Abstract
Introducing newborn screening (NBS) services for sickle cell disease (SCD) in Africa has been proven to be one of the most cost-effective approach to reducing morbidity and mortality associated with this condition. In view of this evidence, efforts have been made by countries in Africa where SCD prevalence is high to pilot NBS programmes and to strengthen comprehensive care services for SCD. While it is important to reap the benefits of NBS for SCD in Africa in terms of overall quantitative measures, it is also important to understand how certain social and cultural conditions may disproportionately influence the outcomes of screening for some groups. The aim of this study was to analyse the role of gender norms before and after NBS for SCD in Tanzania, and to assess how they influence the quality of care of diagnosed children. Using qualitative methods, we did in-depth interviews with families of children with SCD identified through the NBS services and focus group sessions with nurses working in neonatal and postnatal sections of regional referral hospitals in Dar es Salaam. By analysing the experiences of both the families and nurses, we were able to provide evidence on, firstly, the gendered relations that undergird childcare and, secondly, how those relations influence the quality of care the child may potentially receive. The results emphasize the importance of studying the social implications of SCD in Africa, especially with regard to improving the quality of care for patients with SCD in the region. We propose simple interventions, including gender-conscious health education and genetic counselling, which can help to improve the community understanding of genetic diseases while also reducing gender-related inequalities related to SCD care in Africa.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
SCD is one of the most common genetic conditions in Africa. Of the 300,000 births of children born with SCD globally each year, 75% are in Africa, making it the most-affected region worldwide (Kuznik et al. 2016; Makani et al. 2011). Clinical manifestations of the disease can include pain crises, anaemia, infections, stroke and organ damage—all of which can cause frequent hospitalizations and early death (Makani et al. 2011; Saidi et al. 2016; Lima et al. 2014; Wang et al. 2015). Without intervention, 50 to 90% of the children born with the disease will die before 5 years of age (Chakravorty and Williams 2015). However, early identification of SCD-affected children through NBS complemented with prophylactic interventions and comprehensive care services has been shown to reduce the number of under-five mortalities by almost 70% (King et al. 2015; Yanni et al. 2009). In response to this evidence, efforts have been made by countries in Africa where SCD prevalence is high to pilot NBS programmes and to strengthen comprehensive care services for SCD (Ohene-Frempong et al. 2008; Tshilolo et al. 2008; Odunvbun et al. 2008; Mcgann et al. 2013; Tubman et al. 2016; Green et al. 2016; Kuznik et al. 2016; Nkya et al. 2019).
Tanzania is among the countries with the highest birth rates of children with SCD in Africa (Makani et al. 2011). In 2015, following the successes of NBS programmes in other African countries, the first pilot NBS project was started with the intention of assessing the feasibility of implementing NBS for SCD in Tanzania (Nkya et al. 2019). Since then, there has been significant progress in integrating NBS and comprehensive care services for SCD into the existing public healthcare infrastructure (Tluway and Makani 2017). While it is important to harness the benefits of NBS for SCD in Tanzania and Africa in general, it is also important to understand how social and cultural constructs may disproportionately impede the success of SCD interventions in particular ways in different settings (Okwi et al. 2009; McGann et al. 2015; Wittenbrink 2016; Green et al. 2016; Brown 2012; Galadanci et al. 2014; Mukinayi et al. 2018). Evidence in countries like Brazil, where prevalence of SCD is high, suggest that despite the availability of NBS and comprehensive care for SCD, mortality and morbidity trends were still high (Sabarense et al. 2015; Lima et al. 2014). Poor outcomes were linked to low public knowledge of the disease, as well as economic and social factors (McGann et al. 2015). The factors outlined by McGann et al. also resonate in many parts of Africa. Therefore, as Tanzania moves to expand its NBS and comprehensive SCD care services, it is important to consider the specific ways in which social, political and economic factors shape the implementation of health interventions.
To this end, this article specifically unpacks the connections between socially constructed gender roles and norms in Tanzania, and the implementation of new NBS programming. We add to a body of sociological and qualitative literature which demonstrates the systemic vulnerabilities that women face in SCD care. For example, qualitative studies have shown that, in some communities in Africa where the prevalence of SCD is high, the disease is believed to originate solely on the side of mothers (de Vries et al. 2020; Daak et al. 2016; Dennis-Antwi et al. 2011; Green et al. 2016; Marsh et al. 2011; Mubyazi and Njunwa 2011; Mukinayi et al. 2018; Nzewi 2001). The gendering of sickle cell inheritance, and the blame placed on mothers alone, contributes to a problematic stigmatization of mothers raising children with the condition (Marsh et al. 2011; Fullwiley 2006). This can negatively impact marriage and family relationships and, in the most extreme cases, can contribute to many fathers’ decision to leave women alone to bear the entire burden of caring for the child (Dennis-Antwi et al. 2011; Marsh et al. 2011). Studies done elsewhere have also shown how the social and psychological burden of care for a child with SCD often falls disproportionately on mothers (Marsh et al. 2011; Evans et al. 1988; Craft-Rosenberg et al. 2012; Mitchell et al. 2007; Neilsen 2013; Wittenbrink 2016; Olwit et al. 2018; Aiko Bruce et al. 2018; Green et al. 2016). This literature collectively emphasizes the need to focus specifically on the intersecting vulnerabilities of gender and SCD in Africa.
Our study emerges at this intersection, aiming to increase the body of knowledge around SCD, gendered narratives and the potential effects of gender norms on the quality of care of diagnosed children, before and after NBS for SCD in Tanzania.
Methodology
Study setting
This study was implemented in Dar es Salaam region in Tanzania where both pilot NBS for SCD programmes of 2015/2016 and 2017/2018 were implemented. The 2015/2016 project was implemented in Temeke regional hospital and Muhimbili National Hospital. The programme that started in 2017 was implemented in Temeke regional hospital with plans to expand in Amana and Mwananyamala hospitals. Figure 1 provides context of the three regions in Dar es Salaam and the geographical distribution of registered SCD patients between 2004 and 2009 in the region (Makani et al. 2011).
A map of Dar es Salaam regions showing geographical distribution of SCD patient in the region between 2004 and 2009, extracted from Makani et al. 2011 (Mortality in Sickle Cell Anemia in Africa: A prospective cohost study)
Study population and enrolment
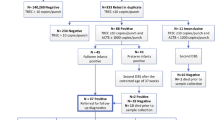
Participants for this study were families of children with SCD identified through the NBS programme and nurses working in postnatal and neonatal sections in regional and district hospitals in Dar es Salaam (Nkya et al. 2019). Parents and other caretakers (e.g. grandparents, adult siblings or other extended kin) were recruited by phone and during clinic visits in the Paediatric Sickle Cell Clinic in Temeke District Referral Hospital. In total, 47 children were found to have SCD from the pilot screening programmes between October 2015 and March 2019. Out of this total, 27 families were randomly selected and invited to participate in this study, but only 15 families participated. Reasons for non-participation are as follows: 2 mothers could not participate because their children died, 1 mother moved to another city, 5 families were not reachable, 1 mother agreed to participate but did not show up for the interview, 1 mother was sick, 2 families denied having children with SCD when contacted. Figure 2 summarizes the enrolment process for families. We also enrolled 14 nurses working in postnatal and neonatal sections of three regional referral hospitals in Dar es Salaam. Enrolled nurses were from postnatal and neonatal sections because nurses in those sections were involved in the implementation of NBS programmes. The aim of engaging with healthcare workers was to understand their experiences of working with sickle cell patients and their families, and especially their perspectives on the place of gendered roles in sickle cell care.
Data collection methods
In-depth interviews (IDIs) and focus group interviews (FGIs) were used as data collection methods. All interviews were conducted by the first author (DB) in Swahili and were audio recorded. Duration of the interviews were between 45 and 60 min. Guides were used to structure both the group discussions with nurses and in-depth interviews with families, but neither discussions nor interviews were strictly limited to the content of the guides.
In-depth interviews/focus group interviews
In-depth interviews (13) and focus group interviews (1) were conducted with families whose children were diagnosed with SCD through the NBS programme between 2015 and 2019. After the first and only focus group interviews with three mothers (P4, P14, P15), the research team decided the method was not practical to collect meaningful data and therefore in-depth interviews became the main method used to collect information from the mothers. Three out of the 13 IDIs conducted with families were conducted with two interlocutors together—P5, P6, P13. The interviews labelled P5 and P6 were with couples, and P13 was with a mother and grandmother of the child together. The two interviews with couples (P5 and P6) were the only interviews for this study that included fathers. The remaining interviews were done with only mothers. The interlocutor from the in-depth interview labelled P4 was also a participant in the initial focus group interview. Out of the 15 mothers, three (P1, P3, P4) have older children with SCD, and two of the mothers who participated in the FGI were first-time parents (P14, P15). Participants came from varying domestic relationships: some were mothers who still live with the fathers of their children, some were separated from the children’s fathers at the time of the interview, and others were other extended kin (such as grandparents) who were caring for the child in lieu of, or alongside, parents. During the interviews, we were interested in understanding who the mothers rely on for support and what source of support they receive from the child’s father and other family members. Summary of the enrolment flow chart for the IDIs and FGIs is described in Fig. 2.
Focus group discussions with nurses
Four FGDs were conducted with nurses working in postnatal and neonatal units of three regional hospitals in Dar es Salaam region. In the pilot NBS for SCD programmes at Temeke and Amana Hospitals, interviews were done in postnatal and neonatal sections respectively. At Mwananyamala hospital, interviews were done with nurses from both postnatal and neonatal sections. The discussions with the nurses were done in hospital settings and at times the number of participants fluctuated from three to five with some nurses leaving and joining as they became available. Using FGD guide, we requested nurses to describe scenarios that they have encountered gender-related issues. Nurses who participated have more than 2 years of experience working in the hospitals and also in either postnatal or neonatal section. Summary of the enrolment process is described in Fig. 3.
Data management and analysis
The interviews were digitally recorded and transcribed verbatim. The audio files and Word versions of the transcriptions were filed in project folders on an encrypted laptop. The transcriptions were cleaned and prepared for analysis. Thematic content analysis was used to guide data analysis in this study as described elsewhere (Treadwell et al. 2017). The analysis started with a reading of the transcriptions and listening to the audio records. The initial translations from Kiswahili to English were done randomly for only five transcripts (FGI with families and IDIs number one to four) to allow more people to be involved in the analysis stage. DB started coding the five transcripts in English and used the transcripts to develop a codebook. The coding process was determined by the main research aim: to understand the experiences of families and nurses related to the gendered aspects of childcare before and after a newborn tests positive for SCD. After the initial coding, parts of two transcripts were anonymized and coded with a group of eight members. The input from the group was used to further inform the development of the codebook (DeCuir-Gunby et al. 2011). The codebook was then used to code the remaining transcripts. When new issues came up from other transcripts, a new code was added to best represent the quotation. The process of analysing, interpreting and connecting the meanings of the different codes was done manually through iterative process until no new information emerge from the transcripts (DeCuir-Gunby et al. 2011). Related codes were grouped into similar thematic groups. Further translation into English was only necessary for the quotations included in this paper.
Results
The themes emerging from the in-depth interviews and group interviews were grouped into six main themes: (1) ways in which a father or husband was considered to be supportive to the mother; (2) ways in which mothers relied on support from other family members; (3) ways in which socio-cultural norms exacerbated vulnerabilities of the mothers; (4) ways in which healthcare provision reinforced the existing gender vulnerabilities; (5) ways that healthcare professionals could work with families to reduce the burden of vulnerabilities to the mothers; (6) potential consequences if mothers were left without support.
Ways in which a father or husband was considered to be supportive to the mother
Support through understanding and caring for the child (or children)
In interviews, mothers expressed several ways that they thought their partners were supportive. Some mothers expressed support and understanding from their partners from the beginning when provided with the test results for SCD:
...My husband prepared me for a long time before breaking the news [that the newborn child has SCD], and I am thankful that the results were given to him first. He [the husband] told me to be strong because another child has SCD as well [older children who are twins had SCD], so I got myself together and started attending clinics. (P1)
In other cases, mothers reported support from partners to help with the sick child, especially for families with older children who have SCD. In one particular family (P4), an older child with SCD was sick and had to be hospitalized and the mother has a newborn baby who has SCD too. The father stayed in the hospital with the older child while the mother went back home to take care of the newborn baby.
... His dad [her husband] will have to come back from work and stay with him [the older child] in the hospital, and I will have to go back home with the baby. (P4).
Support and understanding if the father has a family member with SCD
Most of the participating mothers who described their partners as supportive and understanding also mentioned that their partners had family members with SCD. The impact of a partner’s experience with SCD in their extended family is exemplified by the quotations below from two mothers, P2 and P1:
I am so grateful that my husband is very supportive of our child. He is treating him like all the other children, also [mother remembered something], when he heard that our child has SCD, he asked his mother if there has been a family member with the disease in their own family, and his mother told him yes, and he [the husband] told her [his mother], the problem [the disease] has now entered in my family and I can’t do anything about it. (P2)
P1 was specifically asked why she thinks her husband is very supportive. This was her response:
He [the husband] is supportive because he knows the problem is in his family [finish with emphasis]. His sister has the same disease, she is always sick but both her children do not have the disease, but they [her children] have inherited this disease through her brother [who is her husband], so the problem is on his side!! (P1)
Financial support through providing for the healthcare costs
Unsurprisingly, fathers or husbands were also considered supportive when they contributed to the healthcare-related costs. This may be through providing the bus fare to the clinics, paying for the healthcare costs or buying health insurance.
As I have told you [interviewer], if he [father of the child] knows we need bus fare or maybe the child has flu or fever, he will give us money to buy medicines…if we told him we don’t have folic acid or Pen v [Penicillin], he will give us money to buy the drugs. I’m so thankful to God and that’s how we live. (P9)
An interview with P5 shows in what ways fathers can be counted on by their partners despite not being able to come to the clinics:
He can’t come to clinics because of work responsibilities, but for us to attend clinics he is giving us money for transport and food. And he knows with our hospital you can’t just come and go so he must also give us money to eat in the afternoon. (P5)
Fathers who are supportive but unavailable due to work responsibilities
Some mothers acknowledge the limitations on how men can be expected to be supportive, citing their time commitments and work responsibilities. They divide the responsibilities of familial care into the domestic, day-to-day labour and the need for “feeding the family”:
It’s not like my husband is not willing to support me, because there are other men who might say “don’t tell me anything about your child, just deal with it yourself” [complete abandonment], but there are men who will tell you like this: “I really want to help you, but if I will stay at home with you taking care of the child or going to the clinics with you, that means you will not eat that day. (P3)
Ways in which mothers relied on support from other family members
Most of the mothers who were involved in this study have described receiving support from close family members to help in caring for the children. The support was more likely if the family already had a history of SCD, especially in the husbands’ families. Interestingly, all the support mentioned were from other women, whether within the family or outside the family.
When we asked P10 how she manages having a child with sickle cell alongside two other young children, this was her response: “If she’s sick and will have to be hospitalized, my sister [the child’s aunt] will stay with her in the hospital, I will have to stay at home with my little children but will go to the hospital every day to bring them food” (P10).
A more detailed explanation was provided by P3, who she is seeking support in the absence of the father.
There was this day when I came to the hospital with my two kids. The older child was hospitalized and his father was not around [he travelled]. When I got to the hospital, I had to call one of my relatives [to tell her] that I am here at the hospital and my son has been hospitalized, please come and help me with the other kid, and she came to the hospital to help me out. (P3)
Since this mother had three other children besides the two children with SCD, we were interested to know who is taking care of the other three children at home if she is hospitalized. Here was her follow-up response: “My fourteen-year-old daughter will be at home cooking for the other kids and taking care of the house” (P3).
During one of the interviews of a young mother of a child with SCD and her mother (P13), we noticed that the grandmother was more active in responding than the mother. We asked the mother why she was quiet and the grandmother responded “She goes to work every day and I am the one who lives with the child and is taking care of the child”. The family did not want to comment on the father’s involvement in supporting the child.
Ways in which own socio-cultural norms exacerbate vulnerabilities of the mothers
Some of the experiences of the mothers seem to originate from socio-cultural norms. The initial response from majority of the fathers after receiving the news that the child has SCD was to assume that the child got the disease from the mother. Some issues raised by the families indicated stigma in the communities associated with the disease.
In the beginning, he said [the husband] you are the one who has the problem, but this problem is not even in my own family. Just a day before yesterday, when I was educated that this may happen from both parents. I did educate him and I think he has started to understand. FGD with the mothers, P14
During the focus group discussion with nurses at Temeke hospital, participants shared a similar concern:
In many families when the problem (SCD) happens, women will be blamed and not the men, they will think SCD is from the mother’s side and may even decide to stay far away from the family and this is because of the paternalistic societies we live in. You will mostly see this happening to poor families and not the middle or upper class families. Nurses FGD (1) _ Hospital (1)
Ways in which healthcare provision reinforced the existing gender vulnerabilities
During the interviews, we noted mothers were requested to screen their newborn babies while in the postnatal ward and at this point fathers were not involved. Except for one family, fourteen mothers involved in this project received the results themselves directly through telephone. Thereafter, they came for the post-results counselling or health education session, again most of them returning without their partners. During the FGIs mothers were asked if, at any point during the NBS, men were involved and if they felt it was important to involve men in the decision-making. All three mothers said they felt that there was no need to involve men. Later they were further asked whether, looking back, they still thought men were not supposed to be involved. Here are a few responses from the mothers:
I think it would have been better if men were involved, I just assumed that I will just tell him and he will be able to understand, because everything was going very fast and I didn’t think we needed to wait for his decision [the fathers’ decision]. I also left his phone numbers, so we were both waiting for the results together. FGD with the mothers, P15
In one of the interviews with both parents (P6), the results were given to the father first. In this couple, we noticed better understanding and support from the father.
I receive a call from the doctor and was asked to come to the hospital, at that time my wife was not in town, so I came to see the doctor alone [without the baby]. There were other families and we were educated about the disease, but I want to know more about this disease. (P6)
The example below comes from a mother whose husband was in denial after being provided with the results. For this couple, the education session helped the husband to understand their joint role in genetic inheritance:
My husband was shocked [knowing that the child has sickle cell] because we both [mother and father] don’t have SCD, so where did the disease come from? But when we came here [hospital] we were educated and slowly started to understand. (P9)
During the FGDs with the nurses, we asked if they thought men were supposed to be involved and how they could be involved.
There is a need for both the mother and the father to be involved, because for the child to get SCD will require both parents to have the trait. Even in the screening form, we request for the father’s number, but mostly we educate the mothers who will go and tell the father. Nurses FGD (3) _ Hospital (2)
Together, the above quotations suggest two points: (1) families benefit when both fathers and mothers are equally included in the diagnosis and health education process and (2) since equal inclusion is rare, mothers were left with the dual responsibility of caring for the child and educating their partner.
Ways that healthcare professionals could work with families to reduce the burden of vulnerabilities to the mothers
Nurses had several suggestions for ways that the healthcare system could potentially work to reduce the burden on women. For example, in the discussions with nurses in the neonatal section at hospital (2), a suggestion was made to start providing health education on SCD at the antenatal clinics. This is because most mothers come to the clinics with their partners at least once during their antenatal visits.
Education reaches the men but very little and based on how the women understand. From my experience, men do come to the antenatal clinics although the number is still very small. And for those who will come with their partners they will be given first priority [assuming that they have to go back to work], we can do the same in sickle cell clinics, but I am sure the number of men will still be very small. Nurses FGD (2) _ Hospital (2)
In the discussion with nurses at the hospital (3), one nurse provided an example from her own experience in counselling a family with albinism to come to terms with the child’s condition. Nurses were optimistic that proper counselling and education at the clinic would help to educate the men into accepting the situation and to also provide support to the mother in childcare.
I will give you an example, I once saw a child with a genetic condition [albinism]. Both parents they never knew someone in their own families who had albinism. The mother was so shocked, how is she going to tell the husband. When the father came to see the child, we asked him to come in the office, we educated him that the child with albinism is like any other child but will need extra protection. When they left the hospital they both accepted the situation and thought it was normal. We can do the same with SCD, but as what the other nurse has said, the education should start during the antenatal section. Nurses FGD (4) _ Hospital (3)
Potential consequences if mothers were left without support
In the case of most mothers interviewed in this study, it was so clear how much they are struggling with the burden of caring for their child with sickle cell, as well as other children, alongside other domestic responsibilities if left without support. Even when available at home, men seem to leave the responsibilities of caring for the children to the mothers. Even when men are working, they do hesitate in financially supporting the healthcare costs of the children. Only 2 of the 15 women interviewed in this study were working mothers and therefore the remaining 13 mothers were fully financially dependent on their husbands or families.
But in most of the times, if I can be honest, for example, a child may be sick at night and I will tell him that the child is not feeling well, he is just going to tell me to take the money and go to the hospital alone with the child. (P3)
A similar concern was also raised during the discussion with the nurses,
If you visit the sickle cell clinics you will find mothers who are there struggling with the children, if you ask them, some will say when the baby was born and started to get sick so often, the father abandoned us. Those cases are so many in sickle cell clinics. Nurses FGD (2) _ Hospital (2)
Most of the mothers who were not working could not afford to buy health insurance for the kids, when asked what the response from the fathers or husbands is:
Now, I am pushing for the kids to have insurance, I remind him all the time, but you know the problem with men, it is until you push him so much before they agree on anything, but not for them to decide on their own. (P4)
Discussion
Findings from this study provided evidence of how parental responsibilities in the care of SCD have been highly influenced by gender. Previous studies have similarly focused on domestic work, the gendered division of labour and the care of chronically ill children (Doucet 2015). Research has shown that the pre-existing role of mothers within the family, especially household responsibilities including taking care of the children, continues even as care for a chronically ill child increases the demands on her labour (Hartmann 1981). The research described here reinforces these conclusions; the primary responsibility of caring for a child with SCD in Tanzania is largely understood as mothers’ responsibility.
These routine negotiations between different kinds of domestic responsibilities and care suggest a need to pay attention to the demands that SCD care places on the time and availability of caretakers, which in this case is the child’s mother. This research specifically aims to understand how new measures to increase NBS in Africa could be better designed to address gender inequities. Here we recognize that there are particularities of both the healthcare setting and gendered relations in Africa that add unique challenges to chronic care. We wanted to understand how the quality of care for SCD in Tanzania changes based on the dynamics of gender within a household. This study cautions against the wholesale implementation of public health interventions used elsewhere without careful analysis of the local specificities of gender relations and roles. Below, we focus our discussion of the results around three points that have direct implications for the long-term quality of SCD care: systemic vulnerabilities, support provision and the role of the clinic.
Gendered layers of vulnerabilities
The vulnerability of the mothers in this study increased with an increased burden of care. The burden became greater as the number of children with SCD in the family also increased. As SCD is a recessively inherited genetic disease, there are chances of the family having another child with the disease. The mother who was already burdened with the responsibilities of caring for one child or more children with SCD is now crippled with the additional burden of having a second child with SCD. This is somewhat mitigated by the accumulation of knowledge and experience managing the disease for other children. But the time commitments of hospitalizations, clinic visits and disruptions of daily life increase with each additional child. This has implications for the available time a mother can spend on other responsibilities, whether domestic or otherwise.
These problems were to some extent compounded by the fact that some families, informed by a socio-cultural belief system, blame mothers for the inheritance of the sickle cell gene. This blame is often reduced when the husband’s family has a known history of having a family member with the disease. In some families, this lay understanding of the origin of the disease limits the support the mother may potentially receive from the husband and his family—a finding that echoes previous studies (e.g. Treadwell et al. 2015; Dennis-Antwi et al. 2011; Marsh et al. 2011). However, for families where men provide financial support for the healthcare-related costs, children were more likely to access and afford the healthcare. For other families in which men were less supportive, what women were able to achieve was limited by the fact that they were not be able to afford the healthcare-related costs, which exacerbates the different layers of vulnerabilities that the mothers are already experiencing (Luna and Vanderpoel 2013).
To describe all of the ways in which women in Tanzania could potentially be vulnerable is beyond the scope of this article. But we hope to have demonstrated here that (1) the responsibilities of care for a child or children with SCD jeopardizes women’s abilities to engage in expected forms of domestic and non-domestic labour and (2) blame for the genetic inheritance of SCD raises the potential for abandonment and compounds existing vulnerabilities. More research should be done on how women cope with and resist these vulnerabilities; in this study, we saw how single mothers are sometimes able to successfully manage their children’s care even independently without support. But more visible were the ways in which the responsibilities placed on women to manage a newborn with SCD both reflect and reproduce gendered inequities, and further, the necessity of systems of support for women caring for sickle cell–diagnosed children.
Support in many forms
In addition to demonstrating the necessity of support for sickle cell care, the results demonstrate the ways in which support can take many different forms. In some families, men were emotionally supportive in caring for the sick child, but their practical availability for care was limited due to work responsibilities. Some of these fathers do provide financial support for healthcare-related costs, including bus fare, medicines and health insurance. In these families, children were more likely to access healthcare, and the families could afford healthcare costs. Understandably, in families in which men were less financially supportive, mothers described feeling frustrated by limitations to accessing healthcare and were unable to afford healthcare-related costs. Out of 15 mothers interviewed in this study, only two mothers were employed outside the home and therefore depend on financial support from their partners for both normal household expenses and the extensive costs of medical care. This observation complemented findings from studies elsewhere which reported improvement in quality of childcare in a family where both parents are involved (Evans et al. 1988; Mitchell et al. 2007; Craft-Rosenberg et al. 2012).
The results above also suggest that financial support is not the only form of support that women rely on; mothers of children with SCD discussed the need for a shared emotional burden of care, and the burden of collecting knowledge and understanding the disease treatment, as well as the need for the support in going to clinic appointments, hospitalizations and managing routine care as exemplified by P3.
In most cases where men were not involved, mothers tend to rely for support from other family members. However, even the support outside a mother and a father is gendered. Mothers were more supported by other women within their own extended families than men. It is also worth noting that it is common for families affected by SCD to rely on their families for emotional or financial support, a point brought up in previous research as well (Fullwiley 2006; Craft-Rosenberg et al. 2012). This all suggests that, given the gendering of domestic care work, health providers should consider the other relevant networks of support beyond the mother-father dyad. Genetic counselling may need to include women within the larger support network, and public health interventions should consider how to best accommodate the multiplicity of forms and providers of support that facilitate healthcare attainment.
In this study, familiarity with the disease also played an important role. If the husband’s family history includes any family member with SCD, the mothers were more likely to be supported compared to mothers whose husband’s family were unfamiliar with the disease. Here this shifts slightly the way we might think about genetic counselling and health education. It is important for health interventions to move beyond the nuclear family unit, and to consider the ways in which extended familial relationships can support, hinder or otherwise change the level of access to and quality of SCD care.
The role of the clinic in reproducing inequality
The results here also point toward the role of the clinic in reproducing gendered inequality. With no ill intent, the clinic culture has continued to assume the role of the mother as the primary caretaker of chronically ill children. While this may reflect the reality of many families, the clinic’s assumption can actually perpetuate or naturalize care as women’s work. For example, as shown in the results, when mothers were asked to screen their children for SCD in the postnatal ward, their partners were not involved. And similarly, when the results were given out, the calls were made to the mothers alone. Out of the 15 women involved in this study, only two came with their husbands for education after the screening. In only two families, results were given first to the father by the clinician, mostly because the mother’s phone was not reachable. In those families, we noticed that the fathers were more supportive of the child’s healthcare needs. Similar results were observed in families where the fathers attended the education session after the screening. Using the cases in this study, it is fair to assume that if men were involved from the beginning, then they will feel as responsible as women in taking responsibility for childcare.
These results signify the need for genetic counselling and health education models to emphasize fathers’ involvement in childcare. Positive outcomes are expected based on previous engagement models elsewhere that involve men (Gervais et al. 2015). Broadly, there needs to be a balance between making fathers feel equally responsible for children’s healthcare, making sure that mothers are equipped to access care if they are not supported and including extended kin networks as support for the child’s healthcare.
Conclusion
Through analysing the gendered experiences of a small subset of families who were identified through the NBS programme, this study strengthens evidence on how the burden of sickle cell care may affect women more heavily than men—building on previous studies of the gendered nature of sickle cell care. It also demonstrates that there are specific areas for potential intervention: (1) different layers of vulnerabilities experienced by the mothers, (2) the need for different forms of support from a wide variety of people and how they can be integrated in the healthcare (3) and the clinic as a potential site for reproducing gender inequities. We propose simple interventions, including gender-conscious health education and genetic counselling, which can help to improve the community understanding of genetic diseases while also reducing gender-related inequalities related to SCD care in Africa. Additional attention to these areas by bioethicists, public health workers and healthcare providers would be an important step in improving sickle cell care as NBS and other comprehensive care services become more available. While we narrowly offer evidence here on SCD, NBS and gender roles in Tanzanian healthcare, this study has larger implications for how we think about the efficacy of a health intervention, and the need for feminist approaches to the ethics of genetic medicine in Africa.
Study limitations
This study was implemented in a hospital setting. In view of that, participants at times may have said things they believed were acceptable in those settings.
References
Brown S-E (2012) Cultural models of genetic screening & perceptions of sickle cell disease in high-risk Guadeloupean French communities. Dissertation Abstracts International Section A: Humanities and Social Sciences. ProQuest Information & Learning. http://ezproxy.ecu.edu.au/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2012-99050-452&site=ehost-live&scope=site
Bruce A, Aisha AW, Alvadj-Korenic T, Mayan M, Greenslade H, Plaha M, Venner MA (2018) A complex interface: exploring sickle cell disease from a parent’s perspective, after moving from Sub-Saharan Africa to North America. Pediatr Hematol Oncol 35(7–8):373–384. https://doi.org/10.1080/08880018.2018.1541949
Chakravorty S, Williams TN (2015) Sickle cell disease: a neglected chronic disease of increasing global health importance. Arch Dis Child 100(1):48–53. https://doi.org/10.1136/archdischild-2013-303773
Craft-Rosenberg M, Pehler S-R, Houston ML (2012) Sickle cell disease and the family. In: Encyclopedia of Family Health. SAGE Publications, Inc. https://doi.org/10.4135/9781412994071.n314
Daak AA, Elsamani E, Ali EH, Mohamed FA, Abdel-Rahman ME, Elderdery AY, Talbot O, Kraft P, Ghebremeskel K, Elbashir MI, Fawzi W (2016) Sickle cell disease in Western Sudan: genetic epidemiology and predictors of knowledge attitude and practices. Trop Med Int Health 21(5):642–653. https://doi.org/10.1111/tmi.12689
de Vries J, Landouré G, Wonkam A (2020) Stigma in African genomics research: gendered blame, polygamy, ancestry and disease causal beliefs impact on the risk of harm. Soc Sci Med 258(May):113091. https://doi.org/10.1016/j.socscimed.2020.113091
DeCuir-Gunby JT, Marshall PL, McCulloch AW (2011) Developing and using a codebook for the analysis of interview data: an example from a professional development research project. Field Methods 23(2):136–155. https://doi.org/10.1177/1525822X10388468
Dennis-Antwi JA, Culley L, Hiles DR, Dyson SM (2011) ‘I can die today, I can die tomorrow’: lay perceptions of sickle cell disease in Kumasi, Ghana at a point of transition. Ethn Health 16:465–481. https://doi.org/10.1080/13557858.2010.531249
Doucet A (2015) Parental responsibilities: dilemmas of measurement and gender equality. J Marriage Fam 77(1):224–242. https://doi.org/10.1111/jomf.12148
Evans RC, Kathleen Burlew A, Oler CH (1988) Children with sickle-cell anemia: parental relations, parent-child relations, and child behavior. Soc Work (U S) 33(2):127–130. https://doi.org/10.1093/sw/33.2.127
Fullwiley D (2006) Biosocial suffering: order and illness in urban West Africa. BioSocieties 1(4):421–438. https://doi.org/10.1017/s1745855206004042
Galadanci N, Wudil BJ, Balogun TM, Ogunrinde GO, Akinsulie A, Hasan-hanga F, Mohammed AS et al (2014) Current sickle cell disease management practices in Nigeria. Int Health 6(1). https://doi.org/10.1093/inthealth/iht022
Gervais C, de Montigny F, Lacharité C, Dubeau D (2015) The father friendly initiative within families: using a logic model to develop program theory for a father support program. Eva Program Plann 52(October):133–141. https://doi.org/10.1016/j.evalprogplan.2015.04.006
Green NS, Mathur S, Kiguli S, Makani J, Fashakin V, LaRussa P, Lyimo M, Abrams EJ, Mulumba L, Mupere E (2016) Family, community, and health system considerations for reducing the burden of pediatric sickle cell disease in Uganda through newborn screening. Glob Pediatr Health 3(March):2333794X1663776. https://doi.org/10.1177/2333794x16637767
Hartmann HI (1981) The family as the locus of gender, class, and political struggle: the example of. Source: Signs. 6
King LGC, Bortolusso-Ali S, Cunningham-Myrie CA, Reid MEG (2015) Impact of a comprehensive sickle cell center on early childhood mortality in a developing country: the Jamaican experience. J Pediatr 167(3):702–705.e1. https://doi.org/10.1016/j.jpeds.2015.06.028
Kuznik A, Habib AG, Munube D, Lamorde M (2016) Newborn Screening and prophylactic interventions for sickle cell disease in 47 countries in Sub-Saharan Africa: a cost-effectiveness analysis. BMC Health Serv Res 16(1):304. https://doi.org/10.1186/s12913-016-1572-6
Lima ARG, Ribeiro VS, Nicolau DI (2014) Trends in mortality and hospital admissions of sickle cell disease patients before and after the newborn screening program in Maranhão, Brazil. Rev Bras Hematol Hemoter 37(1):12–16. https://doi.org/10.1016/j.bjhh.2014.11.009
Luna F, Vanderpoel S (2013) Not the usual suspects: addressing layers of vulnerability. Bioethics 27(6):325–332. https://doi.org/10.1111/bioe.12035
Makani J, Cox SE, Soka D, Komba AN, Oruo J, Mwamtemi H, Magesa P, Rwezaula S, Meda E, Mgaya J, Lowe B, Muturi D, Roberts DJ, Williams TN, Pallangyo K, Kitundu J, Fegan G, Kirkham FJ, Marsh K, Newton CR (2011) Mortality in sickle cell anemia in Africa: a prospective cohort study in Tanzania. PLoS One 6(2):e14699. https://doi.org/10.1371/journal.pone.0014699
Marsh VM, Kamuya DM, Molyneux SS (2011) ‘All her children are born that way’: gendered experiences of stigma in families affected by sickle cell disorder in rural Kenya. Ethn Health 16(4–5):343–359. https://doi.org/10.1080/13557858.2010.541903
Mcgann PT, Ferris MG, Ramamurthy U, Santos B, de Oliveira V, Bernardino L, Ware RE (2013) A prospective newborn screening and treatment program for sickle cell anemia in Luanda, Angola. Am J Hematol 88(12):984–989. https://doi.org/10.1002/ajh.23578
McGann PT, Grosse SD, Santos B, de Oliveira V, Bernardino L, Kassebaum NJ, Ware RE, Airewele GE (2015) A cost-effectiveness analysis of a pilot neonatal screening program for sickle cell anemia in the Republic of Angola. J Pediatr 167(6):1314–1319. https://doi.org/10.1016/j.jpeds.2015.08.068
Mitchell MJ, Lemanek K, Palermo TM, Crosby LE, Nichols A, Powers SW (2007) Parent perspectives on pain management, coping, and family functioning in pediatric sickle cell disease. Clin Pediatr 46(4):311–319. https://doi.org/10.1177/0009922806293985
Mubyazi GM, Njunwa KJ (2011) Is sickle cell disease sufficiently prioritized in policy and socio-economic research on diseases in Tanzania? Lessons for the past 50 years. Tanzania J Health Res 13(5 SUPPL.ISS):1–14. https://doi.org/10.4314/thrb.v13i5.4
Mukinayi BM, Kalenda DK, Mbelu S, Gulbis B (2018) Awareness and attitudes of 50 congolese families affected by sickle cell disease: a local survey. Pan Afr Med J 29(January). https://doi.org/10.11604/pamj.2018.29.24.12276
Neilsen CM (2013) Chronic sorrow and illness ambiguity in caregivers of children with sickle cell disease. Master of Science Thesis- Human Development and Family Studies, Michigan State University
Nkya S, Mtei L, Soka D, Mdai V, Mwakale PB, Mrosso P, Mchoropa I et al (2019) Newborn screening for sickle cell disease: an innovative pilot program to improve child survival in Dar Es Salaam, Tanzania. Int Health 11:589–595. https://doi.org/10.1093/inthealth/ihz028
Nzewi E (2001) Malevolent Ogbanje: recurrent reincarnation or sickle cell disease? Soc Sci Med 52
Odunvbun ME, Okolo AA, Rahimy CM (2008) Newborn screening for sickle cell disease in a Nigerian hospital. Public Health 122(10):1111–1116. https://doi.org/10.1016/j.puhe.2008.01.008
Ohene-Frempong K, Oduro J, Tetteh H, Nkrumah F (2008) Screening newborns for sickle cell disease in Ghana: table 1. Pediatrics 121(Supplement 2):S120.2–S1S121. https://doi.org/10.1542/peds.2007-2022UUU
Okwi AL, Byarugaba W, Ndugwa CM, Parkes A, Ocaido M, Tumwine JK (2009) Knowledge gaps, attitude and beliefs of the communities about sickle cell disease in Eastern and Western Uganda. East Afr Med J 86(9):442–449
Olwit C, Mugaba M, Osingada CP, Nabirye RC (2018) Existence, triggers, and coping with chronic sorrow: a qualitative study of caretakers of children with sickle cell disease in a national referral hospital in Kampala, Uganda. BMC Psychol 6(1):50. https://doi.org/10.1186/s40359-018-0263-y
Sabarense AP, Lima GO, Silva LML, Viana MB (2015) Characterization of mortality in children with sickle cell disease diagnosed through the newborn screening program. J Pediatr 91(3):242–247. https://doi.org/10.1016/j.jped.2014.08.006
Saidi H, Smart LR, Kamugisha E, Ambrose EE, Soka D, Peck RN, Makani J (2016) Complications of sickle cell anaemia in children in Northwestern Tanzania. Hematology 21(4):248–256. https://doi.org/10.1080/10245332.2015.1101976
Tluway F, Makani J (2017) Sickle cell disease in Africa : an overview of the integrated approach to health, research, education and advocacy in Tanzania, 2004-2016. Br J Haematol 177(6):919–929. https://doi.org/10.1111/bjh.14594.Sickle
Treadwell MJ, Anie KA, Grant AM, Ofori-Acquah SF, Ohene-Frempong K (2015) Using formative research to develop a counselor training program for newborn screening in Ghana. J Genet Couns 24(2):267–277. https://doi.org/10.1007/s10897-014-9759-7
Treadwell MJ, Makani J, Ohene-Frempong K, Ofori-Acquah S, McCurdy S, De Vries J, Bukini D et al (2017) Stakeholder perspectives on public health genomics applications for sickle cell disease: a methodology for a Human Heredity and Health in Africa (H3Africa) Qualitative Research Study. OMICS J Integr Biol 21(6):323–332. https://doi.org/10.1089/omi.2017.0047
Tshilolo L, Kafando E, Sawadogo M, Cotton F, Vertongen F, Ferster A, Gulbis B (2008) Neonatal screening and clinical care programmes for sickle cell disorders in Sub-Saharan Africa: lessons from pilot studies. Public Health 122(9):933–941. https://doi.org/10.1016/j.puhe.2007.12.005
Tubman VN, Marshall R, Jallah W, Guo D, Ma C, Ohene-Frempong K, London WB, Heeney MM (2016) Newborn screening for sickle cell disease in Liberia: a pilot study. Pediatr Blood Cancer 63(4):671–676. https://doi.org/10.1002/pbc.25875
Wang Y, Liu G, Caggana M, Kennedy J, Zimmerman R, Oyeku SO, Werner EM, Grant AM, Green NS, Grosse SD (2015) Mortality of New York children with sickle cell disease identified through newborn screening. Genet Med 17(6):452–459. https://doi.org/10.1038/gim.2014.123
Wittenbrink B (2016) The relationship between support systems and disease burden for families coping with sickle cell disease in South Africa and Cameroon. Master of Science Thesis- Duke Global Health Institute, Duke University- North Carolina
Yanni E, Grosse SD, Yang QH, Olney RS (2009) Trends in pediatric sickle cell disease-related mortality in the United States, 1983-2002. J Pediatr 154(4):541–545. https://doi.org/10.1016/j.jpeds.2008.09.052
Acknowledgements
We thank the parents and nurses who have participated in this research, the Sickle Cell Programme at Muhimbili University of Health and Allied Sciences, and the staff and administration of Temeke, Amana and Mwananyamala referral hospitals in Dar es Salaam. We thank the feminists bioethics reading group at the Ethox Centre for their valuable inputs. We also thank Rebekah Ciribassi for her significant contribution in reviewing the revised version of this manuscript.
Funding
Commonwealth Scholarship Commission funded the first author (DB) to spend 1 year at Ethox centre where analysis and writing of this work was done. Research funding for this work was supported through DMRET and SPARCO grant.
Author information
Authors and Affiliations
Contributions
DB designed the study, interacted with participants, performed the interviews and assisted in the transcriptions and translations and analysis and drafting of the manuscript. JM and MP supervised the project and reviewed the drafts of the manuscript. LM assisted with the data collection and reviewing of the manuscript. CM, SN, SM and KM assisted in revising the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical consideration
The study was approved by the MUHAS Research Ethics Committee (Ref. No. 2017-10-20/AEC/Vol. XII/85). Written informed consent was requested from the participants prior to the conduct of the study. The study involved research participants who were 18 years and older to ensure that all participants have reached the legal age to consent as required by the Government of Tanzania. No identifiable information was collected during the interviews or discussions. Numbers were used to identify participants during the discussions. Hospital files of the children were not linked to the data collected for this study to ensure anonymity.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bukini, D., Mbekenga, C., Nkya, S. et al. Influence of gender norms in relation to child’s quality of care: follow-up of families of children with SCD identified through NBS in Tanzania. J Community Genet 12, 143–154 (2021). https://doi.org/10.1007/s12687-020-00482-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-020-00482-4