Abstract
Patients with acute coronary syndrome (ACS) are thought to have multiple vulnerable coronary plaques. We analyzed non-culprit plaques in patients with ACS vs. stable angina pectoris (SAP) by means of color-coded intravascular ultrasound (iMap-IVUS). Patients who underwent percutaneous coronary intervention were divided into an ACS group (n = 39) and an SAP group (n = 35). Non-culprit lesions were imaged by 40-MHz iMap-IVUS, and the plaque characteristics were compared between the two groups. Plaque volume was similar between the two groups. The fibrotic volume (%FV) was less in the ACS group than in the SAP group (70.2 ± 10.4 vs. 76.5 ± 7.2 %, respectively, P < 0.01), whereas the lipidic volume and necrotic volume (%NV) were greater in the ACS group (8.2 ± 0.4 vs. 6.3 ± 0.4 %, P < 0.01; 15.1 ± 7.9 vs. 9.9 ± 4.8 %, P < 0.01). An inverse correlation was found between %FV and total plaque volume (ACS group: r = −0.52, P < 0.01; SAP group: r = −0.31, P = 0.01), and a positive correlation was found between %NV and total plaque volume (ACS group: r = 0.56, P < 0.01; SAP group: r = 0.41, P < 0.01). Furthermore, the slope of the regression line showing the relation between plaque volume and necrotic volume was significantly steeper for the ACS group than for the SAP group (P < 0.05). Non-culprit lesions are particularly vulnerable in ACS patients. Non-culprit lesions are particularly vulnerable in ACS patients. Furthermore, the stronger correlation between plaque volume and %NV was observed in ACS patients than in SAP patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute coronary syndrome (ACS) is commonly caused by rupture of vulnerable plaque and subsequent thrombotic occlusion. It has been suggested that patients with ACS are likely to have multiple vulnerable plaques because plaque rupture is frequently observed not only at the culprit lesion but also at non-culprit lesions or vessels [1–3]. Understanding the tissue characteristics of non-culprit plaques in patients with ACS may be important for preventing subsequent cardiovascular events.
Vulnerable plaque has been defined by multiple pathological factors, such as a thin cap with a large lipid core, acute inflammation, endothelial denudation with superficial platelet aggregation, plaque fissuring, superficial calcification, a glistening yellow appearance, intraplaque hemorrhage, vessel stenosis of more than 90 %, endothelial dysfunction, and high risk for rupture. Tissue characteristics of plaque can now be identified in vivo by means of various intracoronary imaging modalities such as color-coded intravascular ultrasound (color IVUS), optical coherence tomography (OCT), and coronary angioscopy [4]. Color IVUS, in particular, can characterize the tissue components of coronary plaque. There are currently three types of color IVUS tissue characterization systems: virtual histology (VH)-IVUS, integrated backscatter (IB)-IVUS, and iMAP-IVUS. Previous studies performed by means of these various systems have revealed significantly high lipid content and a large necrotic area in the culprit lesions associated with ACS [5–8]. However, the features of non-culprit lesions in ACS patients have not been confirmed with the use of the most novel color IVUS system, iMAP, which characterizes tissue by an advanced neuro-learning pattern recognition system for assessing spectral similarity of radiofrequency IVUS signals. An ex vivo validation study showed accuracies at the highest levels of confidence of 97, 98, 95, and 98 % for necrotic, lipidic, fibrotic, and calcified regions, respectively [9]. Therefore, we used iMAP to identify and compare the tissue characteristics of non-culprit lesions in patients with ACS and in patients with stable angina pectoris (SAP).
Materials and methods
Study patients
This study was a single-center observational study that included 74 patients who underwent percutaneous coronary intervention (PCI) for ACS or SAP between April 2011 and September 2011 at Nihon University Itabashi Hospital. They were divided into two groups: an ACS group (n = 39) and an SAP group (n = 35). ACS included acute myocardial infarction (33 patients, 84.6 %) and unstable angina pectoris (6 patients, 15.4 %). Acute myocardial infarction was diagnosed on the basis of biomarker elevation [e.g., creatine kinase (CK), CK-MB isoform, or troponin T elevation], an ST-T-specific change in the electrocardiogram, and a history of precordial chest pain. Unstable angina pectoris was defined as angina with worsening or at-rest chest pain with a specific electrocardiogram change [10, 11]. All patients included had an angiographically determined coronary diameter stenosis of at least 75 % (relative to the diameter of adjacent normal coronary artery). The lesions studied were selected retrospectively by statistical matching of IVUS-derived plaque volumes between the two groups. Patients with advanced kidney disease or undergoing hemodialysis, those with familial hyperlipidemia, severe liver disease, or hyperthyroidism, and those who had undergone coronary bypass surgery or had significant left main coronary disease were excluded from the study. We analyzed 85 non-culprit lesions in culprit vessels (40 lesions in ACS patients and 45 lesions in SAP patients). The study was conducted according to the Declaration of Helsinki and with the approval of the institutional review boards. Written informed consent for entry of this study was obtained from all patients included.
IVUS procedure
All patients received unfractionated heparin (5000 U) intraarterially before the percutaneous coronary intervention (PCI). We gained access via the radial or femoral artery. For ethical reasons, the culprit lesion was first treated by implantation of a bare metal stent or drug-eluting stent, and IVUS was performed only for the culprit vessel. After PCI, we analyzed non-culprit lesions of at least 5 mm in length in the culprit vessel and that were detected at least 5 mm from the site of the culprit lesion. We examined lesions in which the maximum cross-sectional plaque area represented more than 25 % of total vessel area. The length of 5 mm was chosen so that the lumen at its narrowest point would be centered over the lesion. Plaques having a calcification with an angular span of more than 90° were excluded. All plaque segments that met the above-mentioned criteria were selected. After intracoronary administration of nitroglycerin, the lesions were imaged and tissue-characterized by 40 MHz IVUS (Atlantis™ SR Pro 40 MHz Catheter) with the use of an iLAB™ console and iMAP™ system (Boston Scientific Co. Ltd, Fremont, CA, USA) during continuous pullback at 0.5 mm/s.
The area or percentage of each tissue component was measured and calculated with the use of QIvus 2.0 quantitative analysis software (Medis Medical Imaging Systems bv, Leiden, The Netherlands). The external elastic membrane (EEM) area and lumen area were first measured. The plaque area was calculated as the EEM area minus the lumen area. Plaque burden was calculated as the plaque area divided by the EEM area. The volume of each component was then calculated from cross-sections of 0.5 mm each covering the entire 5-mm lesion.
In iMAP analysis, components of the plaques were classified as fibrotic (depicted in green), lipidic (yellow), necrotic (pink), and calcified (blue). The percentage of each tissue component [(%FV) % fibrotic volume; (%LV) % lipidic volume; (%NV) % necrotic volume; and (%CV) % calcified volume] was calculated as the volume of each divided by the total plaque volume. The IVUS and iMAP evaluations were done by two physicians experienced in IVUS and iMAP analyses (T.N. and M.S.). The areas behind calcifications with an angular span of less than 90° span or coronary guidewire were not measured for each tissue component, although the EEM area was measured by trace extrapolation around the drop-out area.
Statistical analysis
Discrete variables are presented as numbers and percentages. Continuous variables are presented as mean ± SD. Between-group differences in mean values were analyzed by unpaired Student’s t test or Wilcoxon rank-sum test. Between-group differences in discrete variables were analyzed by Chi-square test or Fisher’s exact test. Correlation was determined by the Pearson correlation coefficient. Differences in slopes of the regression line pertaining to each plaque component between the ACS group and SAP group were assessed by analysis of covariance (ANCOVA). Multiple logistics regression analysis was performed to identify the determinants of ACS. P < 0.05 (two-sided) was accepted as statistically significant. All statistical analyses were performed with JMP 9 version 9.0.0 (SAS Institute Inc, Cary, NC, USA).
Results
Patient characteristics
Patients’ baseline clinical characteristics are shown per group in Table 1. Only the prevalence of prior myocardial infarction, the serum triglyceride level, and the spectrum of concomitant drugs differed between the groups. Prior myocardial infarction was significantly more prevalent in the SAP group than in the ACS group. The triglyceride level was significantly higher in the SAP group than in the ACS group, although the mean value was around 140 mg/dl and thus in good control. Use of ARB/ACE-I, statins, nitrate, aspirin, and thienopyridine was more common in the SAP group than in the ACS group. Although statins were used by more patients in the SAP group than in ACS group, the LDL cholesterol level was comparable between the two groups. The target coronary vessels in which non-culprit lesions were observed were also comparable. In addition, the proportion of imaged segments that were proximal or distal to the PCI site was comparable.
Gray-scale IVUS measurements
In the total 74 patients, 85 non-culprit lesions were analyzed by means of IVUS. Plaque volume at non-culprit lesions was matched between the two groups (ACS; 40 lesions, SAP; 45 lesions). Minimal lumen area (MLA) and EEM area at the MLA within the imaged non-culprit lesions of the ACS group vs. SAP group were as follows: MLA, 7.5 ± 0.5 vs. 7.1 ± 0.5 mm2, P = 0.53; EEM area, 15.7 ± 0.7 vs. 14.7 ± 0.7 mm2, P = 0.32). Plaque burden at the MLA was also similar (46.6 ± 1.8 vs. 47.5 ± 1.7 %, respectively, P = 0.73). Furthermore, gray-scale IVUS-derived volume data were also comparable (Table 2). Plaque volumes matched in the 5-mm non-culprit lesions. EEM volume (vessel volume), lumen volume, and % plaque volume were also similar.
Color IVUS measurements
Representative iMAP images from patients with SAP and ACS are shown in Fig. 1. As shown in these images, the non-culprit lesions in patients with ACS vs. the non-culprit lesions in patients with SAP contained more necrotic and lipidic tissues. The percentages of each tissue component within the total plaque volume measured by iMAP are shown in Fig. 2. The absolute volume of each tissue component is shown in Table 3. Although fibrotic volume was similar between the two groups, lipidic and necrotic volumes were greater in the ACS group than in the SAP group. %FV was significantly greater in the SAP group than in the ACS group (76.5 ± 7.2 vs. 70.2 ± 10.4 %, respectively, P < 0.01). However, %LV and %NV were significantly greater in the ACS group than in the SAP group (%LV: 8.2 ± 0.4 vs. 6.3 ± 0.4 %, respectively, P < 0.01; %NV: 15.1 ± 7.9 vs. 9.9 ± 4.8 %, P < 0.01), whereas %CV was similar between the two groups (1.4 ± 0.2 vs. 1.1 ± 0.1 %, respectively, P = 0.29).
Representative images from a patient with SAP and a patient with ACS. Left panels are coronary angiograms. The red lines correspond to the cross-sections of non-culprit lesion imaged by gray-scale IVUS (middle panels) and color IVUS (right panels). The upper row images are from an SAP patient, and a large fibrous tissue component (green) is seen in the iMAP image. The lower row images are from an ACS patient, and the necrotic and lipidic components within the plaque are much larger than those in the SAP patient
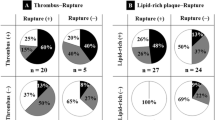
Correlation between each tissue component volume and plaque volume is shown in Fig. 3. Fibrotic, lipidic, and necrotic volumes correlated significantly with plaque volume. The slopes of the regression lines showing the relation between plaque volume and fibrotic volume were significantly steeper for the SAP group than for the ACS group (P < 0.05 by ANCOVA). To the contrary, the slope of the regression line showing the relation between plaque volume and necrotic volume was significantly steeper for the ACS group than for the SAP group (P < 0.05 by ANCOVA).
Correlation between plaque volume and the absolute volume of each tissue component. a Fibrotic volume, b lipidic volume and c necrotic volume were significantly correlated with plaque volume. The slopes of the regression line of relationships of fibrotic volume–plaque volume were significantly steeper in SAP group than in ACS group. On the other hand, the slopes of the regression line of relationships of necrotic volume–plaque volume were significant steeper in ACS group than in SAP group. Asterisk comparison of slopes between SAP vs. ACS, P < 0.05 by ANCOVA
Correlations between % volume of each tissue component and plaque volume are shown in Fig. 4. %FV correlated inversely and significantly with plaque volume. %LV and %NV correlated positively and significantly with plaque volume. The slopes of the regression lines showing the relations between plaque volume and %FV and plaque volume and %NV were significantly steeper for the ACS group than for the SAP group (P < 0.05 by ANCOVA).
Correlation between plaque volume and percent volume of each tissue component. a % Fibrotic volume provided a significant inverse correlation with plaque volume, b % lipidic volume and c % necrotic volume were significantly correlated with plaque volume. The slopes of the regression line of relationships of % fibrotic volume–plaque volume and % necrotic volume–plaque volume were significantly steeper in ACS group than in SAP group. Asterisk comparison of slopes between SAP vs. ACS, P < 0.05 by ANCOVA
Multivariate analysis
Results of multiple logistic regression analysis for the determinants of ACS are shown in Table 4. Ten variables with a P value <0.05 in univariate analysis were entered into multivariate analysis, and the triglyceride level, %NV, and the use of aspirin were shown to be significant determinants of ACS.
Discussion
The major finding of the present study was that non-culprit plaques were more lipidic and necrotic and less fibrotic in patients with ACS than in patients with SAP, although plaque volume and MLA were similar between the two groups. Moreover, %FV, %LV and %NV correlated positively or negatively with total plaque volume in both groups. Multivariate analysis showed %NV to be a significant determinant of ACS.
Patients with a history of ACS, in comparison to patients with stable coronary artery disease, have a higher secondary risk of future cardiovascular events. This tendency is recognized even in the Japanese, who have a lower risk of atherosclerotic cardiovascular events compared to that of their Western counterparts [12, 13]. It is reasonable to speculate that this is due in part to a difference in plaque characteristics in the non-culprit, non-target, or residual segment of the coronary artery branch between ACS and SAP.
Differences in tissue characteristics of non-culprit coronary atherosclerotic plaques between ACS and SAP patients have been thus far been demonstrated by means of other vascular imaging modalities. Ando et al. showed, by means of IB-IVUS, that non-culprit lesions were more lipidic in ACS patients than in patients with SAP [5]. Liu, et al. showed, by mean of VH-IVUS, that non-culprit lesions were more lipidic and less fibrotic in ACS patients than in SAP patients [8]. In addition, Thieme, et al. showed, by means of coronary angioscopy, that yellow plaques, considered to be lipid-rich, were more prevalent in ACS patients than in SAP patients [14]. Our study, which was based on the latest modality, iMAP, and performed under statistical matching of plaque volume as well as MLA between the ACS and SAP patients, reinforced these earlier findings.
Our study also provided insight into the relation between total plaque volume and the percentage volume of each tissue component. Although total plaque volume was similar between the two groups, %NV and %LV correlated positively with total plaque volume, whereas %FV correlated inversely with total plaque volume. In addition, the slopes of the regression lines showing the relations between plaque volume and %FV and plaque volume and %NV were significantly steeper for the ACS group than for the SAP group. The PROSPECT trial, which was based on VH-IVUS, showed that VH-IVUS-derived thin cap fibroatheromas (VH-TCFA), with a minimum lumen area of ≤4 mm2, and a large plaque burden (≥70 %), had a greater likelihood of causing a future event within 3 years [15]. Dohi, et al. reported a positive correlation between the extent of lipid-rich plaque measured by near-infrared spectroscopy and IVUS-derived plaque burden [16]. These findings suggest that the coronary plaque volume as well as necrotic or lipidic tissue burden together determine the likely course of the cardiovascular disease. The difference in the slopes of the regression lines representing the relations between plaque volume and the plaque tissue characteristics has an important implications: first, that the larger plaque volume, the greater the vulnerability, especially in ACS patients, and second, that simply assessing the plaque volume by other modalities including gray-scale IVUS remains useful for evaluating plaque vulnerability. To the contrary, the more modest slope and the lower values in the SAP group suggest that plaque is less vulnerable over the entire range of plaque volume in SAP patients.
A history of smoking seemed to be more common in our study patients than in previously reported study groups [17, 18]. We included both current and former smoking when we calculated the prevalence of smoking. Kato et al. reported a prevalence of almost 60 % smoking, including current and former smoking, in ACS and non-ACS patients [19]. Therefore, our study patients seem to represent patients commonly seen in clinical practice. In addition, the use of statins differed significantly between our two groups, and we had to consider whether this difference influenced our study results. However, our multivariate analysis showed that the use of statins was not a significant determinant of ACS. So we felt that, although the use of statins might differ from that of previously reported clinical trials, it is safe to assume that statin use did not affect the results of our study.
Determinants of ACS
We found %NV derived by iMAP, the triglyceride level, and the use of aspirin to be significantly associated with ACS. Ando et al., using IB-IVUS, showed that non-culprit coronary lesions in ACS patients were associated with lipid-rich plaque. Their findings seemed to differ from ours, which suggested the importance of the necrotic volume rather than the lipid volume. However, the definitions of necrotic tissues and lipidic tissues differed between the two studies, with some overlap in the characterization of necrotic vs. lipidic [9, 20]. Thus, the study conclusions were not as discrepant as they might have appeared initially.
The lower triglyceride level and the less frequent use of aspirin that we found to be associated with ACS could be related to a difference in ACS and SAP patients’ clinical status upon hospital admission. ACS patients usually undergo emergency PCI and have been in a fasting state for a longer time and have not been given medications prior to admission. SAP patients usually undergo elective PCI and have been given medications. This could be related to the lower triglyceride levels in our ACS patients than in our SAP patients. Another factor we should consider might be that the concomitant drugs for cardiovascular disease might be different between SAP and ACS patients at the time of catheterization. These factors should also be considered in both univariate and multivariate analyses. Especially, use of aspirin, which was shown by multivariate analysis to be a major determinant, is a clinically effective for preventing secondary thrombus-related cardiovascular events, so the administration of aspirin might be less likely in de novo ACS patients at the admission.
Clinical implications
Our findings have important clinical implications. First, visual evidence was provided to help us understand the importance of vigorous management of plaque vulnerability especially in ACS patients. Second, assessment of plaque volume alone, in the absence of tissue characterization, can pinpoint plaque vulnerability in ACS patients. Third, detection of a necrotic core by iMAP might be important in predicting a future ACS event.
Limitations
This study was performed in a small number of patients at a single center. Ultrasound-based iMAP analysis was inadequate for plaques with a very large superficial calcified core, so patients with such plaques were excluded from the study. Thus, patients with very severe atherosclerosis were not examined in this study. Moreover, only culprit vessels were analyzed because non-culprit vessels were excluded for ethical reasons.
Conclusion
The present study showed non-culprit lesions in ACS patients to be more vulnerable than non-culprit lesions in SAP patients. Furthermore, the vulnerability in ACS patients was significantly correlated with plaque volume, suggesting that total plaque volume is a direct representation of plaque vulnerability in ACS patients. In addition, the necrotic tissue content was mainly associated with the incidence of ACS. Overall, our findings indicate that vigorous medical management aimed at reducing plaque vulnerability is necessary for secondary prevention, especially in ACS patients.
References
Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O’Neill WW. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000;343:915–22.
Mann J, Davies MJ. Mechanisms of progression in native coronary artery disease: role of healed plaque disruption. Heart. 1999;82:265–8.
Hong MK, Mintz GS, Lee CW, Kim YH, Lee SW, Song JM, Han KH, et al. Comparison of coronary plaque rupture between stable angina and acute myocardial infarction: a three-vessel intravascular ultrasound study in 235 patients. Circulation. 2004;110:928–33.
Vancraeynest D, Pasquet A, Roelants V, Gerber BL, Vanoverschelde JL. Imaging the vulnerable plaque. J Am Coll Cardiol. 2011;57:1961–79.
Ando H, Amano T, Matsubara T, Uetani T, Nanki M, Marui N, Kato M, et al. Comparison of tissue characteristics between acute coronary syndrome and stable angina pectoris. An integrated backscatter intravascular ultrasound analysis of culprit and non-culprit lesions. Circ J. 2011;75:383–90.
Hopkins PN, Heiss G, Ellison RC, Province MA, Pankow JS, et al. Coronary artery disease risk in familial combined hyperlipidemia and familial hypertriglyceridemia: a case–control comparison from the national heart, lung, and blood institute family heart study. Circulation. 2003;108:519–23.
Kozuki A, Shinke T, Otake H, Shite J, Matsumoto D, Kawamori H, et al. Feasibility of a novel radiofrequency signal analysis for in vivo plaque characterization in humans: comparison of plaque components between patients with and without acute coronary syndrome. Int J Cardiol. 2013;167:1591–6.
Liu HL, Zhang J, Ma DX, Luo JP, Yang SL, Han W, et al. Coronary plaque characterization of non-culprit or nontarget lesions assessed by analysis of in vivo intracoronary ultrasound radio-frequency data. Chin Med J (Engl). 2009;122:622–6.
Sathyanarayana S, Carlier S, Li W, Thomas L. Characterisation of atherosclerotic plaque by spectral similarity of radiofrequency intravascular ultrasound signals. EuroIntervention. 2009;5:133–9.
Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-st-segment elevation myocardial infarction: executive summary and recommendations. A report of the A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee on the management of patients with unstable angina. Circulation. 2000;102:1193–209.
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of st-elevation myocardial infarction: executive summary: a report of the A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:485–510.
Sato H, Kinjo K, Ito H, Hirayama A, Nanto S, Fukunami M, et al. Effect of early use of low-dose pravastatin on major adverse cardiac events in patients with acute myocardial infarction: the oacis-lipid study. Circ J. 2008;72:17–22.
Kimura T, Morimoto T, Furukawa Y, Nakagawa Y, Shizuta S, Ehara N, et al. Long-term outcomes of coronary-artery bypass graft surgery versus percutaneous coronary intervention for multivessel coronary artery disease in the bare-metal stent era. Circulation. 2008;118:S199–209.
Thieme T, Wernecke KD, Meyer R, Brandenstein E, Habedank D, Hinz A, et al. Angioscopic evaluation of atherosclerotic plaques: validation by histomorphologic analysis and association with stable and unstable coronary syndromes. J Am Coll Cardiol. 1996;28:1–6.
Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–35.
Dohi T, Maehara A, Moreno PR, Baber U, Kovacic JC, Limaye AM, et al. The relationship among extent of lipid-rich plaque, lesion characteristics, and plaque progression/regression in patients with coronary artery disease: a serial near-infrared spectroscopy and intravascular ultrasound study. Eur Heart J Cardiovasc Imaging. 2015;16:81–7.
Nozue T, Yamamoto S, Tohyama S, Fukui K, Umezawa S, Onishi Y, et al. Comparison of the effects of pitavastatin versus pravastatin on coronary artery plaque phenotype assessed by tissue characterization using serial virtual histology intravascular ultrasound. Heart Vessels. 2013;30:36–44.
Hong MK, Park DW, Lee CW, Lee SW, Kim YH, Kang DH, et al. Effects of statin treatments on coronary plaques assessed by volumetric virtual histology intravascular ultrasound analysis. J Am Coll Cardiol Intv. 2009;2:679–88.
Kato K, Yonetsu T, Kim SJ, Xing L, Lee H, McNulty I, et al. Nonculprit plaques in patients with acute coronary syndromes have more vulnerable features compared with those with non-acute coronary syndromes: a 3-vessel optical coherence tomography study. Circ Cardiovasc Imaging. 2012;5:433–40.
Kawasaki M, Takatsu H, Noda T, Sano K, Ito Y, Hayakawa K, et al. In vivo quantitative tissue characterization of human coronary arterial plaques by use of integrated backscatter intravascular ultrasound and comparison with angioscopic findings. Circulation. 2002;105:2487–92.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sudo, M., Hiro, T., Takayama, T. et al. Tissue characteristics of non-culprit plaque in patients with acute coronary syndrome vs. stable angina: a color-coded intravascular ultrasound study. Cardiovasc Interv and Ther 31, 42–50 (2016). https://doi.org/10.1007/s12928-015-0345-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-015-0345-1