Abstract
Groundbreaking progress has been recently made in elucidating the signaling pathways that are altered in adrenocortical carcinoma (ACC), an endocrine malignancy that still has an unfavorable prognosis, and in understanding its genomic structure. These advances need now to be translated to create cellular and animal models more relevant to human disease in order to develop new and more effective diagnostic procedures and targeted therapies against this deadly malignancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adrenocortical carcinoma (ACC) is a rare endocrine malignancy with a poor prognosis. Surgery could be curative in the great majority of cases with localized disease, but ACC often relapses or is already metastatic at the time of diagnosis. In those cases, therapeutic options are limited to the use of mitotane, an adrenolytic drug whose introduction in ACC treatment dates back to 1960s, that can be associated to systemic chemotherapy [1, 2]. However, therapeutic results have generally remained poor and a consensus exists about the urgent need for novel drugs that are more efficient to fight against this deadly malignancy. A steadily increasing number of laboratories worldwide is therefore actively engaged in basic and translational research to develop better therapies for ACC. A critical element for those developments consists in a better understanding of the biology of ACC, and in particular of the molecular mechanisms that regulate its growth and spread, through approaches that include the identification of new biomarkers for disease diagnosis and relapse, the generation of new cell and animal models and the preclinical testing of new therapies. The last session (Closing the gap at the bench: molecules to organisms) at the recent 5th International Adrenal Cancer Symposium (Ann Arbor MI, October 14–15, 2015) provided a unique opportunity for both basic scientists and clinicians to discuss the latest developments in the field. Here, we will make a brief discussion of the presentations in Ann Arbor trying to put them in the context of current research in the domain of ACC biology.
New Biomarkers for ACC
MicroRNA (miRNA) is a class of evolutionarily conserved, small non-coding eukaryotic RNA molecules which regulate gene expression at the level of translation. They are implicated in virtually every biological process and also have a relevant role in tumorigenesis. Several studies have reported that a distinct microRNA expression signature can differentiate ACC from adrenocortical benign tumors. In addition, the expression levels of specific miRNAs in the tumor are prognostic markers reviewed in [3]. Recent studies have revealed that circulating miRNAs may represent potential biomarkers of malignancy in ACC patients [4–6]. However, further studies on larger cohorts are needed to precisely assess their diagnostic and prognostic role, in particular to monitor tumor recurrence. A new twist in the field of miRNA is their potential use as therapeutic tools. At the Ann Arbor meeting, Dr. Stan Sidhu (University of Sydney, Australia) presented results of a recently published study from his group showing that miR-7, which has a tumor suppressor role in ACC, can reduce growth of H295R and primary ACC cells xenografts when administered in the form of targeted, clinically safe delivery vesicles (nanocells) [7].
Another promising area of research is the study of circulating tumor cells (CTCs) in ACC patients. CTCs are neoplastic cells originating from either the primary tumor or metastases, which can be detected and isolated in the peripheral blood of cancer patients. CTCs are a reliable tool for prognosis and follow-up in several solid human malignancies [8]. A preliminary study has revealed that CTCs are present in the circulation of ACC patients but not in patients with benign adrenocortical tumors. In addition, a significant decrease in the number of CTCs has been reported following surgery compared to presurgical samples [9]. CTCs isolation may allow to obtain a “liquid biopsy” of ACC, which could be especially useful to monitor the occurrence of relapses and to study the evolution of ACC genomes during disease progression or chemotherapeutic treatments. Other approaches that may provide in the near future minimally invasive access to ACC genetic information for diagnostic and prognostic purposes include the study of cell-free DNA and exosomes in the bloodstream [10], while differential analysis of the urinary steroid metabolome may help to distinguish malignant from benign adrenal tumors [11, 12].
Cellular Models for ACC
Compared to most other malignancies, one serious shortcoming of ACC is the availability of virtually only one differentiated human adrenocortical cell line, the NCI-H295 and its derivatives reviewed in [13]. Another human cell line (SW-13), which has been used in several studies as a model for ACC, lacks expression of adrenocortical markers and does not produce steroids [13, 14]. Therefore, its usefulness as an ACC model cell line is highly questionable. As an additional tool, the SJ-ACC3 human adrenocortical cell line has been established from a pediatric tumor. This cell line only grows as subcutaneous xenografts in immunodeficient mice [15]. More recently, another pediatric cell line growing as xenografts has been established in the same laboratory from a different patient (G. Zambetti, personal communication). At the Ann Arbor meeting, Dr. Constanze Hantel (University of Munich, Germany) described a new human adrenocortical xenograft model (MUC-1), also growing as a cell line, established in her laboratory from a neck metastasis of an adult ACC. These new ACC cell lines will be very important in the near future to expand and diversify the studies on adrenocortical cells beyond the NCI-H295 model.
Animal Models for ACC
A few animal models have been reported for ACC. Some of them exploit injection of adrenocortical cell lines (most commonly NCI-H295) in immunodeficient mice, while others are derived from genetically modified animals.
-
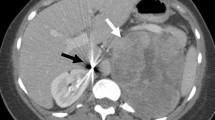
Xenograft models: the first report of a subcutaneous xenograft animal model for ACC dates back to 2000 [16]. Since that time, numerous studies have used this model to monitor its sensitivity to different drug treatments reviewed in [17]. A major drawback of this model is the absence of the capacity to metastasize, which is in sharp contrast to human ACC. This renders the subcutaneous xenograft model not convenient for studies aimed at investigation of the cellular and molecular mechanisms of metastasis formation in ACC and to test therapies for metastatic disease. An orthotopic model of ACC consisting in normal bovine adrenocortical cells implanted under the renal capsule of immunodeficient mice has also been described. Genetic modification of those cells with an oncogenic version of Ras and a dominant-negative p53 induced malignant tumor formation with local dissemination [18]. Possibilities to boost the metastatic capacities of adrenocortical cells in future studies may include the use of new administration routes (intravenous, etc.) and the modulation of the expression of endogenous factors (adhesion molecules, cytokines, etc.) favoring metastasis formation.
-
Genetic models: genetic models of adrenocortical neoplasia have been described, but in general, they exhibit only limited malignant character.
-
a)
Gonadectomy can induce neoplasia in the adrenal cortex of the domestic ferret and in some strains of mice, as well as in some lines of genetically modified mice in a non-neoplasia-prone background reviewed in [19]. Transgenic mice harboring multiple copies of the Sf-1 (Nr5a1) gene also develop adrenocortical neoplasia in the absence of gonadectomy [20]. The common features of those models are proliferation of neoplastic cells in a subcapsular location in the adrenal expressing gonadal markers, most probably derived from undifferentiated adrenogonadal progenitors [21] and little tendency to spread beyond the locoregional location.
-
b)
Other genetic models of adrenocortical neoplasia are based on genes and signaling pathways that are altered in ACC.
Wnt/β-Catenin
A seminal study by Tissier et al. first showed that activation of the Wnt/β-catenin signaling pathway is a hallmark of both benign and malignant adrenocortical tumors [22]. Further genomic studies have confirmed that gene mutations that have the consequence to activate this pathway are encountered at high frequency both in adult [23] and children [24] adrenocortical tumors. Remarkably, the gene most frequently mutated or deleted in adult ACC is ZNRF3, encoding a E3 ubiquitin-protein ligase that acts as a negative regulator of the Wnt signaling pathway by mediating the ubiquitination and degradation of the Wnt receptor complex components Frizzled and LRP6. Studies in various mouse models have shown that β-catenin activation in the adrenal has relatively weak oncogenic effects, even when combined with overexpression of the IGF2 growth factor [25–27], suggesting the requirement of further genetic hits for tumor development. Based on the results in human ACC, it will be interesting to study the effect of mouse Znrf3 inactivation on adrenocortical tumor development. However, β-catenin antagonism either by drugs [28] or by RNA interference [29, 30] is able to significantly decrease ACC cell proliferation in vitro and their growth as xenografts. Those data suggest that counteracting β-catenin activity in ACC could be a promising therapeutic strategy to be assessed by future studies. However, it will very important to tailor the choice of Wnt pathway inhibitors, targeting with drugs either upstream components (porcupine and tankyrase inhibitors) or downstream effectors (CBP, p300) of the pathway [31], according to the specific genetic alterations present in the individual patient with ACC.
TP53
Germline mutations in the tumor suppressor TP53 gene are associated with Li-Fraumeni syndrome, a multiple tumor syndrome one of whose hallmarks is the high frequency of adrenocortical tumors [32]. On the other side, adrenocortical tumors in children are often associated with germline TP53 mutations in the absence of other neoplasms [33, 34]. A peculiar epidemiological situation is present in southern Brazil, where the R337H TP53 mutation is present at a very high frequency (0.3 %) in the population and is associated with adrenocortical tumors in children with low penetrance [35, 36]. Conversely, TP53 germline mutations are uncommonly found in patients diagnosed with ACC as adults [37, 38] but somatic alterations in the p53/Rb pathway were identified in about 30 % of adult ACC [23]. This pathway then appears to represent a major driver of oncogenic transformation in ACC, similarly to many other malignancies. A new transgenic mouse model was presented at the Ann Arbor meeting by Dr. Pierre Val (University of Clermont, Clermont-Ferrand, France) where expression the SV40 T antigen, which binds to and inactivates both the p53 and the Rb tumor suppressor proteins, was targeted to the adrenal cortex under the control of the Akr1b7 promoter ([39] and A.M. Lefrançois-Martinez, personal communication). Adrenal T transgenic mice develop adrenocortical carcinomas that metastasize with high frequency and will provide a very useful model to test novel therapies against metastatic ACC. Studies are also in progress in Dr. Gerard Zambetti’s laboratory (St. Jude Children’s Research Hospital, Memphis TN, USA) to characterize the phenotype of mice bearing the targeted R334H Tp53 mutation, homologous to human R337H (G. Zambetti, personal communication).
Novel Drugs and Strategies for ACC Treatment
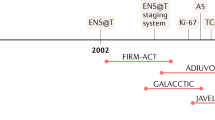
The recent conspicuous advances in our understanding of ACC biology have led to the proposal of a series of new therapies targeting some among the major actors in ACC pathogenesis; see [40–42] for review. However, for the moment, novel drugs have not gone beyond the preclinical stage of investigation or have produced unsatisfactory results when introduced in the clinic. This has been the case for IGF-1R inhibitors, whose trial in ACC patients was based on promising preclinical data [43, 44]. However, a clinical trial with the orally available IGF-1R inhibitor linsitinib (OSI-906) did not show positive effects of the drug on overall or progression-free survival in ACC patients [45]. Several elements can be invoked to account for those disappointing results:
-
The trial involved patients with advanced disease who already received intense chemotherapeutic treatment.
-
Since a partial response was observed in a small group of patients in that study, the identification of predictive biomarkers may help to identify patients that will benefit from IGF-1R inhibitors therapy.
-
Other drugs may need to be associated to IGF-1R inhibitors to completely block downstream signaling pathways regulating proliferation and apoptosis of ACC cells. Another study in fact observed disease stabilization in ACC patients treated with a combination of the IGF-1R antibody cixutumumab and the mTOR inhibitor temsirolimus [46].
Recent studies suggest that the SOAT1 (Sterol-O-Acetyl Transferase 1) enzyme is a novel emerging therapeutic target in ACC. In Ann Arbor, Dr. Matthias Kroiss (University of Würzburg, Germany) presented the results of a groundbreaking study from his group that for the first time identified a molecular target for mitotane. Mitotane was found to inhibit SOAT1, causing accumulation of free cholesterol, oxysterols and fatty acids inside adrenocortical cells, induction of ER stress and, ultimately, cell death. The study by the Würzburg team has also shown that SOAT1 expression levels are variable in ACC, being low or absent in about one third of cases [47]. This provides a rationale to screen patients with ACC for SOAT1 expression in their tumor to predict their response to mitotane. In another session of the symposium, Dr. Gary Hammer presented data showing the efficacy of ATR-101, a new orally available SOAT1 inhibitor, in preclinical models of ACC. A phase I clinical trial for safety and tolerability of ATR-101 is currently ongoing (https://clinicaltrials.gov/ct2/show/NCT01898715).
Conclusion
The recent great advances in our understanding of ACC biology need now to be translated to create cellular and animal models that are closer to the human disease in order to develop new, more effective diagnostic procedures and targeted therapies against this deadly neoplasm. Close collaboration between basic scientists and clinicians as well as maintenance and further expansion of international ACC patients registries is considered essential for the success of this endeavor.
References
Terzolo M, Angeli A, Fassnacht M et al (2007) Adjuvant mitotane treatment for adrenocortical carcinoma. N Eng J Med 356:2372–2380
Fassnacht M, Terzolo M, Allolio B et al (2012) Combination chemotherapy in advanced adrenocortical carcinoma. N Eng J Med 366:2189–2197
Singh P, Soon PSH, Feige J-J et al (2012) Dysregulation of microRNAs in adrenocortical tumors. Mol Cell Endocrinol 351:118–128
Chabre O, Libé R, Assie G et al (2013) Serum miR-483-5p and miR-195 are predictive of recurrence risk in adrenocortical cancer patients. Endocr Relat Cancer 20:579–594
Patel D, Boufraqech M, Jain M et al (2013) MiR-34a and miR-483-5p are candidate serum biomarkers for adrenocortical tumors. Surgery 154:1224–1228
Szabó DR, Luconi M, Szabó PM et al (2014) Analysis of circulating microRNAs in adrenocortical tumors. Lab Invest 94:331–339
Glover AR, Zhao JT, Gill AJ et al. (2015) microRNA-7 as a tumor suppressor and novel therapeutic for adrenocortical carcinoma. Oncotarget
Sun YF, Yang XR, Zhou J et al (2011) Circulating tumor cells: advances in detection methods, biological issues, and clinical relevance. J Cancer Res Clin Oncol 137:1151–1173
Pinzani P, Scatena C, Salvianti F et al (2013) Detection of circulating tumor cells in patients with adrenocortical carcinoma: a monocentric preliminary study. J Clin Endocrinol Metab 98:3731–3738
Cai X, Janku F, Zhan Q et al (2015) Accessing genetic information with liquid biopsies. Trends Genet 31:564–575
Arlt W, Biehl M, Taylor AE et al (2011) Urine steroid metabolomics as a biomarker tool for detecting malignancy in adrenal tumors. J Clin Endocrinol Metab 96:3775–3784
Kerkhofs TM, Kerstens MN, Kema IP et al (2015) Diagnostic value of urinary steroid profiling in the evaluation of adrenal tumors. Horm Cancer 6:168–175
Wang T, Rainey WE (2012) Human adrenocortical carcinoma cell lines. Mol Cell Endocrinol 351:58–65
Doghman M, Cazareth J, Douguet D et al (2009) Inhibition of adrenocortical carcinoma cell proliferation by steroidogenic factor-1 inverse agonists. J Clin Endocrinol Metab 94:2178–2183
Pinto EM, Morton C, Rodriguez-Galindo C et al (2013) Establishment and characterization of the first pediatric adrenocortical carcinoma xenograft model identifies topotecan as a potential chemotherapeutic agent. Clin Cancer Res 19:1740–1747
Logié A, Boudou P, Boccon-Gibod L et al (2000) Establishment and characterization of a human adrenocortical carcinoma xenograft model. Endocrinology 141:3165–3171
Hantel C, Beuschlein F (2015) Xenograft models for adrenocortical carcinoma. Mol Cell Endocrinol
Herbet M, Salomon A, Feige JJ et al (2012) Acquisition order of Ras and p53 gene alterations defines distinct adrenocortical tumor phenotypes. PLoS Genet 8:e1002700
Bielinska M, Kiiveri S, Parviainen H et al (2006) Gonadectomy-induced adrenocortical neoplasia in the domestic ferret (Mustela putorius furo) and laboratory mouse. Vet Pathol 43:97–117
Doghman M, Karpova T, Rodrigues GA et al (2007) Increased steroidogenic factor-1 dosage triggers adrenocortical cell proliferation and cancer. Mol Endocrinol 21:2968–2987
Looyenga BD, Hammer GD (2006) Origin and identity of adrenocortical tumors in inhibin knockout mice: implications for cellular plasticity in the adrenal cortex. Mol Endocrinol 20:2848–2863
Tissier F, Cavard C, Groussin L et al (2005) Mutations of β-catenin in adrenocortical tumors: activation of the Wnt signaling pathway is a frequent event in both benign and malignant adrenocortical tumors. Cancer Res 65:7622–7627
Assié G, Letouzé E, Fassnacht M et al (2014) Integrated genomic characterization of adrenocortical carcinoma. Nat Genet 46:607–612
Pinto EM, Chen X, Easton J et al (2015) Genomic landscape of paediatric adrenocortical tumours. Nat Comm 6:6302
Berthon A, Sahut-Barnola I, Lambert-Langlais S et al (2010) Constitutive beta-catenin activation induces adrenal hyperplasia and promotes adrenal cancer development. Hum Mol Genet 19:1561–1576
Heaton JH, Wood MA, Kim AC et al (2012) Progression to adrenocortical tumorigenesis in mice and humans through insulin-like growth factor 2 and β-catenin. Am J Pathol 181:1017–1033
Drelon C, Berthon A, Ragazzon B et al (2012) Analysis of the role of Igf2 in adrenal tumour development in transgenic mouse models. PLoS One 7:e44171
Doghman M, Cazareth J, Lalli E (2008) The T cell factor/beta-catenin antagonist PKF115-584 inhibits proliferation of adrenocortical carcinoma cells. J Clin Endocrinol Metab 93:3222–3225
Gaujoux S, Hantel C, Launay P et al (2013) Silencing mutated β-catenin inhibits cell proliferation and stimulates apoptosis in the adrenocortical cancer cell line H295R. PLoS One 8:e55743
Salomon A, Keramidas M, Maisin C et al (2015) Loss of β-catenin in adrenocortical cancer cells causes growth inhibition and reversal of epithelial-to-mesenchymal transition. Oncotarget 6:11421–11433
Kahn M (2014) Can we safely target the WNT pathway? Nat Rev Drug Discov 13:513–532
Wagner J, Portwine C, Rabin K et al (1994) High frequency of germline p53 mutations in childhood adrenocortical cancer. J Natl Cancer Inst 86:1707–1710
Varley JM, McGown G, Thorncroft M et al (1999) Are there low-penetrance TP53 alleles? Evidence from childhood adrenocortical tumors. Am J Hum Genet 65:995–1006
Wasserman JD, Novokmet A, Eichler-Jonsson C et al (2015) Prevalence and functional consequence of TP53 mutations in pediatric adrenocortical carcinoma: a children’s oncology group study. J Clin Oncol 33:602–609
Ribeiro RC, Sandrini F, Figueiredo B et al (2001) An inherited p53 mutation that contributes in a tissue-specific manner to pediatric adrenal cortical carcinoma. Proc Natl Acad Sci U S A 98:9330–9335
Custódio G, Parise GA, Kiesel FN et al (2013) Impact of neonatal screening and surveillance for the TP53 R337H mutation on early detection of childhood adrenocortical tumors. J Clin Oncol 31:2619–2626
Herrmann LJM, Heinze B, Fassnacht M et al (2012) TP53 germline mutations in adult patients with adrenocortical carcinoma. J Clin Endocrinol Metab 97:E476–E485
Raymond VM, Else T, Everett JN et al (2013) Prevalence of germline TP53 mutations in a prospective series of unselected patients with adrenocortical carcinoma. J Clin Endocrinol Metab 98:E119–E125
Ragazzon B, Lefrançois-Martinez AM, Val P et al (2006) Adrenocorticotropin-dependent changes in SF-1/DAX-1 ratio influence steroidogenic genes expression in a novel model of glucocorticoid-producing adrenocortical cell lines derived from targeted tumorigenesis. Endocrinology 147:1805–1818
Maluf DF, de Oliveira BH, Lalli E (2011) Therapy of adrenocortical cancer: present and future. Am J Cancer Res 1:222–232
Kerkhofs TMA, Ettaieb MHT, Hermsen IGC et al (2015) Developing treatment for adrenocortical carcinoma. Endocr Relat Cancer 22:R325–R338
Creemers SG, Hofland L, Korpershoek E et al. (2015) Future directions in the diagnosis and medical treatment of adrenocortical carcinoma. Endocr Relat Cancer
Almeida MQ, Fragoso MCBV, Lotfi CFP et al (2008) Expression of insulin-like growth factor-II and its receptor in pediatric and adult adrenocortical tumors. J Clin Endocrinol Metab 93:3524–3531
Barlaskar F, Spalding AC, Heaton JH et al (2009) Preclinical targeting of the type I insulin-like growth factor receptor in adrenocortical carcinoma. J Clin Endocrinol Metab 94:204–212
Fassnacht M, Berruti A, Baudin E et al (2015) Linsitinib (OSI-906) versus placebo for patients with locally advanced or metastatic adrenocortical carcinoma: a double-blind, randomised, phase 3 study. Lancet Oncol 16:426–435
Naing A, Lorusso P, Fu S et al (2013) Insulin growth factor receptor (IGF-1R) antibody cixutumumab combined with the mTOR inhibitor temsirolimus in patients with metastatic adrenocortical carcinoma. Br J Cancer 108:826–830
Sbiera S, Leich E, Liebisch G et al (2015) Mitotane inhibits Sterol-O-Acyl transferase 1 triggering lipid-mediated endoplasmic reticulum stress and apoptosis in adrenocortical carcinoma cells. Endocrinology 156:3895–3908
Acknowledgments
We thank the speakers of the session “Closing the gap at the bench: molecules to organisms” at the Ann Arbor meeting, Gerard Zambetti and Anne-Marie Lefrançois-Martinez, for allowing us to cite their unpublished results before publication. Matthias Kroiss is also thanked for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
5th International ACC Symposium Session: Closing the Gap at the Bench: Molecules to Organisms
Rights and permissions
About this article
Cite this article
Lalli, E., Sasano, H. 5th International ACC Symposium: An Outlook to Current and Future Research on the Biology of Adrenocortical Carcinoma: Diagnostic and Therapeutic Applications. HORM CANC 7, 44–48 (2016). https://doi.org/10.1007/s12672-015-0240-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-015-0240-3