Abstract
Family health history collection and genetic testing are core elements for the successful translation of genomics into primary care practice. Yet, little is known about how pediatric providers implement these elements in practice. We surveyed the membership of the American Academy of Pediatrics regarding family health history (FHH) collection and genetic testing in the primary care setting. Three hundred forty-nine (349) responses were analyzed with the initial response rate of 43.3%. Four principal findings were noted—(1) family health history is still recognized as a critical part of the medical evaluation; (2) perceived obstacles for FHH are time in obtaining the FHH and concerns about the family’s knowledge of their FHH; (3) a 3-generation family history is out of the scope of routine care and alternate methods should be considered; (4) most primary care providers (PCPs) do not feel comfortable ordering, interpreting, and counseling regarding current genetic testing. Expanded genetic/genomic education at multiple levels (undergraduate medical education, graduate medical education, and maintenance of certification) is clearly indicated to allow PCPs to integrate these vital elements into a current evaluation (acute care or health maintenance) in the primary care setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The era of genetic and genomic medicine is upon us (Saul 2013). Various initiatives from different professional organizations are attempting to translate the incredible progress in the analysis of the human genome since the Human Genome Project from 1990 to 2003 to the clinical sector—especially the primary care sector (www.geneticsinprimarycare.aap.org; www.acmg.net; www.genome.gov/27554614).
In many ways, the family health history and its resultant pedigree is the first and foremost genetic test. This elegantly simple tool requires two steps—to collect it and to interpret what was collected (Tarini and McInerney 2013). The information obtained can guide the clinician and family alike as to the likelihood of various health problems in the family and suggest various clinical interventions, both therapeutic and supportive. This information can identify potential trouble signs or “red flags” that need attention early in childhood.
Despite the important role ascribed to genetic testing and family history in the translation of genomics into pediatric primary care, little is known about pediatric primary care providers’ perception of these elements. To provide a more thorough inquiry of primary care pediatric providers’ attitudes regarding family history screening and genetic testing practice management for children with genetic conditions, a survey of AAP members (Periodic Survey of Fellows #87) was initiated in 2014. The results, reported herein, provide an interesting analysis of the status of family history screening and genetic testing analysis across a broad sampling of AAP fellows.
Methods
Study design and study sample
Data were generated from the 87th Periodic Survey of Fellows conducted by the American Academy of Pediatrics (AAP). The Periodic Survey is distributed 3 to 4 times annually on topics of importance to pediatricians. The survey was an 8-page self-administered questionnaire mailed to a random sample of 1627 non-retired US members of the AAP selected from a list of 53,859 between December 2013 and June 2014. All mailings included an introductory letter from the executive director of the AAP and a business-reply return envelope; the initial mailing only included a flyer describing the periodic survey and its uses, as well as a $2.00-bill as a token of appreciation. Non-respondents were mailed another survey (maximum of 6 mailings) and emailed with a link to the questionnaire for on-line completion (maximum of two emails).
Survey questionnaire
PS#87 was designed in collaboration with members of the AAP Committee on Genetics and members of the AAP Genetics in Primary Care Institute (GPCI). Questions addressed pediatricians’ knowledge, attitudes, practices, and barriers surrounding family history taking and genetic testing/evaluation. Likert-type scales were used to assess the proportion of new and established patients with whom pediatricians collect and update family history information (collapsed to “never/rarely/some of the time” [1–50% of patients] vs “usually/most/all of the time” [51–100% of patients]). Pediatricians were also asked who collects family histories, where they are conducted and in what format, as well as the types of disorders and number of generations included in the histories (each with defined answer categories). Likert-type scales were also used to assess attitudes and barriers to family history taking and genetic testing/evaluation (collapsed to “strongly agree/agree” vs “neutral/disagree/strongly disagree”; “very important” vs “moderately/somewhat/of little or no importance”; and “moderate/significant barrier” vs “somewhat/not at all a barrier”). Questions on physician and practice characteristics were also included. The survey was approved by the AAP Institutional Review Board as exempt from human subject review and pilot-tested for clarity with a random sample of 200 AAP members. The survey instrument is available upon request from the corresponding author.
Data analysis
Analysis for this report is limited to pediatricians who have completed residency training, are General Pediatricians (defined as ≥50% of their professional time spent in General Pediatrics versus a Subspecialty), and provide patient care in an ambulatory care setting. Descriptive statistics were used to assess differences in response to family history taking and genetic testing/evaluation in pediatric practices by pediatrician practice and personal characteristics including age, gender, practice setting (solo/2-physician practice vs group/health maintenance organization vs hospital/clinic), practice location (inner city vs urban not inner city vs suburban vs rural), practice ownership (full or part-owner vs employee/independent contractor/other), estimated number of weekly health supervision visits, and proportion of patients covered by public health insurance (Medicaid, State Children’s Health Insurance Program (SCHIP), Tricare, or other) in their practice.
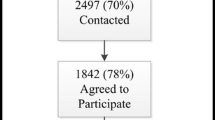
A total of 705 surveys were received (642 mailed and 62 electronic returns) for a return rate of 43.3%; 667 of those surveys were eligible and completed cases included in the analysis. The 349 responses used in the analysis were further selected by the criteria above (General Pediatricians [greater than or equal to 50% of their time in general pediatrics versus a subspecialty] who have completed residency training and provide care in an ambulatory setting). In order to assess non-response bias, we used one-sample proportion tests and t tests to compare respondents and the sample population on several characteristics (age, gender, geographical region of the US and AAP membership status) available through the AAP administrative database. Respondents were more likely to be older and have a membership status of full “Fellow” or “Specialty Fellow”; therefore, sample weights were created based on categorical age and membership status. The response rate for each subgroup is equal to the number of respondents in that subgroup divided by the total number in the eligible sample for that group. The non-response weight for a weighting class is calculated by taking the inverse of the response rate (i.e., 1/probability of responding). The weights were then rescaled in order to sum to the analytic sample size of 667 and to average back to 1. Weighted percents are given, along with unweighted counts and “Ns.” Analysis was conducted using SPSS Statistical software, version 18.0 (IBM SPSS, Inc., Chicago, IL).
Results
Respondents were primarily female (65%), identified themselves as white, and non-Hispanic/Latino (74%); the average age was 48 years. They reported an average of 91 ambulatory patient visits per work week, most provided care in a group practice or health maintenance organization (64%) and practiced in a suburban area (55%) (Table 1).
Family health history taking
The overwhelming majority (99%) of PCPs collected information about the health history of an individual’s biological relatives (the family health history) with either new or established patients. Ninety-seven percent of pediatricians report collecting family health history (FHH) with new patients and 67% report collecting FHH with established patients. The specific breakdown is shown in Table 2 for additional elements (updated FHH, place where FHH collected, person collecting the FHH, format of FHH form, method of recording FHH, generations of FHH collected, and the content of FHH collected).
As shown in Table 3, the respondents to this survey noted that the FHH is a very important part of primary care and they felt confident in being able to obtain the appropriate information and to establish a care plan based on that information. In addition, they noted the importance of knowing the breadth of disorders (family health) across generations. When the FHH revealed information that other family members may be at risk, 84.8% of PCPs agreed or strongly agreed that PCPs have a duty-to-inform such family members.
The predominant barriers to taking an adequate FHH were reported to be inadequate time (60.5%—moderate to significant) and uncertainty as to the accuracy/reliability of the information (38.5%—moderate to significant) (Table 4). Electronic health record utilization, lack of practice tools, and language or cultural differences were cited by less than 25% to be moderate or significant barriers to obtain the FHH.
Genetic testing
The approach to evaluation of patients identified as at-risk for a genetic related disorder will frequently involve genetic testing and/or referral to a geneticist or other specialist for testing. Three-fourths of pediatricians said they have identified at least one patient during the 12 months prior to the survey as at-risk for a genetic related disorder; the average number of patients so identified is 6.4. About one-half of pediatricians (50.6%) refer many or most/all of their patients identified as at-risk for a genetic related disorder to geneticists or other specialist rather than ordering genetic testing themselves. Less than 10% said they ordered genetic tests themselves (without referral) for many or most/all of their patients identified as at risk.
Nearly all (95.0%) of respondents had referred patients for genetic consultation (Table 5). Of those who referred patients, the following six (6) factors were all identified as “very” important in their decision to refer the following: complexity/severity of the disorder (71.5%), lack of knowledge about the condition (53.2%), desire for management recommendations (70.9%), known treatments are available (58.6%), parents’ desire for more information (61.7%), and providing information about recurrence risks/family planning (62.0%).
Availability of insurance coverage and malpractice concerns had less impact on decision making with insurance availability reported as very important by 20.9% of pediatricians and malpractice concerns reported by only 8.6%. Age, gender, practice area, and type of practice were not significantly associated with any significant differences in these decision factors.
The four (4) barriers (Table 6) most frequently identified by providers regarding their ordering of genetic testing were as follows: lack of training identifying genetic risks and choosing appropriate tests (53.1% reported as moderate/significant barrier), inadequate time during typical office visit to interpret genetic tests (48.9%), lack of training in genetic interpretation (60.2%), and lack of guidelines for care management (57.4%).
Seventy-two percent (71.8%) of pediatricians felt there are situations in which it is the role of the PCP to provide genetic testing and evaluation (Table 7). Only 7.0% of pediatricians felt they received frequent requests from parents for genetic testing. While the vast majority (86.2%) of pediatricians feel they are confident in their ability to interpret newborn screening results, a much smaller number feel confident in their ability to either interpret genetic test results (31.8%) or explain genetic test results to parents (36.0%).
Three-fourths of respondents reported they were either moderately (33.2%) or very (41.7%) interested in CME programs having to do with genetics in primary care.
Discussion
A previous literature review noted that perhaps genetics has focused so much on rare and unusual diseases that are rarely seen in the primary care setting that PCPs have a difficult time seeing the relevance of genetics and genomics in everyday practice and suggested that the real challenge is to engage providers with ways to apply genetics and genomics information into their practices (Mikat-Stevens et al. 2015). Scott and Trotter (2013) and Rinke et al. (2014) also discuss some of the perceived difficulties with the integration of genetics and genomics into primary care. The survey results reported herein integrate with four key points for advancing genetics and genomics and primary care—the importance of FHH to PCPs, perceived obstacles for obtaining the FHH for PCPs, how to obtain the FHH in a relevant manner, and genetic testing as a vital part of PCP care going forward.
The importance of FHH
The integration of genetics/genomics into primary care initially centers on the elegantly simple yet potentially complex FHH. The overwhelming majority of respondents (99%) collect a FHH. FHH is in the first wave of historical information that can direct a more targeted history-taking (by specific inquiries), suggest the search for additional features on physical examination, and lead to a variety of testing (radiographic, metabolic, genetic, and others). The importance of the FHH cannot be over-emphasized in the evaluation of the patients in the twenty-first century (Doerr et al. 2014; Edelman et al. 2014; Guttmacher et al. 2004; Pyeritz 2012; Wu et al. 2015; Yoon et al. 2002).
Perceived obstacles for FHH
A previous quality improvement project to see if tangible steps could be taken to advance the integration of genetic and genomic medicine in the primary care setting demonstrated that positive strides can be made but several obstacles still exist (Rinke et al. 2016). The amount of available time to obtain the FHH in the office setting and the family’s knowledge of their own FHH were perceived to be two main obstacles.
Sixty-one percent (61%) of PCPs in this study reported “inadequate time” to collect the desired information, and up to 39% noted that inadequate knowledge of one’s own family history was a barrier to sufficient FHH information. Additionally, 85% of PCPs feel the duty to warn families about risks in the family.
It is of interest that over three-fourths of the respondents collect the FHH in the exam room with entry into the EHR at that time. Over 50% of respondents report that they collect the information verbally with the family. Open-ended questions (37%) and checklists (51%) are employed frequently. This suggests that tools to facilitate FHH collection using modern technology will have increased acceptance going forward (especially for the collection of FHH in the exam room); so, the development of such tools should continue to occur. Such tools have not been created for broad distribution as of yet. The “Toolkit to Improve Care for Pediatric Patients with Genetic Conditions in Primary Care” provides some useful examples that can be used (https://geneticsinprimarycare.aap.org/YourPractice/Pages/Toolkit.aspx).
All of these obstacles should encourage the development of methods to enhance collection of FHH and assure its reliability to improve acceptance of the relevance of these tasks and their integral part in primary care medicine.
Obtaining a relevant FHH
Relevant FHHs (defined as FHHs that are clinically impactful now and going forward) are often dependent on the type of clinical encounter for the PCP. The reports of Tarini and McInerney (2013) and Scott and Trotter (2013) suggest a path forward for the time limitations that were noted in the survey. For an acute care visit with potential contributory FHH, a targeted FHH is pertinent. Such an FHH concentrates on specific disorders relevant to the presenting symptoms and might be multigenerational but not necessarily three generations. For a health maintenance visit, a tailored FHH focusing on health issues relevant to the child’s age and life stage might suffice. Like a targeted FHH, a tailored FHH might obtain multigenerational information but not necessarily three generations. A comprehensive FHH, information about a range of disorders in the family including disorders that might not be immediately relevant to the age-based health, might be collected as needed for a more complex situation in the PCP setting but is typically not practical for most clinical encounters. The PCP also has the opportunity to construct a progressive family history over the life of the child. This FHH will be particularly pertinent as the interaction with family progresses over the years and as each child transitions to adult care.
Though not specifically ascertained via the survey cited herein, we suggest that being instructed on the various “techniques” of FHH collection might demystify the perceived difficulties, increase its relevance in the primary care setting, and enhance care. Such instruction will need to be rooted in undergraduate medical education and expanded throughout the medical education process, including graduate medical education, continuing medical education and maintenance of certification.
Genetic testing as a vital part of care
Genetic testing is becoming a vital part of care going forward; yet, most PCPs report the need for more education (Saul 2013). Lack of experience, confidence, and care guidelines reported in this survey continue to be barriers in the optimal use of genetic testing. While more than half of the respondents identify lack of training to identify genetic risk factors and choosing appropriate tests as well as lack of training in genetic interpretation, the majority recognize the role of the PCP in the evaluation of the at-risk patient.
Most PCPs in this study report that genetic testing can provide helpful information about recurrence risks for other family members. However, these same providers overwhelmingly feel that geneticists are more qualified than they are to provide that genetic testing and evaluation. PCPs feel confident in their ability to interpret Newborn Screening results but are much less confident in their ability to interpret other genetic test results or in explaining these results to parents. The AAP’s published guidelines for the evaluation of individuals with global developmental delay do provide some guidance and suggest an initial evaluation that PCPs can consider (Moeschler et al. 2014).
Genetic testing has advanced over the last several decades leading to many different modalities currently available to the PCP. The advent of direct to consumer/physician marketing underscores the importance of the PCPs experience and confidence with the available testing options. While concern for family psychological distress or anxiety about genetic testing was not a significant barrier noted by respondents, recognizing and understanding the profound effects of genetic testing are particularly important in the pediatric population.
Further training and education regarding genetic testing in the primary care setting will logically have multiple benefits—faster recognition of conditions where early diagnosis and treatment are critical to care, ease of testing in resource-poor areas, enhanced collaboration with specialists, enhanced partnership between the PCP and the family, and greater confidence in PCPs for expanded care. These benefits can provide the PCP with the self-reliance necessary for many of the early stages of evaluations for patients with potential genetic conditions.
Limitations
This study only sampled members of the AAP, and at the time of the survey, it was estimated that approximately 62% of board-certified pediatricians were members of the AAP. The analysis was further restricted to general pediatricians who have completed residency and spent at least 50% of their time in the ambulatory care setting. The responses recorded were self-reported, and the survey analysts did not know the specific content that the respondents asked their families in the clinical setting.
Summary
The results of this study are consistent with the need for expanded genetic education in medical school curricula, residency education and continuing medical education to keep pediatric PCPs, in an ever-changing environment, adept at collecting and using FHH information and ordering and interpreting genetic testing. Additional strategies are needed to mitigate time barriers and maximize the ease of EHR use. Any subsequent educational efforts should involve multiple education entities (undergraduate medical education, graduate medical education), medical certifying entities (American Board of Medical Specialties), and professional medical societies. Periodic surveys to assess educational efforts will serve to highlight progress and focus on additional needs.
Abbreviations
- AAP:
-
American Academy of Pediatrics
- GPCI:
-
Genetics in Primary Care Institute
- FHH:
-
Family health history
- PCP:
-
Primary care provider
- PS:
-
Periodic survey
References
Doerr M, Edelman E, Gabitzsch E, Eng C, Teng K (2014) Formative evaluation of clinician experience with integrating family history-based clinical decision support into clinical practice. J Pers Med 4(2):115–136. doi:10.3390/jpm4020115
Edelman EA, Lin BK, Doksum T, Drohan B, Edelson V, Dolan SM, Hughes KS, O’Leary J, Galvin SL, Degroat N, Pardanani S, Feero WG, Adams C, Jones R, Scott J (2014) Implementation of an electronic genomic and family health history tool in primary prenatal care. Am J Med Genet C Semin Med Genet 166C(1):34–44. doi:10.1002/ajmg.c.31389
Guttmacher AE, Collins FS, Carmona RH (2004) The family history—more important than ever. N Engl J Med 351(22):2333–2336
http://www.genome.gov/27554614, accessed September 2, 2016 [Inter-Society Coordinating Committee for Practitioner Education in Genomics (ISCC)]
https://geneticsinprimarycare.aap.org/Pages/default.aspx, accessed September 2, 2016
https://geneticsinprimarycare.aap.org/YourPractice/Pages/Toolkit.aspx, pages 15–31, accessed September 2, 2016
https://www.acmg.net/, accessed September 5, 2016
Mikat-Stevens N, Larson I, Tarini B (2015) Primary care providers’ perceived barriers towards integration of genetic services: a systematic review of the literature. Genet Med 17(3):169–176
Moeschler J, Shevell M, Committee on Genetics of the AAP (2014) Comprehensive evaluation of the child with intellectual disability or global developmental delays. Pediatrics 134(3):e903–e918. doi:10.1542/peds.2014-1839
Pyeritz RE (2012) The family history: the first genetic test and still useful after all those years? Genet Med 14(1):3–9
Rinke ML, Driscoll A, Mikat-Stevens N, Healy J, Colantuoni E, Elias AF, Pletcher BA, Gubernick RS, Larson I, Chung WK, Tarini BA (2016) A quality improvement collaborative to improve pediatric primary care genetic services. Pediatrics 137(2):1–10
Rinke ML, Mikat-Stevens N, Saul R, Driscoll A, Healy J, Tarini BA (2014) Genetic services and attitudes in primary care pediatrics. Am J Med Genet A 164A(2):449–455
Saul RA (2013) Genetic and genomic literacy in pediatric primary care. Pediatrics 132:S198–S202
Scott J, Trotter T (2013) Primary care and genetics and genomics. Pediatrics 132:S231–S237
Tarini BA, McInerney JD (2013) Family history in primary care pediatrics. Pediatrics 132:S203–S210
Wu RR, Myers RA, McCarty CA, Dimmock D, Farrell M, Cross D, Chinevere TD, Ginsburg GS, Orlando LA, Family Health History Network (2015) Protocol for the “implementation, adoption, and utility of family history in diverse care settings” study. Implement Sci 10:163. doi:10.1186/s13012-015-0352-8
Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ (2002) (2002). Can family history be used as a tool for public health and preventive medicine? Genet Med 4(4):304–310
Acknowledgements
The authors wish to thank Karen O’Connor from the Division of Research of the American Academy of Pediatrics for her valuable assistance with the preparation of the tables, manuscript preparation, and manuscript review.
Contributors’ statements
Robert A. Saul: Dr. Saul assisted in the design of the survey, drafted the initial manuscript, and approved the final manuscript as submitted.
Tracy Trotter: Dr. Trotter critically reviewed the manuscript, revised the manuscript, and approved the final manuscript as submitted.
Kerry Sease: Dr. Sease critically reviewed the manuscript, revised the manuscript, and approved the final manuscript as submitted.
Beth Tarini: Dr. Tarini assisted in the design of the survey, critically reviewed the manuscript, revised the manuscript, and approved the final manuscript as submitted.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding source
No funding was secured for this study.
Financial disclosure
The authors (Saul, Trotter, Sease and Tarini) have no financial relationships relevant to this article to disclose.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Beth Tarini was formerly affiliated to Department of Pediatrics, University of Michigan, Ann Arbor, MI
Rights and permissions
About this article
Cite this article
Saul, R.A., Trotter, T., Sease, K. et al. Survey of family history taking and genetic testing in pediatric practice. J Community Genet 8, 109–115 (2017). https://doi.org/10.1007/s12687-016-0291-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-016-0291-3