 480,000–720,000 IU/day for 2–7 days. With the pulse-spray method, urokinase 240,000 IU was administrated three times per day. The APTT, serum d-dimer, fibrinogen, hemoglobin level, and platelet count were checked daily.
CDT and UFH infusion via the access sheath were performed simultaneously to prevent thrombus formation. The APTT was maintained between 1.5- and 2.0-times the control level. Repeat venography was performed from the sheath every 2 or 3 days to assess the degree of thrombolysis. During CDT, blood pressure, pulsation, and the puncture site were assessed three times daily.
Additional procedures, such as catheter aspiration, balloon angioplasty, and stent implantation, were performed as needed [percutaneous angioplasty (PTA) was performed for cases with significant stenotic lesion in the iliac or common femoral veins]. When flow-limiting residual stenosis on venography or a stenosis area > 70% in the iliac vein on intravascular ultrasound (IVUS) was observed after thrombolysis and additional balloon dilatation, a self-expanding nitinol stent implantation was considered. The stent length was chosen based on the length of the stenotic lesion on venography, and the stent diameter was selected based on the measurements of the distal healthy venous diameter on IVUS. Additional balloon dilatation was performed after stent implantation (stent expansion was measured using IVUS imaging). CDT was continued until at least 90% thrombus removal with flow restoration was achieved, and the maximum treatment duration was 7 days. When a serious complication occurred, the procedure was discontinued.
Oral anticoagulation therapy was started after CDT, and it was continued at least 6 months. Warfarin was overlapped with continuous UFH, and UFH administration continued until the international normalized ratio reached 2–3. A direct oral anticoagulant was started 2 h after discontinuation of UFH: edoxaban 60 mg was administered once daily with or without food or 30 mg once daily to patients with a creatinine clearance of 30–50 mL/min or a bodyweight of ≤ 60 kg or to patients who were receiving concomitant treatment with potent P-glycoprotein inhibitors; rivaroxaban 15 mg was administered twice daily for the first 3 weeks, followed by 15 mg once daily; and apixaban 10 mg twice daily was administered for the first 7 days, followed by 5 mg twice daily.
Assessment of thrombus lysis
An angiographic evaluation was performed every 2 or 3 days after the initial CDT. The early efficacy of CDT was determined by the lysis grade, which was based on the post-lysis thrombus size. Thrombus lysis was examined in six venous segments: inferior vena cava, common iliac vein, external iliac vein, common femoral vein, superficial femoral vein, and popliteal vein. The thrombus score was 0 when the vein was patent and residual stenosis in < 50% of the vessel diameter (Fig. 1d); 1 when the vein was ≥ 50% stenotic lesion and there was antegrade flow (Fig. 1e); and 2 when it was completely occluded (Fig. 1f). The total thrombus score before and after CDT was calculated by adding the scores of each segment.
Moreover, the extent of thrombolysis was calculated after the completion of treatment, which included lysis and any additional adjunctive procedures such as balloon angioplasty and implantation of self-expanding nitinol stents to treat residual iliac vein stenosis lesions after thrombolysis, as the difference between the pre-lysis and post-lysis thrombus scores divided by the pre-lysis score. It was subsequently classified as follows: grade I, < 50% lysis; grade II, 50–99% lysis; and grade III, 100%, or complete lysis. Early success was defined as ≥ 50% lysis (lysis grade II or III) and forward flow restoration.
Safety outcomes
The safety outcomes included complications related to thrombolysis during or soon after the CDT procedure. Bleeding that resulted in a hemoglobin decrease of at least 2 g/dL required a transfusion of at least 2 U of packed red blood cells, occurred in the retroperitoneal, intracranial, or a critical organ, or contributed to death was categorized as a major complication. Clinically relevant non-major bleeding included epistaxis, a large visible hematoma, and spontaneous macroscopic hematuria. All other hemorrhages were categorized as trivial [13].
Venous patency and PTS
After 6 months and 12 months of follow-up, the venous system, including the iliac, femoral, and popliteal veins, was examined with duplex ultrasonography. Regained iliofemoral patency was described as flow in the pelvic and femoral veins, compressibility of the femoral vein, and no functional venous obstruction at any level [14]. Venous valve insufficiency was defined as reverse flow > 1 s in the popliteal vein when standing.
PTS was diagnosed after 12 months based on the Villalta scale; five patient-rated venous symptoms and six clinician-rated physical signs were assessed [15, 16]. A Villalta score ≥ 5 represents PTS, and a score ≥ 15 or the presence of a venous ulcer represents severe PTS. Recurrent DVT or PE was confirmed using objective imaging methods performed during the follow-up visits at our hospitals.
Statistical analysis
Continuous data are presented as means and standard deviations with interquartile ranges as appropriate. An analysis of the correlation between two findings and procedure-related variables was performed using the t test and Pearson Chi-square test. Predictors of primary success and the risk of PTS were evaluated by univariate and multivariate analyses using logistic regression models. P < 0.05 was considered statistically significant. All statistical analyses were performed using the SPSS statistical package (version 18.0; SPSS, Chicago, IL, USA).
Results
A total of 52 patients with proximal DVT in the iliac vein underwent CDT between 2011 and 2018. The baseline characteristics of the patients are shown in Table 1. The median duration of symptoms before thrombolysis was 7.7 days (1–18 days). At least one risk factor for venous thrombosis was reported for 24 patients (46%). Inherited thrombophilia was observed in two patients (4%), and a malignant tumor was observed in eight patients (15%). The continuous infusion method was performed for 29 patients and the pulse-spray infusion method was performed for 23 patients. Non-massive PE before CDT was diagnosed in 10 (19%) patients.
PTA and stenting
Adjunctive balloon angioplasty was performed for 40 patients (77%) (Table 1). Self-expanding nitinol stents were implanted in the iliac vein in 21 patients (40%). Stent diameter and length were 11.0 ± 1.3 mm (10–14 mm) and 60.8 ± 23.2 mm (40–80 mm), respectively. EPIC 11, SMART 5, E-LUMINEXX 2, and Absolute 1 stents were used. All patients with a stent underwent IVUS imaging.
Lysis effect and venous patency
Thrombus lysis was examined in six venous segments: inferior vena cava, common iliac vein, external iliac vein, common femoral vein, superficial femoral vein, and popliteal vein. Based on the lysis grading method described previously, complete lysis (grade III) was achieved in 8 of 52 (15%) limbs, 50–99% lysis (grade II) was achieved in 35 of 52 (67%) limbs, and < 50% lysis (grade I) was achieved in 9 of 52 (17%) limbs (Table 2). Therefore, early success (i.e., grade II and grade III) was observed in 43 patients (83%). The mean CDT duration was 5.1 ± 1.8 days, and the total urokinase dose was 267 ± 106 × 104 IU.
Table 3 shows no statistically significant difference in patient characteristics and procedure details of patients with (lysis grades II and III) and without (grade I) effective lysis. However, those who had early success had a shorter interval from symptom onset to CDT and more frequently underwent the pulse-spray method than those who had CDT failure. No significant predictor of early success was observed in the univariate and multivariate analyses.
Safety outcomes
No symptomatic PE was noted during treatment. Bleeding complications occurred in 8 (15%) patients (4 had puncture site hematoma and 1 had gastrointestinal bleeding). Three patients (6%) received a blood transfusion. CDT was discontinued in 1 patient.
Vessel patency and Villalta score at follow-up
The mean clinical follow-up period was 757 ± 540 days (8–2235 days). One-year clinical follow-up was performed for 43 patients (83%); PTS occurred in seven patients. All PTS cases were mild (Villalta score, 5–10). During the observation period, no patient died or had recurrent DVT. At the 12-month follow-up, venous patency was examined using ultrasonography for 34 patients, of whom 23 (68%) had patency of iliac vein, 10 had autologous vein occlusion, and one had stent occlusion.
Patients without PTS had higher early success rates than those with PTS (Table 4). Age, body mass index, laterality of DVT, and oral anticoagulation were not significantly different between patients with and those without PTS. The patency of the iliac vein tended to be higher in the no PTS group, but there was no significant difference between groups (75% vs. 33%; P = 0.13). Regurgitation of the popliteal vein was equal in the two groups. Early success was only significantly associated with PTS in the multivariate analyses.
Discussion
In this study, CDT using urokinase was successful (lysis grades II and III) for 83% of patients with acute DVT in the iliac vein, which was similar to the findings of other studies (83–92%). Patients without PTS more often had early success (lysis grades II and III) than those with PTS.
Previous studies with long-term follow-up reported that venous patency is correlated with reduced PTS frequency [8, 14, 17], although no correlation between the lysis grade and patency or PTS was found [18]. Our results provide further support of the importance of patency for improved clinical results, as previously suggested. However, in the recent ATTRACT trial, pharmacomechanical thrombolysis did not prevent PTS in patients with acute proximal DVT [12], which attracted numerous debates; one possible reason could be that 42% of patients enrolled in the ATTRACT trial had thrombus formation only in the femoropopliteal vein. Venous return from the femoral and great saphenous veins is significantly impaired because of iliac vein obstruction. In fact, additional thrombus removal therapy reduced PTS incidence among patients with isolated iliac or iliofemoral DVT in the sub-analysis of the ATTRACT trial; however, CDT did not reduce PTS incidence in femoropopliteal DVT cases. In our study, only isolated iliac DVT or iliofemoral DVT was included. Therefore, CDT for iliac vein thrombosis could contribute to preventing PTS development, and we believe that patients with pelvic vein thrombosis are suitable candidates for CDT treatment to prevent PTS. Moreover, we assume that acute isolated iliac vein and iliofemoral thromboses are appropriate candidates for CDT and that aggressive thrombolytic treatment is not more effective than anticoagulation for superficial femoral vein thrombosis.
This study included patients with acute DVT symptoms. CDT was started within 7 days from symptom onset for 26 (60%) patients with lysis grades II and III and for only two patients (22%) with lysis grade I. Nonetheless, no statistically significant difference in CDT outcomes for patients with lysis grades II and III and those with lysis grade I was found (P = 0.08). The time interval from DVT onset to CDT initiation is theoretically a crucial contributor to successful thrombolysis, because time-dependent structural changes and organization of the clot may prevent thrombolysis. Recent guidelines recommended that CDT initiation should be performed within 14 days [19]. In a study by Mewissen et al., complete lysis was achieved in 34% of the patients with symptoms for ≤ 10 days and in 19% of those with symptoms for > 10 days; a statistically significant difference in the complete lysis rate was found [6]. In our study, no correlations between symptom duration and PTS development were observed. Nevertheless, the interval from symptom onset to CDT was shorter for those with early success than for those with CDT failure.
Furthermore, the pulse-spray method was used for 21 patients (49%) with early success and only one patient (11%) with CDT failure. The pulse-spray method tended to result in early success; however, no statistically significant difference between continuous infusion and pulse-spray methods was observed (P = 0.07). Most recent studies used the continuous infusion method, and no comparative studies have examined the differences in outcomes of the two infusion methods for patients with iliofemoral DVT. However, a retrospective study showed that the pulse-spray method has better outcomes and is superior to continuous infusion for the treatment of iliofemoral DVT [20]. Hence, the pulse-spray method possibly has better effects on PTS reduction.
In our study, the initial success cases had lower PTS occurrence than the no success cases at 1 year after CDT. Moreover, no predictor of initial success was found; however, patients with early success tended to undergo the pulse-spray method and had a shorter interval from symptom onset to CDT compared with those with CDT failure. In addition, patients without PTS had higher early success rates than those with PTS. Therefore, early intervention within 7 days and the use of a pulse-spray method could improve early success rates, thus leading to the reduction of PTS.
Recently, tissue plasminogen activator has been used for CDT. However, tissue plasminogen activator is currently approved only for PE with shock in Japan. Moreover, urokinase could only be used for CDT in DVT cases. In this study, the urokinase dose administered was much lower than that used in previous western studies [6]. Because Asians are at higher risk for bleeding risk than Whites, the urokinase dose used in our practice is reasonable for achieving early success and preventing major bleeding events.
Study limitations
This study had several limitations. First, it was a non-randomized observational study, including highly selected patients. Therefore, we could not compare the additional CDT therapy with conventional anticoagulation therapy alone, and inferences regarding the optimal treatment for iliac vein thrombosis could not be determined in this study. Second, a small number of patients were enrolled in this study, quite a few cases were lost to follow-up because of various reasons, and the number of patients with longer follow-up was small. The small number of patients in this study possibly contributed to the absence of statistical differences. Hence, further studies should include numerous patients.
Conclusion
In this retrospective study, early success for acute DVT in the iliac vein had less frequent PTS after 1 year from the onset of DVT. Patients with early success tended to undergo the pulse-spray method and had a shorter interval from symptom onset to CDT.
The use of pulse-spray method and early initiation of CDT since DVT onset were potential markers of thrombolysis success.
References
Kahn SR. The post-thrombotic syndrome. Hematol Am Soc Hematol Educ Progr. 2010;2010:216–20.
Kahn SR, Comerota AJ, Cushman M, Evans NS, Ginsberg JS, Goldenberg NA, et al. The postthrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2014;130:1636–61.
Kahn SR. The post-thrombotic syndrome: progress and pitfalls. Br J Haematol. 2006;134:357–65.
Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e419S–94S.
Bjarnason H, Kruse JR, Asinger DA, Nazarian GK, Dietz CA Jr, Caldwell MD, et al. Iliofemoral deep venous thrombosis: safety and efficacy outcome during 5 years of catheter-directed thrombolytic therapy. J Vasc Interv Radiol. 1997;8:405–18.
Mewissen MW, Seabrook GR, Meissner MH, Cynamon J, Labropoulos N, Haughton SH. Catheter-directed thrombolysis for lower extremity deep venous thrombosis: report of a national multicenter registry. Radiology. 1999;211:39–49.
AbuRahma AF, Perkins SE, Wulu JT, Ng HK. Iliofemoral deep vein thrombosis: conventional therapy versus lysis and percutaneous transluminal angioplasty and stenting. Ann Surg. 2001;233:752–60.
Elsharawy M, Elzayat E. Early results of thrombolysis vs anticoagulation in iliofemoral venous thrombosis. A randomised clinical trial. Eur J Vasc Endovasc Surg. 2002;24:209–14.
Schulman S. Getting intimate with the venous thrombus. J Thromb Haemost. 2009;7:1266–7.
Enden T, Haig Y, Kløw NE, et al. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. Lancet. 2012;379:31–8.
Haig Y, Enden T, Grøtta O, Slagsvold CE, Sandvik L, Ghanima W, et al. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial. Lancet Haematol. 2016;3:e64–71.
Vedantham S, Goldhaber SZ, Julian JA, Kahn SR, Jaff MR, Cohen DJ, et al. Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis. N Engl J Med. 2017;377:2240–52.
Büller HR, Davidson BL, Decousus H, Gallus A, Gent M, Piovella F, et al. Subcutaneous fondaparinux versus intravenous unfractionated heparin in the initial treatment of pulmonary embolism. N Engl J Med. 2003;349:1695–702.
Enden T, Kløw NE, Sandvik L, Slagsvold CE, Ghanima W, Hafsahl G, et al. Catheter-directed thrombolysis vs anticoagulant therapy alone in deep vein thrombosis: results of an open randomized, controlled trial reporting on short-term patency. J Thromb Haemost. 2009;7:1268–75.
Kahn SR, Partsch H, Vedantham S, Prandoni P, Kearon C. Definition of post thrombotic syndrome of the leg for use in clinical investigations: a recommendation for standardization. J Thromb Haemost. 2009;7:879–83.
Villalta S, Bagatella P, Piccioli A, Lensing A, Prins M, Prandoni P, et al. Assessment of validity and reproducibility of a clinical scale for the post thrombotic syndrome. Haemostasis. 1994;24:158.
Broholm R, Sillesen H, Damsgaard MT, Jørgensen M, Just S, Jensen LP, et al. Postthrombotic syndrome and quality of life in patients with iliofemoral venous thrombosis treated with catheter-directed thrombolysis. J Vasc Surg. 2011;54:18S–25S.
Haig Y, Enden T, Slagsvold CE, Sandvik L, Sandset PM, Kløw NE. Determinants of early and long-term efficacy of catheter-directed thrombolysis in proximal deep vein thrombosis. J Vasc Interv Radiol. 2013;24:17–24.
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149:315–52.
Foegh P, Jensen LP, Klitfod L, Broholm R, Bækgaard N. Editor’s choice—factors associated with long-term outcome in 191 patients with ilio-femoral DVT treated with catheter-directed thrombolysis. Eur J Vasc Endovasc Surg. 2017;53:419–24.
Acknowledgements
We want to thank Editage (http://www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Human rights statements and ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institution and national) and with the Helsinki Declaration of 1964 and later revisions. Informed consent was obtained from all patients who were included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakamura, H., Anzai, H. & Kadotani, M. Less frequent post-thrombotic syndrome after successful catheter-directed thrombolysis for acute iliofemoral deep vein thrombosis. Cardiovasc Interv and Ther 36, 237–245 (2021). https://doi.org/10.1007/s12928-020-00661-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-020-00661-7